Abstract
The plasmid DNA encoding the fliC gene of Burkholderia pseudomallei combined with CpG oligodeoxynucleotide (ODN) was injected intramuscularly into BALB/c mice, resulting in the increased production of certain humoral antibodies and flagellin-specific spleen cell clonal expansion. CpG ODN, as an immunoadjuvant, was added to the plasmid containing the fliC gene in order to obtain ongoing expression in muscle for a long period. Functional expression of flagellin from the constructed CpG-modified plasmid in transfected peritoneal exudate cells of BALB/c mice was shown by reverse transcription-PCR and Western blotting. Furthermore, BALB/c mice immunized with the modified plasmid had relatively higher resistance to B. pseudomallei infection in vivo than did mice immunized with unmodified plasmid DNA. The time course of restricted bacterial growth in spleen and liver and changes in the cytokine profiles of immunized mice suggested that the stimulated phagocytic cells would be able to kill the bacteria eventually, possibly as a consequence of the induction of Th-1-type immune polarization in vivo. Th-1-type immune polarization was detected in response to flagellin induction in mice immunized with CpG-modified plasmid DNA by the appearance of increased levels of immunoglobulin G2a antibodies and gamma interferon-secreting cells specific to flagellin. The exogenous CpG motifs added to the fliC gene would contribute to an adjuvant-like response that enhances the flagellin-specific immunogenicity and provides protection against B. pseudomallei infection. This CpG-modified plasmid DNA vaccination is an important potential strategy that should be developed to protect against melioidosis.
Burkholderia pseudomallei, a causative agent of melioidosis, often causes various symptoms ranging from an unapparent, localized, chronic infection to a fully blown systemic infection (4). Acute septicemia manifests as the most serious form for patients with melioidosis (3). At the onset of the disease, the bacterium seems to invade the cells of the host and persist for a long latency period. A fatal relapse can occur many years after the initial infection (11). Immunocompromised patients, in particular those suffering from diabetes mellitus, may easily acquire a B. pseudomallei infection, a situation which can become life threatening (3). Clinically, prolonged treatment with antibiotics such as ceftazidime or amoxicillin-clavulanate is required to cure melioidosis (38). Vaccination would be an extremely valuable and preferred approach to prevent adults from suffering a relapse or as a treatment for immunocompromised patients who are admitted with melioidosis (26).
Based upon their relatively high immunogenicity and their ability to induce humoral antibodies, several somatic antigens such as lipopolysaccharide (LPS) and flagellin protein have been reported as potential targets for use as vaccines for melioidosis (1, 2). However, despite active or passive immunization with these antigens, the protection against B. pseudomallei infection is insufficient (21, 27). In a mouse model for B. pseudomallei infection, C57BL/6 mice (relatively resistant to B. pseudomallei) have revealed significant up-regulation of immunoglobulin G2a (IgG2a) production and the Th-1-related cytokines, while BALB/c mice, susceptible to B. pseudomallei infection, showed much lower levels of induction (19, 35). The use of monoclonal antibodies to neutralize the Th-1-related cytokines in mice, gamma interferon (IFN-γ), tumor necrosis factor alpha (TNF-α), and interleukin-12 (IL-12), resulted in these mice being susceptible to subsequent B. pseudomallei infection (30). It seems that the Th-1 immune response plays an important defense role in protecting against B. pseudomallei infection. However, these vaccines, which are currently under development, because they use purified somatic antigens or recombinant proteins are hampered in their ability to induce a cell-mediated immune (CMI) response, and therefore this may limit their potential (8).
Plasmid DNA vaccination, a strategy that allows for the development of a strong CMI, has been recognized as an efficacious immunization route against intracellular bacteria (10, 15-16, 23). The CpG motif (PuPuCpGPyPy) provides an adjuvant-like response that improves the specific immunity of the genes of interest. The CpG motif has been reported to contribute to the induction of strong immunogenicity in animals after DNA vaccination (23). Sato et al. showed that plasmid DNA with a CpG motif could induce high antibody, CMI, and IFN-γ production in mice (31). Klinman et al. reported that CpG motifs inserted upstream of a cytomegalovirus enhancer and downstream of a terminator of a gene of interest produced predominantly a Th-1-type cytokine response (22). Recognizing that the Th-1-type immune response plays an important defense role in B. pseudomallei infection, we suggest that a CpG-modified DNA vaccine would be able to promote a Th-1-type immune response and thus have protective efficacy against melioidosis.
In this study, the flagellin (fliC) somatic antigen, one of the major components needed for bacterial motility, was used to develop a plasmid DNA vaccine. Although the involvement of flagellin in pathogenesis is ambiguous, the flagellin protein is still recognized as a vaccine target because antiflagellin antibody can inhibit bacterial motility in vitro and also provides some protection against B. pseudomallei infection when used for passive immunization (1, 9, 12). We have therefore explored its protective role against melioidosis in BALB/c mice by using plasmid DNA vaccination. Further, the plasmid DNA encoding the flagellin protein has been modified by the addition of two immunostimulatory CpG motifs.
MATERIALS AND METHODS
ODNs and plasmids.
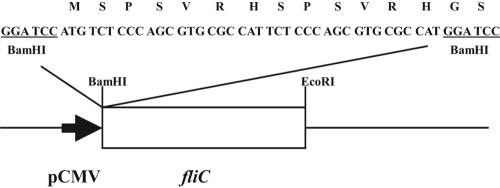
The oligodeoxynucleotides (ODNs) as synthesized by MdBio Inc. (Taipei, Taiwan) are made up of DNA consisting of an unmethylated CpG motif (5′-TCT CCC AGC GTG CGC CAT-3′) and based upon the work of Elkins et al. (13). The mammalian expression vector pcDNA3/fliC encoding the B. pseudomallei flagellin was created from pGEX4T-2/fliC using appropriate restriction sites (7). This unmethylated ODN (containing two CpG motifs) was added to the plasmid sequence using BamHI linkers on the oligonucleotide sequence of the ODN (Fig. 1). The CpG-modified plasmid construct (pcDNA3/CpG-fliC) was confirmed by DNA sequencing.
FIG. 1.
An illustration of plasmid pcDNA3/CpG-fliC construction. The ODN (5′-TCT CCC AGC GTG CGC CAT-3′) was added onto the plasmid pcDNA3/fliC (driven by the cytomegalovirus promoter, pCMV) using BamHI linkers.
DNA transfection and expression.
The preparation of peritoneal exudate cells (PECs) followed the procedures described in the previous report (34). Transient transfection was performed using Lipofectin reagent (Gibco-BRL, Paisley, United Kingdom) according to the manufacturer's instructions. The transfected cells were harvested 48 h later and washed three times with phosphate-buffered saline (PBS). Total RNA was extracted using Trizol reagent (Life Technologies Inc., Rockville, MD). Reverse transcription-PCR (RT-PCR) amplification was performed using the Fast-Run Moloney murine leukemia virus RT-PCR kit (Promega Inc., Madison, WI) with the specific primers for the fliC gene. The reaction was carried out in a thermal cycler (Perkin-Elmer 2400; Perkin-Elmer Inc., Wellesley, MA,). The following profile was set up: 37°C for 1 h (one cycle); 94°C for 5 min (one cycle); and 94°C for 1 min, 61°C for 1 min, and 72°C for 1.5 min (30 cycles). The amplified products were analyzed on a 1% agarose gel. The cell culture was also used to prepare total cell extracts, and then immunoblotting was performed to analyze the specific gene expression (7).
Immunization of mice.
Six-week-old female BALB/c mice were obtained from the Laboratory Animal Center (Taipei, Taiwan) of the National Science Council. The mice were randomly assigned, six to an experimental group. All immunizations of the mice were carried out by intramuscular injection. The first group was immunized with pcDNA3/fliC (50 μg) in PBS and codelivered with CpG ODN at various doses ranging from 1 to 100 μg. The second group was immunized with the CpG-modified plasmid, pcDNA/CpG-fliC (100 μg). The third group was immunized with the unmodified plasmid pcDNA3/fliC (200 μg). As controls, mice were injected with pcDNA3 vector alone or PBS alone. The data for antibody analysis derived from mice injected with PBS gave the same results as for the pcDNA3 control group and are therefore not shown in data sheets. Each animal was boosted twice with the same doses.
Antibody analysis.
Serum samples were collected in the tail vein at a 2-week interval. Total IgG and the IgG specific to flagellin levels were analyzed by enzyme-linked immunosorbent assay. Briefly, the 96-well microplates were coated with flagellin (0.5 μg/ml) overnight at 4°C. The flagellin preparation was performed according to a procedure described in a previous report (7). The contaminant LPS was removed from the flagellin preparation by passage through a polymyxin B column according to the manufacturer's instructions (Detoxi-Gel; Pierce Chemical Co., Rockford, IL). In this study, the LPS concentration of flagellin was kept at the dose of <0.5 ng/ml. The plates were washed and incubated with twofold serial dilutions of serum samples after an 8-week immunization for 1 h at 37°C. The diluted (1:1,000) anti-mouse IgG (IgG1, IgG2a, IgG2b, or IgG3) conjugated with peroxidase (Zymed, San Francisco, CA) was then added and incubated for 1 h at 37°C. The reacting solutions were read at an optical density at 405 nm in an Anthos 2010 microplate reader (Anthos Labtec Instruments GmbH, Wals, Salzburg, Austria).
Proliferation of spleen cells.
The six mice per test group were sacrificed after an 8-week immunization. The spleen of each sacrificed mouse was separated using a syringe needle and dispersed through a 70-μm wire mesh screen. The proliferation of the spleen cell preparations (2 × 105 cells/well) was measured as described in a previous report (5). In order to determine the measurement of stimulation, flagellin antigen (10 μg/well) was added to the tested wells for 3 days of incubation. Concanavalin A (5 μg/ml) was used as a positive control. The stimulation index was defined as the ratio of [3H]thymidine uptake (counts per minute) of the flagellin antigen-stimulated cells to the corresponding counts for the nonstimulated control (medium only).
Cytokine assays.
The induction of IFN-γ was evaluated by enzyme-linked immunospot assay (ELISPOT; Biosource, Camarillo, CA). The assay for up-regulation of IFN-γ cytokines was conducted by the standard manufacturer protocols (Biosource). The spleen cells (5 × 105 cells/well) from each mouse were seeded onto the plates, and the flagellin (10 μg/ml) was used for stimulation for 5 h at 37°C. After the formation of spots, the spot numbers were scored with the aid of a dissecting microscope. The IFN-γ-secreting formation units were determined as the mean of triplicate wells.
Protection assay.
The 16 strains of B. pseudomallei (Table 1) originated from melioidosis patients admitted to the Kaohsiung Veterans General Hospital (6). The isolates were confirmed by standard biochemical tests and ID 32 GN profiles from commercial kits (API system; BioMérieux, Marcy l'Etoile, France).
TABLE 1.
Strains, isolation, and characterization of B. pseudomallei isolates in this study
| Strain no. | Isolation
|
Disease presentation
|
||
|---|---|---|---|---|
| Origin | Time (yr) | Clinical manifestation(s) | Outcome | |
| VGH01 | Blood | 1994 | Pneumonia with empyema | Cure |
| VGH02 | Blood | 1994 | Peritonitis | Death |
| VGH03 | Blood | 1994 | Mycotic aneurysm, abdominal aorta | Cure |
| VGH04 | Blood | 1995 | Septic pulmonary emboli | Death |
| VGH05 | Blood | 1996 | Septic arthro-osteomyelitis, subcutaneous abscesses | Cure |
| VGH06 | Blood | 1996 | Pneumonia | Death |
| VGH07 | Blood | 1996 | Septic arthro-osteomyelitis | Cure |
| VGH08 | Blood | 1996 | Primary septicemia | Death |
| VGH09 | Splenic abscess | 1996 | Hepatosplenic abscesses | Cure |
| VGH10 | Blood | 1998 | Pneumonia | Death |
| VGH11 | Blood | 1998 | Pneumonia, peritonitis | Death |
| VGH12 | Hepatic abscess | 1998 | Hepatosplenic abscesses | Cure |
| VGH13 | Paraspinal abscess | 2001 | Spondylitis, paraspinal abscess | Cure |
| VGH14 | Blood | 2001 | Multiple organ abscesses (skin, prostate), septic arthro-osteomyelitis | Cure |
| VGH15 | Blood | 2001 | Pneumonia | Cure |
| VGH16 | Blood | 2001 | Mycotic aneurysm, thoracic aorta | Death |
The strains were grown in Luria-Bertani (LB) medium for 16 h at 37°C. The suspensions of 16 isolates were respectively adjusted to an optical density at 660 nm of 0.5. One hundred microliters of each suspension was diluted to the indicated concentration with PBS and then was used for inoculation immediately. Also, this suspension was plated on LB plates to determine the numbers of bacteria by colony counting. Subsequent to an 8-week immunization period, mice were inoculated via the tail vein with 105 CFU of the mixed B. pseudomallei suspension in sterile PBS (50 μl). Control mice received sterile PBS only. The inoculated mice were killed, and their livers and spleens were excised at the indicated times after inoculation. These organs were weighed and separately homogenized in sterile PBS, and then serial dilutions were plated on LB agar. The numbers of bacteria were counted as CFU. The determination of bacterial loads in liver or spleen was duplicated from six mice (three mice were used in each experiment).
To determine the survival of mice after an infection by B. pseudomallei, 10 mice from each experimental group (immunized with pcDNA3/fliC, pcDNA3/CpG-fliC, or pcDNA3 for 8 weeks) were injected with 105 CFU of B. pseudomallei in the tail vein. Over 14 days, survival of the mice was recorded. Each experimental group was repeatedly treated three times, and the average survival rate was calculated.
RT-PCR assay.
As described above, the spleen was prepared from mice after an infection with B. pseudomallei (105 CFU) at the indicated days. The intensity of cytokine-specific mRNA was measured by the RT-PCR method (35). Total RNA was extracted from spleen cells with Trizol reagent, and RT-PCR amplification was performed. The specific primers (obtained from MdBio Inc.) were used as reported by Ulett et al. (35). The PCR products were electrophoresed on a 2% agarose gel and visualized by staining with ethidium bromide (0.2 μg/ml). The relative intensity of RT-PCR products was quantified using NIH Image software, with β-actin mRNA as a reference control. The level of cytokine-specific mRNA was determined by the average derived from three independent experiments.
Statistical analysis.
A Mann-Whitney U test or Fisher exact test was performed in order to analyze any differences between the test and control groups. Differences were considered significant at P < 0.05.
RESULTS
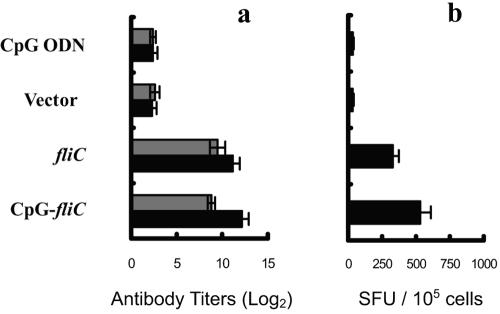
CpG ODN improves the immune response induced by DNA vaccination.
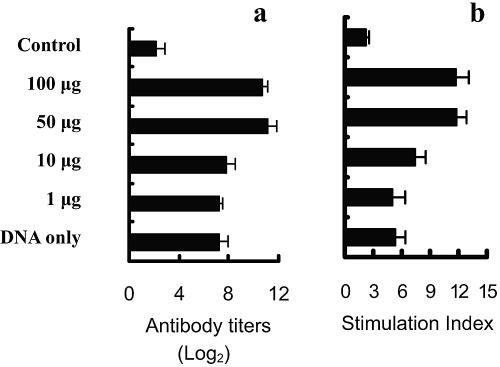
Previously, we found that the BALB/c mice primed and boosted with a suboptimal dose of pcDNA3/fliC (50 μg) were capable of inducing a lower level of antiflagellin antibodies in sera than were mice immunized with 200 μg of pcDNA3/fliC (data not shown). In order to examine whether CpG-mediated activation promotes the development of antigen-specific immunity, pcDNA3/fliC (50 μg) combined with CpG ODN (ranging from 1 to 100 μg) was used to immunize BALB/c mice both for priming and for boosting. A higher antibody response was obtained when CpG ODN was used to “boost” the intramuscular injections. The level of humoral antibody in the mouse sera and the clonal expansion of the spleen cells in response to flagellin were enhanced by the addition of CpG ODN at various concentrations, and this occurred in a dose-response manner (Fig. 2). Thus, the results indicated that CpG ODN could effectively improve the induction of flagellin-specific IgG production and the spleen cell proliferation when the experimental BALB/c mice were immunized with plasmid DNA (50 μg) and CpG ODN (50 μg) together.
FIG. 2.
Improvement of mouse immune response by plasmid DNA in the presence of CpG ODN. The BALB/c mice were immunized with pcDNA3/fliC (DNA only) or in a combination with CpG ODN (doses of CpG ODN ranging from 1 μg to 100 μg). As controls, the mice were immunized with pcDNA3. After an 8-week immunization, the humoral antibodies in the sera (a) and the level of cellular proliferation in spleen cells (b), both specific for flagellin, were determined. Each set of data is based on measurements deriving from six mice.
Protection against B. pseudomallei infection by CpG-modified DNA.
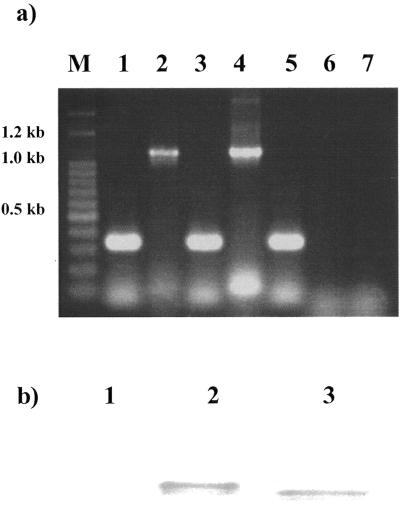
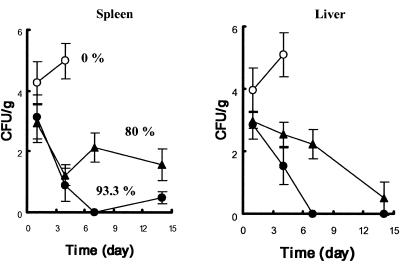
The plasmid pcDNA3-derived gene of interest has been shown to persist in muscle for over 1 year (39). To test whether the CpG motifs provide a selective advantage for backbone anchored in plasmid by promoting a specific immune response that is able to eliminate the infecting bacteria in vivo, two CpG motifs were added into the plasmid (pcDNA3/fliC) and this new plasmid (pcDNA3/CpG-fliC) was used to study the long-term immune response after DNA vaccination. This modified plasmid was functional because, upon transfection, the plasmid was able to transcribe intact mRNA and translate flagellin protein in PECs of BALB/c mice. This was shown by RT-PCR analysis (Fig. 3a) and the presence of a specific immunoreactive band on Western blotting (Fig. 3b). When BALB/c mice were immunized with the modified plasmid (pcDNA3/CpG-fliC), immunogenicity increased in a dose-responsive manner, and it was further shown that 100 μg was the optimal dose for the intramuscular injection of the modified plasmid (data not shown). Thus, mice immunized with 100 μg or 200 μg of pcDNA3/CpG-fliC or pcDNA3/fliC, respectively, were used for the remaining comparative studies. The 50% lethal dose for clinical isolates of B. pseudomallei among BALB/c mice ranges from <101 to 105 CFU (19, 33), and the colony morphology of B. pseudomallei varies concomitantly with an increase in the virulence of this bacterium following in vivo passage through mice (29, 33). Haase et al. (17) indicated that strains different by randomly amplified polymorphic DNA genotyping were isolated from the same patient without reinfection with B. pseudomallei taking place. Regarding the relative complexity of virulence of individual B. pseudomallei strains and variation seen in phenotypic and genotypic change occurring after onset of melioidosis, we determined if the pcDNA3/fliC- or pcDNA3/CpG-fliC-immunized mice would be protected from infection by other strains with different genotypes or phenotypes. Thus, the immunized mice, seropositive for flagellin, were infected with 105 CFU of a mix of different strains of B. pseudomallei, and it appeared that the pcDNA3/CpG-fliC-immunized mice showed a relatively lower bacterial load in the spleen and liver (Fig. 4), two common sites for B. pseudomallei extrapulmonary infection. When strain VGH07 was used as a representative of B. pseudomallei isolates for inoculation into mice, the bacterial loads in liver or spleen in pcDNA3/CpG-fliC-immunized mice were lower than those in the pcDNA3/fliC-immunized mice (data not shown). This indicated that the growth of different strains was indeed restricted in pcDNA3/CpG-fliC-immunized mice. In the control group (BALB/c mice immunized with vector DNA), the bacteria grew rapidly during the initial 2 days of infection. Some bacterial counts were not able to be determined 6 days subsequent to infection because the respective mice were all dead. The survival of immunized mice was followed for 14 days when those mice were injected with B. pseudomallei in the tail vein. The survival values determined from three times of independent experiments with 10 mice for each investigation were found to be 8, 8, and 8 (80% mean survival rate), and 10, 9, and 9 (93.3% mean survival rates) for the pcDNA3/fliC- and pcDNA3/CpG-fliC-immunized mouse groups, respectively. Although the pcDNA3/CpG-fliC-immunized mouse group did not have a higher survival rate (P = 0.254), this group indeed exhibited a significantly low bacterial load (P < 0.05) in vivo on day 14 compared to that in the pcDNA3/fliC-immunized mouse group.
FIG. 3.
Expression of flagellin in PECs. Plasmid pcDNA3/CpG-fliC was transfected into PECs using Lipofectin reagent. (a) After a 48-h transfection, the flagellin-specific mRNA was measured from total RNA extracted in transfectants. The molecular size markers used herein (lane M) included 1.5 kb, 1.2 kb, and ladders from 1 to 0.1 kb. As examples of PECs transfected with pcDNA3/fliC, the RT-PCR products for the β-actin gene and for the fliC gene are shown in lanes 1 and 2, respectively. As examples of PECs transfected with pcDNA3/CpG-fliC, the RT-PCR products for the β-actin gene and for CpG-fliC gene are shown in lanes 3 and 4, respectively. As controls (nontransfected PECs), the RT-PCR products for the β-actin gene, the fliC gene, and the CpG-fliC gene are shown in lanes 5, 6, and 7, respectively. (b) These transfectants were lysed and immunoreacted with antiflagellin antibody. Lane 1, nontransfected PECs; lane 2, PECs transfected with pcDNA3/CpG-fliC; lane 3, PECs transfected with pcDNA3/fliC.
FIG. 4.
Infection by B. pseudomallei of immunized BALB/c mice. The six immunized mice, which were seropositive for flagellin, were infected with 105 CFU of B. pseudomallei by intravenous injection in the tail. After the indicated time, the bacterial survival in the spleen and liver from the pcDNA3/fliC (▴)- or pcDNA3/CpG-fliC (•)-immunized mouse groups was determined. The mice were immunized with pcDNA3 as a control (○). Means and standard deviations for bacterial survival in these two organs were calculated by averaging the measurement of (duplicate) samples deriving from three mice (three mice were used in each experiment).
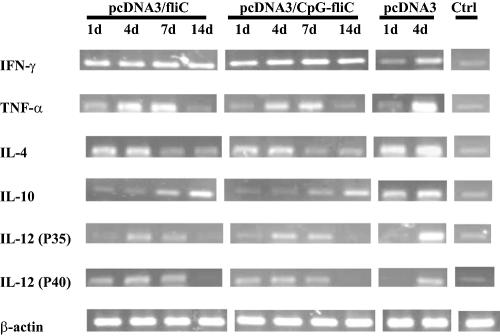
Cytokine gene expression in DNA-vaccinated mice.
Since mice that develop a Th-1 immune response are resistant to B. pseudomallei infection (19), the possibility that the polarization of cytokine expression might contribute to the resistance against B. pseudomallei by immunized mice was examined herein. As shown in Fig. 5, the mean relative intensity of cytokine expression is summarized in Table 2, such results revealing that the relative mRNA expression of the genes for cytokines IFN-γ, TNF-α, IL-12/p35, and IL-12/p40 was significantly increased in immunized mice compared to nonimmunized mice, when β-actin mRNA was used as the internal control. No significant intergroup difference was noted for IL-4. When the profiles for cytokine expression were compared between the two vaccinated mouse groups (pcDNA3/fliC and pcDNA3/CpG-fliC), the maximum level of IFN-γ mRNA (mainly macrophage effector cytokines) was observed to be present on day 7 in both mouse groups, and this cytokine expression was higher in pcDNA3/CpG-fliC-immunized mice than in pcDNA3/fliC-immunized mice (P < 0.05) (Table 2). In the control groups, all cytokine genes (except for IL-4) were overproduced at the onset of B. pseudomallei infection (Table 2).
FIG. 5.
Changes in cytokine profiles. The BALB/c mice were immunized with pcDNA3/fliC, pcDNA3/CpG-fliC, or pcDNA3. The immunized mice, which were seropositive for flagellin, were infected with 105 CFU of B. pseudomallei by intravenous injection in the tail. Subsequent to the indicated time delay (in days), extracted spleen cells were used to examine the intracellular level of cytokine-specific mRNA by RT-PCR.
TABLE 2.
Changes in cytokine profiles
| Cytokine | Relative intensity of cytokine profile (%)a
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| pcDNA3/fliCb
|
pcDNA3/CpG-fliCb
|
pcDNA3b
|
Nonc | ||||||||
| 1 dd | 4 d | 7 d | 14 d | 1 d | 4 d | 7 d | 14 d | 1 d | 4 d | ||
| IFN-γ | 32 ± 2.5 | 31 ± 2.5e | 36 ± 2.0f | 31 ± 3.5f | 30 ± 0.6 | 35 ± 1.5e | 49 ± 1.5 | 40 ± 2.5 | 25 ± 4.5 | 52 ± 3.0 | 3 ± 2.5 |
| TNF-α | 19 ± 3.0 | 34 ± 1.5e | 32 ± 2.0 | 12 ± 2.5 | 20 ± 1.5 | 34 ± 2.1e | 25 ± 2.5 | 8 ± 2.6 | 14 ± 3.1 | 46 ± 4.0 | 3 ± 2.5 |
| IL-4 | 23 ± 2.0 | 21 ± 1.5 | 12 ± 2.0 | 14 ± 1.0 | 22 ± 1.5 | 22 ± 2.6e | 11 ± 3.2 | 11 ± 1.0 | 21 ± 2.5 | 25 ± 2.0 | 2 ± 1.5 |
| IL-10 | 13 ± 2.1 | 13 ± 3.5e | 22 ± 4.1 | 34 ± 3.1 | 13 ± 3.0 | 11 ± 3.2e | 17 ± 3.5 | 43 ± 3.1 | 21 ± 2.5 | 26 ± 3.1 | 2.3 ± 2.5 |
| IL-12(p35) | 25 ± 4.0 | 33 ± 2.5e | 25 ± 1.5 | 4 ± 3.6 | 27 ± 2.5 | 32 ± 1.5e | 27 ± 1.5 | 2.3 ± 2.0 | 23 ± 2.1 | 42 ± 2.5 | 4 ± 2.0 |
| IL-12(p40) | 12 ± 2.5 | 27 ± 2.5e | 19 ± 1.0 | 1.6 ± 2.0 | 15 ± 2.0 | 28 ± 2.6e | 19 ± 1.2 | 1 ± 1.0 | 10 ± 1.5 | 41 ± 3.2 | 2.3 ± 2.1 |
Relative intensity of RT-PCR products was quantified using NIH Image software, with β-actin mRNA as a reference control.
Level of cytokine-specific mRNA expression in the mice immunized with pcDNA3/fliC, pcDNA3/CpG-fliC, and pcDNA3.
Nonimmunized mice used as negative control (without infection).
The indicated day represents the time of exposure to B. pseudomallei by intravenous injection.
Significant difference (P < 0.05) compared with the mouse group immunized with pcDNA3.
Significant difference (P < 0.05) compared with the mouse group immunized with pcDNA3/CpG-fliC on day 7 or day 14, respectively.
Flagellin-induced IgG2a production and IFN-γ secretion.
We further studied whether, following B. pseudomallei infection, there arose a change of Th-1-related cytokine profile for the pcDNA3/CpG-fliC-immunized mice. Both the production of flagellin-specific IgG2a and the number of flagellin-induced IFN-γ-secreting cells among the spleen cells examined were used to evaluate the caliber of Th-1 immune response. The flagellin-specific IgG2a production in BALB/c mice immunized with pcDNA3/CpG-fliC (IgG2a/IgG1 ratio = 11.3) was higher than that in the mouse group immunized with pcDNA3/fliC (IgG2a/IgG1 ratio = 2.7) (Fig. 6a). Upon stimulation with flagellin, there was also an increase in the number of IFN-γ-secreting cells from spleen in the pcDNA3/CpG-fliC group compared to the pcDNA3/fliC mouse group (Fig. 6b). These results indicate that greater Th-1 polarization was generated by the plasmid DNA containing the CpG motifs. In contrast, there was no increase in IgG2a production or IFN-γ-secreting cells specific to flagellin in BALB/c mice immunized with pcDNA3 as a negative control or when CpG ODN alone was injected. Thus, it is possible to exclude direct stimulation by the CpG motif as the reason for the Th-1 inflammation response (Fig. 6). Taken together, the modified CpG plasmid DNA carrying the fliC gene is able to induce flagellin-specific IgG2a production and an increase in IFN-γ-secreting cells, both of which are characteristic of Th-1 polarization. Therefore, that might be the reason that this vaccine can confer effective protection against B. pseudomallei infection in immunized mice.
FIG. 6.
Production of IgG subclasses and IFN-γ-secreting cells. The experimental BALB/c mice were immunized with pcDNA3/CpG-fliC (CpG-fliC), pcDNA3/fliC (fliC), pcDNA3 (vector), or free CpG ODN (CpG ODN). After 8 weeks of immunization, the antibody titers for IgG1 and IgG2a in the sera (a) and the IFN-γ-secreting cells from the spleen (b) specific to flagellin were determined. Each set of data is based upon the results derived from a sample of six mice.
DISCUSSION
It has been reported recently that the CpG ODN induces inflammatory cytokines and confers nonspecific protection against B. pseudomallei innately (36, 40). However, it is not clear whether this motif can create an adjuvant-like response and enhance a specific antigen-induced immune response against the bacterium in vivo. Our finding demonstrates that free CpG ODN enhances the flagellin-specific immune response in BALB/c mice after intramuscular injection with plasmid DNA encoding flagellin. Furthermore, this plasmid DNA, when modified to carry two copies of the CpG motifs, is able to improve resistance against B. pseudomallei infection.
After immunization with a mixture of soluble CpG ODN and plasmid DNA 8 weeks later, specific IgG2a production and spleen cell clonal proliferation increased, which was accompanied by an increase of the amount of CpG ODN injected. However, in this study, it was very difficult to maintain this response for 12 weeks in BALB/c mice, even when the CpG ODN was repeatedly injected (data not shown). By contrast, when the two CpG ODNs were placed ahead of the fliC gene, this new plasmid was able to enhance and prolong the immune response for at least 14 weeks. This confirms that the plasmid DNA containing the CpG motifs is superior to free CpG ODN in terms of persistence in muscle. Upon the immunization of BALB/c mice, the significant humoral and cellular immune responses were induced with 100 μg of pcDNA3/CpG-fliC and 200 μg of pcDNA3/fliC. In conclusion, the CpG-modified plasmid would be a strategy to develop a vaccine.
The levels of inflammatory cytokines, particularly IFN-γ and, to a lesser extent, IL-12 and TNF-α, have been reported to be elevated in BALB/c mice when infected with B. pseudomallei (30). Such cytokine levels have been correlated, to some extent, with the severity of the disease in melioidosis patients (25, 32). Under normal circumstances, an excessive and unregulated production of inflammatory cytokines leads to septic shock and death of the patient, depending on the bacterial burden and the timing of cytokine production relative to the time of bacterial exposure (20, 24, 28). In this study, all the BALB/c control group mice died and the time of death correlated with the load of bacterial infection or with the peak levels of the investigated cytokines. By contrast, the immunized mice, when infected with B. pseudomallei, did not show a rapid increase in the level of inflammatory cytokines, although the Th-1-related cytokines were significantly induced compared to the outcome for nonimmunized mice. Bacterial multiplication would seem to be restricted by the specific immune mechanism, and an up-regulation of the specific cytokines would appear to have provided protection against B. pseudomallei infection.
The IFN-γ-dominated Th-1 response facilitates the elimination of B. pseudomallei in the early infection stage (30). After an infection by the intravenous route, the immune responses in immunized BALB/c mice in this study have also been found to involve Th-1-type polarization. In particular, IFN-γ production in BALB/c mice immunized with pcDNA3/CpG-fliC was more pronounced than that in the mice immunized with pcDNA3/fliC. The results suggest that the CpG motifs inserted into the plasmid DNA can act as an immunostimulant to enhance the Th-1 immune response, leading to more protection against B. pseudomallei.
The immunostimulatory CpG motifs would seem to produce innate protection against melioidosis in BALB/c mice; however, this is nonspecific and is usually only maintained for approximately 15 days after the injection of the CpG oligonucleotide (40). We have demonstrated here that pcDNA3/CpG-fliC-vaccinated mice are still immunized against the bacteria beyond 56 days as measured by the increase in the IgG2a/IgG1 ratio, the up-regulation of IFN-γ in specific response to flagellin, and the 93.3% survival rate of the BALB/c mice after B. pseudomallei infection. The exogenous CpG motifs added to the fliC gene would contribute to an adjuvant-like response that enhances the flagellin-specific immunogenicity and provides protection against B. pseudomallei for a longer period.
Certainly, the effective protection confirmed by CpG-modified plasmid DNA immunization needs to be explored further. B. pseudomallei presents various abilities in virulence and diversity form, both genotypically and phenotypically (17, 29, 33). Different levels of protection in immunized BALB/c mice infected with different strains of B. pseudomallei may be induced. In addition, a wide range of factors, such as the plasmid vector, delivery route, nature of the antigen, and the mouse strain, may also affect the levels of the effector molecules produced by helper T cells (14, 18, 37). Nevertheless, we have shown that the BALB/c mice immunized with the CpG-modified plasmid encoding flagellin produce protection against challenge with single or mixed strains of B. pseudomallei, and this suggests that this is a potential strategy for the development of a DNA vaccine against B. pseudomallei. Further studies are required to improve the efficacy of the DNA immunization process and to provide a better understanding of the mechanisms of protection afforded by such immunization.
Acknowledgments
This project was supported by an NSC (ROC) grant (NSC93-2314-B-242-010 and NSC 94-2320-B-242-003) and by a VGH grant (VGHKS95-013).
Editor: J. B. Bliska
REFERENCES
- 1.Brett, P. J., D. C. Mah, and D. E. Woods. 1994. Isolation and characterization of Pseudomonas pseudomallei flagellin proteins. Infect. Immun. 62:1914-1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brett, P. J., and D. E. Woods. 1996. Structural and immunological characterization of Burkholderia pseudomallei O-polysaccharide-flagellin protein conjugates. Infect. Immun. 64:2824-2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brett, P. J., and D. E. Woods. 2000. Pathogenesis of and immunity to melioidosis. Acta Trop. 74:201-210. [DOI] [PubMed] [Google Scholar]
- 4.Chaowagul, W., N. J. White, D. A. Dance, Y. Wattanagoon, P. Naigowit, T. M. Davis, S. Looareesuwan, and N. Pitakwatchara. 1989. Melioidosis: a major cause of community-acquired septicemia in northeastern Thailand. J. Infect. Dis. 159:890-899. [DOI] [PubMed] [Google Scholar]
- 5.Chen, Y. L., S. N. Wang, W. J. Yang, Y. J. Chen, H. H. Lin, and D. Shiuan. 2003. Expression and immunogenicity of Mycoplasma hyopneumoniae heat shock protein antigen P42 by DNA vaccination. Infect. Immun. 71:1155-1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen, Y. S., S. C. Chen, C. M. Kao, and Y. L. Chen. 2003. Effects of soil pH, temperature and water content on the growth of Burkholderia pseudomallei. Folia Microbiol. (Prague) 48:253-256. [DOI] [PubMed] [Google Scholar]
- 7.Chen, Y. S., D. Shiuan, S. C. Chen, S. M. Chye, and Y. L. Chen. 2003. Recombinant truncated flagellin of Burkholderia pseudomallei as a molecular probe for diagnosis of melioidosis. Clin. Diagn. Lab. Immunol. 10:423-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen, Y. S., Y. S. Hsiao, H. H. Lin, C. M. Yen, S. C. Chen, and Y. L. Chen. 6 September 2005, posting date. Immunogenicity and anti-Burkholderia pseudomallei activity in BALB/c mice immunized with plasmid DNA encoding flagellin. Vaccine [Online.] doi: 10.1016/j.vaccine.2005.08.069. [DOI] [PubMed]
- 9.Chua, K. L., Y. Y. Chan, and Y. H. Gan. 2003. Flagella are virulence determinants of Burkholderia pseudomallei. Infect. Immun. 71:1622-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cornell, K. A., H. G. Bouwer, D. J. Hinrichs, and R. A. Barry. 1999. Genetic immunization of mice against Listeria monocytogenes using plasmid DNA encoding listeriolysin O. J. Immunol. 163:322-329. [PubMed] [Google Scholar]
- 11.Currie, B. J., D. A. Fisher, N. M. Anstey, and S. P. Jacups. 2000. Melioidosis: acute and chronic disease, relapse and re-activation. Trans. R. Soc. Trop. Med. Hyg. 94:301-304. [DOI] [PubMed] [Google Scholar]
- 12.DeShazer, D., P. J. Brett, R. Carlyon, and D. E. Woods. 1997. Mutagenesis of Burkholderia pseudomallei with Tn5-OT182: isolation of motility mutants and molecular characterization of the flagellin structural gene. J. Bacteriol. 179:2116-2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elkins, K. L., T. R. Rhinehart-Jones, S. Stibitz, J. S. Conover, and D. M. Klinman. 1999. Bacterial DNA containing CpG motifs stimulates lymphocyte-dependent protection of mice against lethal infection with intracellular bacteria. J. Immunol. 162:2291-2298. [PubMed] [Google Scholar]
- 14.Feltquate, D. M., S. Heaney, R. G. Webster, and H. L. Robinson. 1997. Different T helper cell types and antibody isotypes generated by saline and gene gun DNA immunization. J. Immunol. 158:2278-2284. [PubMed] [Google Scholar]
- 15.Ferraz, J. C., E. Stavropoulos, M. Yang, S. Coade, C. Espitia, D. B. Lowrie, M. J. Colston, and R. E. Tascon. 2004. A heterologous DNA priming-Mycobacterium bovis BCG boosting immunization strategy using mycobacterial Hsp70, Hsp65, and Apa antigens improves protection against tuberculosis in mice. Infect. Immun. 72:6945-6950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gurunathan, S., D. M. Klinman, and R. A. Seder. 2000. DNA vaccines: immunology, application, and optimization. Annu. Rev. Immunol. 18:927-974. [DOI] [PubMed] [Google Scholar]
- 17.Haase, A., A. Melder, H. Smith-Vaughan, D. Kemp, and B. Currie. 1995. RAPD analysis of isolates of Burkholderia pseudomallei from patients with recurrent melioidosis. Epidemiol. Infect. 115:115-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haddad, D., S. Liljeqvist, S. Stahl, P. Perlmann, K. Berzins, and N. Ahlborg. 1998. Differential induction of immunoglobulin G subclasses by immunization with DNA vectors containing or lacking a signal sequence. Immunol. Lett. 61:201-204. [DOI] [PubMed] [Google Scholar]
- 19.Hoppe, I., B. Brenneke, M. Rohde, A. Kreft, S. Haussler, A. Reganzerowski, and I. Steinmetz. 1999. Characterization of a murine model of melioidosis: comparison of different strains of mice. Infect. Immun. 67:2891-2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hotchkiss, R. S., and I. E. Karl. 2003. The pathophysiology and treatment of sepsis. N. Engl. J. Med. 348:138-150. [DOI] [PubMed] [Google Scholar]
- 21.Jones, S. M., J. F. Ellis, P. Russell, K. F. Griffin, and P. C. Oyston. 2002. Passive protection against Burkholderia pseudomallei infection in mice by monoclonal antibodies against capsular polysaccharide, lipopolysaccharide or proteins. J. Med. Microbiol. 51:1055-1062. [DOI] [PubMed] [Google Scholar]
- 22.Klinman, D. M., G. Yamshchikov, and Y. Ishigatsubo. 1997. Contribution of CpG motifs to the immunogenicity of DNA vaccines. J. Immunol. 158:3635-3639. [PubMed] [Google Scholar]
- 23.Krieg, A. M. 2002. CpG motifs in bacterial DNA and their immune effects. Annu. Rev. Immunol. 20:709-760. [DOI] [PubMed] [Google Scholar]
- 24.Krieg, A. M. 2003. CpG DNA: trigger of sepsis, mediator of protection, or both? Scand. J. Infect. Dis. 35:653-659. [DOI] [PubMed] [Google Scholar]
- 25.Lauw, F. N., A. J. Simpson, J. M. Prins, M. D. Smith, M. Kurimoto, S. J. van Deventer, P. Speelman, W. Chaowagul, N. J. White, and T. van der Poll. 1999. Elevated plasma concentrations of interferon (IFN)-gamma and the IFN-gamma-inducing cytokines interleukin (IL)-18, IL-12, and IL-15 in severe melioidosis. J. Infect. Dis. 180:1878-1885. [DOI] [PubMed] [Google Scholar]
- 26.Leelarasamee, A. 2004. Recent development in melioidosis. Curr. Opin. Infect. Dis. 17:131-136. [DOI] [PubMed] [Google Scholar]
- 27.Nelson, M., J. L. Prior, M. S. Lever, H. E. Jones, T. P. Atkins, and R. W. Titball. 2004. Evaluation of lipopolysaccharide and capsular polysaccharide as subunit vaccines against experimental melioidosis. J. Med. Microbiol. 53:1177-1182. [DOI] [PubMed] [Google Scholar]
- 28.Netea, M. G., J. W. van der Meer, M. van Deuren, and B. J. Kullberg. 2003. Proinflammatory cytokines and sepsis syndrome: not enough, or too much of a good thing? Trends Immunol. 24:254-258. [DOI] [PubMed] [Google Scholar]
- 29.Nigg, C., J. Ruch, E. Scott, and K. Noble. 1955. Enhancement of virulence of Malleomyces pseudomallei. J. Bacteriol. 71:530-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santanirand, P., V. S. Harley, D. A. Dance, B. S. Drasar, and G. J. Bancroft. 1999. Obligatory role of gamma interferon for host survival in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 67:3593-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sato, Y., M. Roman, H. Tighe, D. Lee, M. Corr, M. D. Nguyen, G. J. Silverman, M. Lotz, D. A. Carson, and E. Raz. 1996. Immunostimulatory DNA sequences necessary for effective intradermal gene immunization. Science 273:352-354. [DOI] [PubMed] [Google Scholar]
- 32.Suputtamongkol, Y., D. Kwiatkowski, D. A. Dance, W. Chaowagul, and N. J. White. 1992. Tumor necrosis factor in septicemic melioidosis. J. Infect. Dis. 165:561-564. [DOI] [PubMed] [Google Scholar]
- 33.Ulett, G. C., B. J. Currie, T. W. Clair, M. Mayo, N. Ketheesan, J. Labrooy, D. Gal, R. Norton, C. A. Smith, J. Barnes, J. Warner, and R. G. Hirst. 2001. Burkholderia pseudomallei virulence: definition, stability and association with clonality. Microbes Infect. 3:621-631. [DOI] [PubMed] [Google Scholar]
- 34.Ulett, G. C., N. Ketheesan, and R. G. Hirst. 1998. Macrophage-lymphocyte interactions mediate anti-Burkholderia pseudomallei activity. FEMS Immunol. Med. Microbiol. 21:283-286. [DOI] [PubMed] [Google Scholar]
- 35.Ulett, G. C., N. Ketheesan, and R. G. Hirst. 2000. Cytokine gene expression in innately susceptible BALB/c mice and relatively resistant C57BL/6 mice during infection with virulent Burkholderia pseudomallei. Infect. Immun. 68:2034-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Utaisincharoen, P., W. Kespichayawattana, N. Anuntagool, P. Chaisuriya, S. Pichyangkul, A. M. Krieg, and S. Sirisinha. 2003. CpG ODN enhances uptake of bacteria by mouse macrophages. Clin. Exp. Immunol. 132:70-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vercammen, M., T. Scorza, K. Huygen, J. De Braekeleer, R. Diet, D. Jacobs, E. Saman, and H. Verschueren. 2000. DNA vaccination with genes encoding Toxoplasma gondii antigens GRA1, GRA7, and ROP2 induces partially protective immunity against lethal challenge in mice. Infect. Immun. 68:38-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White, N. J. 2003. Melioidosis. Lancet 361:1715-1722. [DOI] [PubMed] [Google Scholar]
- 39.Wolff, J. A., J. J. Ludtke, G. Acsadi, P. Williams, and A. Jani. 1992. Long-term persistence of plasmid DNA and foreign gene expression in mouse muscle. Hum. Mol. Genet. 1:363-369. [DOI] [PubMed] [Google Scholar]
- 40.Wongratanacheewin, S., W. Kespichayawattana, P. Intachote, S. Pichyangkul, R. W. Sermswan, A. M. Krieg, and S. Sirisinha. 2004. Immunostimulatory CpG oligodeoxynucleotide confers protection in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 72:4494-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]