Abstract
Treatment with an oligodeoxynucleotide (ODN) containing CPG motifs (CpG ODN 7909) was found to protect BALB/c mice from lung infection or death after aerosol challenge with Burkholderia mallei. Protection was associated with enhanced levels of gamma interferon (IFN-γ)-inducible protein 10, interleukin-12 (IL-12), IFN-γ, and IL-6. Preexposure therapy with CpG ODNs may protect victims of a biological attack from glanders.
Burkholderia mallei, the causative agent of glanders, naturally infects equines, but it can also cause serious disease in a variety of hosts, including humans, where the disease, although rare, tends to be severe, debilitating, and often fatal (13, 15). Although B. mallei is a category B biothreat agent, there presently are no reliable means to protect humans against glanders acquired from accidental or deliberate exposure.
Stimulating Toll-like receptor 9 (TLR9) expressed on human plasmacytoid dendritic cells and B cells (5) with an oligodeoxynucleotide (ODN) containing CPG motifs (CpG ODN) results in the systemic expression of Th1-like cytokines and chemokines and in the activation of NK cells, dendritic cells, macrophages, and some subpopulations of lymphocytes in both mice and humans (8, 22). The stimulation of innate immunity with CpG ODNs has been shown to protect rodents against subsequent infection with diverse intracellular infections, including tularemia (3), listeriosis (6, 9), and those caused by Plasmodium yoelii (4) and Leishmania challenge (19). In studies using Burkholderia pseudomallei, a microorganism related to B. mallei, a CpG ODN was shown to confer protection to mice challenged intraperitoneally (i.p.) (21).
Different classes of CpG ODNs with distinct immune properties have been described previously (7, 20). A-class CpG ODNs, such as CpG 2216 (5′ GGGGGACGATCGTCGGGGGG), have poly(G) sequences on the 5′ and/or 3′ ends, which are phosphorothioate modified for nuclease resistance and induce the production of high levels of alpha interferon (IFN-α) in plasmacytoid dendritic cells and marked NK and γδ T-cell activation with relatively little B-cell stimulation (11). In contrast, B-class CpG ODNs, such as CPG 7909 (5′ TCGTCGTTTTGTCGTTTTGTCGTT), have a complete phosphorothioate backbone and induce the production of modest levels of IFN-α, with much weaker NK cell activation, but with profound B-cell activation (10). Because these ODN classes have such disparate immune effects, it is important to determine which of the immune profiles may be associated with protection from infection.
In this study, we evaluated CpG ODN protective efficacy in terms of the ability to (i) prevent the colonization of the lungs, spleens, and livers and to (ii) prevent lethality in treated mice challenged by aerosol with the virulent China 7 strain of B. mallei (ATCC 23344). Significant differences in organ bacterial counts were determined by analysis of variance with a post hoc Dunnett's test for comparison with a control group. Significant differences in survival after challenge were determined using Fisher exact tests with a stepdown Bonferroni adjustment for multiple comparisons and Kaplan-Meier survival analysis and log rank tests with stepdown Bonferroni adjustment for multiple comparisons. Significant differences in the mean time to death were determined using t tests with stepdown Bonferroni adjustment for multiple comparisons (14a).
Effect of CpG ODNs on bacterial load.
Six- to 8-week-old female BALB/c mice (5 mice per group) (Charles River Laboratories, Wilmington, MA) were given 100 μg (5 mg/kg) of CPG 7909 (B class) or CpG 2216 (A class) i.p. 48 h before aerosol challenge (0.2 times a 50% lethal dose [LD50] = 200 CFU) (12, 16) with virulent B. mallei grown overnight in tryptone broth (Difco) containing 4% glycerol. The CpG ODNs were provided by the Coley Pharmaceutical Group (Wellesley, MA), contained undetectable levels of endotoxin, and were administered in Hanks' balanced salt solution (HBSS). Five, 11, and 18 days after challenge, mice (5 per group) were euthanized for determination of bacterial counts in the spleens, livers, and lungs. Organs were removed from euthanized (with CO2) mice and were weighed and dissociated in 5 ml of HBSS. Appropriate dilutions were plated, and the number of B. mallei CFU per organ was determined. Mice were evaluated individually.
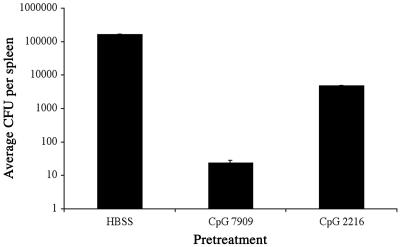
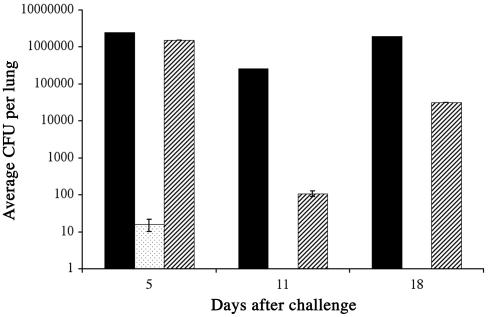
CPG 7909 pretreatment significantly decreased (P < 0.01) the numbers of B. mallei CFU in the spleen 5 days after challenge compared to mice given HBSS (Fig. 1). Bacterial numbers in spleens of mice treated with CpG 2216 were not significantly different from those of controls. Furthermore, CPG 7909 dramatically restricted or reduced to undetectable levels the growth of B. mallei in lungs of mice exposed to a low aerosol dose of B. mallei 5 (P < 0.0001), 11 (P < 0.001), or 18 days (P < 0.001) previously, compared to mice given HBSS or CpG 2216 (Fig. 2). Lungs from mice given saline or CpG 2216 were heavily infected. Livers of animals in all groups were not consistently infected (data not shown). Spleen weights, a measure of the level of B. mallei load and inflammatory response, did not increase between 5 and 18 days after challenge in mice treated with CPG 7909, whereas spleen weights of mice given HBSS or CpG 2216 increased significantly (data not shown). While spleens from mice pretreated with CPG 7909 were clearly protected 5 days after aerosol challenge, the effect on spleen bacterial counts 11 and 18 days after challenge was less clear. At these time points, all CpG treatment groups contained a mixture of infected and uninfected animals. On day 11, 2 of 5 mice given CPG 7909 had infected spleens (9 × 103 and 2 × 108 CFU per spleen) and 3 of 5 mice given CpG 2216 had residual infection (4 × 105, 2 × 106, and 1 × 106 CFU), while on day 18, 2 of 5 mice given CPG 7909 had infected spleens (5 × 106 and 1 × 107 CFU) and 2 of 3 mice (remaining survivors) receiving CpG 2216 had residual infection (700 and 850 CFU). Therefore, protection of the spleen afforded by CpG ODNs at these later time points was not evident on the basis of infection.
FIG. 1.
CPG 7909 pretreatment can reduce the numbers of microorganisms in the spleens of infected mice. Mice were injected i.p. with HBSS, CPG 7909, or CpG 2216 48 h before aerosol challenge with B. mallei. Five days after challenge, the numbers (geometric mean) of bacteria in the spleens of infected mice were determined. Bars indicate ±1 standard error.
FIG. 2.
CPG 7909 pretreatment can eliminate or reduce the numbers of microorganisms in the lungs of infected mice. Mice were injected i.p. with HBSS (▪), CPG 7909 (░⃞), or CpG 2216 (▨) 48 h before aerosol challenge with B. mallei. Five, 11, and 18 days after challenge, the numbers (geometric mean) of bacteria in the lungs of infected animals were determined. Bars indicate ±1 standard error.
Effect of CpG ODNs on survival.
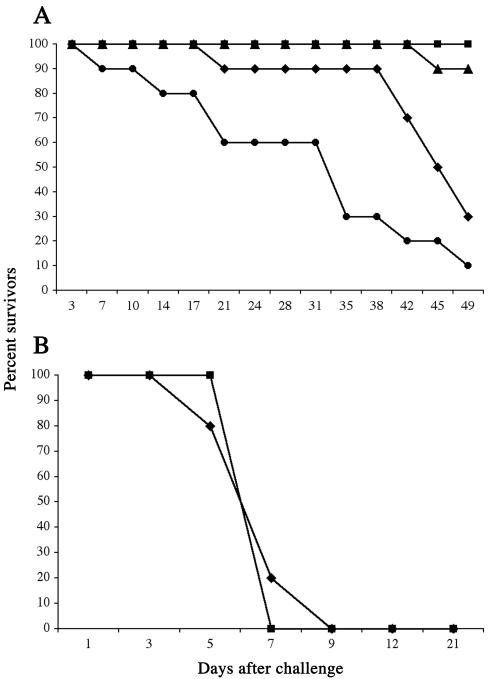
To determine whether CpG ODN could prevent death of challenged animals and to evaluate the effect of the CpG ODN administration schedule on survival, female BALB/c mice (10 per group) were injected i.p. with 100 μg (5 mg/kg) of CPG 7909 48 h before challenge, the day of challenge, or 24 h after aerosol challenge (2 LD50) with B. mallei. We found that CPG 7909 administered 2 days before or on the day of challenge was able to protect mice against a lethal aerosol infection of B. mallei (Fig. 3A). Seven weeks after challenge, 100% of mice pretreated with CPG 7909 survived, whereas 70% of control mice died (P < 0.01). When CPG 7909 was given the day of challenge, only 10% of treated mice died (P < 0.05). However, when CPG 7909 was given 1 day after challenge, 90% of the mice died (P > 0.05). The mean times to death were 41 days for the mice given HBSS, 43 days (representing one mouse) for the mice given CPG 7909 the day of challenge, and 27 days for the mice given CPG 7909 1 day after challenge. The times to death of these experimental groups were not significantly different from that of controls (P > 0.05). CpG 2216 given 48 h before aerosol challenge (2 × LD50) was not protective (Fig. 3B) (P > 0.05).
FIG. 3.
(A) CPG 7909 given 48 h before or on the day of challenge can protect mice from lethality due to B. mallei challenge. Mice were injected i.p. with HBSS (♦) or CPG 7909 48 h before challenge (▪), the day of challenge (▴), or 24 h (•) after aerosol challenge with B. mallei. (B) CpG 2216 pretreatment does not protect mice from lethality due to B. mallei challenge. Mice were injected i.p. with HBSS (♦) or CpG 2216 (▪) 48 h before challenge with B. mallei.
Effect of CpG ODNs on cytokine profiles.
In an effort to determine correlates of protection and discover possible mechanisms of immunity, we evaluated chemokines/cytokines in plasma and bronchial alveolar lavage (BAL) fluid that are known to be important in protective immunity against intracellular pathogens. Chemokines/cytokines that are important in generating Th1 immunity include IFN-γ-inducible protein 10 (IP-10), a chemokine with chemoattractant properties for CD4-positive T cells; IFN-γ, a cytokine that activates macrophages; interleukin-12 (IL-12), a cytokine that induces IFN-γ production and stimulates the proliferation of activated T cells and NK cells; and IL-6, a cytokine important in inflammation.
Three, 6, 24, and 48 h after CPG 7909, CpG 2216, or control ODN 2137 injection, plasma and BAL of BALB/c mice (5 mice per group) were examined for levels of IP-10, IL-12(p40), IL-6, and IFN-γ by using commercially available antigen capture enzyme-linked immunosorbent assay kits (IP-10 from R&D Systems, Minneapolis, MN; IL-12, IL-6, and IFN-γ from DB Biosciences, Mississauga, Ontario, Canada). Each sample was tested in duplicate. ODN 2137 had the same nucleotide sequence as CPG 7909, except the CpGs were inverted to GpCs. Chemokine/cytokine levels were determined for each mouse, mean levels were determined for treatment groups, and significant differences in chemokine/cytokine levels in plasma and BAL were determined using t tests (Excel; Microsoft Corp., Redmond, WA).
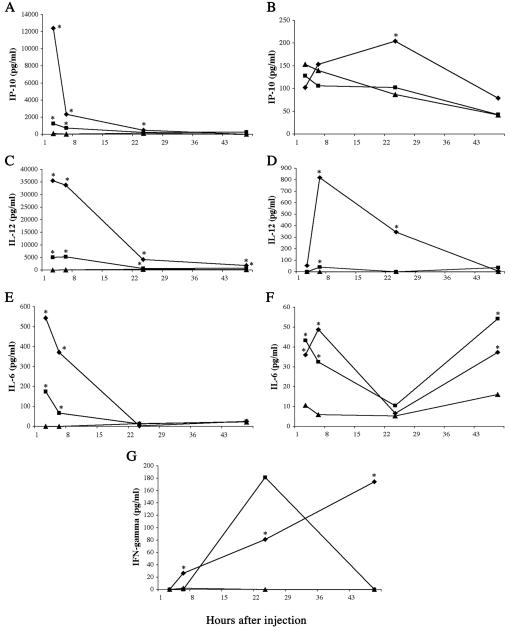
Mice injected with CPG 7909 had significantly higher levels of IP-10 (P < 0.01) in the plasma than those stimulated by ODN 2137 when measured 3, 6, and 24 h after injection (Fig. 4A). The levels of IP-10 induced by CPG 7909 injection were (12-fold) higher than IP-10 levels induced by CpG 2216 3 h after injection. When the BAL fluid was examined for IP-10, CPG 7909 stimulated significantly higher levels (P < 0.01) than ODN 2137 24 h after injection (Fig. 4B).
FIG. 4.
CpG ODN pretreatment can increase the levels of IP-10 in plasma (A) and BAL fluid (B), IL-12 in plasma (C) and BAL fluid (D), IL-6 in plasma (E) and BAL fluid (F), and IFN-γ in plasma (G). Mice were injected i.p. with CPG 7909 (♦), CpG 2216 (▪), or ODN 2137 (▴) 3, 6, 24, or 48 h before determination of chemokine/cytokine concentration. *, statistical significance of at least P < 0.05 between chemokine/cytokine levels stimulated by CpG ODN and levels stimulated by control ODN 2137. Actual levels of statistical significance are found in the text.
Plasma levels of IL-12 stimulated by CPG 7909 and CpG 2216 were significantly higher than control levels at all time points measured (P < 0.05) (Fig. 4C). However, 3 and 6 h after injection, over six times the concentration of IL-12 was found in the plasma of mice given CPG 7909 compared to that in mice given CpG 2216. IL-12 levels found in the BAL fluid of CPG 7909-stimulated mice peaked 6 h after injection and were significantly higher than control levels 6 and 24 h after injection (P < 0.05) (Fig. 4D). The level of IL-12 stimulated by CpG 2216 injection was significantly elevated compared to levels in controls 6 h after injection (P < 0.05), although still eightfold less than IL-12 levels stimulated by CPG 7909.
IL-6 levels found in the plasma 3 and 6 h after injection of CPG 7909 or CpG 2216 were significantly elevated compared to levels in controls (P < 0.05) (Fig. 4E). However, CPG 7909 stimulated five times the concentration of IL-6 that CpG 2216 did. IL-6 found in the BAL fluid after injection of either CpG ODN was significantly higher than control levels 3, 6, and 48 h after injection (P < 0.05) (Fig. 4F).
Plasma levels of IFN-γ stimulated by CPG 7909 were significantly higher (P < 0.05) than levels stimulated by ODN 2137 6, 24, and 48 h after injection. CpG 2216 did not stimulate levels of IFN-γ that were significantly higher than those of controls (P > 0.05) (Fig. 4G).
To our knowledge, this paper represents the first published study on the ability of CpG to protect mice against a B. mallei infection. The CPG 7909 used in the present study is optimized for stimulation of human TLR9 (but is also active in the mouse). Furthermore, CPG 7909 (now known as PF 3512767 when used for human cancer therapy) has been administered to more than 700 humans in various clinical trials, where it has shown an acceptable safety profile and has induced a Th1-like pattern of cytokine and chemokine expression (8). In a recent study, CpG ODN 1826, which is optimized for stimulation of the mouse TLR9 and is virtually inactive for stimulation of human cells, protected mice from a lethal i.p. infection with a related microorganism, B. pseudomallei (21). In that study, CpG-treated mice exhibited elevated serum IL-12 and IFN-γ levels and decreased bacteremia. Spleens, livers, and lungs of treated, challenged mice were free of bacteria 4 days after challenge. The administration of CpG was not protective if administered after or at the time of challenge. Protection stimulated by injecting CpG ODN 1826 was accompanied by an early rise in IL-12, IFN-γ, nitric oxide synthetase, and nitric oxide. CpG 1826 also stimulated increased phagocytosis of B. pseudomallei by RAW 264.7 mouse macrophages (17, 18).
We showed that CPG 7909 pretreatment dramatically improved survival, completely protected the lungs of infected mice from infection, and also partially protected the spleens. However, we do not know the mechanism whereby systemic treatment with CPG 7909 protects mice from an aerosol challenge of virulent B. mallei. The stimulation of Th1 cytokines by activated dendritic cells expressing TLR9 (2) is a likely protective mechanism in this experimental system. Activation results in the induction of IL-12 and IFN-α/β, which in turn stimulate the NK cell production of IFN-γ. We noted that IL-12 induction was measurable 3 h after injection of CPG 7909 (Fig. 4C), and IFN-γ production was increasing 48 h after injection (Fig. 4G). The early induction of IL-12, detected in the lung BAL fluid and plasma, followed by the gradual rise in IFN-γ could stimulate effector cells that would act to protect the host from lethal challenge. Although the protective efficacy of IFN-γ against glanders has not been established, IFN-γ has been shown to be a protective mechanism in a murine model of melioidosis (14). We also measured an early rise in IP-10 (Fig. 4A), whose role in the protective response is to attract lymphocytes to the site of infection, thereby contributing to the development of Th1-mediated immunity. Similarly, the early induction of IL-6 (Fig. 4E) could result in the early release of inflammatory mediators that can increase the rate of bacterial phagocytosis and subsequent activation of T and NK cells. The operative mechanism in providing resistance to B. mallei infection is relatively short-lived, as CpG ODN pretreatment greater than 2 weeks before challenge was not protective (data not shown).
While the mechanism of lung protection induced by CPG 7909 in mice challenged with virulent B. mallei remains unknown, the demonstration that this product can effectively stimulate chemokines/cytokines associated with Th1-type immunity suggests that it may be effective for protecting the lungs of at-risk persons from an imminent biological attack with this biothreat agent or others. Rapidly acting drugs that activate innate immune cells, like CpG ODNs, might induce a broad-spectrum array of antimicrobial immune defenses that potentially could protect victims until the exact nature of the assault could be determined and more-specific therapies administered. The activation of innate immune responses before infection might control bacterial proliferation and viral replication before the host developed fatal infection.
Animal care and use.
The facility where this research was conducted is fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care International. Challenge studies were conducted at the United States Army Medical Research Institute of Infectious Diseases, Fort Detrick, MD, in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals and adhere to principles stated in the Guide for the Care and Use of Laboratory Animals (10a). Other animal studies were conducted in the Animal Care Facility of Coley Pharmaceutical Group, Ottawa, Canada, which is fully accredited by the Canadian Council on Animal Care. All animal experiments were subject to approval by the Coley Canada Animal Care Committee, under the guidelines and requirements of the Canadian Council on Animal Care.
Editor: J. T. Barbieri
REFERENCES
- 1.Reference deleted.
- 2.Bauer, S., C. J. Kirschning, H. Hacker, V. Redecke, S. Hausmann, S. Akira, H. Wagner, and G. B. Lipford. 2001. Human TLR9 confers responsiveness to bacterial DNA via species-specific CpG motif recognition. Proc. Natl. Acad. Sci. USA 98:9237-9242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elkins, K. L., T. R. Rhinehart-Jones, S. Stibitz, J. S. Conover, and D. M. Klinman. 1999. Bacterial DNA containing CpG motifs stimulates lymphocyte-dependent protection of mice against lethal infection with intracellular bacteria. J. Immunol. 162:2291-2298. [PubMed] [Google Scholar]
- 4.Gramzinski, R. A., D. L. Doolan, M. Sedegah, H. L. Davis, A. M. Krieg, and S. L. Hoffman. 2001. Interleukin-12- and gamma interferon-dependent protection against malaria conferred by CpG oligodeoxynucleotide in mice. Infect. Immun. 69:1643-1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hornung, V., S. Rothenfusser, S. Britsch, A. Krug, B. Jahrsdorfer, T. Giese, S. Endres, and G. Hartmann. 2002. Quantitative expression of toll-like receptor 1-10 mRNA in cellular subsets of human peripheral blood mononuclear cells and sensitivity to CpG oligodeoxynucleotides. J. Immunol. 168:4531-4537. [DOI] [PubMed] [Google Scholar]
- 6.Klinman, D. M., J. Conover, and C. Coban. 1999. Repeated administration of synthetic oligodeoxynucleotides expressing CpG motifs provides long-term protection against bacterial infection. Infect. Immun. 67:5658-5663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krieg, A. M. 2002. CpG motifs in bacterial DNA and their immune effects. Annu. Rev. Immunol. 20:709-760. [DOI] [PubMed] [Google Scholar]
- 8.Krieg, A. M., S. M. Efler, M. Wittpoth, M. J. Al Adhami, and H. L. Davis. 2004. Induction of systemic TH1-like innate immunity in normal volunteers following subcutaneous but not intravenous administration of CPG 7909, a synthetic B-class CpG oligodeoxynucleotide TLR9 agonist. J. Immunother. 27:460-471. [DOI] [PubMed] [Google Scholar]
- 9.Krieg, A. M., L. Love-Homan, A. K. Yi, and J. T. Harty. 1998. CpG DNA induces sustained IL-12 expression in vivo and resistance to Listeria monocytogenes challenge. J. Immunol. 161:2428-2434. [PubMed] [Google Scholar]
- 10.Krug, A., S. Rothenfusser, V. Hornung, B. Jahrsdorfer, S. Blackwell, Z. K. Ballas, S. Endres, A. M. Krieg, and G. Hartmann. 2001. Identification of CpG oligonucleotide sequences with high induction of IFN-alpha/beta in plasmacytoid dendritic cells. Eur. J. Immunol. 31:2154-2163. [DOI] [PubMed] [Google Scholar]
- 10a.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academies Press, Washington, D.C.
- 11.Rothenfusser, S., V. Hornung, A. Krug, A. Towarowski, A. M. Krieg, S. Endres, and G. Hartmann. 2001. Distinct CpG oligonucleotide sequences activate human gamma delta T cells via interferon-alpha/-beta. Eur. J. Immunol. 31:3525-3534. [DOI] [PubMed] [Google Scholar]
- 12.Roy, C. J., M. Hale, J. M. Hartings, L. Pitt, and S. Duniho. 2003. Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhal. Toxicol. 15:619-638. [DOI] [PubMed] [Google Scholar]
- 13.Sanford, J. P. 1990. Pseudomonas species (including melioidosis and glanders), p. 1692-1696. In G. L. Mandell, R. G. Douglas, and J. E. Bennett (ed.), Principles and practice of infectious diseases, 3rd ed. Churchill Livingstone, New York, N.Y.
- 14.Santanirand, P., V. S. Harley, D. A. Dance, B. S. Drasar, and G. J. Bancroft. 1999. Obligatory role of gamma interferon for host survival in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 67:3593-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14a.SAS Institute. 2004. SAS 9.1. SAS Institute, Cary, N.C.
- 15.Smith, G. R., and C. S. F. Easman. 1990. Bacterial diseases, p. 392-397. In M. T. Parke and L. H. Collie (ed.), Principles of bacteriology, virology and immunity. B. C. Decker, Philadelphia, Pa.
- 16.USAMRIID. Standard operating procedure number TX-02-01-00. U.S. Army Medical Research Institute of Infectious Diseases, Fort Detrick, Md.
- 17.Utaisincharoen, P., N. Anuntagool, P. Chaisuriya, S. Pichyangkul, and S. Sirisinha. 2002. CpG ODN activates NO and iNOS production in mouse macrophage cell line (RAW 264.7). Clin. Exp. Immunol. 128:467-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Utaisincharoen, P., W. Kespichayawattana, N. Anuntagool, P. Chaisuriya, S. Pichyangkul, A. M. Krieg, and S. Sirisinha. 2003. CpG ODN enhances uptake of bacteria by mouse macrophages. Clin. Exp. Immunol. 132:70-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verthelyi, D., M. Gursel, R. T. Kenney, J. D. Lifson, S. Liu, J. Mican, and D. M. Klinman. 2003. CpG oligodeoxynucleotides protect normal and SIV-infected macaques from Leishmania infection. J. Immunol. 170:4717-4723. [DOI] [PubMed] [Google Scholar]
- 20.Vollmer, J., R. Weeratna, P. Payette, M. Jurk, C. Schetter, M. Laucht, T. Wader, S. Tluk, M. Liu, H. L. Davis, and A. M. Krieg. 2004. Characterization of three CpG oligodeoxynucleotide classes with distinct immunostimulatory activities. Eur. J. Immunol. 34:251-262. [DOI] [PubMed] [Google Scholar]
- 21.Wongratanacheewin, S., W. Kespichayawattana, P. Intachote, S. Pichyangkul, R. W. Sermswan, A. M. Krieg, and S. Sirisinha. 2004. Immunostimulatory CpG oligodeoxynucleotide confers protection in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 72:4494-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao, Q., J. Temsamani, R. Z. Zhou, and S. Agrawal. 1997. Pattern and kinetics of cytokine production following administration of phosphorothioate oligonucleotides in mice. Antisense Nucleic Acid Drug Dev. 7:495-502. [DOI] [PubMed] [Google Scholar]