Abstract
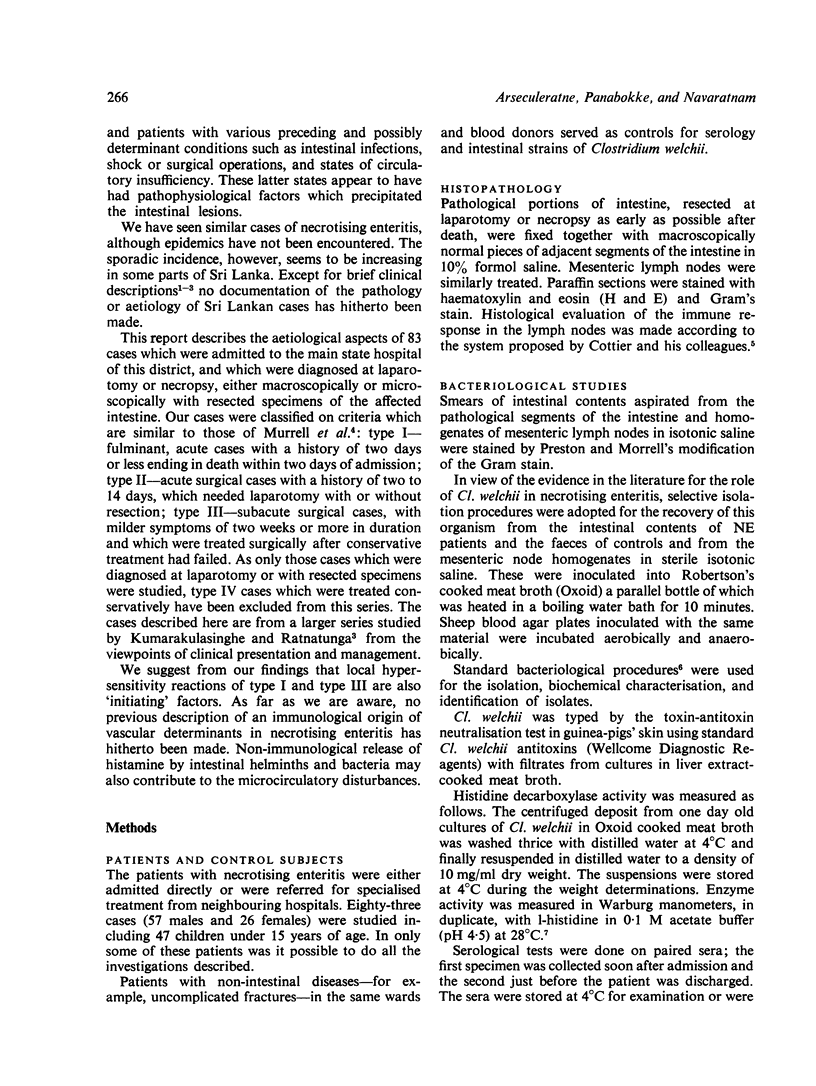
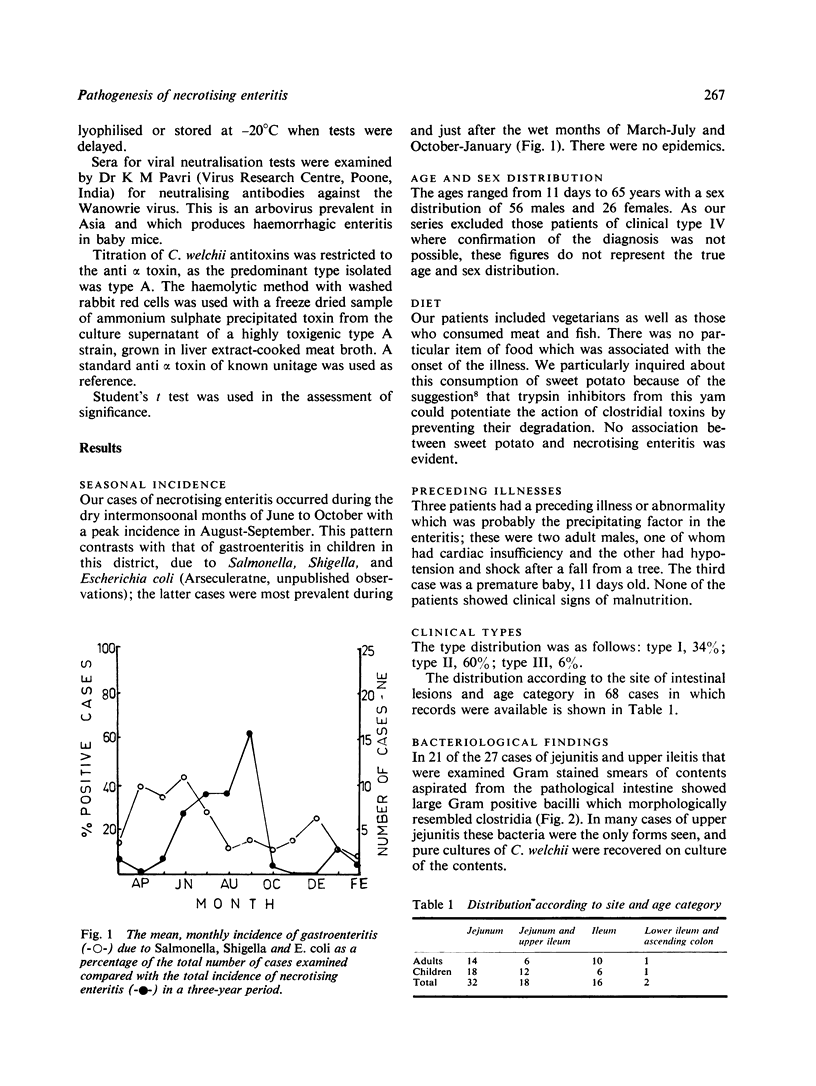
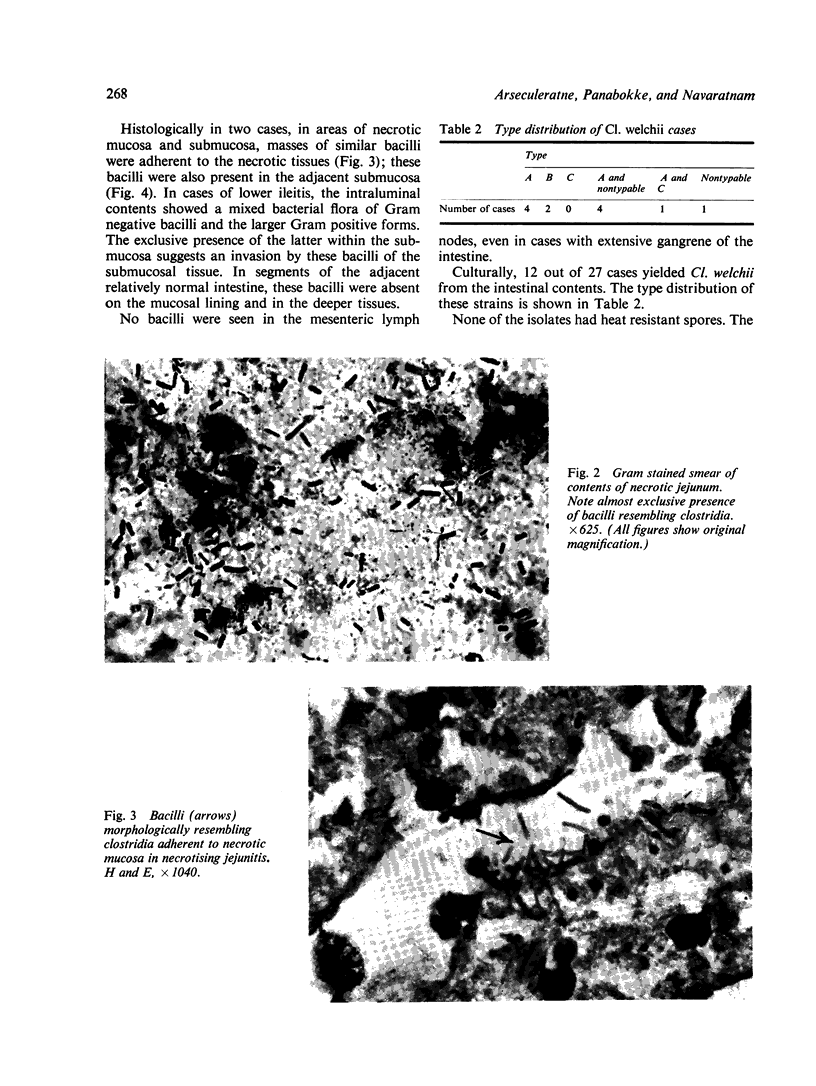
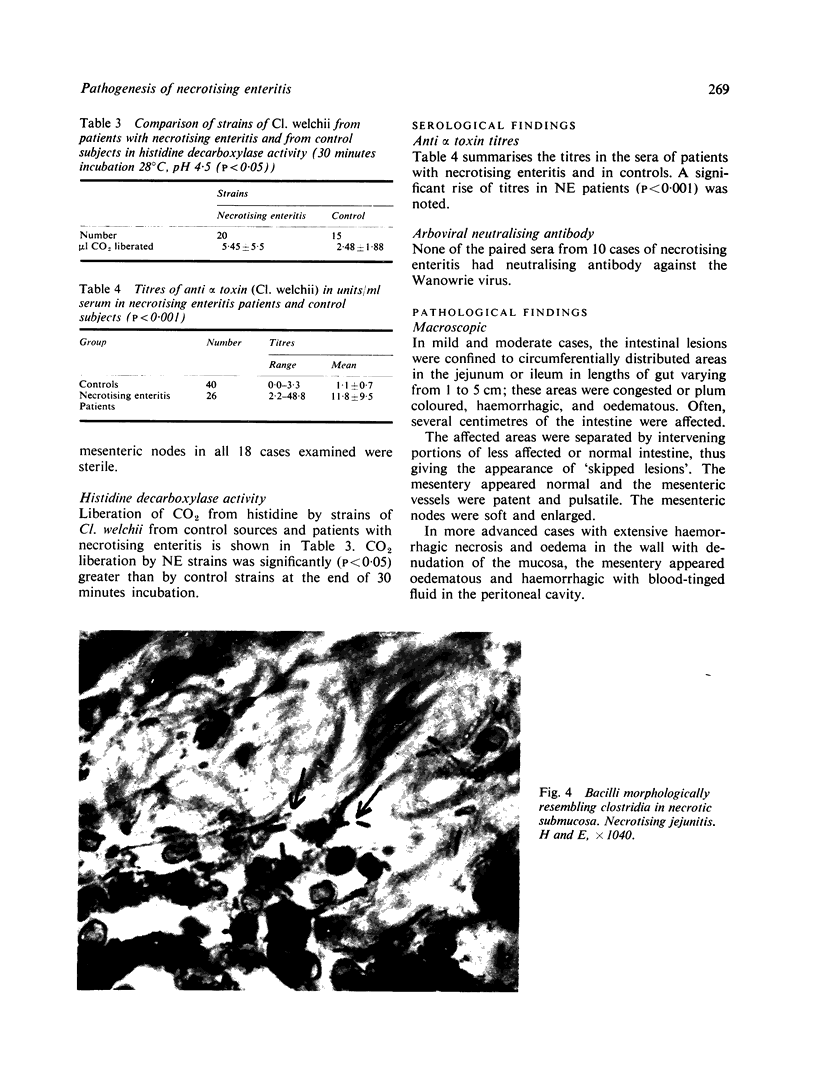
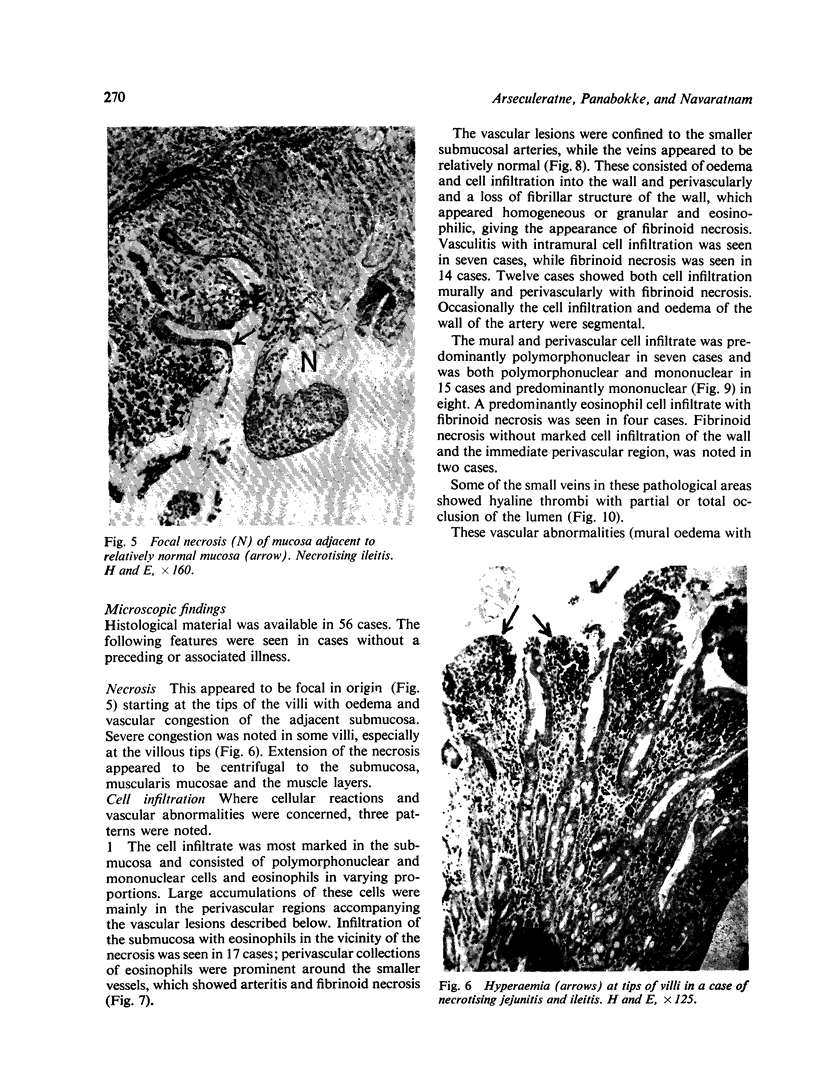
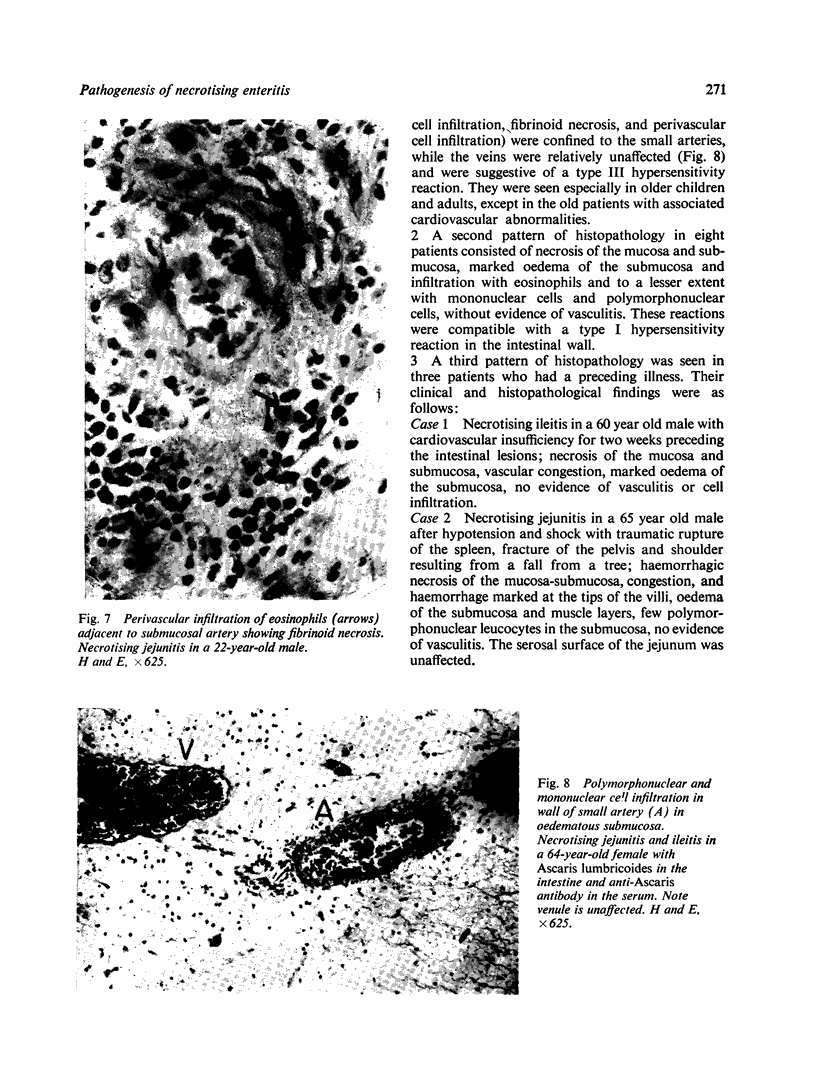
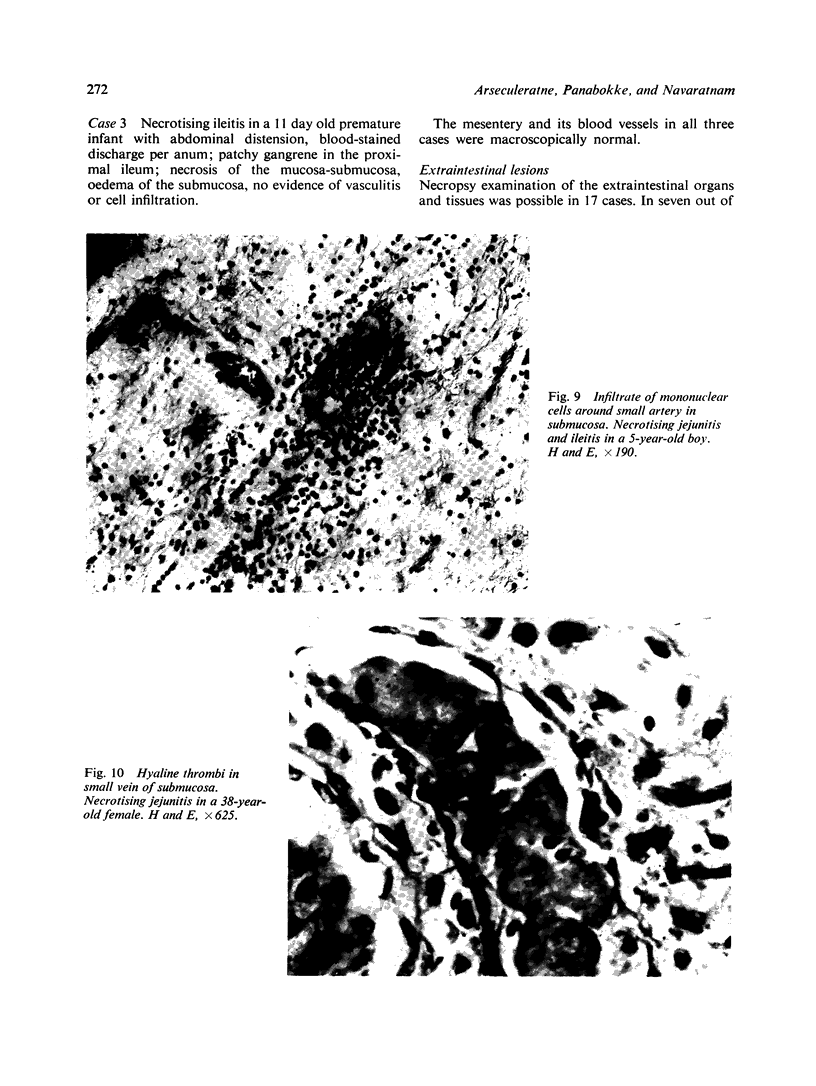
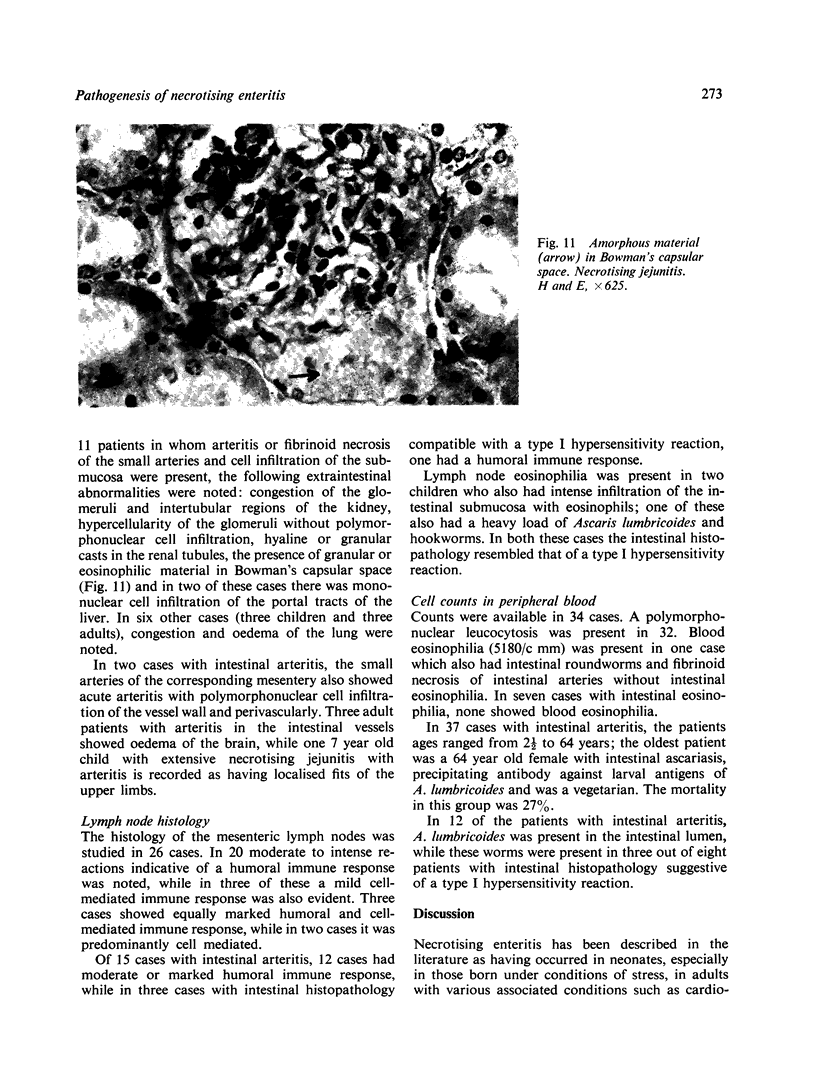
The aetiological aspects of 83 sporadic cases of necrotising enteritis (NE) have been studied. Of 56 cases in which histology of the intestine was possible, eight showed appearances (oedema and local eosinophilia) suggestive of a type I hypersensitivity reaction, while in 37 the appearances were suggestive of a type III reaction. We suggest that these reactions, which were more common in children and young adults, were initiating factors in the intestinal necrosis. The type III reactions (submucosal arteritis, fibrinoid necrosis of arteriolar walls, intramural and perivascular infiltration with polymorphonuclear, mononuclear, and eosinophil cells, and submucous oedema) were in seven cases accompanied by extraintestinal lesions (hypercellularity of glomeruli, amorphous material in the Bowman's capsular space, tubular casts, mononuclear cell infiltration into the hepatic portal tracts, congestion and oedema of the lung) which were compatible with systemic immune complex disease. The mesenteric lymph nodes in 12 out of 15 cases with intestinal arteritis showed appearances indicative of a humoral immune response. We suggest that NE is a two-stage process. In stage 1, a necrotic focus is established in the intestinal mucosa-submucosa by 'initiating' factors of vascular (functional or organic) or microbial (exotoxic, endotoxic, or Shwartzman) origin. Functional circulatory insufficiency in the intestine is of particular relevance to necrotising enteritis in neonates and in adults with traumatic shock or cardiac insufficiency. The jejunal and--to a lesser extent--the ileal microcirculation appear to be particularly vulnerable to microcirculatory insufficiency. Ninety-seven per cent of our cases were of NE of the small intestine of which 76% involved the jejunum alone or as a part of a jejunoileitis. These 'initiating' factors act either singly or synergistically with 'promoting' factors (changes in the volume, composition, or pH of the diet, intestinal stasis, or bacterial factors) in the establishment of necrotic foci in the intestine. Stage 2 results from the colonisation of the necrotic foci by intestinal clostridia, the toxigenic capacity of which will determine the progress of the intestinal lesion. Clinically established NE is essentially gas gangrene of the intestinal wall. Our bacteriological findings (microscopic, cultural, and serological) support a pathogenetic role of Cl. welchii in the established stages of necrotising enteritis. Strains of Cl. welchii from NE cases had significantly higher histidine decarboxylase activity than strains from control sources; it is possible that the resultant histamine production could act as a promoting factor in stage 1. Neutralising antibody against the Wanowrie virus, an Asian arbovirus which produces haemorrhagic enteritis in mice, was absent in the paired sera from 10 cases examined.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- COCHRANE C. G., WEIGLE W. O. The cutaneous reaction to soluble antigen-antibody complexes; a comparison with the Arthus phenomenon. J Exp Med. 1958 Nov 1;108(5):591–604. doi: 10.1084/jem.108.5.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottier H., Turk J., Sobin L. A proposal for a standardized system of reporting human lymph node morphology in relation to immunological function. J Clin Pathol. 1973 May;26(5):317–331. doi: 10.1136/jcp.26.5.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EGGLESTON L. V. Effects of cations on amino acid decarboxylases. Biochem J. 1958 Mar;68(3):557–560. doi: 10.1042/bj0680557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FIELD H. I., GOODWIN R. F. The experimental reproduction of enterotoxaemia in piglets. J Hyg (Lond) 1959 Mar;57(1):81–91. doi: 10.1017/s0022172400019914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GELL P. G., HINDE I. T. Observations on the histology of the Arthus reaction and its relation to other known types of skin hypersensitivity. Int Arch Allergy Appl Immunol. 1954;5(1):23–46. doi: 10.1159/000228084. [DOI] [PubMed] [Google Scholar]
- GERMUTH F. G., Jr, POLLACK A. D. The production of lesions of serum sickness in normal animals by the passive transfer of antibody in the presence of antigen. Bull Johns Hopkins Hosp. 1958 May;102(5):245–262. [PubMed] [Google Scholar]
- HERMANN R. E. PERFORATION OF THE COLON FROM NECROTIZING COLITIS IN THE NEWBORN: REPORT OF A SURVIVAL AND A NEW ETIOLOGIC CONCEPT. Surgery. 1965 Aug;58:436–441. [PubMed] [Google Scholar]
- Hauschild A. H., Niilo L., Dorward W. J. Clostridium perfringens type A infection of ligated intestinal loops in lambs. Appl Microbiol. 1968 Aug;16(8):1235–1239. doi: 10.1128/am.16.8.1235-1239.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikura H., Hayasaka H., Kikuchi Y. Acute regional ileitis at Iwanai in Hokkaido--with special reference to intestinal Anisakiasis. Sapporo Igaku Zasshi. 1967 Oct-Nov;32(4):183–196. [PubMed] [Google Scholar]
- Johansson S. G., Mellbin T., Vahlquist B. Immunoglobulin levels in Ethiopian preschool children with special reference to high concentrations of immunoglobulin E (IgND). Lancet. 1968 May 25;1(7552):1118–1121. doi: 10.1016/s0140-6736(68)90187-6. [DOI] [PubMed] [Google Scholar]
- KILLINGBACK M. J., WILLIAMS K. L. Necrotizing colitis. Br J Surg. 1961 Sep;49:175–185. doi: 10.1002/bjs.18004921413. [DOI] [PubMed] [Google Scholar]
- KOSLOWSKI L., SCHNEIDER H. H., HEISE C. Experimentelle Untersuchungen über die Histaminbildung des Bac. Enterotoxicus im vergleich mit anderen pathogenen anaeroblern. Klin Wochenschr. 1951 Jan 1;29(1-2):29–30. doi: 10.1007/BF01480883. [DOI] [PubMed] [Google Scholar]
- LITT M. EOSINOPHILS AND ANTIGEN-ANTIBODY REACTIONS. Ann N Y Acad Sci. 1964 Aug 27;116:964–985. doi: 10.1111/j.1749-6632.1964.tb52562.x. [DOI] [PubMed] [Google Scholar]
- Lawrence G., Walker P. D. Pathogenesis of enteritis necroticans in Papula New Guinea. Lancet. 1976 Jan 17;1(7951):125–126. doi: 10.1016/s0140-6736(76)93160-3. [DOI] [PubMed] [Google Scholar]
- Litt M. Studies in experimental eosinophilia. IX. Inhibition by puromycin of the eosinophil response which hemocyanin elicits in guinea pig lymph nodes. J Immunol. 1972 Aug;109(2):222–226. [PubMed] [Google Scholar]
- Lloyd J. R. The etiology of gastrointestinal perforations in the newborn. J Pediatr Surg. 1969 Feb;4(1):77–84. doi: 10.1016/0022-3468(69)90186-9. [DOI] [PubMed] [Google Scholar]
- MIZRAHI A., BARLOW O., BERDON W., BLANC W. A., SILVERMAN W. A. NECROTIZING ENTEROCOLITIS IN PREMATURE INFANTS. J Pediatr. 1965 Apr;66:697–705. doi: 10.1016/s0022-3476(65)80003-8. [DOI] [PubMed] [Google Scholar]
- Murrell T. G., Roth L., Egerton J., Samels J., Walker P. D. Pig-bel: enteritis necroticans. A study in diagnosis and management. Lancet. 1966 Jan 29;1(7431):217–222. doi: 10.1016/s0140-6736(66)90048-1. [DOI] [PubMed] [Google Scholar]
- Parish W. E., Rhodes E. L. Bacterial antigens and aggregated gamma globulin in the lesions of nodular vasculitis. Br J Dermatol. 1967 Mar;79(3):131–147. doi: 10.1111/j.1365-2133.1967.tb15822.x. [DOI] [PubMed] [Google Scholar]
- Pedersen P. V., Hansen F. H., Halveg A. B., Christiansen E. D. Necrotising enterocolitis of the newborn--is it gas-gangrene of the bowel? Lancet. 1976 Oct 2;2(7988):715–716. doi: 10.1016/s0140-6736(76)90009-x. [DOI] [PubMed] [Google Scholar]
- Robinson J. W., Mirkovitch V. The recovery of function and microcirculation in small intestinal loops following ischaemia. Gut. 1972 Oct;13(10):784–789. doi: 10.1136/gut.13.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein H., Beck J., Solomon A., Schmaman A. Gastroenteritis with necrotizing enterocolitis in premature babies. Br Med J. 1972 Jun 10;2(5814):616–619. doi: 10.1136/bmj.2.5814.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch T. P., Sumitswan S. Acute segmental ischaemic enteritis in Thialand. Br J Surg. 1975 Sep;62(9):716–719. doi: 10.1002/bjs.1800620911. [DOI] [PubMed] [Google Scholar]