Abstract
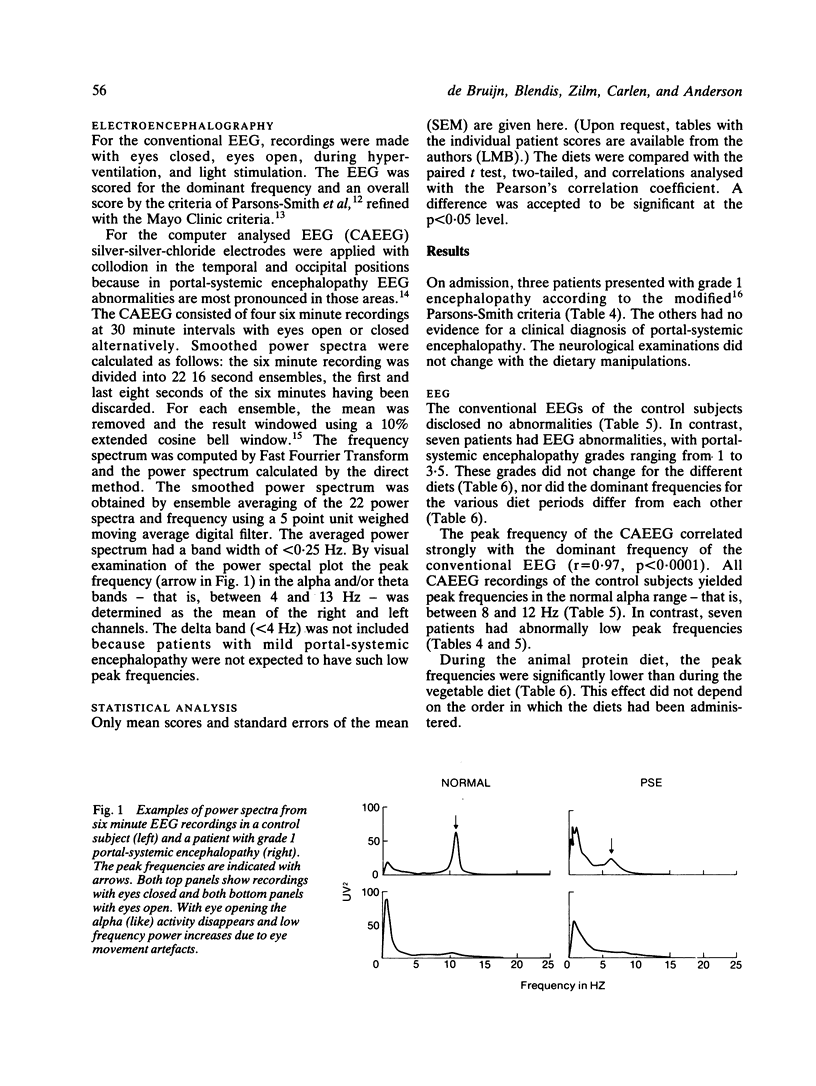
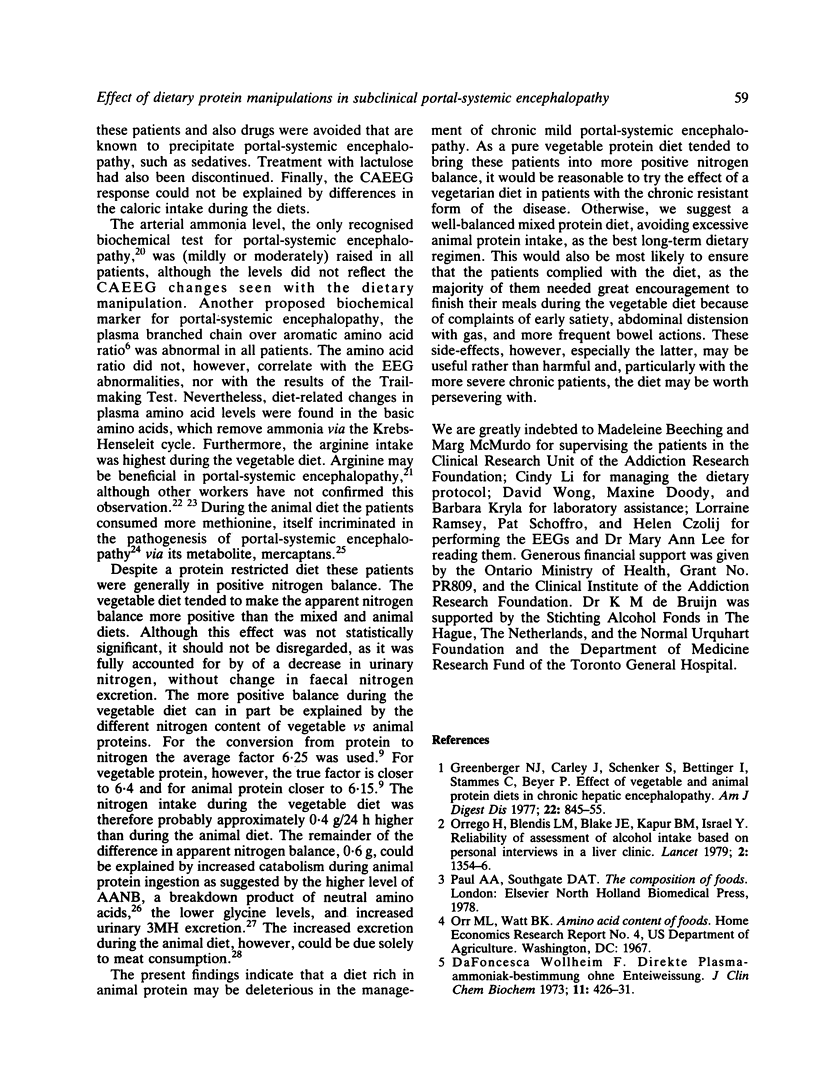
Eight stable cirrhotic patients with mild or subclinical portal-systemic encephalopathy (PSE) were studied after shunt surgery when they were off all antiencephalopathic therapy. Equal amounts of mixed proteins were alternated with animal or vegetable protein in a crossover protocol under metabolic conditions for five consecutive, one week periods. The different dietary periods were not associated with either a change in the neurological impairment score or the Trailmaking Tests, which showed a learning effect. The peak frequencies of the computer analysed EEG (CAEEG) were lower during the animal (6.58 +/- 0.42 Hz) than the vegetable (7.10 +/- 0.44 Hz) diet (p 0.01). Neither arterial ammonia levels nor plasma amino acid ratios changed with the diets, whereas urinary 3-methyl-histidine excretion increased during the animal diet. During the vegetable diet the apparent nitrogen balance tended to be more positive than during either the mixed or animal diets associated with decrease in the urinary nitrogen excretion. The peak frequency of the CAEEG is the most sensitive test to monitor methods of treatment in portal-systemic encephalopathy. A vegetable protein diet, rather than overall protein restriction, should be considered in the management of this disorder, particularly when the nutritional state is poor.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carlen P. L., Wilkinson D. A., Wortzman G., Holgate R., Cordingley J., Lee M. A., Huszar L., Moddel G., Singh R., Kiraly L. Cerebral atrophy and functional deficits in alcoholics without clinically apparent liver disease. Neurology. 1981 Apr;31(4):377–385. doi: 10.1212/wnl.31.4.377. [DOI] [PubMed] [Google Scholar]
- Conn H. O., Leevy C. M., Vlahcevic Z. R., Rodgers J. B., Maddrey W. C., Seeff L., Levy L. L. Comparison of lactulose and neomycin in the treatment of chronic portal-systemic encephalopathy. A double blind controlled trial. Gastroenterology. 1977 Apr;72(4 Pt 1):573–583. [PubMed] [Google Scholar]
- FAHEY J. L., NATHANS D., RAIRIGH D. Effect of L-arginine on elevated blood ammonia levels in man. Am J Med. 1957 Dec;23(6):860–869. doi: 10.1016/0002-9343(57)90295-4. [DOI] [PubMed] [Google Scholar]
- Greenberger N. J., Carley J., Schenker S., Bettinger I., Stamnes C., Beyer P. Effect of vegetable and animal protein diets in chronic hepatic encephalopathy. Am J Dig Dis. 1977 Oct;22(10):845–855. doi: 10.1007/BF01076158. [DOI] [PubMed] [Google Scholar]
- HARPER H. A., NAJARIAN J. S. A clinical study of the effect of arginine on blood ammonia. Am J Med. 1956 Dec;21(6):832–842. doi: 10.1016/0002-9343(56)90097-3. [DOI] [PubMed] [Google Scholar]
- LAIDLAW J. The application in general medical conditions of a visual method of assessing and representing generalized electroencephalographic abnormalities. J Neurol Neurosurg Psychiatry. 1959 Feb;22(1):69–76. doi: 10.1136/jnnp.22.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieber C. S. Alcohol, protein metabolism, and liver injury. Gastroenterology. 1980 Aug;79(2):373–390. [PubMed] [Google Scholar]
- Marliss E. B., Wei C. N., Dietrich L. L. The short-term effects of protein intake on 3-methylhistidine excretion. Am J Clin Nutr. 1979 Aug;32(8):1617–1621. doi: 10.1093/ajcn/32.8.1617. [DOI] [PubMed] [Google Scholar]
- McClain C. J., Zieve L., Doizaki W. M., Gilberstadt S., Onstad G. R. Blood methanethiol in alcoholic liver disease with and without hepatic encephalopathy. Gut. 1980 Apr;21(4):318–323. doi: 10.1136/gut.21.4.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orrego H., Blake J. E., Blendis L. M., Kapur B. M., Israel Y. Reliability of assessment of alcohol intake based on personal interviews in a liver clinic. Lancet. 1979 Dec 22;2(8156-8157):1354–1356. doi: 10.1016/s0140-6736(79)92831-9. [DOI] [PubMed] [Google Scholar]
- PARSONS-SMITH B. G., SUMMERSKILL W. H., DAWSON A. M., SHERLOCK S. The electroencephalograph in liver disease. Lancet. 1957 Nov 2;273(7001):867–871. doi: 10.1016/s0140-6736(57)90005-3. [DOI] [PubMed] [Google Scholar]
- PHEAR E. A., RUEBNER B., SHERLOCK S., SUMMERSKILL W. H. Methionine toxicity in liver disease and its prevention by chlortetracycline. Clin Sci. 1956 Feb;15(1):93–117. [PubMed] [Google Scholar]
- REYNOLDS T. B., REDEKER A. G., DAVIS P. A controlled study of the effects of L-arginine on hepatic encephalopathy. Am J Med. 1958 Sep;25(3):359–367. doi: 10.1016/0002-9343(58)90073-1. [DOI] [PubMed] [Google Scholar]
- Read A. E., McCarthy C. F., Ajdukiewicz A. B., Brown G. J. Encephalopathy after portacaval anastomosis. Lancet. 1968 Nov 9;2(7576):999–1001. doi: 10.1016/s0140-6736(68)91295-6. [DOI] [PubMed] [Google Scholar]
- Rehnström S., Simert G., Hansson J. A., Johnson G., Vang J. Chronic hepatic encephalopathy. A psychometrical study. Scand J Gastroenterol. 1977;12(3):305–311. doi: 10.3109/00365527709180932. [DOI] [PubMed] [Google Scholar]
- Richterich R., Küffer H. Die Bestimmung des Harnstoffs in Plasma und Serum (Urease/Berthelot-Methode) mit dem Greiner Electronic Selective Analyzer GSA II. Z Klin Chem Klin Biochem. 1973 Dec;11(12):553–564. [PubMed] [Google Scholar]
- Rikkers L., Jenko P., Rudman D., Freides D. Subclinical hepatic encephalopathy: detection, prevalence, and relationship to nitrogen metabolism. Gastroenterology. 1978 Sep;75(3):462–469. [PubMed] [Google Scholar]
- Rosen H. M., Yoshimura N., Hodgman J. M., Fischer J. E. Plasma amino acid patterns in hepatic encephalopathy of differing etiology. Gastroenterology. 1977 Mar;72(3):483–487. [PubMed] [Google Scholar]
- Young V. R., Munro H. N. Ntau-methylhistidine (3-methylhistidine) and muscle protein turnover: an overview. Fed Proc. 1978 Jul;37(9):2291–2300. [PubMed] [Google Scholar]
- da Fonseca-Wollheim F. Direkte Plasmaammoniakbestimmung ohne Enteiweissung. Verkesserter enzymatischer Ammoniaktest, II. Mitteilung. Z Klin Chem Klin Biochem. 1973 Oct;11(10):426–431. [PubMed] [Google Scholar]


