Abstract
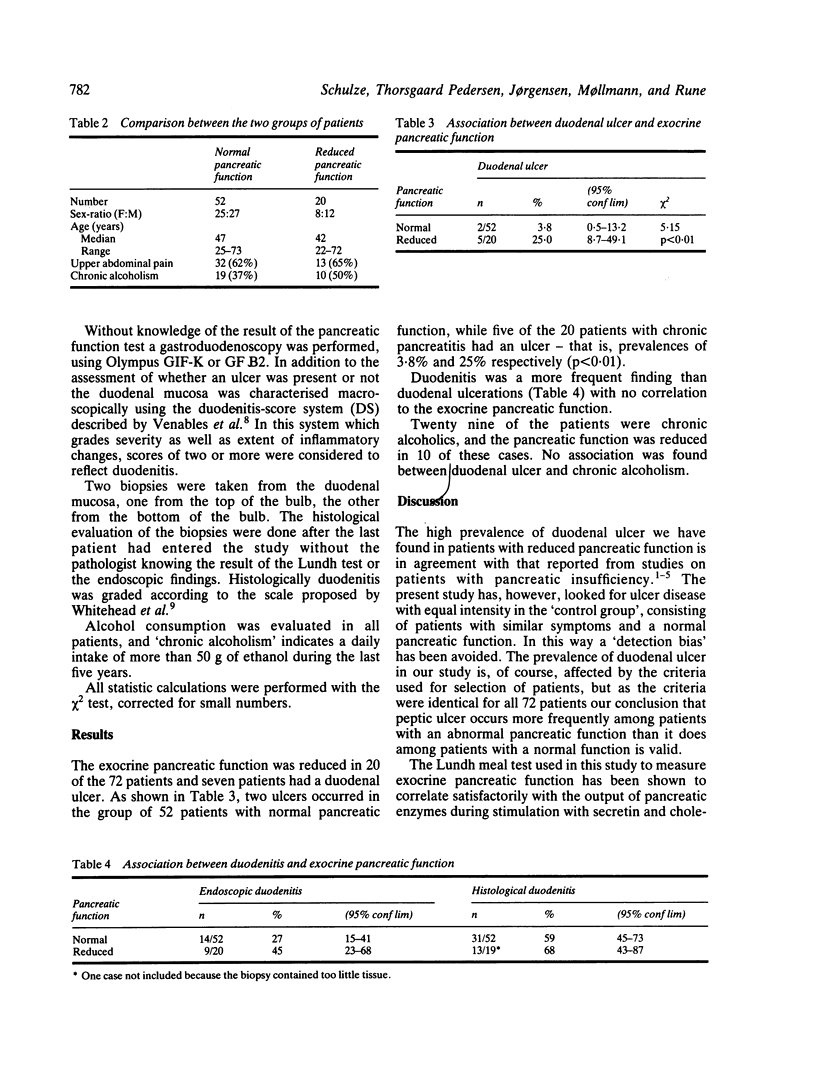
Seventy two patients admitted to a medical department with dyspepsia but without a previous diagnosis of peptic ulcer disease or chronic pancreatitis were studied consecutively. A pancreatic function test (Lundh meal test) and an upper endoscopy was made in all patients. There was no difference in age, sex ratio, occurrence of upper abdominal pain or chronic alcoholism between the groups of patients with reduced pancreatic function (20) and the group with normal function (52). Seven duodenal ulcers were found, two in patients with normal pancreatic function (2/52 = 3.8%; 95% conf lim: 0.5-13.2) and five in patients with reduced pancreatic function (5/20 = 25%; 95% conf lim: 8.7-49.1). This difference was statistically significant (p less than 0.01). Duodenitis occurred with equal frequency in the two groups.
Full text
PDF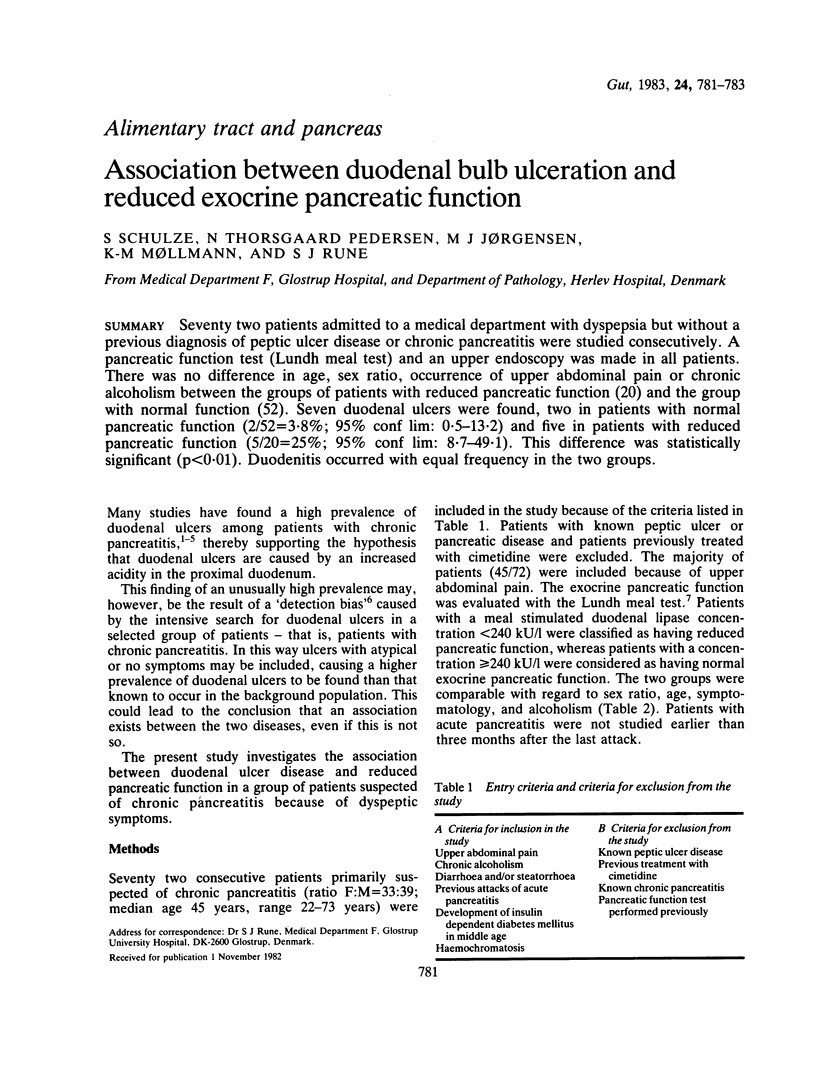

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bernades P., Callet B., Dupuy R. Etude clinique et évolutive de 102 cas de pancréatite chronique. Nouv Presse Med. 1975 Jan 18;4(3):149–152. [PubMed] [Google Scholar]
- Braganza J. M., Rao J. J. Disproportionate reduction in tryptic response to endogenous compared with exogenous stimulation in chronic pancreatitis. Br Med J. 1978 Aug 5;2(6134):392–394. doi: 10.1136/bmj.2.6134.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson R. M. Factors complicating observed associations between peptic ulcer and other diseases. Gastroenterology. 1975 Jun;68(6):1608–1614. [PubMed] [Google Scholar]
- Dreiling D. A., Naqvi M. A. Peptic ulcer diathesis in patients with chronic pancreatitis. Am J Gastroenterol. 1969 Jun;51(6):503–510. [PubMed] [Google Scholar]
- Dutta S. K., Russell R. M., Iber F. L. Impaired acid neutralization in the duodenum in pancreatic insufficiency. Dig Dis Sci. 1979 Oct;24(10):775–780. doi: 10.1007/BF01317211. [DOI] [PubMed] [Google Scholar]
- FITZGERALD O., FITZGERALD P., FENNELLY J., MCMULLIN J. P., BOLAND S. J. A CLINICAL STUDY OF CHRONIC PANCREATITIS. Gut. 1963 Sep;4:193–216. doi: 10.1136/gut.4.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahrenkrug J., Schaffalitzky de Muckadell O. B., Rune S. J. pH threshold for release of secretin in normal subjects and in patients with duodenal ulcer and patients with chronic pancreatitis. Scand J Gastroenterol. 1978;13(2):177–186. doi: 10.3109/00365527809181745. [DOI] [PubMed] [Google Scholar]
- James O., Agnew J. E., Bouchier I. A. Chronic pancreatitis in England: a changing picture? Br Med J. 1974 Apr 6;2(5909):34–38. doi: 10.1136/bmj.2.5909.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottaleb A., Kapp F., Noguera E. C., Kellock T. D., Wiggins H. S., Waller S. L. The Lundh test in the diagnosis of pancreatic disease: a review of five years' experience. Gut. 1973 Nov;14(11):835–841. doi: 10.1136/gut.14.11.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regan P. T., Malagelada J. R., Dimagno E. P., Go V. L. Postprandial gastric function in pancreatic insufficiency. Gut. 1979 Mar;20(3):249–254. doi: 10.1136/gut.20.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead R., Roca M., Meikle D. D., Skinner J., Truelove S. C. The histological classification of duodenitis in fibreoptic biopsy specimens. Digestion. 1975;13(3):129–136. doi: 10.1159/000197701. [DOI] [PubMed] [Google Scholar]
- Worning H., Müllertz S., Thaysen E. H., Bang H. O. pH and concentration of pancreatic enzymes in aspirates from the human duodenum during digestion of a standard meal in patients with pancreatic diseases. Scand J Gastroenterol. 1968;3(1):83–90. doi: 10.3109/00365526809180104. [DOI] [PubMed] [Google Scholar]
- Worning H. The pancreatic secretion of amylase as compared to the amylase concentration in the intestinal contents after ingestion of a meal. Scand J Gastroenterol. 1971;6(3):257–260. doi: 10.3109/00365527109180704. [DOI] [PubMed] [Google Scholar]


