Nine decades after the disappearance of the infamous Spanish flu, its ghost is threatening again. In many countries, panicking citizens are buying drugs from uncertain sources through the internet for a disease that does not yet exist.1 In September 2005, Dr Nabarro, the World Health Organization's public health expert coordinating the response to avian influenza, told the Associated Press that a global avian influenza pandemic could kill 150 million people worldwide.2 What are the risks of a pandemic and is stockpiling antiviral drugs the best response?
How real is the risk of pandemic?
A new pandemic with a highly pathogenic influenza strain is obviously possible. But other infectious agents present similar risks—for example, an Ebola epidemic with airborne transmission, an AIDS epidemic with a much more virulent strain of HIV (superbug), or massive food poisoning such as the dioxin crisis. Airborne transmission of the extremely lethal Ebola Zaire virus might cause a devastating epidemic and is popular in both fiction and (alleged) non-fiction. The HIV superbug appeared in February 2005 in New York as a virus with multiple mutations, multiple drug resistance, and a rapid course of infection, but in only one person. The case served to rekindle the US public's fear after interest in AIDS had been waning because of Iraq.
In the Belgian dioxin crisis, dioxins got mixed up in the food chain, causing levels of exposure to dioxins similar to those in the 1980s.3 The crisis fell conveniently (for the political opposition) just before an election. Competitors in the highly regulated European food market saw their chance to increase market shares. Seven million chicken and 60 000 pigs were slaughtered. Not one person has been detected with any observable consequence of dioxin poisoning.
Perception of risk
In a global world with global media coverage and competition for sensational news, any hypothetical doomsday scenario that could capture the public imagination risks unleashing a media storm. Disease experts are vying for attention and consequent research funding. The perception of risk is then easily distorted from the actual risk. People intuitively overestimate the risk of rare events and underestimate the risk of common events.4
People perceive unlikely and uncertain catastrophes as more threatening than frequent and likely risks. The risk that next winter you will be killed in a car crash is far higher than that you will killed by highly pathogenic flu, an unusual event. Moreover, you are much more likely to be killed by non-pandemic flu than by pandemic flu.5 Winter flu causes cumulatively more disease and death than pandemic flu, but as annual flu occurs annually we are used to it.
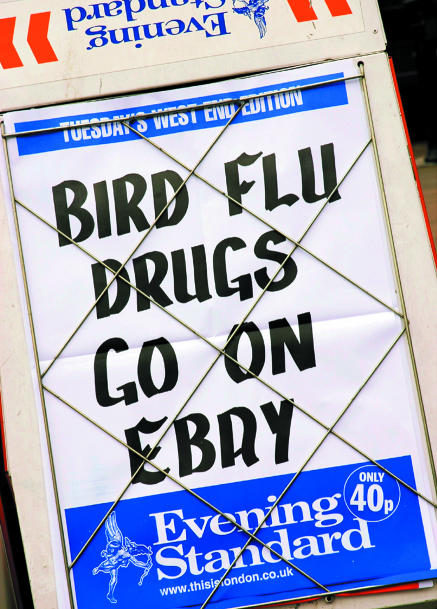
Figure 1.
Getting into a flap about flu
Credit: NICHOLAS BAILEY/REX
Perception of risk is linked to the subjective feeling of control: although driving your car is more dangerous than taking a plane, the risk of driving is more readily accepted than the risk of flying. The threat of a pandemic is particularly scary as we lack control, which in turn tempts us into aimless activity.
Confusion about flu
In the popular press and citizens' minds, avian influenza, winter flu, pandemic flu, and a catastrophic pandemic like Spanish flu are confounded, with some help from disease advocates. We should therefore classify flu epidemics.5
Annual winter flu—Since the 1980s winter flu has caused between two and five excess deaths per 100 000 person-years.6 Most of those who die are frail, predominantly elderly people and those with chronic heart or lung disease. Among people younger than 65, excess mortality was 0 to 1 per million.6
Pandemic of avian flu among birds—Outbreaks of avian flu are frequent.7 The recent outbreak is caused by a virus that can infect humans, as were similar outbreaks since 1997. The virus is highly pathogenic but cannot sustain an epidemic among humans. Since 2003, about 60 people have died each year worldwide.8
Influenza A viruses—These viruses also cause pandemics. In the last 1968-9 pandemic excess mortality was 14 per 100 000 person-years, some three times more than in annual winter flu. The excess death rate among people younger than 65 was 6 per 100 000, with most of these deaths in people aged 50-65.6
Spanish flu—The infamous 1918-9 outbreak claimed an estimated 250 000 deaths in the United Kingdom alone. It combined the highly unusual characteristics of high pathogenicity, the ability to transmit between humans, and high mortality among young people.6 The excess death rate was 166 per 100 000 among people older than 65 but 546 per 100 000 among younger people—a hundred times higher than the rate in the 1968-9 pandemic. This is the only catastrophic flu pandemic with high case fatality among younger people known in all human history.9
Price of control
The wish to feel in control over the looming pandemic, accompanied by clever marketing, has caused an uncontrolled scramble for stockpiles of antiviral drugs. Two neuraminidase inhibitors are active against flu, zanamivir and oseltamivir.10 Neuraminidase inhibitors have been available since the end of the 1990s but have been used rarely during winter flu epidemics. The drugs inhibit virus spread within the respiratory tract, but viral reproduction largely precedes the symptoms.11 They are therefore not very effective in treating clinical flu.12 If taken early after the appearance of symptoms, they reduce the duration of disease by one day; the effectiveness in true life will be worse than in regularly controlled and motivated clinical trial populations. Case fatality is low in patients under 65, limiting potential cost effectiveness to frail patients at high risk of complications, treated within the first 48 hours of symptoms.13
A recent Cochrane review of neuraminidase inhibitors concluded against over-reliance on antiviral drugs.14 It found no credible evidence that neuraminidase inhibitors were effective in avian influenza. Oseltamivir resistant viruses have been observed in up to 16% of infected children. Although these drugs may prevent symptoms and complications, they do not prevent infection or suppress viral nasal excretion, which promotes further viral spread. The successful marketing of these drugs seems to be more the invention of “an ill by a pill.”15
The scramble for neuraminidase inhibitors shows the effects of patenting laws. The manufacturer has the monopoly and the rational monopolist sets the price based on “what the market will bear.” Rich countries are stockpiling the drugs, at an average of $5 (£3; €4) a person, representing less than 1% of their annual healthcare budgets.16 But $5 is higher than the annual healthcare budget for 300 million poor Africans. The Asian nations where the avian flu causes most deaths and where the risks of recombination of avian and human flu are highest cannot afford stockpiles of neuraminidase inhibitors.16
Summary points
The perceived threat of a hypothetical pandemic of avian flu among humans fuels fear
Avian flu, winter flu, pandemic flu, and Spanish flu are often confused and mixed up
Stockpiling antiviral drugs lacks an evidence base and is costly
The energy unleashed by the fear of a pandemic should be directed at tackling real health problems
The development of oseltamivir was a final step in a long history of human discovery, starting in 1942.10 In this long walk, funded in large part by taxpayers,16 the name of Hoffman La Roche appears in 1997, describing oseltamivir. The company should be rewarded justly. Justly does not mean cashing in all the rewards of five decades of research: innovative drugs are not created in an intellectual vacuum by a lonely genius. Present incentives direct all pharmaceutical research to the block-buster drugs that target the scares of the ageing rich. If shortage of production capacity for oseltamivir leads to patenting laws being revised so that industry incentives are redirected to the disease burden of the world, the blindly selfish scramble for neuraminidase inhibitors would turn out to be a blessing.17
Managing global pandemics globally
In history, epidemics and the fear they caused were fertile grounds for public health breakthroughs. The plague epidemics in the Middle Ages in Europe are at the origin of public health authorities. Flu pandemics teach us that global health problems need global solutions. Can the fear of a catastrophic flu pandemic be put to good use?
The old medical humanist adage “To cure sometimes, to relieve often, to comfort always” remains central. There are no magic pills to replace the competent care of dedicated nurses and doctors. In a pandemic, maintaining sufficient admission capacity for acute cases will be crucial. Sufficient capacity of acute care beds and strengthened health services can respond to all types of emergencies, not only a flu pandemic. This holds even more for the weaker healthcare systems in developing countries.18
Our annual foe, winter flu, has killed far more people since the second world war than the number who died in the 1918 pandemic. We could turn the panic for bird flu to better use by increasing our capacity to produce vaccines and increasing vaccination coverage.
If WHO didn't exist, we would have to invent it. A pandemic, even a pandemic of iatrogenic panic, needs global health governance and an institution with an international mandate in health to intervene. However, rather than increasing the panic, supporting wasteful investments in large stocks of drugs of no clear use, and following mindlessly the advice of disease experts with undeniable interests, WHO should help countries to strengthen their health systems and improve their generic capacity to deal with all types of emergencies, not just a hypothetical flu pandemic. WHO should advocate the need for expanded capacity to produce vaccines and for fairer and more workable health exceptions to the international trade agreements.
Conclusion
Panic in epidemics is a part of the human condition.19 The increase in health scares may reflect the absence of real attacks, making us over-react to hypothetical dangers. We should use panic, with good reason or not, to tackle the larger agenda of preventable and curable disease in the world, starting with low vaccination rates in winter flu. International health policy should stay cool and not be distracted by the latest health scare and its industry sponsored quick fix. The humanist road leading to adequate healthcare services for all citizens of the world is still long.
Contributors and sources: LB has a longstanding interest in priority setting in health care and has published widely on public health decision making. WVD is an academic specialised in health systems in developing countries. He is working on control of epidemics and on health policies in countries in fast transition. For this article they studied papers and reports from the scientific literature and authoritative bodies describing the history, effectiveness, and cost-effectiveness of neuraminidase inhibitors in the treatment and prevention of influenza. LB had the idea for the article and discussed it with WVD. LB wrote subsequent drafts, which were completed and reviewed by WVD. Both will act as guarantors.
Competing interests: None declared.
References
- 1.Boersema D. Vogelgriep leidt tot run op virusremmer via website [Bird flu causes run for antivirals through website]. Volkskrant 2005. Oct 20.
- 2.CNN. Bird flu may kill 150m, warns UN, 30 September 2005. www.cnn.com/2005/WORLD/asiapcf/09/29/birdflu.un/ (accessed 13 Mar 2005).
- 3.Bernard A, Hermans C, Broeckaert F, De Poorter G, De Cock A, Houins G. Food contamination by PCBs and dioxins. Nature 1999;401: 231-2. [DOI] [PubMed] [Google Scholar]
- 4.Bellaby P. Communication and miscommunication of risk: understanding UK parents' attitudes to combined MMR vaccination. BMJ 2003;327: 725-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simonsen L, Clarke MJ, Williamson GD, Stroup DF, Arden NH, Schonberger LB. The impact of influenza epidemics on mortality: introducing a severity index. Am J Public Health 1997;87: 1944-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simonsen L, Clarke MJ, Schonberger LB, Arden NH, Cox NJ, Fukuda K. Pandemic versus epidemic influenza mortality: a pattern of changing age distribution. J Infect Dis 1998;178: 53-60. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Spread of avian influenza viruses among birds. www.cdc.gov/flu/avian/gen-info/spread.htm (accessed 13 Mar 2006).
- 8.Macfarlane JT, Lim WS. Bird flu and pandemic flu. BMJ 2005;331: 975-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beveridge WI. The chronicle of influenza epidemics. Hist Philos Life Sci 1991;13: 223-34. [PubMed] [Google Scholar]
- 10.Gubareva LV, Kaiser L, Hayden FG. Influenza virus neuraminidase inhibitors. Lancet 2000;355: 827-35. [DOI] [PubMed] [Google Scholar]
- 11.Dolin R. Influenza. In: Harrison's Principles of Internal Medicine. 15th ed. McGraw-Hill, New York, 2001: 1125-30.
- 12.Cooper NJ, Sutton AJ, Abrams KR, Wailoo A, Turner D, Nicholson KG. Effectiveness of neuraminidase inhibitors in treatment and prevention of influenza A and B: systematic review and meta-analyses of randomised controlled trials. BMJ 2003;326: 1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institute for Health and Clinical Excellence. Guidance on the use of zanamivir, oseltamivir and amantadine for the treatment of influenza. Technology appraisal No 58. www.nice.org.uk/pdf/58_Flu_fullguidance.pdf (accessed 13 Mar 2006).
- 14.Jefferson T, Demicheli V, Rivetti D, Jones M, Di Pietrantonj C, Rivetti A. Antivirals for influenza in healthy adults: systematic review. Lancet 2006;367: 303-13. [DOI] [PubMed] [Google Scholar]
- 15.Moynihan R, Cassels A. Selling sickness: how the world's biggest pharmaceutical companies are turning us all into patients. Berkley, CA: Greystone Books, 2005.
- 16.Lokuge B, Drahos P, Neville W. Pandemics, antiviral stockpiles and biosecurity in Australia: what about the generic option? Med J Aust 2006;184: 16-20. [DOI] [PubMed] [Google Scholar]
- 17.Barton JH, Emanuel EJ. The patents-based pharmaceutical development process: rationale, problems, and potential reforms. JAMA 2005;294: 2075-82. [DOI] [PubMed] [Google Scholar]
- 18.Van Damme W, Van Lerberghe W. Strengthening health services to control epidemics: empirical evidence from Guinea on its cost-effectiveness. Trop Med Int Health 2004;9: 281-91. [DOI] [PubMed] [Google Scholar]
- 19.Van Damme W, Van Lerberghe W. Epidemics and fear. Trop Med Int Health 2000;5: 511-4. [DOI] [PubMed] [Google Scholar]