Abstract
Objective
To assess the etiology, treatment, and utility of anal ultrasound in men with fecal incontinence and to review the outcomes of conservative (nonoperative) treatment.
Summary Background Data
The etiology of fecal incontinence in women is almost exclusively from obstetric or iatrogenic surgical injuries resulting in damage to the anal sphincters and/or pudendal nerves. Corresponding data on men with fecal incontinence are sparse.
Methods
Between January 1995 and January 1998, 37 men with fecal incontinence were evaluated in the John Radcliffe Hospital anorectal ultrasound unit. Their clinical histories, anal ultrasound results, anorectal physiology studies, and responses to conservative therapy were reviewed.
Results
Median age was 57 years. Major incontinence was present in 27% of the patients. Anal ultrasound localized anal sphincter damage in nine patients, and the characteristics of these nine patients with sphincter damage were then compared with the remaining 28 without sphincter damage. Prior anal surgery was more common in patients with sphincter damage. Hemorrhoids were more common in patients without sphincter damage. Anorectal physiology studies revealed significantly lower mean maximum resting and squeeze pressures in patients with sphincter damage, confirming poor sphincter function. With 92% follow-up, patients without sphincter damage were more likely to improve with nonoperative therapy.
Conclusions
Anal ultrasound is extremely useful in the evaluation of fecal incontinence in men. Unlike women, the majority of men do not have a sphincter defect by anal ultrasound, and conservative management is usually successful in these patients. In contrast, in men with anal sphincter damage, almost all of these defects resulted from previous anal surgery. Conservative management rarely is successful in these cases, and surgical repair of the anal sphincter may be indicated. Therefore, because the presence or absence of sphincter damage on anal ultrasound usually predicts the response to nonoperative treatment, anal ultrasound should be used to guide the initial management of men with fecal incontinence.
Fecal incontinence is a devastating and socially embarrassing problem that affects approximately 1% to 5% of the general population. 1 It is often difficult to treat because the underlying etiology is frequently unknown or not amenable to therapy. Fecal incontinence occurs more commonly in women, in the elderly, and in patients with physical limitations and poor health. 2 In fact, the incidence has been reported as high as 39% within the nursing home patient population. 2
Most studies on fecal incontinence have focused on the diagnosis and treatment of women with this disorder. The most common identifiable causes in women include obstetric or iatrogenic surgical injuries resulting in damage to the internal and/or external anal sphincters, or injuries to the pudendal nerves resulting from childbirth and/or straining. Anal ultrasound (AUS) can readily detect defects in the sphincteric complex in up to 87% of incontinent women. 3 Anorectal physiology studies can identify pudendal nerve injuries in a significant number of the remaining patients. 4 Therefore, most female patients prove to have identifiable, physiologic causes of fecal incontinence.
Although women represent the majority of patients with fecal incontinence, several studies have reported that the incidence in men is higher than has been appreciated previously. 2,5 A population-based study in Wisconsin revealed that men made up 37% of all patients with fecal incontinence, but only one third of them sought treatment from a physician. 2 Accordingly, studies characterizing fecal incontinence in men are sparse. 6–8 Therefore, we evaluated our experience with fecal incontinence in male patients over a 3-year period.
METHODS
All male patients referred to the anorectal physiology unit at the John Radcliffe Hospital for evaluation of fecal incontinence between January 1995 and January 1998 form the basis of this study. Clinical histories and severity of fecal incontinence were recorded by a single clinical nurse specialist using a standard form. All patients underwent digital examination, proctoscopy, and rigid sigmoidoscopy by a colorectal specialist. All patients underwent AUS and anorectal physiology studies at our institution.
AUS was performed with a Bruel & Kjaer 10-MHz scanner (Bristol, UK). Anorectal physiology studies were performed with the patient in the left lateral position using a station pull-through technique with an air-filled microballoon catheter connected to a Druck transducer, a Lectromed amplifier, and a high-speed pen recorder type MX-6 (Ormed, Welwyn Garden City, UK). Threshold volume and maximum tolerated volume were measured using an air-filled balloon positioned in the distal part of the rectum. The rectoanal inhibitory reflex was studied by measuring the response of the resting anal pressure to distention of the rectum. A fall of ≥20% denoted a positive response. Anorectal sensation was measured in the upper, middle, and lower anal canal using the mucosal electrosensitivity method. 9 Pudendal nerve terminal motor latency was measured as described by Kiff and Swash. 10
All patients with fecal incontinence were managed initially by a nonoperative, conservative regimen. This consisted of dietary adjustment (usually adopting a low-residue diet), constipating agents (usually loperamide), and if necessary agents to assist complete evacuation (usually bisacodyl suppository 5 to 10 mg per rectum or microlax enemas). First- or second-degree hemorrhoids were treated on an outpatient basis by rubber-band ligation. Patients were followed by outpatient appointments, supplemented by telephone questionnaire if necessary.
Analysis of variance and Fisher’s exact test were used to compare differences between two groups using SPSS software. Significance was defined as p ≤ 0.05.
RESULTS
During the 3-year study period, 37 male patients with fecal incontinence were evaluated. Median age was 57 years (range 21 to 82 years). (During the same period, 272 women with fecal incontinence were assessed.)
Severity of Symptoms
Ten of the patients (27%) had episodes of incontinence to solid feces (major incontinence). The other 27 (73%) had episodes of incontinence to liquid stool or flatus (minor incontinence). The median frequency of incontinent episodes was one per day. Most patients (84%) experienced the sensation of needing to evacuate (call to stool), but only 38% of them were able to defer their movements. Thirty-eight percent reported the need to wear pads secondary to incontinence. Excessive straining during bowel movements occurred in 3%, incomplete emptying in 22%. Rectal bleeding was present in 14%, abdominal pain in 8%, rectal pain in 14%, and pruritus ani in 35%.
Past Medical History
Sixteen of the patients (43%) had a history of, or the presence of, hemorrhoids at the time of evaluation. Twelve (32%) had a history of anal surgery, on average 11 ± 2 years before evaluation. The most common previous operation was a hemorrhoidectomy (n = 7), followed by lateral sphincterotomy (n = 3), anal stretch (n = 3), and fistulectomy (n = 2). No patients in this series had a history of congenital anorectal atresia or any generalized disorder that could have been responsible for incontinence. No patient gave a history of anoreceptive intercourse.
Anal Ultrasound
Of the 37 patients, 9 (24%) had a defect or defects in the sphincter complex. Eight patients had a defect or defects in the internal sphincter, and five had a lesion or lesions in the external sphincter. Therefore, patients were easily classified into two groups by AUS: those with sphincter defects (SD, n = 9) and those without physical defects (NSD, n = 28). Mean sphincter length was similar—3.3 ± 0.2 cm in the SD group and 3.5 ± 0.1 cm in the NSD group.
Anorectal Physiology Studies
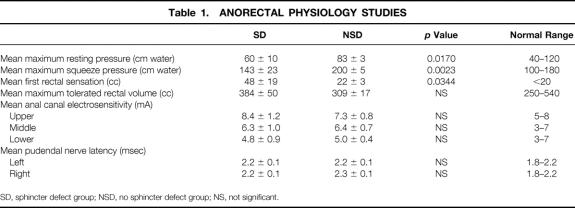
The results of anorectal physiology studies are shown in Table 1. The values for the SD and NSD groups were compared. Both mean maximum resting pressure and maximum squeeze pressures were significantly lower in the SD group (60 ± 10 vs. 83 ± 3 cm water, p = 0.017; 143 ± 3 vs. 200 ± 5 cm water, p = 0.0023, respectively). Mean pressure to elicit a first rectal sensation was higher in the SD group than in the NSD group (48 ± 19 vs. 22 ± 3 cm water, p = 0.0344). There was no significant difference in mean maximum tolerated rectal volume (rectal capacity). All patients in both groups had positive rectoanal inhibitory reflexes. Electrosensitivity of the upper, middle, and lower anal canal and pudendal nerve latencies were within normal limits in both groups as well.
Table 1. Anorectal Physiology Studies
Comparison of the Groups
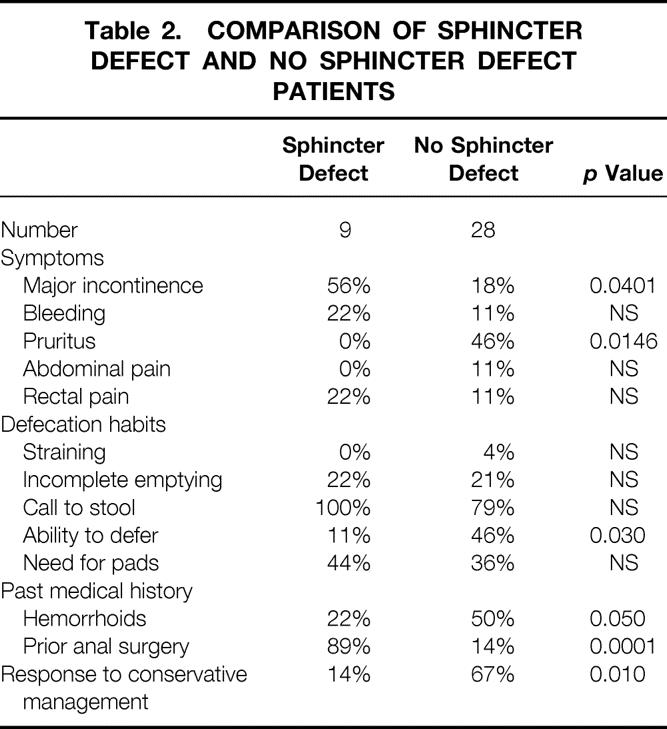
Patients in the two groups were compared with respect to the severity of symptoms, defecation habits, and past medical history (Table 2). With respect to symptoms, major incontinence was present in a higher percentage of the SD group (56% vs. 18%, p = 0.0401). The incidence of pruritus was significantly higher in the NSD group (46% vs. 0%, p = 0.0146). There were no significant differences between the groups in the incidence of bleeding, abdominal pain, or rectal pain. In comparing defecation habits, there was no significant difference in straining, incomplete emptying, call to stool, or the use of pads. However, the SD group had a lesser ability to defer stools (11% vs. 46%, p = 0.030). With regard to past medical history, hemorrhoids were significantly more common in the NSD group (50%) than in the SD group (22%) (p = 0.050). Interestingly, 89% of the SD group had had prior anal surgery, compared with only 14% of the NSD group (p = 0.0001).
Table 2. Comparison of Sphincter Defect and No Sphincter Defect Patients
Follow-Up
Of the 37 patients, 34 (92%) were seen or contacted in follow-up after a trial of conservative management. Median follow-up was 10 months (range 3 to 36 months). Twelve patients (35%) reported significant improvement or total resolution of symptoms, whereas seven (21%) had slight improvement. Of these 19 patients with improvement, 9 had taken constipating medications, 6 had had hemorrhoids treated, 3 had responded to dietary changes, and 1 had had total relief by cessation of antibiotic therapy. Fifteen patients (44%) had no change in their symptoms.
In comparing the two groups (Table 2), of the seven SD patients seen in follow-up, six (86%) had no change in their symptoms with conservative management and are awaiting definitive treatment. Only one (14%) had experienced resolution of his symptoms. In contrast, in the NSD group, 67% had improvement of symptoms with the conservative approach described. The difference in response rates between the two groups was statistically significant (p = 0.010).
DISCUSSION
The importance of obstetric factors in the etiology of female fecal incontinence, either through direct sphincter injury or damage to sphincter innervation, has come to be appreciated in recent years. 11,12 As in our experience, most reports from anorectal physiology units suggest that >90% of patients referred for evaluation of fecal incontinence are women. Few studies have focused on fecal incontinence in men. 6–8 However, population studies suggest that at least one third of fecally incontinent patients within the general population are men. 2 The reason for this discrepancy is unclear.
In this study of 37 male patients, 27% had episodes of solid stool incontinence (major incontinence); the remainder had episodes of liquid and/or gas incontinence (minor incontinence). Patients with minor seepage (or soiling) are difficult to manage successfully. The majority of patients in this study complained of seepage, in addition to true incontinence. However, the higher incidence of pruritus ani (47%) and hemorrhoids (50%) in the NSD group suggests that some of the patients described as having minor fecal incontinence in this study might well be described as “soilers” or “seepers” by others.
Two recent studies have concentrated on men with fecal leakage 6 or seepage, 7 in the absence of other obvious anorectal pathology. Sentovich et al 6 studied 25 men with fecal incontinence and distinguished “leakers” (56%) from those with true incontinence (44%). They argued that the distinction is easy to make, and reported significant manometric differences. Patients with true incontinence had low anal canal pressures. Patients with leakage had intermediate pressures, between normal and the truly incontinent group, but tended to have longer anal canals. They argued that because of the long anal canal, small amounts of stool are left in the anal canal and may subsequently leak some time after a bowel movement. Parellada et al 7 identified a similar group of men with idiopathic seepage, but found resting anal canal pressures to be greater than controls.
We agree with both of these groups that fecal seepage is a disorder of anal canal clearing, which typically results in minor staining of the underwear after defecation, pruritus ani, moist anus, and/or perianal eczema. Most cases result from local pathology such as hemorrhoids, which should be treated in the usual manner. These patients do not usually require more detailed anorectal physiologic investigation.
No patient in this study gave a history of anoreceptive intercourse. The importance of anoreceptive intercourse in the etiology of fecal incontinence is uncertain. Chun et al 8 reported lower resting anal canal pressures in men with a history of anorectal intercourse compared with matched controls, although squeeze pressures were similar and no defects in either the internal or external sphincter were demonstrated by ultrasound.
Previous anal surgery was, as expected, more common in the SD group. The risks of iatrogenic damage to the anal sphincter mechanism are well known. 4,10–12 There has been a trend over the past few years to avoid any procedures that may compromise the anal sphincter mechanism. For anal fissures, the Lords anal stretch has been largely abandoned, and pharmacologic methods of reducing anal sphincter pressures are replacing lateral internal sphincterotomy. For fistulas, the more widespread use of drainage setons may have reduced the incidence of significant sphincter damage.
Anorectal manometry indicated that the SD group had lower resting and squeeze pressures compared with the NSD group. However, the median for both groups was close to the normal range for controls previously assessed in the same laboratory. The remainder of the physiologic results, apart from a marginally increased volume to first rectal sensation, were within the normal range for both groups of patients. Impaired rectal sensation has been reported to be associated with fecal incontinence, particularly with minor seepage. 13
The patients in this study did not routinely undergo any further investigation of their fecal incontinence. In severe cases, particularly if the clinical picture is not adequately explained by the basic anorectal physiology and ultrasound, further investigation is needed. Our next line of studies would include ambulatory manometry, barium enema, and/or colonoscopy to assess colonic and rectal motility and/or magnetic resonance imaging to rule out any underlying pathology in the lumbosacral spinal region. In none of the patients in this study who underwent these additional tests were abnormalities found that would explain their fecal incontinence.
The conservative (nonoperative) management of the patients in this study followed the general principles for the treatment of fecal incontinence. The results of sphincter repair, even for isolated muscle defects, are not perfect, and most patients should undergo a thorough trial of nonoperative treatment. The use of constipating drugs was the most effective medical treatment in this group. This study highlights the role of AUS in discriminating patients who may benefit from conservative measures from those who are likely to require surgical intervention.
In conclusion, AUS proved to be the most useful investigation for predicting the success of nonoperative therapy for the treatment of fecal incontinence in men. Patients with no sphincter defect demonstrated on ultrasound tended to have less severe incontinence and were more likely to respond to simple, nonoperative measures, including dietary adjustment, constipating drugs, and/or banding of hemorrhoids. Patients with an ultrasonographically demonstrated sphincter defect should be warned that their condition is difficult to treat conservatively and that surgical correction of the defect may well be required.
Discussion
Dr. John H. Pemberton (Rochester, Minnesota): Fecal incontinence is a big problem, and it will only become bigger as the population ages. Nearly all the literature on fecal incontinence is about female fecal incontinence. This paper addresses the problem in men and is thus nearly unique. It is important to separate major and minor fecal incontinence, as patients with minor fecal incontinence invariably respond to conservative measures, such as stool-bulking agents and irrigation to insure complete rectal emptying.
As I said, I have enjoyed this presentation very much, but I do have a few questions. I do not understand the recommendation to treat patients with low-residue diets as part of the conservative management routine for fecal incontinence. We have found over a long period of time that high-fiber diets and stool-bulking agents will help to insure complete emptying and better control of the stools which become of a more manageable consistency. Could the authors comment on this apparent disparity in the two practices?
I think there is a superb take-home practice point in this paper. If the male patient has as sphincter defect on ultrasound and major fecal incontinence, then it should be fixed—simply and quite clearly. There is little chance that conservative measures will help. If not, then conservative measures would likely work two thirds to 80% of the time. What, however, would the authors recommend for a patient with a defect and minor fecal incontinence? Will it get better? Does he need immediate repair?
I agree that the outcome of repair or a sphincter defect is indeed variable and should not be undertaken lightly. But in men, the consequence may not be as great as in women if there is complication, because men have a much longer and more robust anal canal than do women.
Finally, I do not see a reference in this paper or the presentation to the use of biofeedback management for the management of fecal incontinence. We feel that even in patients with sphincter defects—and I will agree these are mainly women—that they can regain some degree of reasonable control of the stool in about half time, thus sparing an operation. Would the authors please comment on pelvic floor training or biofeedback in the management of minor and major fecal incontinence in men, with and without sphincter defects?
Dr. James V. Sitzmann (Washington, D.C.): As everyone here knows, continence is the result of—to be continent is the result of a series of very complex and interdependent functions which involve both the colon (and the) small intestine, especially colonic water absorption function and colonic reservoir functions, in addition to rectal innervation and anal sphincteric control.
This rather excellent study and tremendous presentation by Herb Chen and his colleagues evaluates the use of anorectal ultrasound and anorectal manometry to evaluate the integrity of the latter two functions, that being anal sphincteric control and rectal innervation. My questions are the following:
What percentage of these patients had colonic motility problems, and what role will colonic motility or dismotility issues play in incontinence? The data indicated failure to respond to the low-fiber diet and loperamide in a subgroup of spastic or hypermodal bowel patients.
What is the need for other radiographic evaluation in the evaluation of patients with incontinence? Specifically, what is the role for barium enema or defecography?
And, finally, a significant number of nonsphincter-damaged–group patients had relatively minor incontinence symptoms. What percentage of these patients simply had exuberant hemorrhoids and needed to go right to hemorrhoidectomy or to conservative management of hemorrhoids?
Lastly, where does anorectal ultrasound fit in our evaluation of these patients? Should we employ anorectal ultrasound on all patients who are incontinent or patients who fail conservative management or simply in patients who are incontinent and have had prior surgery?
Dr. Ward O. Griffen, Jr. (Frankfort, Michigan): I’d just like to ask—I presume, of course, you use ultrasound after you have done a rectal exam? And oftentimes with a rectal exam, you can detect a sphincter defect. How much does this procedure cost, and how time-consuming is it? Because I think that would be important.
Dr. Bruce D. George (Closing Discussion): To take, first of all, Dr. Pemberton’s questions, I am reluctant, initially, to disagree about the management in terms of low-residue or high-residue diet. I can only say that our experience in Oxford is that a low-residue diet is helpful in the vast majority of patients, particularly with more minor fecal incontinence. I am not aware of any randomized control trials comparing the two, and I think that would be quite an appropriate way forward to answer that question.
Your next question about the problem of a male patient with minor fecal incontinence with a defect demonstrated on ultrasound. I agree that that is a difficult problem. I think the major benefit in rectal ultrasound is that it does demonstrate—if it does demonstrate a defect, it tells you that conservative treatment is unlikely to be beneficial. You then at least know where you stand, and you can weigh out the benefits of staying as you are with conservative treatment, which may not help a lot, versus the risks of sphincter repair, which I am afraid we all have to accept. The results of sphincter repairs are not wonderful, and a person with minor symptoms, I would certainly be reluctant to embark on sphincter reconstruction.
You touched on the question of biofeedback. We have not addressed that question. We do use biofeedback principally in female patients with both constipation problems and incontinence, but it was not the primary purpose of this study to address that question.
Dr. Sitzmann, you raised the possibility of the question of colonic motility problems in these patients. I agree that fecal incontinence in men, particularly if it is not clear after basic assessment including physiology and ultrasound, is a difficult problem. And our next phase of investigations in that very small minority of patients would be ambulatory colonic motility and also probably a pelvic lumbosacral MRI scan to look particularly for back problems or, as you alluded to, a colonic motility problem.
And you mentioned defecography. I would agree that incontinence is not just a problem of motor function. Sensation is important, and also the ability to evacuate correctly. And many patients will have an associated evacuation problem which may come to light with detailed defecography.
And, finally, Mr. President, I would stress that we always examine our patients with rectal examinations before an anorectal ultrasound. And several studies have shown that, certainly, our finger is not as good as anorectal ultrasound at detecting subtle sphincter defects.
Footnotes
Correspondence: Herbert Chen, MD, Department of Surgery, Blalock 685, The Johns Hopkins Hospital, 600 N. Wolfe St., Baltimore, MD 21287.
Presented at the 110th Annual Meeting of the Southern Surgical Association, December 6–9, 1998, The Breakers, West Palm Beach, Florida.
Accepted for publication December 1998.
References
- 1.Enck P, Bielefedt K, Rathmann W, Purrman J, Tschope D, Erckenbrecht JF. Epidemiology of faecal incontinence in selected patient groups. Int J Colorectal Dis 1991; 6: 143–146. [DOI] [PubMed] [Google Scholar]
- 2.Nelson R, Norton N, Cautley E, Furner S. Community-based prevalence of anal incontinence. JAMA 1995; 274: 559–561. [PubMed] [Google Scholar]
- 3.Law PJ, Kamm MA, Bartram CI. Anal endosonography in the investigation of faecal incontinence. Br J Surg 1991; 78: 312–314. [DOI] [PubMed] [Google Scholar]
- 4.Snooks SJ, Swash M, Henry MM, Setchell M. Effect of vaginal delivery on the pelvic floor: a five-year follow-up. Br J Surg 1990; 77: 1358–1360. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA, Li Z, Andruzzi E, et al. US householder survey of functional GI disorders: prevalences, sociodemography, and health impact. Dig Dis Sci 1993; 38: 1569–1580. [DOI] [PubMed] [Google Scholar]
- 6.Sentovich SM, Rivela LJ, Blatchford GJ, Christensen MA, Thorson AG. Patterns of male fecal incontinence. Dis Colon Rectum 1995; 38: 281–285. [DOI] [PubMed] [Google Scholar]
- 7.Parellada CM, Miller AS, Williamson MER, Johnston D. Paradoxical high anal resting pressures in men with idiopathic fecal seepage. Dis Colon Rectum 1988; 41: 593–597. [DOI] [PubMed] [Google Scholar]
- 8.Chun AB, Rose S, Miltrani C, Silvestre AJ, Wald A. Anal sphincter structure and function in homosexual males engaged in anoreceptive intercourse. Am J Gastroenterology 1997; 92: 465–468. [PubMed] [Google Scholar]
- 9.Roe Am, Bartolo DC, Mortenson NJ. New method for assessment of anal sensation in various anorectal disorders. Br J Surg 1986; 73: 310–312. [DOI] [PubMed] [Google Scholar]
- 10.Kiff ES, Swash M. Slowed conduction in the pudendal nerves in idiopathic (neurogenic) fecal incontinence. Br J Surg 1984; 71: 614–616. [DOI] [PubMed] [Google Scholar]
- 11.Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal sphincter disruption during vaginal delivery. N Engl J Med 1993; 329: 1905–1911. [DOI] [PubMed] [Google Scholar]
- 12.Snooks SJ, Swash M, Henry MM, Setchell MM. Risk factors in childbirth causing damage to the pelvic floor innervation. Int J Colorectal Dis 1986; 1: 20–24. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann BA, Timmcke AE, Gathright JB, Hicks TC, Opelka FG, Beck DE. Fecal seepage and soiling: a problem of rectal sensation. Dis Colon Rectum 1995; 38: 746–748. [DOI] [PubMed] [Google Scholar]