Abstract
Objective and Background
Tertiary medical centers continue to be under extreme pressure to deliver high-complexity care, but paradoxically there is considerable pressure within these institutions to reduce their emphasis on tertiary care and refocus their efforts to develop a more community-like practice. The genesis of this pressure is the perceived profitability of routine surgical activity when compared with more complex care. The purpose of this study is to assess how the total cost and profit (loss) margin can vary for an entire trauma service. The authors also evaluate payments for specific trauma-related diagnostic-related groups (DRGs) and analyze how hospital margins were affected based on mortality outcome.
Materials and Methods
The authors analyzed the actual cost of all trauma discharges (n = 692) at their level I trauma center for fiscal year 1997. Data were obtained from the trauma registry and the hospital cost accounting system. Total cost was defined as the sum of the variable, fixed, and indirect costs associated with each patient. Margin was defined as expected payments minus total cost. The entire population and all DRGs with 10 or more patients were stratified based on survival outcome, Injury Severity Score, insurance status, and length of stay. The mean total costs for survivors and nonsurvivors within these various categories and their margins were evaluated.
Results
The profit margin on nonsurvivors was $5898 greater than for survivors, even though the mean total cost for nonsurvivors was $28,821 greater. Within the fixed fee arrangement, approximately 44% of transfers had a negative margin. Both survivors and nonsurvivors become increasingly profitable out to 20 days and subsequently become unprofitable beyond 21 days, but nonsurvivors were more profitable than survivors.
Conclusions
There is a wide variance in both the costs and margins within trauma-related DRGs. The DRG payment system disproportionately reimburses providers for nonsurvivors, even though on average they are more costly. Because payers are likely to engage in portfolio management, patients can be transferred between hospitals based on the contractual relationship between the payer and the provider. This payment system potentially allows payers to act strategically, sending relatively low-cost patients to hospitals where they use fee-for-service reimbursement and high-cost patients to hospitals where their reimbursement is contractually capped. Although specific to the authors’ trauma center and its payer mix, these data demonstrate the profitability of maintaining a level I trauma center and preserving the mission of delivering care to the severely injured.
Tertiary medical centers continue to accept and treat highly complex patients. In fact, university-based medical centers are often thought of as “the last stop” for many of these patients. Although these centers benefit from the educational challenges presented by the most severely injured, the persistent transfer of high-acuity patients into the university system can place the tertiary medical center in a difficult situation within the community referral base. Although medically obligated to accept all patients regardless of acuity, it is the more complex cases that potentially compromise the economic position of the tertiary institution. This perceived economic compromise results from the belief that the most severely injured are not only the most costly but are also among the riskiest patients financially and the least well reimbursed. The cost of treating these patients is typically high and extremely variable (even when controlling for diagnosis); because of the fixed fee contracts that hospitals have with many insurers, trauma services can lose significant sums of money on large numbers of patients. The financial losses and financial risks are compounded by the dearth of information both from within individual hospitals and more generally in the medical literature. Physicians are working in the dark.
The potential outcome of treating these complex patients is one of severe economic strain. Moreover, current surgical doctrine maintains the belief that community-based practices that consist of more elective outpatient surgery are in fact more profitable. Currently, while most if not all health systems are focusing considerable effort on cost containment, little attention has been directed toward patient mix or payer activities and how their actions may affect the service bottom line. The purpose of this study is to assess the profit (loss) margin on the trauma service, and to determine how survival status and patient complexity affect costs and margins. In addition, the study is designed to investigate the possibility that financial risk management could play a significant role in a service’s ability to ensure the delivery of consistently high-quality care.
METHODS
We analyzed cost data for all trauma discharges (n = 692) from our level I trauma center in fiscal year 1997. Data were obtained from the trauma registry and the hospital cost accounting system, TSI (Transition Systems Incorporated). These data include patient age, length of stay (LOS), discharge status, Injury Severity Score (ISS), diagnostic-related group (DRG) assignment, transfer status, financial classification (insurance status), total cost, and expected payment.
Allocations of costs to the trauma service are based on applying various cost accounting standards from the hospital general ledger, billing, and payroll systems. Total cost of a patient care encounter is defined as variable cost plus hospital and trauma service overhead. Margin is defined as expected payments minus the total cost.
All analyses were performed in the following fashion. The entire population was evaluated and then subsequently stratified based on survivor, transfer, or insurance status, ISS greater than or less than 15, length of stay, and DRG allocation. Through a systematic data mining process, various permutations of these variables were analyzed. Cost per case and margin were determined for the entire population and subsequently stratified by survivor or nonsurvivor status. Also, LOS was determined for the entire population and stratified based on survivor status. The difference in mean cost per case between the nonsurvivors and survivors was computed.
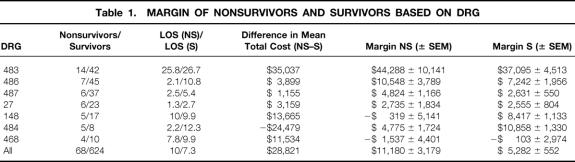
DRG stratification was determined based on DRGs that contained 10 or more patients and had at least one nonsurvivor within their classification—thus, DRGs 483, 486, 487, 27, 148, 484, and 468 were analyzed (Table 1). The definitions of each DRG are as follows: 27—traumatic stupor and coma >1 hour; 148—major small and large bowel procedure with complication; 468—OR procedure unrelated to principal diagnosis; 483—tracheostomy excluding face, mouth, neck diagnosis; 484—craniotomy for multiple trauma; 486—other procedure for multiple trauma; 487—other multiple significant trauma.
Table 1. Margin of Nonsurvivors and Survivors Based on DRG
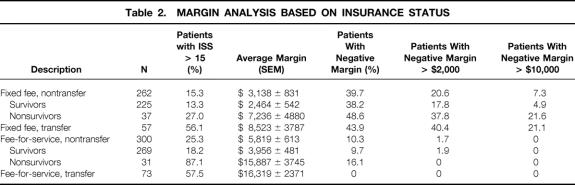
Patients were then reclassified based on insurance and transfer status. They were then indexed by survivor status and ISS. Margins were calculated as well as a focused determination of the percentage of patients who had large negative margins (Table 2). Classification of fixed fee contracts would include previously contracted arrangements (Medicare, Medicaid, Blue Cross/Blue Shield, or HMO payments); “non-fixed fee” arrangements represented the commercial payers who had no preexisting contract with the hospital.
Table 2. Margin Analysis Based on Insurance Status
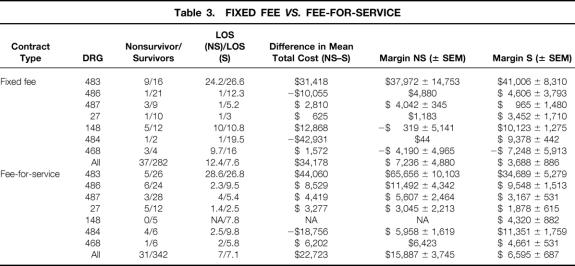
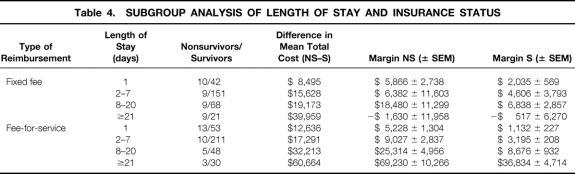
Patients with fixed fee contracts were then analyzed based on DRG grouping and insurance status. Survival status, LOS, and margins were then evaluated. This analysis was also performed for the non-fixed fee group (Table 3). The fixed fee contract and fee-for-service patients were then evaluated based on LOS, with attention focused on the margins associated with LOS (Table 4).
Table 3. Fixed Fee vs. Fee-for-Service
Table 4. Subgroup Analysis of Length of Stay and Insurance Status
RESULTS
The mean age of the entire population was 42 years—54 ± 3 for nonsurvivors and 40 ± 1 for survivors. Sixty of the 692 patients (9.8%) died while on the service. Mean LOS was 7.54 days for all patients—10 days for nonsurvivors and 7.3 days for survivors. The mean total cost was $48,721 ± 7098 for nonsurvivors and $19,791 ± 1263 for survivors. The profit margin was $11,180 ± 3,179 for nonsurvivors and $5,282 ± 552 for survivors (see Table 1).
Analysis of the insurance status revealed a wide variance in the margins based on the type of insurance and whether the patient was transferred from another institution. The largest payers—Medicare, Medicaid, Blue Cross/Blue Shield, and a university-sponsored HMO (M-Care)—all had fixed fee (DRG-based) contracts with the hospital. All or nearly all of the remaining payers had traditional fee-for-service reimbursement, presumably because they had no formal contract with the hospital. Table 2 depicts the number of patients who were classified by these parameters and the margins associated with these patient classifications. As might be expected, >50% of the patients transferred to the university trauma service sustained severe injury (ISS >15) regardless of the patient’s insurance status. Of particular interest is the presence of the largest profit margins in the transfer group. Based on their insurance status, we evaluated the percentage of patients with negative margins and whether a transfer occurred. Finally, the table notes the percentage of cases in each category that involved negative margins, losses >$2000, and losses >$10,000. In the fixed fee group, approximately 44% of the transfers had a negative margin, and approximately half of those with a negative margin had a loss >$10,000. All transfers survived.
We then divided the population based on the presence of a fixed fee contract or fee-for-service arrangement (see Table 3). Aggregate analysis revealed that fixed fee patients have narrower profit margins than fee-for-service patients, and that survivors have lower margins ($3,688 ± 886) than nonsurvivors ($7,236 ± 4880). A longer LOS typically yielded higher margins regardless of reimbursement or morbidity (see Table 4). The one exception to this result was that margins dropped off significantly on average for fixed fee patients whose stays lasted ≥3 weeks. The high standard errors for this subgroup indicate that the negative average margins could have resulted from a small group of highly unprofitable patients.
DISCUSSION
Economic analysis of patient care remains constrained by a relative paucity of accurate, reliable information. Few centers currently have the opportunity to look critically at their true costs associated with patient care, and even fewer data are available to clinicians regarding payer reimbursement and behavior. Moreover, as margins continue to come under pressure from payers, health systems have an increasing need for pertinent economic information.
Our analysis of the entire population reveals that nonsurvivors cost approximately $28,000 more than survivors, but on the whole are more generously reimbursed. In fact, Table 1 demonstrates that the margin for many DRGs is greater for nonsurvivors than survivors. Moreover, considerable variation in individual patient margins is evident by the progressively increasing standard error of the mean within each DRG margin, when comparing nonsurvivors with survivors.
When patients were classified into a fixed fee (DRG, prospective payment) arrangement, and compared with a non-fixed fee arrangement (fee for service) as in Table 2, the data demonstrate that the most complex patients are being transferred into the medical center. Roughly 57% of all transfers have an ISS >15, compared with 21% for patients who are not transferred. Our analysis reveals that although the trauma service rarely incurs losses on fee-for-service patients, negative margins are routine in fixed fee cases. For example, 40.4% of fixed fee transfer patients incur average losses >$2000. The reasons for this are straightforward: fee-for-service reimbursement closely tracks costs, whereas fixed fee reimbursements do not. Moreover, by virtue of having large patient bases, the fixed fee payers (Medicare, Medicaid, Blue Cross/Blue Shield, and the university HMO) can negotiate more favorable terms. Table 2 demonstrates that the margin progressively increases as complexity rises in patients on a noncontracted payment plan of fee for service. Also of note, none of the transfers died. Clinically, this results from the nature of traumatic injury: most patients who survive the first 24 hours will ultimately be discharged alive.
The subgroup analyses (see Tables 3 and 4) reveal significant variations in both the mean profit margin and the standard errors. These analyses raise the possibility that fixed fee payers could use observable patient characteristics and financial considerations to decide where to transfer patients. For example, consider a hypothetical patient in a community hospital many miles from our trauma service. Suppose the patient is insured by a company that has a fixed fee contract with our trauma service (e.g., Blue Cross), and that the insurer knows that the patient will have an LOS that is likely to exceed 3 weeks. The insurance company may then have a strong financial incentive to transfer that patient to our trauma service (even if there are other closer level I centers), because on average it can expect to reimburse the hospital $517 lessthan the actual cost of providing that patient’s care. More generally, insurers have clear financial incentives to transfer their most costly patients within each DRG to hospitals where they have fixed fee contracts and to transfer their least costly patients to hospitals where they have fee-for-service contracts.
This variation in reimbursement and profit margin exposes the service to considerable financial risk. This risk is not just from the obvious fluctuations in overall trauma service profits that such variation can create, but also from the fact that the service’s patient mix could shift adversely. Such a shift could arise spontaneously or by the deliberate actions of individual payers. If, for any reason, the patient mix shifts even slightly from more to less profitable DRGs or patient types, the service’s aggregate margin could drop significantly. It is not unusual among fixed fee patients for losses to mount to $30,000 or more, and losses >$10,000 are relatively routine (see Table 2). If the service were to lose the most profitable 5% of its patient base to other health systems and replace them with an equal number of highly unprofitable patients, its aggregate profits would plummet.
Such a shift is not implausible. The hospital faces stiff competitive forces, and whether or not insurers actually steer patients to rival trauma centers, they can threaten to do so and in the process pressure the hospital to accept lower reimbursements for those DRGs where the hospital’s margins are highest. Moreover, in some cases insurers with fixed fee contracts can steer their highest-cost patients to our service. The fixed fee caps the insurer’s financial exposure and shifts the liability for all costs in excess of the cap over to our trauma service. Conversely, when a potential transfer patient is likely to incur only modest costs, an insurer may be less likely to transfer that patient to a service that levies a substantial fixed fee. In short, the trauma service might receive a disproportionate number of unprofitable patients. The prospects for such “adverse selection” are well known in insurance markets, and they are bolstered in this case by the service’s status as a level I trauma center, willing and able to accept the most severely injured (and therefore highest cost) transfer patients. 1
As the tables in this paper demonstrate, it is often not difficult for the payer at the time of admission to determine whether a patient will incur high costs. It is important to emphasize that to date, there is no clear evidence that this adverse selection occurs systematically. Indeed, Table 2 shows that transfer patients (and more severely injured patients in general) provide higher rather than lower average margins than nontransfer patients, easing some concerns about the potential for such strategic behavior. However, the table also demonstrates that the service loses money on 40% of all fixed fee transfer patients. This suggests that financial considerations may ultimately play a role in some transfer decisions and could become more significant over time, as financial pressures on payers continue to grow.
It is also important to note the importance of the hospital’s transfer center, which would presumably thwart such strategic behavior if it ever arose. Physicians should work closely with these centers to ensure that patients are not being transferred to their trauma services for financial reasons alone. They should also work to preclude any financial prejudice on the transfer center’s part against patients who need care but who are likely to incur costs well in excess of the fixed fee that the payer is obligated to make.
Currently, most if not all surgical services are deficient in their ability to profile patients according to their clinical parameters and relate those data to financial outcomes. The reason for this deficiency is the lack of accurate databases that combine clinical, administrative, and financial data. In contrast, this type of data collection and mining capability is currently available to the payer community. This information pool creates an enhanced ability for the payers to leverage their information into the realm of patient care. The ability to develop, understand, and ultimately manage a portfolio of patients is critical to the longevity and survival of a trauma service.
The original goal of this study was to understand how death affected costs and margins on a trauma service. Interestingly, we have found evidence that potentially allows payers to select patients with a more complex disease process for transfer to certain providers based on their contractual status. Although this is a reasonable risk management process for insurers, it is in reality a form of portfolio management—except in this case, the portfolio consists not of financial instruments, but of patients and their attendant risk. To be clear, the reason for payers to engage in this type of portfolio management is to reduce their risk and optimize their return. 2 As payers develop such portfolio management, trauma centers and health systems will also be forced to develop market strategies that manage risk while continuing to ensure quality patient care.
Discussion
Dr. John J. Ferrara (Detroit, Michigan): I’d like to first thank the authors for a timely submission of their abstract, which sheds further light on an issue that Dr. Taheri and colleagues have spent a great deal of energy addressing, that being whether there yet exists any financial justification at least for maintaining level I trauma centers in the days of shrinking healthcare reimbursement, assuming, of course, that these centers still provide a higher quality of trauma care delivery than would otherwise be available to our citizens.
I won’t reiterate Dr. Taheri’s methodology or results at this time, as his data were clearly presented, but I would encourage you to review his data when it becomes available in published form because it has major implications for the future of all trauma centers.
My take from Dr. Taheri’s data is pretty much in the good news/bad news fashion. First off, within the Michigan health system, at least, trauma still pays, and it actually pays pretty well overall. The bad, but hardly unexpected, news is that reimbursement for care of the fixed-fee patient is considerably less than that given to the fee-for-service patients. Moreover, reimbursement diminishes with hospitalization time, such that about 3 weeks into the patient’s admission, they begin to tip the financial balance in the opposite direction.
So if you look at his data, you can see that reimbursement for dead patients dramatically exceeded that for patients who survived, because I must presume most died within that financially golden initial 3 weeks of hospitalization.
Finally, trauma patients who were transferred from other institutions held a greater profit margin than for nontransfer patients, whether they were fee-for-service or fixed-fee. On the surface, this would appear to be good news insofar as it mutes the concern that trauma centers are already receiving increased numbers of transfers from hospitals who perceive that these patients will be unable to meet their financial obligations.
However, if you simply cull out the fixed-fee patient population and then look at reimbursement depending upon whether or not they were transferred, it is clear while the percent of patients with a negative margin is the same whether or not they were transferred, the percentage of patients who resulted in a large financial burden was much higher in the patients who were transferred when compared to those directly admitted to their facility. I don’t know whether these data in specific are amenable to statistical analysis, but it at least gives us food for thought as capitated care continues to creep into our payer mix.
And so I’d ask Dr. Taheri whether he thinks that we have really reached the stage wherein hospitals may elect to deemphasize the human element of providing quality healthcare for the trauma victim in favor of defining a healthy financial outcome. If so, data such as these may set the tone for administrators trying to determine at an early stage in trauma care which patients will provide a profit margin and keep them, whether or not the surgeon feels comfortable in providing care for that patient, and then look to transfer potential financial drains to trauma centers?
Since Paul is now pursuing his master’s degree in business administration, and therefore may be uniquely qualified to address this issue, I would first ask him to comment as to whether this stage has been or will be reached, and if so, what trauma centers can do about it.
I would also ask him to comment on his payer mix, which apparently has very few self-paying patients. I assume the financial outcome of centers with a high burden of self-pay patients—those which my residents refer to as having had a negative wallet biopsy—would appear to be somewhat less rosy, for want of a better term.
President Griffen: The next discussant will be Dr. Lewis Flint, but in Dr. Flint’s absence, Dr. Bernard M. Jaffe of New Orleans, Louisiana, will present his comments.
Dr. Bernard M. Jaffe (New Orleans, Louisiana): Thanks, Dr. Griffen, Dr. Copeland. While Dr. Griffen is correct that Lew asked that I would discuss the paper since he couldn’t be here, Dr. Griffen should know me well enough to know that this is not distinctly Dr. Flint’s comments only, but has an interjection of some of my own thoughts and philosophy as well:
Dr. Lewis M. Flint, Jr. (New Orleans, Louisiana): I think this is a very important paper also, and I congratulate Dr. Taheri and his colleagues and Dr. Greenfield for performing such an important study. There are certain things that I find remarkable about it. I know there are lots of hospitals in this country that couldn’t provide the cost data that would be required to actually perform the study, and I think there are fewer still who would be willing to give this information out. The data, I think, are inherently dangerous. That is, I think there are some payers who would find that the reimbursements for some of their care are so profitable that when they reassess their negotiations with University of Michigan Hospitals, they may look at this and say, “We are paying too much for some of this care,” and I think that’s a significant risk and one I hope that this paper will not have unleashed. On the other hand, there certainly is some salvation because a lot of the insurers don’t read the scientific literature. This is going to be published in the scientific literature rather than the business literature, so I think there probably is some freedom, and I think the risk is relatively small.
Dr. Flint is concerned about an implication of the data, and I agree with him that there is really a financial reward of certain patients who die or are allowed to die quickly. By extrapolation, of course, that would imply that the most profitable trauma care would be the service that moved the survivors out quickly and let the nonsurvivors die within the first 2 weeks. That means there is a potentially dangerous message, that the sickest patients should then require and be provided with less and less care based on the reimbursement. If we allow portfolio management, as you have called the delivery of care services and its manipulation in this paper, to dictate our care, then I think we really are falling into the category that makes us potentially even worse than the insurers.
I think that our responsibility as physicians is to continue to provide care. And while we have to be very mindful of the financial burden—because if we are not mindful of it, we will be reminded of it—I think our still-primary commitment has to be caring for patients, not caring for their “wallet biopsy.”
One of the implications of the paper that I think is least clear in the manuscript is the suggestion of the importance of the fact that nonsurvivors are more profitable to hospitals than survivors. I have already discussed to some degree what the implications of that comment are. On the other hand, because of the low mortality rate, there are nine times as many survivors as nonsurvivors. And, of course, the financial viability of the trauma service is not the nonsurvivors, but the survivors. And I think we have to keep this in mind because, in fact, that’s really where the action is.
Dr. Flint was relatively concerned that the paper doesn’t stratify mortality into immediate, that is, emergency room, and the operating room, early and later, presumably in the intensive care unit. Such information would be enormously valuable to be able to devise appropriate management strategies which might do such things as be able to prolong the profitability to 30 days, for example, instead of 21, and that would make an enormous difference.
I think these data are important and, I am sure, are obtainable and would provide useful information for those of us who continue to practice trauma care.
I have only one question for Dr. Taheri, and I suspect it is one that will be most difficult for him to answer. This has been a retrospective study. The real question is, has he developed enough information about survival and finances to be able to perform a similar study prospectively? If he can make a prospective study of this kind of information, I think then we will really have revolutionized trauma care in this country.
Dr. Robert S. Rhodes (Philadelphia, Pennsylvania): This study is particularly noteworthy because it measures costs, not charges. Furthermore, these costs should be analyzed by their various components.
I share their concerns about DRGs, but believe there are several points that warrant further consideration. The first is that even though the DRGs are the basis of the prospective payment reimbursement system, they were actually originally developed as a management tool only later adopted by the Federal Government as the basis for reimbursement. And the criticisms of their applicability as a reimbursement system have been longstanding.
Potentially perverse strategies that arise as pointed out in the paper are actually not a product of the DRGs alone but are a function of the heterogeneity of reimbursement systems in our healthcare system, along with the heterogeneity of incentives. Some people have actually cynically questioned whether this heterogeneity and lack of coordination among our healthcare system really then deserves the term of “system.” These points lead to several questions. Would you comment on the relatively large variability of the costs within each of the DRGs and what aspects of cost accounted for this variability, and do you have specific recommendations based on such analysis on how to control such cost?
And, lastly, as a general comment, would you comment on the overall mission of the tertiary medical center being driven by seeking profitable patients versus seeking profitability among the patients such medical centers are uniquely equipped to serve? This, I think, very much relates to Dr. Griffen’s emphasis in his presidential address, in which the concerns and the priorities seem to be running askew.
Dr. Harlan D. Root (San Antonio, Texas): President Griffen, Secretary Copeland, Fellows and Guests. I think this is an excellent analysis of a very difficult problem, both in gaining information from the hospital to elicit costs and payments, but I think that it is long overdue.
I think that the burden of cost of trauma care in the United States has been absorbed into the rest of the healthcare system, and I think it is important that the burden of the costs be sorted out. Because in our state of Texas, although auto insurance is mandatory, only about 50% of people carry it. The minimum liability is $10,000 to $20,000, and the personal injury protection is a minimum of $2000.
So my question to the authors are two:
In your analysis, could you discuss the role of auto insurance contribution to this issue of reimbursement, since Michigan enjoys what is becoming ever more rare: no-fault insurance. And no-fault insurance is vigorously fought by all plaintiffs’ attorneys since it denies what they think is their opportunity to earn a living.
And my second question is, if you can sort out the reimbursement by the auto insurance of Michigan, what proportion of your reimbursement would derive therefrom?
I think this burden of the trauma care cost increases the apparent overall charges that the public resents. And yet, with a well-contained disease entity such as motor vehicle crashes, which I assume must be 95% of the experience at Michigan, I think that it is only right that the auto insurance be adequate to cover the costs which you are so nicely identifying for us.
President Griffen: This is a question for the audience. Today’s newspaper, the USA Today, had on the front page the fact that more physicians are getting MBAs. How many in this audience have MBAs or are thinking about it or are in the process of getting an MBA? Just a show of hands.
That’s interesting. I thought it would be higher than that. I think it’s going to be higher if you ask the same question next year.
One additional comment. “Qualifiers” is a very crass term. I usually call it a “fiscal examination” rather than a physical examination.
Dr. Paul A. Taheri (Closing Discussion): Let me start by addressing some of Dr. Ferrara’s comments. Initially, you commented on the statistical analyses applied here, whether they should be applied. That’s a very difficult question, because when you are dealing strictly with financial numbers, we are not sure what defines economic significance. Although we can apply statistical tests to the numbers, we are not sure what they actually would mean. So we are sort of wrestling with that very issue, and many economists are also unclear in the healthcare field, what is economically significant.
When it gets to the hospital administrators versus the human element of physicians, I would like to make it clear that as physicians, we are looking at all this retrospectively in a post hoc analysis. Of course, at the time of transfer or admission, we know nothing about the patient’s insurance status. And usually we don’t know that for several days. I think this is a very important issue, though, that who probably does know this information in a prospective fashion is in fact the hospital and the administrative milieu that exists.
The fact that we are trying to disseminate this information to physicians, I think, is just the very point we need to do, that we need to become cognizant of this so there are no transfer policies created by the hospital administration that may deflect or refer patients to other health systems or other institutions in the community that may be either differently set up from their cost structure or may have different resources available.
So I think the major message here is that physicians are beginning to get the data, albeit it is somewhat difficult, through various administrative cycles.
As it relates to our self-pay, in our particular population, we are fortunate in that respect. We have about a 94% insured population. It varies a little bit, but basically it’s around 6% to 7% a year, and that has been pretty consistent over the past 6 to 8 years. So our self-pay is limited. We are a suburban trauma center and not an intercity situation.
As it relates to Dr. Jaffe and some of Dr. Flint’s comments, first let me address the issue about publication of this type of data and the publication of margins or costs or reimbursements, because it’s a very important issue for all of us, because many of the hospitals, while some claim they don’t have the data, my suspicion is that actually many of them do. Obviously, the University of Michigan does. And there has been considerable controversy about letting this data out of the institution and what is going to be the long-term sequelae of it and will it be used against us as a negotiating tactic by payers. Obviously, I don’t have the exact answer to that yet because this is sort of the third or fourth paper we have put out on this topic, but we have not seen any negative impact on our reimbursement. In fact, we are tracking that because that has been one of the concerns of the hospital.
Secondarily, I think physicians can no longer afford to work in a black box. We just have to know what’s going on out there. If we are being held accountable for fiscal activity within our services or departments, it is imperative that we begin to have data, to begin to understand how the hospital is set up. And also, as it relates to the margin issue, I think cost data, while ours is a total cost and we have broken it down to the various components of fixed, variable, and indirect, we could discuss the actual cost allocation within the institution probably for a week at least, just to find out where the CEO’s salary goes.
So at this point I think the cost issue is an important one to put out, even though it may not be the exact cost in any institution. As well, I would comment that the costing structures between hospitals are different, so they may be different in Memphis or Atlanta than they are in Michigan. And even within Michigan, many hospitals have different cost structures.
As it relates to portfolio management, Dr. Jaffe’s comment on that, we are not advocating that we would not take care of a patient based on insurance status. Actually, what our position is, I think it is important that we know so that we have an understanding of what kind of resources we will need from a budgeting perspective year to year. And, as well, it also can protect us from the administrator setting up transfer centers which may actually deflect nonpaying or poorly reimbursed patients.
Dr. Rhodes’ question regarding some of the incentives and some of the heterogeneity of the population: there is a large variability in costs within DRGs, and it is precisely for that, because DRG is sort of a wastebasket diagnosis, there are 467 of these, and there is variability by which patients funnel into them.
In fact, polytrauma patients who undergo a tracheostomy, regardless of having a head injury, long bone fractures, or what-have-you, all funnel into the same DRG, which is actually a particularly lucrative DRG for the hospital. So there is variation within each of these DRG populations.
And to quickly address Dr. Root’s comments, I think that the role of auto insurance in Michigan is a pivotal one; it sort of gives us a second-hit theory. What the hospital does is go to the primary insurer first to get a certain percentage of the reimbursement. And once they use up that resource, they move right on to the auto insurer and hit them up for a second piece of the charge for the patient. So we are lucky in that sense in Michigan. And I don’t know the exact number of patients who had no-fault insurance. But, again, our patient population is about 94% blunt, so it is a predominant number of our patient population.
Footnotes
Correspondence: Paul A. Taheri, MD, Division of Trauma, Burn and Emergency Surgery, University of Michigan Medical Center, 1500 E. Medical Center Dr., Ann Arbor, MI 48109-0033.
Presented at the 110th Annual Meeting of the Southern Surgical Association, December 6–9, 1998, The Breakers, West Palm Beach, Florida.
Accepted for publication December 1998.
References
- 1.Milgrom P, Roberts J. Economics, organization, and management. Englewood Cliffs, NJ: Prentice Hall Press; 1991.
- 2.Edwin EJ, Martin G. Modern portfolio theory and investment analysis, 5th ed. New York: John Wiley & Sons; 1995.