Abstract
Objective
To evaluate the influence of the laparoscopic technique in hernia repair regarding time to full recovery and return to work, complications, recurrence rate, and economic aspects.
Summary Background Data
Several studies have shown advantages in terms of less pain and faster recovery after laparoscopic hernia repair, whereas others have not, and the cost-effectiveness has been questioned. The laparoscopic technique must be thoroughly compared with the open procedures before its true place in hernia surgery can be defined.
Methods
Six hundred thirteen male patients aged 40 to 75 years were randomized to the conventional procedure, preperitoneal mesh placed by the open technique, or laparoscopic preperitoneal mesh (TAPP). Follow-up was after 7 days, 8 weeks, and 1 year.
Results
Of 613 patients undergoing surgery, 604 (98.5%) were followed for 1 year. Patients who underwent TAPP gained full recovery after 18.4 days, compared with 24.2 days for open mesh (p < 0.001) and 26.4 days for the conventional procedure (p < 0.001). Patients who underwent TAPP returned to work after 14.7 days, compared with 17.7 days for open mesh (p = 0.05) and 17.9 days for the conventional procedure (p = 0.04). They also had significantly less restriction in physical activities after 7 days. The TAPP procedure was more expensive, mainly as a result of longer surgical time and equipment costs, even after compensation for earlier return to work. Complications were more common in the TAPP group, with a varying pattern between the groups. Four recurrences in the conventional, 11 in the open mesh, and 4 in the TAPP group were recorded after 1 year (p = n.s.).
Conclusion
The laparoscopic technique results in both shorter time to full recovery and shorter time to return to work, at the price of substantially increased costs.
The laparoscopic technique has replaced the open approach in many surgical procedures. This development has largely taken place without desirable preceding studies proving the safety and benefit to the patient. Analyses of the surgical results of laparoscopic cholecystectomy have later confirmed that the method is safe and of benefit to the patient, 1,2 although there has been concern about the increased rate of bile duct injury. 3,4 A recent study shows that the minilaparotomy technique and laparoscopy give comparable results in terms of hospital stay and postoperative recovery after cholecystectomy, 5 and the extent to which the laparoscopic technique per se is responsible for the beneficial results observed has been questioned.
The adoption of laparoscopy in hernia surgery poses special problems. First, will laparoscopic hernia repair show recurrence rates as low as those demonstrated with well-established open methods, both with 6–8 and without 9,10 the use of a prosthetic mesh? Second, can the suggested shorter recovery time and shorter off-work period after laparoscopic hernia repair compensate for the increased expenditure for the extra surgical equipment used and the need for general instead of regional or local anesthesia? Traditionally, in open hernia repair, the off-work time has been fairly long, up to 5 to 6 weeks. The ideal necessary off-work time is largely unknown for many surgical procedures and is influenced by doctors’ opinions, patients’ expectations, and the reimbursement system rather than being based on scientific evidence. 11
The present study was designed to evaluate the laparoscopic technique per se by comparing the laparoscopic procedure with both the open preperitoneal mesh technique and the conventional procedure. The primary aim was to compare the treatment groups regarding time to return to normal physical activity, early recurrence rate, and complications. A secondary aim was to evaluate whether there were any differences regarding consumption of medical resources and time to return to work.
METHODS
The study was a randomized, multicenter, open trial with three treatment arms: conventional procedure, open preperitoneal mesh technique, and laparoscopic preperitoneal mesh (TAPP). The study was conducted at 10 hospitals.
Patients
To be eligible for participation, patients were required to be healthy (American Society of Anesthesiology [ASA] group 1 or 2), male, and 40 to 75 years old, with a unilateral, primary or first-recurrence inguinal hernia. Patients who had an irreducible hernia or needed emergency surgery were not eligible for the study. Other exclusion criteria were bilateral hernia, more than one recurrence, and earlier surgery with mesh in the same groin. Patients with complicating diseases resulting in ASA group 3 or 4, contraindications to laparoscopic hernia repair (e.g., known adherences, former major lower abdominal surgery), or “giant” hernia were also excluded from the study.
Randomization and Stratification
The randomization was computer-generated in blocks of six at the coordinating study center and distributed to each center. Patients were randomized at each center by opening consecutively numbered sealed envelopes. The patients were informed of their treatment assignment when the operation was decided. Patients who during the surgical procedure were converted from TAPP to open surgery were analyzed on an intention-to-treat basis. Stratification was made for primary and recurrent hernia and also for age (40 to 60 years and 61 to 75 years).
Data Handling
Data were recorded in a case record form at each participating center. The forms were collected by the study coordinating center, where the transfer to computer data files and statistical analysis were performed.
Ethics
The study was approved by the Ethics Committees in Gothenburg, Linköping, Lund, Uppsala, Umeå, and Örebro, Sweden. Each patient eligible to participate in the study received written and verbal information about the three surgical techniques. The patients gave their informed consent to be randomly allocated to one of the treatment groups.
Statistics
The main efficacy variables were recurrence rate after 1 year and time to full recovery. A second time-dependent efficacy variable was time to end of sick leave. Other discrete efficacy variables were number of patients fully recovered, number of patients back at work, pain in the treated groin, discomfort from the treated groin restricting normal physical activity, and complications.
The dichotomous (i.e., with “yes” or “no” answers) variables were analyzed with Fisher’s exact test. The response variables “pain in the treated groin” and “discomfort from the treated groin restricting physical activity” were multiple choice questions and were analyzed using the Kruskal-Wallis test for the overall treatment comparison; if this was significant, the Wilcoxon rank sum test was used for the pairwise comparisons.
Time to full recovery and time to end of sick leave were to be analyzed by analysis of variance, with type of procedure and center as factors. Because the data for these parameters did not fulfill the homogeneity assumptions needed for an analysis of variance, the data were transformed to the natural logarithm (ln) of the original time scores. The estimates and confidence intervals (which are recalculated back to antilogarithms) for the different treatment comparisons therefore represent the ratio of the true treatment mean instead of the difference.
Sample Size Calculations
With estimated recurrence rates after 1 year of 10% in the conventional hernia repair group and 2% in both mesh graft repair groups and a test power of 80%, alpha level of 0.05, 162 patients were needed in each group. With the same test power and an estimated time to full recovery of 10 days in the laparoscopic group and 35 days in the two openly operated groups, 24 patients were needed in each group. This was calculated assuming astandard deviation of the difference in time of 30. Therefore, 200 patients in each study group were to be included. No interim analyses of significance were performed.
Surgical Procedures
Conventional, open hernia repair was performed by the technique preferred by the surgeon. Nonresorbable, monofilament suture was to be used for the repair. A tension-relieving incision was used when appropriate.
Open hernia repair with a mesh graft was performed using the preperitoneal approach through a split incision. If necessary to reduce hernia sac contents, the peritoneum was opened. The hernia sac was either excised or reduced and left in situ. A large polypropylene mesh graft (Prolene, Ethicon, Somerville, NJ) measuring 10 × 15 cm was attached to Cooper’s ligament and to the transverse fascia with interrupted nonresorbable monofilament sutures. The mesh was to cover both direct and indirect inguinal and femoral openings and to go well below the ileopubic tract. No sutures were allowed below the ilioinguinal tract lateral to Cooper’s ligament. The wound was closed with interrupted or continuous sutures in the fasciae and interrupted or continuous skin closure.
Laparoscopic hernia repair was done through a transabdominal preperitoneal approach using three ports (12, 10, and 5 mm). The peritoneum was incised above the hernia sac and dissected free, and a large polypropylene mesh graft (Prolene) measuring 10 × 15 cm was placed preperitoneally and attached to Cooper’s ligament and the transverse fascia with titanium staples (EMS Hernia Stapler, Ethicon). No staples were to be placed below the ilioinguinal tract lateral to Cooper’s ligament. The mesh was to cover both direct and indirect inguinal and femoral openings and to go well below the ileopubic tract. The peritoneum was closed with a continuous, resorbable suture or metal staples, aiming at complete peritoneal coverage of the mesh.
In all three groups, the wounds were infiltrated with 0.25% bupivacaine (Marcaine, Astra, Södertälje, Sweden) for postoperative pain relief. In the open surgery groups, 15 ml of bupivacaine was infiltrated along the line of incision, 10 ml at the iliac crest at the ilioinguinal and iliohypogastric nerves, and an additional 15 ml under the external fascia. In the laparoscopic group, the incisions were subcutaneously infiltrated with 5 ml of bupivacaine each.
Patients who received a mesh graft were given flucloxacillin (Heracillin, Astra) 1 g twice daily orally the day of surgery. In case of allergy to penicillin, clindamycin (Dalacin, Upjohn, Kalamazoo, MI) 150 mg four times a day was given orally.
Participating Surgeons
Participating surgeons were required to have performed ≥10 laparoscopic hernia repairs and 5 open mesh repairs before entering the study. For the conventional procedure, the surgeon was free to choose the method.
Anesthesia
Open procedures were performed under regional or general anesthesia in accordance with the patient’s preference or depending on anesthesiologic considerations. The laparoscopic procedure was always performed under general anesthesia.
Hospital Stay
The procedures were performed as outpatient procedures when possible, with admission to the hospital for medical and/or social reasons but also in accordance with the patient’s preference. The study protocol did not stipulate when the procedure was to be performed as an outpatient procedure.
Preoperative and Perioperative Parameters
Before surgery, the following parameters were recorded: age, height, weight, primary or recurrent hernia, history and size of hernia, ASA classification, and type of work (desk work, light manual, heavy manual, or no work). Status regarding testes and inguinal innervation was checked.
Surgical time skin-to-skin, type of hernia, perioperative complications, type of anesthesia, and hospital stay were noted.
Postoperative Follow-Up
Follow-up was performed by the study surgeons at scheduled control visits 7 ± 2 days, 8 ± 1 weeks, and 12 ± 1 months after surgery. The patients were asked whether they had had any pain at rest in the treated groin and also whether the operated groin caused any restrictions of activity. These subjective variables were graded on a Likert scale (none, mild, moderate, severe, maximal). The testes, nerve status, and wound and the presence of a recurrent hernia were examined. Hernia recurrence was defined as a palpable, reducible lump in the treated groin, with or without symptoms. In patients with persistent discomfort, or if full recovery was not achieved at the 8-week visit, extra visits were performed at intervals of 4 weeks until full recovery was noted.
Time to full recovery and to end of sick leave was noted by the patient in a self-administered record form. The time to full recovery was defined as when inguinal discomfort did not interfere with normal daily or athletic activities. In terms of sick leave, the patient received written instructions and was encouraged to return to his normal work as soon as he found himself capable. After the operation, the patient received an off-work certificate for 1 week, if needed. This certificate was renewed at the patient’s request for 1 week at a time by visit or by telephone contact with the patient until he could return to work. There were no other restrictions on physical activity, other than the patient’s own experience of pain and discomfort.
Further evaluation regarding recurrence will be made after 3 years.
Estimation of Costs
Cost differences were calculated by setting the cost of the conventional procedure to zero. To this was added the extra perioperative costs (prosthetic mesh, ports, staplers, operating room) involved in the other two procedures. The total cost difference was obtained by compensating for the difference in the length of sick leave. The sick-leave reimbursement was calculated from a statistical mean value per day off work. The values used are shown in Table 1. Because the type of anesthesia depended not only on the type of procedure but also on the preference of the patient, this variable was not included to the calculations. The inpatient/day surgery ratio was also more dependent on factors that were not related to the procedure and therefore was not counted.
Table 1. FIGURES USED IN COST CALCULATION

100 SEK = approximately $12.50 U.S.)
RESULTS
Patient Flow
From November 1993 to June 1996, 613 patients were randomized into the study by the 10 participating centers. Five hundred ninety patients (96.2%) followed the study according to the protocol. Twenty-three patients (3.8%) did not attend the 1-year visit. Ten of these were interviewed by phone, four did not attend because of earlier recurrence during the study follow-up, three died during the study for reasons not related to the operation, and six were missing.
Preoperative Parameters
The groups were well balanced regarding age, height, weight, ASA classification, and duration and size of hernia. Type of work and reasons for not working (unemployed, sick leave, or retired) were also similar in all three groups. In 11% of the procedures, the operation was performed for a recurrent hernia.
Perioperative Parameters
Perioperative data are shown in Table 2. For conventional hernia repair, the Shouldice procedure dominated (65%), but Bassini (17%) and MacVay (9%) repairs were also performed. In three cases, the TAPP procedure was converted to open surgery (because of obesity, adhesions, and a large hernia with gas leakage). In 27 of the TAPP procedures (13%), it was impossible to cover the mesh graft with peritoneum. Perioperative complications are shown in Table 3.
Table 2. PREOPERATIVE AND PERIOPERATIVE VARIABLES BY TREATMENT GROUP
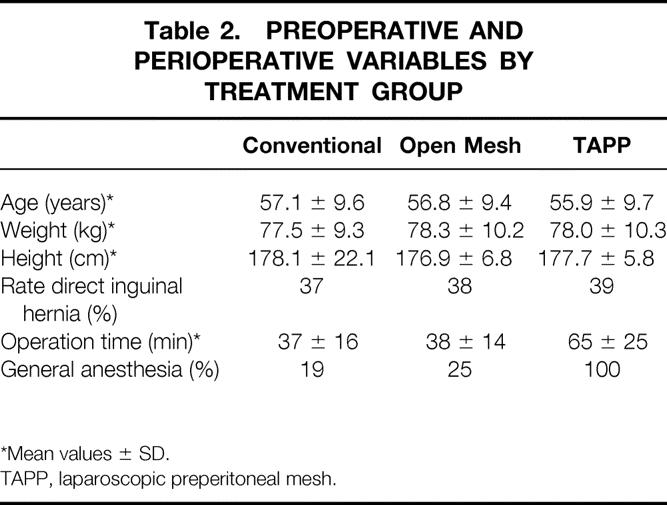
*Mean values ± SD.
TAPP, laparoscopic preperitoneal mesh.
Table 3. COMPLICATION
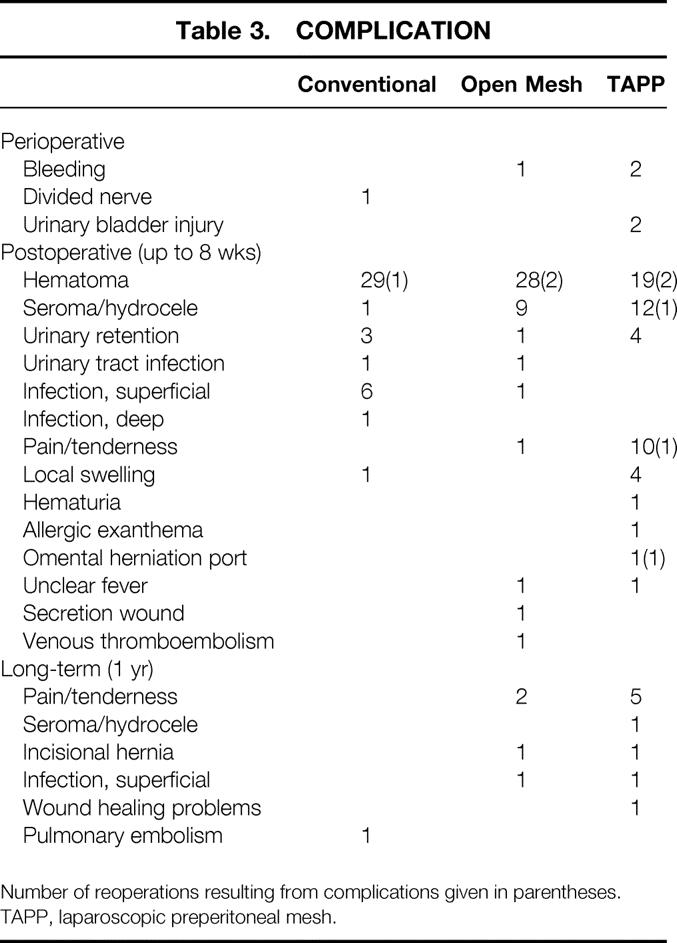
Number of reoperations resulting from complications given in parentheses.
TAPP, laparoscopic preperitoneal mesh.
Postoperative Parameters
Time to Full Recovery
The mean time to full recovery was significantly less in the TAPP group (18.4 days), compared both with the open mesh group (24.2 days, p < 0.001) and the conventional group (26.4 days, p < 0.001) (Table 4).
Table 4. POSTOPERATIVE PARAMETERS

* p < 0.001 vs. conv. (95% CI for ratio 1.23–1.67) and open (1.12–1.53).
† p < 0.05 vs. conv (1.01–1.38) and open (1.00–1.39).
‡ p < 0.05 vs. conv.
∥ p < 0.001 vs. conv and p < 0.05 vs. open.
¶ No statistical analyses performed.
TAPP, laparoscopic preperitoneal mesh.
Return to Work
The mean sick leave period was significantly less in the TAPP group (14.7 days), compared both with the open mesh group (17.7 days, p = 0.05) and the conventional group (17.9 days, p = 0.04). A significant center effect (p = 0.05) was found for this variable, but there were no signs of a treatment-by-center interaction effect—in other words, the pattern of treatment effect was similar in all centers. After 7 days, 26.5% of the patients in the TAPP group were back at work, compared with 15.5% (p = 0.03) in the open mesh group and 9.3% (p < 0.001) in the conventional group (see Table 4). At the 8-week visit, 98.6% in the TAPP group, 96.7% in the open group, and 99.2% in the conventional group were back at work (p = n.s.).
Pain at Rest
Subjective pain at rest in the treated groin at the 7-day visit did not differ significantly among the groups (Table 5). At the 8-week visit, the patients in the open mesh group reported more pain than those in the TAPP group (p = 0.02).
Table 5. PERCENTAGE OF PATIENTS BY SEVERITY OF PAIN IN THE TREATED GROIN AT THE 7-DAY VISIT
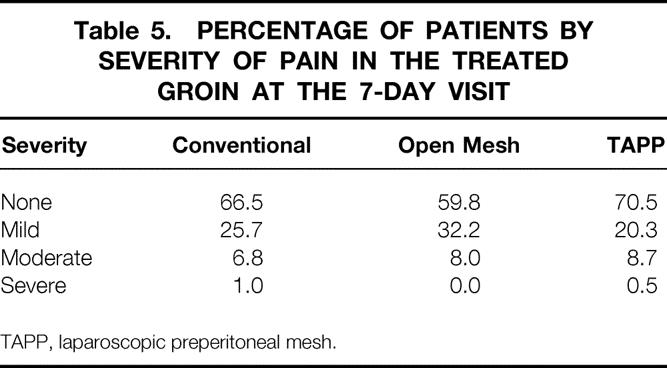
TAPP, laparoscopic preperitoneal mesh.
Restriction of Physical Activity
There were significant differences among the groups in terms of restriction of physical activity at the 7-day visit: 19.4% in the conventional group, 28.5% in the open mesh group, and 40.9% in the TAPP group reported no restriction. These differences are statistically significant when comparing TAPP with open mesh (p = 0.04), TAPP with conventional (p < 0.001), and open mesh with conventional hernioplasty (p = 0.03) (Table 6). The corresponding figures at 8 weeks were 96.9%, 93.2%, and 96.0%, respectively (p = n.s.).
Table 6. PERCENTAGE OF PATIENTS BY SEVERITY OF DISCOMFORT FROM THE TREATED GROIN RESTRICTING PHYSICAL ACTIVITY AT THE 7-DAY VISIT

* p = 0.03 vs. conv.
† p < 0.001 vs. conv. and p = 0.04 vs. open.
TAPP, laparoscopic preperitoneal mesh.
Postoperative Complications
Postoperative complications noted at the 7-day and 8-week visits and at the 1-year follow-up are shown in Table 3.
Recurrence
The total number of recurrences during the first year was 19 (3%) (see Table 4). Ten of the recurrences (8/11 open mesh and 2/4 TAPP) occurred during the first 6 months. In 3 (16%) of the 19 cases, the operation was performed for a recurrent hernia.
Cost Estimation
The perioperative cost was by definition zero for the conventional procedure, 417 krona (SEK; 100 SEK = approximately $12.50 U.S.) for open mesh, and 7063 SEK for TAPP. The total costs, taking into account the reduction of the cost to society for sick leave, were 0 SEK, 350 SEK, and 5988 SEK, respectively. When using reusable ports, the total TAPP cost would be 3483 SEK.
DISCUSSION
The ideal method of hernia repair would cause minimal discomfort to the patient, both during the surgical procedure and in the postoperative course. It would be technically simple to perform and easy to learn, would have a low rate of complications and recurrence, and would require only a short period of convalescence. Finally, cost-effectiveness is important. Does laparoscopic hernia repair meet these demands better than open methods?
First, it is difficult to know with what we compare. The results from specialized centers are often good. Low recurrence rates have been reported with the Shouldice technique, 12 even <1%. 9,10 Other authors have reported higher recurrence rates (approximately 6%) when using the same method, however. 13,14 Series using various mesh techniques have also shown good results. The tension-free hernioplasty introduced by Lichtenstein was used in 1000 consecutive patients with no recurrence after 1 to 5 years of follow-up. 6 A series of 1011 mesh hernia plug repairs with a recurrence rate of 0.2% was presented by Rutkow and Robbins. 15 Stoppa et al used a large prosthetic mesh introduced through the preperitoneal route, also with favorable recurrence rates. 8 It can be assumed, however, that there exists a publication bias and that the results in the general surgical community are not as good. This is confirmed by results from a Swedish prospective registration in eight hospitals, where 17% of the hernia operations were performed for recurrent hernia. 16
It has been claimed that the Shouldice procedure should be the gold standard when evaluating new herniorrhaphy methods. 14 Against this can be argued that there is a learning curve for this procedure. 17 The present study was designed to mimic clinical reality in general surgery, and the conventional method was therefore not standardized, and no specialized hernia centers participated in the study.
Most laparoscopic hernia studies compare laparoscopic mesh procedures with open procedures without mesh. This might lead to difficulties when analyzing to what extent the laparoscopic technique or the prosthetic mesh influences the results. In the present study, the mesh placement was exactly the same in the open and laparoscopic procedures; this design makes it possible to evaluate the role of the minimal access trauma itself for the outcome of the hernia repair. A nonrandomized comparison of TAPP with the open preperitoneal mesh method by Goodwin and Traverso found similar short-term outcomes in the groups but increased cost and complication potential for the TAPP procedure. 18
The results of the present study show a significantly shorter sick-leave period and shorter time to full recovery in the TAPP group than in the open groups. This is in line with earlier published randomized series. 19–28 However, there are also randomized studies that have not shown this favorable shortening of postoperative recovery with the laparoscopic technique. 29–32
A possible bias source is the positive expectations by patients about new techniques, as well as the fact that the study surgeons themselves were responsible for the follow-up. To avoid this, a study with a double-blind design would be needed.
The definition of “normal activity” probably varies between different studies, and therefore the time to return to normal activity is difficult to compare from one study to another. The sick-leave period in our study was fairly long in all groups. This might reflect a tradition in Sweden of long (up to 6 to 8 weeks) sick-leave periods after hernia surgery. Although written information with encouragement to return to work as soon as possible was given to every patient, we assume that the patients in the study were well aware of this tradition. Similar results have been found in other studies. 21,22
Recurrences were more common in the open mesh group, although the difference was not statistically significant. The large proportion of early recurrences (i.e., within 6 months) might reflect technical errors. In this study, both the patients in the open mesh and TAPP groups suffered the drawback of being operated on during the learning curve.
The complication pattern varied among the groups. Seroma and hydrocele were more common in the mesh groups. The chronic pain problems seen in the TAPP group, even after 1 year, were alarming, and this issue needs to be studied further.
The total extra cost for TAPP versus the conventional procedure was calculated to be 5988 SEK. Even when performed with reusable ports, the TAPP procedure carries higher perioperative costs. Much of the extra cost is attributable to the longer duration of the surgical procedure, which can be expected to decrease with increasing experience.
Hernia repair is one of the most commonly performed surgical procedures: approximately 600,000 procedures are performed annually in the United States. 15 In Sweden, 20,376 hernia procedures were registered in 1992 and 16,598 in 1995. 33 A change in the cost for these procedures, therefore, has a large economic impact on society.
Is the additional cost for TAPP outweighed by the shorter sick-leave period? In our study, the laparoscopic technique resulted in shorter time to return to work, but not short enough to compensate for the increased perioperative cost. Different health care and social reimbursement systems, as well as calculations that include reduced production, may produce other results. In this study, a difference of 21 days in time to return to work between TAPP and conventional procedures would be needed to compensate for the extra perioperative cost in the TAPP group compared with those treated with the conventional technique.
A main determinant of cost-effectiveness is the recurrence rate. It has been suggested that recurrences after prosthetic mesh repair appear early after surgery, in contrast to conventional repair, where recurrences appear later in the postoperative course. 21 If this is true, an increased recurrence rate for the conventional group might be expected in time. A high rate of recurrence and subsequent need for reoperation will rapidly consume other advantages to the patient and society. In this study, the patients will be followed up to 3 years, and these long-term results will be published subsequently.
To summarize, it is of great importance that the laparoscopic technique in hernia surgery be thoroughly evaluated before considering it as one of the standard procedures for hernia surgery. In this study, we found substantial advantages for the laparoscopic approach in terms of both time to return to work and to full recovery. However, the method has clear drawbacks: longer operating time, increased costs, and the need for general anesthesia. The complication potential, not the least of which is long-term pain, is worrying. In the future, individual evaluation will probably become more important to determine the most suitable hernia procedure for each patient.
Acknowledgments
The authors thank: the other surgeons in the study: Kai Melén, Värnamo sjukhus, Värnamo; Jörn Holm, Sandvikens sjukhus, Sandviken; Börje Bergman, Ludvika lasarett, Ludvika; Bjarne Rye, Bodens lasarett, Boden; Anders Falk, Östra sjukhuset, Göteborg; Gunnar Henriksson, Kärnsjukhuset, Skövde; and Leif Hoffman, Torsby lasarett, Torsby, all in Sweden; secretary Mayvor Bryngelsson, for skillful handling of paperwork and data management; the staff at the hospitals for their enthusiastic work during the trial; and last but not least, all patients for their willingness to participate in the study.
Footnotes
Correspondence: Bo Johansson, Dept. of Surgery, Norra Älvsborgs Länssjukhus, S-461 85 Trollhättan, Sweden.
Supported by grants from the County of Älvsborg Research and Development Foundation, the Bröderna Eriksson Research Fund, Ethicon, and Astra Pain Control AB.
Accepted for publication February 26, 1999.
References
- 1.Trondsen E, Reiertsen O, Andersen OK, Kjaersgaard P. Laparoscopic and open cholecystectomy. A prospective randomized study. Eur J Surg 1993; 159: 217–221. [PubMed] [Google Scholar]
- 2.Sarli L, Pietra N, Sansebastiano G, et al. Reduced postoperative morbidity after elective laparoscopic cholecystectomy: stratified matched case-control study. World J Surg 1997; 21 (8): 872–878. [DOI] [PubMed] [Google Scholar]
- 3.Adamsen S, Hansen O, Funch-Jensen P, et al. Bile duct injury during laparoscopic cholecystectomy: A prospective nationwide series. J Am Coll Surg 1997; 184 (6): 571–578. [PubMed] [Google Scholar]
- 4.Richardson M, Bell G, Fullarton G. Incidence and nature of bile duct injuries following laparoscopic cholecystectomy: An audit of 5913 cases. West of Scotland Laparoscopic Cholecystectomy Audit Group. Br J Surg 1996; 83 (10): 1356–1360. [DOI] [PubMed] [Google Scholar]
- 5.Majeed AW, Troy G, Nicholl JP, et al. Randomised, prospective, single-blind comparison of laparoscopic versus small-incision cholecystectomy. Lancet 1996; 347: 989–994. [DOI] [PubMed] [Google Scholar]
- 6.Lichtenstein IL, Shulman AG, Amid PK, Montllot MM. The tension-free hernioplasty. Am J Surg 1989; 157: 188–193. [DOI] [PubMed] [Google Scholar]
- 7.Amid PK, Shulman AG, Lichtenstein IL. Open “tension-free” repair of inguinal hernias: The Lichtenstein technique. Eur J Surg 1996; 162: 447–453. [PubMed] [Google Scholar]
- 8.Stoppa RE, Rives JL, Warlaumont CR, et al. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am 1984; 64: 269–285. [DOI] [PubMed] [Google Scholar]
- 9.Glassow F. Inguinal hernia repair using local anaesthesia. Ann R Coll Surg Eng 1984; 66: 382–387. [PMC free article] [PubMed] [Google Scholar]
- 10.Devlin HB, Gillen PHA, Waxman BP, MacNay RA. Short-stay surgery for inguinal hernia: Experience of the Shouldice operation, 1970–1982. Br J Surg 1986; 73: 123–124. [DOI] [PubMed] [Google Scholar]
- 11.Majeed AW, Brown S, Williams N, et al. Variations in medical attitudes to postoperative recovery period. Br Med J 1995; 311: 296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paul A, Troidl H, Williams JI, et al. Randomized trial of modified Bassini versus Shouldice inguinal hernia repair. Br J Surg 1994; 81: 1531–1534. [DOI] [PubMed] [Google Scholar]
- 13.Panos RG, Beck DE, Maresh JE, Harford FJ. Preliminary results of a prospective randomized study of Cooper’s ligament versus Shouldice herniorrhaphy technique. Surg Gynecol Obstet 1992; 175: 315–319. [PubMed] [Google Scholar]
- 14.Hay J-M, Boudet M-J, Fingerhut A, et al. Shouldice inguinal hernia repair in the male adult: The golden standard? A multicenter controlled trial in 1578 patients. Ann Surg 1995; 222: 719–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rutkow IM, Robbins AW. “Tension-free” inguinal herniorrhaphy: A preliminary report on the mesh plug technique. Surgery 1993; 114: 3–8. [PubMed] [Google Scholar]
- 16.Nilsson E, Kald A, Anderberg B, et al. Hernia surgery in a defined population: A prospective three-year audit. Eur J Surg 1997; 163: 823–829. [PubMed] [Google Scholar]
- 17.Kingsnorth AN, Gray MR, Nott DM. Prospective randomized trial comparing the Shouldice technique and plication darn for inguinal hernia. Br J Surg 1992; 79: 1068–1070. [DOI] [PubMed] [Google Scholar]
- 18.Goodwin JS, Traverso LW. A prospective cost and outcome comparison of inguinal hernia repairs. Laparoscopic transabdominal preperitoneal versus open tension-free preperitoneal. Surg Endosc 1995; 9: 981–983. [DOI] [PubMed] [Google Scholar]
- 19.Stoker DL, Spiegelhalter DJ, Singh R, Wellwood JM. Laparoscopic versus open inguinal hernia repair: Randomised prospective trial. Lancet 1994; 343: 1243–1245. [DOI] [PubMed] [Google Scholar]
- 20.Payne JJH, Grininger LM, Izawa MT, et al. Laparoscopic or open inguinal herniorrhaphy? A randomized prospective trial. Arch Surg 1994; 129: 973–981. [DOI] [PubMed] [Google Scholar]
- 21.Liem MSL, van der Graaf Y, van Steensel C, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med 1997; 336: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 22.Kald A, Anderberg B, Carlsson P, et al. Surgical outcome and cost-minimisation analyses of laparoscopic and open hernia repair: A randomised prospective trial with one-year follow-up. Eur J Surg 1997; 163: 505–510. [PubMed] [Google Scholar]
- 23.Tschudi J, Wagner M, Klaiber C, et al. Controlled multicenter trial of laparoscopic transabdominal preperitoneal hernioplasty vs. Shouldice herniorrhaphy. Early results. Surg Endosc 1996; 10: 845–847. [DOI] [PubMed] [Google Scholar]
- 24.Vogt DM, Curet MJ, Pitcher DE, et al. Preliminary results of a prospective randomized trial of laparoscopic onlay versus conventional inguinal herniorrhaphy. Am J Surg 1995; 169: 84–90. [DOI] [PubMed] [Google Scholar]
- 25.Leibl B, Daubler P, Schwarz J, et al. Standardized laparoscopic hernioplasty vs. Shouldice repair. Results of a randomized comparative study. Chirurgie 1996; 67: 465–466. [PubMed] [Google Scholar]
- 26.Champault G, Rizk N, Catheline JM, et al. Inguinal hernia. Preperitoneal laparoscopic surgery vs. the Stoppa procedure. A prospective randomized trial: 100 cases. J Chir (Paris) 1996; 133: 274–280. [PubMed] [Google Scholar]
- 27.Heikkinen T, Haukipuro K, Leppälä J, Hulkko A. Total costs of laparoscopic and Lichtenstein inguinal hernia repairs: A randomized prospective study. Surg Laparosc Endosc 1997; 7: 1–5. [PubMed] [Google Scholar]
- 28.Hauters P, Meunier D, Urgyan S, et al. Prospective controlled study comparing laparoscopy and the Shouldice technique in the treatment of unilateral inguinal hernia. Ann Chir 1996; 50: 776–781. [PubMed] [Google Scholar]
- 29.Lawrence K, Mc Whinnie D, Goodwin A, et al. Randomised controlled trial of laparoscopic versus open repair of inguinal hernia: Early results. Br Med J 1995; 311: 981–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bessell JR, Baxter P, Riddell P, et al. A randomized controlled trial of laparoscopic extraperitoneal hernia repair as a day surgical procedure. Surg Endosc 1996; 10: 495–500. [DOI] [PubMed] [Google Scholar]
- 31.Barkun JS, Wexler MJ, Hinchley EJ, et al. Laparoscopic versus open inguinal herniorrhaphy: Preliminary results of a randomized controlled trial. Surgery 1995; 118: 703–709. [DOI] [PubMed] [Google Scholar]
- 32.Schrenk P, Woisetschlager R, Rieger R, Wayand W. Prospective randomized trial comparing postoperative pain and return to physical activity after transabdominal preperitoneal, total preperitoneal or Shouldice technique for inguinal hernia repair. Br J Surg 1997; 83: 728–729. [DOI] [PubMed] [Google Scholar]
- 33.Kald A. Audit of groin hernia repair. Thesis, University of Linköping, Sweden, 1997.


