Abstract
Objective
Length of stay (LOS) is an important outcome as a marker of resource consumption. Determining which factors increase LOS may provide information on reducing costs and improving the delivery of care. The purpose of this study was to determine the independent association of intraoperative process of care and postoperative events with prolonged LOS after adjusting for preoperative severity of illness in patients undergoing major elective surgery.
Methods
Cases representing 11 elective operations from the National VA Surgical Quality Improvement Program were analyzed using multivariate logistic regression analysis. The outcome, prolonged LOS, was defined as an LOS greater than or equal to the 75th percentile (in days) for each operation. Hierarchical modeling was used to assess the independent association of groups of variables (preoperative patient characteristics, intraoperative process of care, and postoperative adverse events) with prolonged LOS.
Results
For the 11 operations explored, there were 23,919 cases. Common preoperative variables associated with prolonged LOS were functional status, American Society of Anesthesiology class, and age. The most predictive intraoperative and postoperative variables included intraoperative blood transfusion, operative time, return to the operating room, and the number of complications after surgery.
Conclusions
Prolonged LOS is associated with preoperative, intraoperative, and postoperative factors. Although preoperative factors were independently associated with a prolonged LOS, the factors generating the highest risks for a prolonged LOS were the intraoperative process of care and postoperative adverse events. To reduce costs, efforts should be made to improve the intraoperative process of care and to minimize postoperative complications.
The health care system has received much attention in recent years as efforts are made to reduce costs while maintaining or improving the quality of care. 1–5 Studying outcomes has been one method of evaluating health care delivery. One commonly measured outcome of interest is length of stay (LOS). 6 Patients with a prolonged LOS have substantially increased resource consumption. 7 Several studies have addressed the risk factors for poor outcomes for surgical conditions, with emphasis on cardiac surgery. 8–15 Because surgical services represent approximately 40% of all hospital expenses, and elective operations are far more common than emergent operations, 16 it is important to study further those factors related to poor outcomes in elective noncardiac surgery. Identifying which factors are associated with prolonged LOS for elective surgery will provide information on how to improve the delivery of perioperative care and reduce costs.
The association between preoperative factors such as age, American Society of Anesthesiology (ASA) Physical Status Score, functional status, and coexistent illness and prolonged LOS has been previously studied. 17,18 The relation of postoperative complications to LOS has also been studied. 19 Few studies have assessed the independent association of intraoperative process of care and postoperative adverse events with prolonged LOS. We hypothesized that after adjustment for preoperative patient risk factors, intraoperative process of care and postoperative adverse events are important predictors of prolonged LOS after major elective surgery.
METHODS
Data Source
The National VA Surgical Quality Improvement Program (NSQIP), a prospective, multicenter, observational study of risk-adjusted surgical outcomes, provided data for this study. Phase I of the NSQIP included 44 academically affiliated Veterans Affairs medical centers (VAMCs) performing cardiac and noncardiac surgery between October 1, 1991, and December 31, 1993. Phase II included all 123 VAMCs performing major surgery in the Veterans Health Administration (VHA) between January 1, 1994, and August 31, 1995. All operations performed under general, spinal, and epidural anesthesia were eligible for inclusion. Operations were excluded if the patient had been entered into the study for another index procedure within the previous 30 days, or had an operation of known low morbidity and mortality rates (e.g., certain ophthalmologic procedures). Because of large numbers, transurethral prostatectomies (TURP) and transurethral resection of the bladder were sampled. NSQIP data collection procedures have been described elsewhere in detail. 20–22
Definition of Elective Surgery and Operations Studied
The purpose of this study was to determine perioperative factors that may prolong LOS after elective major noncardiac surgery. Elective operations common in both VHA and nonfederal hospitals were chosen for study. Five surgical specialties (general surgery, urology, orthopedic surgery, vascular surgery, and neurosurgery) were selected. The most prevalent operations in these surgical specialties performed on an elective basis included open cholecystectomy, laparoscopic cholecystectomy, partial colectomy, TURP, radical prostatectomy, total knee replacement, total hip replacement, lumbar laminectomy, nonruptured abdominal aortic aneurysm repair, femoral popliteal revascularization, and carotid endarterectomy. Current Procedural Terminology-4 coding (CPT-4) was used to identify all operations.
Case Inclusion
All operations performed on patients aged 18 or older with the identified CPT-4 codes were eligible for inclusion.
Case Exclusion
To exclude operations that were not performed electively, all operations designated as emergency (operation that must be performed as soon as possible and no longer than 12 hours after admission or after the onset of related symptomatology) were excluded. Patients who were ventilator-dependent or ASA class 5 were excluded because they are unlikely to undergo elective surgery.
Definition of Dependent Variable: Prolonged Postoperative LOS
Postoperative LOS was defined as the time from the date of the index operation to the date of discharge, transfer to a subacute service, or death, whichever came first. The outcome of interest was prolonged LOS, defined as an LOS greater than or equal to the 75th percentile for LOS for each operation, including the day of discharge. Twenty-five percent or more of patients undergoing each operation remained in the hospital on or after this day.
Definition of Independent Variables
Preoperative Variables
Patient sociodemographics were assessed, including age as a categorical variable (18 to 29, 30 to 39, 40 to 49, 50 to 59, 60 or older) and race (Hispanic white, Hispanic black, American Indian or Alaska Native, black not of Hispanic origin, Asian or Pacific Islander, or white). Preoperative patient characteristics included diabetes requiring either oral agent or insulin treatment; hypertension requiring medication; smoking within 2 weeks before admission; myocardial infarction within the previous 6 months; history of congestive heart failure within 1 month of surgery; history of chronic obstructive pulmonary disease resulting in one or more of the following: 1) functional disability, 2) hospital admission in the past for treatment of chronic obstructive pulmonary disease requiring chronic bronchodilator therapy, and/or an FEV1 <75% of predicted; history of a transient ischemic attack; history of a cerebrovascular accident (embolic, thrombotic, hemorrhagic) with residual motor, sensory, or cognitive deficit; drug addiction, defined as a history of recreational or narcotic substance abuse; impaired sensorium, defined as a patient who is acutely confused and/or delirious and responds to verbal and/or mild tactile stimulation; weight loss of >10% body weight in the previous 6 months; ethanol abuse of greater than two drinks per day in the 2 weeks before admission; history of claudication; and functional status, categorized in three levels depending on the patient’s ability to carry out activities of daily living (fully independent, partially dependent, or totally dependent). Patients who were partially or fully dependent were compared with patients who were independent. ASA class, a five-point assessment of the patient’s physical condition conducted by the anesthesiologist immediately before surgery, was also collected. For this study, patients who were class 3 (systemic illness with definite functional limitations) or class 4 (severe systemic disease that is a constant threat to life) were compared with patients who were class 2 (systemic illness with mild functional limitations) and class 1 (healthy) patients.
Intraoperative Variables
The length of the operation was defined as the time from the first incision to wound closure. Intraoperative blood transfusion was defined as one or more units of packed red blood cells or whole blood infused while the patient was in the operating room. A transfusion begun in the operating room but completed once the patient left the operating room was included. Type of anesthesia included general, spinal, or epidural.
Postoperative Variables
Bleeding was defined as requiring greater than four units of packed red blood cells or whole blood transfusions within 30 days after surgery. Systemic sepsis was defined as an acutely ill febrile patient with an elevated white cell count, along with at least one positive blood culture. Urine infection, superficial and deep wound infections, and pneumonia were all defined according to the Centers for Disease Control definitions of nosocomial infections. 23
Deep vein thrombosis was defined as the formation, development, or existence of a blood clot or thrombus within the vascular system, which may be coupled with inflammation. The diagnosis was made by the surgeon and confirmed by venogram. Cerebrovascular accident was defined as the development of an embolic, thrombotic, or hemorrhagic vascular accident or stroke with motor, sensory, or cognitive dysfunction that persisted for ≥24 hours.
Return to the operating room was defined as all surgical procedures that required the patient to be taken to the operating room for intervention of any kind within 30 days of the index procedure.
Two variables were created within the dataset, one of which designated a patient having at least 1 of 21 predefined postoperative complications within 30 days of the index procedure. The 21 possible complications were pneumonia, superficial wound infection, deep wound infection, wound dehiscence, unplanned intubation, pulmonary embolus, failure to wean from the ventilator 48 hours after surgery, progressive renal insufficiency, renal failure requiring dialysis, urinary tract infection, cerebrovascular accident, comatose for >24 hours, peripheral neurologic deficit, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, pulmonary edema, prolonged ileus, bleeding requiring more than four units of packed red blood cells, graft failure, deep vein thrombosis, or systemic sepsis. The other variable summed the total number of postoperative complications for each operation. For this study, this variable was analyzed as two, two or more, three or more, or four or more complications and their association with prolonged LOS.
Statistical Analysis
The univariate relation between each perioperative factor and prolonged LOS was tested using the Student’s t test for continuous variables and chi square analysis for categorical variables, with a criterion of p ≤ 0.05. To avoid unstable estimates of the risk for a prolonged LOS and to look at clinically relevant factors, a variable had to be present in >1% of the patients undergoing each operation. To model the risk factors for prolonged LOS, the variables were entered into a multivariate logistic regression model with forward selection and backward elimination with a criterion of p ≤ 0.05. Once the models were formed, the variables were separated into perioperative groups according to the hierarchical order in which they were expected to occur in the process of patient care: 1) preoperative patient factors, sociodemographics, and comorbidities, 2) operative factors, 3) postoperative adverse events, including individual complications, return to the operating room, and the number of postoperative complications, as defined above. The models were then run entering groups of variables in the above order. Each step of entering a set of variables entailed controlling for the effects of variables retained from previous steps, with a resultant c-index at each step. The final model was adjusted for years 1992 and 1993 to adjust for an expected decline in LOS in the years after 1991. Testing of the predictive validity of the models (discrimination) was obtained using the c-index. 24 Phase II was used for cross-validation of phase I models by assessing the resultant discrimination (c-index) within phase II.
RESULTS
Patient Characteristics
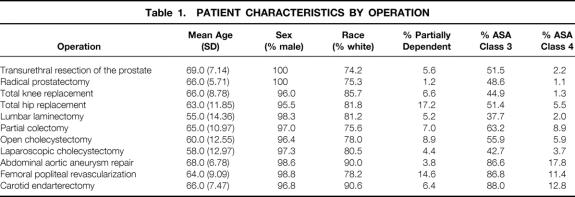
The range of the mean ages was 55 to 69 years of age. The lowest mean ages were among patients undergoing a lumbar laminectomy (55.0 ± 14.4 years) and laparoscopic cholecystectomy (58.0 ± 12.9 years). The highest mean ages were among patients undergoing TURP (69.0 ± 7.1 years) and abdominal aortic aneurysm repair (68.0 ± 6.8 years). Almost all (97.9%) of the patients were men, and 78.5% were white (Table 1 ). Almost 5% of the patients undergoing total hip replacement were women. Among all 11 operations, most patients were ASA class 2 through 4; few were class 1 (0.2% to 9%). Eighty-one percent to 99% of the patients were independent in activities of daily living.
Table 1. PATIENT CHARACTERISTICS BY OPERATION
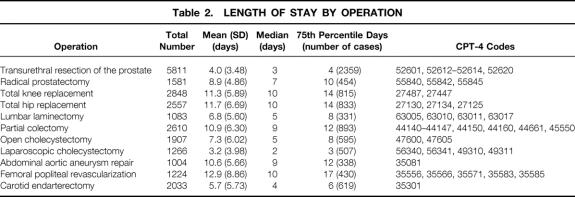
Elective Operations and LOS
There were 23,919 cases among the 11 elective operations, with 8174 cases of prolonged LOS (Table 2 ). The most prevalent operation was TURP (n = 5811). Prolonged LOS was 4 days for TURP, 10 days for radical prostatectomy, 14 days for total knee replacement, 14 days for total hip replacement, 8 days for lumbar laminectomy, 12 days for partial colectomy, 8 days for open cholecystectomy, 3 days for laparoscopic cholecystectomy, 12 days for abdominal aortic aneurysm repair, 17 days for femoral popliteal revascularization, and 6 days for carotid endarterectomy (see Table 2).
Table 2. LENGTH OF STAY BY OPERATION
The mean length of the operation was 1.2 hours (± 0.79) for TURP, 4.1 hours (± 1.42) for radical prostatectomy, 2.9 hours (± 1.07) for total knee replacement, 3.1 hours (± 1.48) for total hip replacement, 3.1 hours (± 1.64) for lumbar laminectomy, 3.4 hours (± 1.52) for partial colectomy, 2.5 hours (± 1.25) for open cholecystectomy, 2.2 hours (± 1.12) for laparoscopic cholecystectomy, 4.2 hours (± 1.59) for abdominal aortic aneurysm repair, 5.1 hours (± 1.90) for femoral popliteal revascularization, and 2.7 hours (± 1.08) for carotid endarterectomy.
Multivariate Predictors of Prolonged LOS
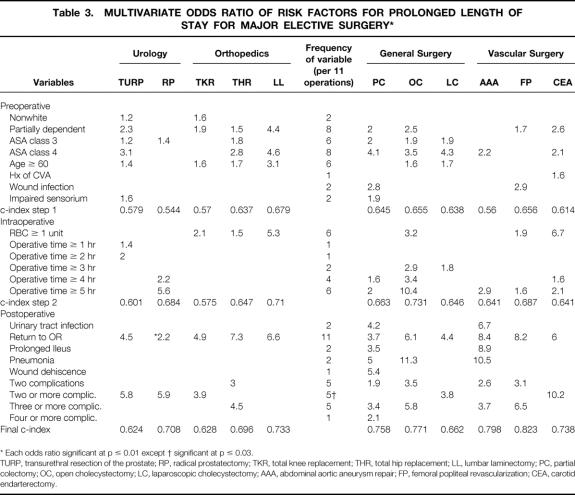
Twenty-three variables were found to be associated with a prolonged LOS for all 11 operations (Table 3 ). Variables that were present in 2 or more of the 11 models were nonwhite race, partially dependent functional status, ASA class 3, age older than 60 years, intraoperative blood transfusion, operative time of 3 or more hours, postoperative urinary tract infection, return to the operating room, postoperative ileus, postoperative pneumonia, two or more complications, and three or more complications. For several operations—TURP, radical prostatectomy, total hip replacement, laparoscopic cholecystectomy, femoral popliteal revascularization, and carotid endarterectomy—individual postoperative complications with the exception of return to the operating room were not significant in the model but were among the variables captured in the number of postoperative complications significantly associated with a prolonged LOS.
Table 3. MULTIVARIATE ODDS RATIO OF RISK FACTORS FOR PROLONGED LENGTH OF STAY FOR MAJOR ELECTIVE SURGERY*
* Each odds ratio significant at p ≤ 0.01 except † significant at p ≤ 0.03.
TURP, transurethral resection of the prostate; RP, radical prostatectomy; TKR, total knee replacement; THR, total hip replacement; LL, lumbar laminectomy; PC, partial colectomy; OC, open cholecystectomy; LC, laparoscopic cholecystectomy; AAA, abdominal aortic aneurysm repair; FP, femoral popliteal revascularization; CEA, carotid endarterectomy.
Table 4 presents the percentage of complications for cases with and without a prolonged LOS that was significant in the model. In all instances, the percentage of complications was much greater for cases with versus without prolonged LOS.
Table 4. FREQUENCY OF SELECTED ADVERSE EVENTS AND RETURN TO THE OPERATING ROOM FOR CASES WITH AND WITHOUT PROLONGED LENGTH OF STAY
* Adverse events that were not present in the final model for each operation.
Urology
For TURP, prolonged LOS was statistically significantly associated with the preoperative factors of nonwhite race, partially dependent functional status, ASA class 3, ASA class 4, impaired sensorium, and age 60 years or older, with a c-index of 0.579. Statistically significant intraoperative factors associated with a prolonged LOS were operative time of 1 to 1:59 hours and 2 to 2:59 hours, with a resultant c-index of 0.601. The addition to the model of the postoperative variables—return to the operating room and the number of complications—resulted in a final c-index of 0.624. The factor with the highest odds ratio (OR) was the presence of two or more complications (OR 5.8, 95% confidence interval [CI] 2.6 to 12.8).
For radical prostatectomy, the preoperative factor significantly associated with prolonged LOS was ASA class 3, with a c-index of 0.544; intraoperative factors included operative time (4 to 4:59 hours, 5 to 5:59 hours). The addition of these variables to the model resulted in a c-index of 0.684. The addition to the model of the postoperative variables—return to the operating room and the development of two or more complications—resulted in a final c-index of 0.708. The factor associated with highest OR was the development of two or more complications after surgery (OR 5.9, 95% CI 3.3 to 10.7).
Orthopedics
For total knee replacement, preoperative risk factors statistically significantly associated with a prolonged LOS include nonwhite race, partially dependent functional status, and age 60 years or older, with a c-index of 0.570. The intraoperative factor associated with a prolonged LOS was the transfusion of one or more units of blood. The addition of this factor resulted in a c-index of 0.575. Postoperative factors associated with a prolonged LOS were the development of two or more complications and return to the operating room. The addition of both postoperative variables to the model resulted in a c-index of 0.628. The factor generating the highest OR was return to the operating room (OR 4.9, 95% CI 3.0 to 6.2).
For total hip replacement, the preoperative factors associated with a prolonged LOS included age 60 years or older, ASA class 3, ASA class 4, and partially dependent functional status, with a c-index for the preoperative variables of 0.637. The intraoperative factor associated with a prolonged LOS was transfusion of one or more units of blood, resulting in a c-index of 0.647. Postoperative factors included two complications, three or more complications, and return to the operating room, resulting in a final c-index of 0.696. The factor associated with the highest OR was return to the operating room (OR 7.3, 95% CI 4.8 to 11.3).
For lumbar laminectomy, preoperative factors associated with a prolonged LOS were partially dependent functional status, ASA class 4, and age 60 years or older, resulting in a c-index of 0.679. The intraoperative factor associated with a prolonged LOS was the transfusion of one or more units of blood. The postoperative variable significantly associated with prolonged LOS, and generating the highest OR for a prolonged LOS, was return to the operating room (OR 6.6, 95% CI 3.0 to 14.3). The addition of the intraoperative variables to the model resulted in a c-index of 0.710; the addition of the postoperative variable resulted in a c-index of 0.733.
General Surgery
For partial colectomy, preoperative factors statistically significantly associated with a prolonged LOS were partially dependent functional status, ASA class 3, ASA class 4, impaired sensorium, and preoperative wound infection, with a c-index for this group of variables of 0.645. Intraoperative factors included operative time (4 to 4:59 hours or 5 to 5:59 hours), resulting in a c-index of 0.663. Postoperative factors associated with a prolonged LOS were one or more complications, wound dehiscence, pneumonia, ileus, and urinary tract infection, return to the operating room, and the number of complications (two, three, four or more). The addition of the postoperative factors resulted in a c-index of 0.758. Factors associated with the greatest OR were the individual postoperative complications urinary tract infection (OR 4.2, 95% CI 2.7 to 6.5), wound dehiscence (OR 5.4, 95% CI 2.3 to 12.8), and pneumonia (OR 5.0, 95% CI 3.0 to 8.4).
For open cholecystectomy, preoperative factors statistically significantly associated with prolonged LOS included partially dependent functional status, ASA class 3, ASA class 4, and age 60 years or older, resulting in a c-index of 0.655. Intraoperative factors included operative time (3 to 3:59 hours, 4 to 4:59 hours, and 5 to 5:59 hours), and intraoperative blood transfusions, with a c-index of 0.731. Postoperative factors included pneumonia, number of complications (two or more), and return to the operating room, with a final c-index of 0.771. Factors associated with the highest OR were operative time 5 to 5:59 hours (OR 10.4, 95% CI 5.8 to 18.7) and postoperative pneumonia (OR 11.3, 95% CI 5.0 to 25.4).
For laparoscopic cholecystectomy, preoperative factors statistically significantly associated with a prolonged LOS were ASA class 3, ASA class 4, and age 60 years or older, with a c-index of 0.638. The intraoperative factor associated with a prolonged LOS was operative time of 3 to 3:59 hours. The addition of this variable resulted in a c-index of 0.646. The postoperative factors associated with a prolonged LOS, and generating the highest OR among all variables in the model, were two or more complications (OR 3.8, 95% CI 1.2 to 12.1) and return to the operating room (OR 4.4, 95% CI 2.0 to 9.8). The addition of the postoperative variables to the model resulted in a final c-index of 0.662.
Vascular Surgery
For abdominal aortic aneurysm repair, the preoperative factor statistically significantly associated with a prolonged LOS was ASA class 4, with a c-index of 0.560. The intraoperative factor associated with a prolonged LOS was operative time (5 to 5:59 hours). Postoperative factors associated with a prolonged LOS were return to the operating room, pneumonia, urinary tract infection, ileus, and number of complications (two, three or more). The addition of the intraoperative variables resulted in a c-index of 0.641, and the addition of the postoperative factors resulted in a c-index of 0.798. The factors generating the highest OR were the postoperative complications return to the operating room (OR 8.4, 95% CI 4.6 to 15.4), ileus (OR 8.9, 95% CI 4.0 to 20.1), and pneumonia (OR 10.5, 95% CI 5.2 to 21.2).
For femoral popliteal revascularization, preoperative factors associated with a prolonged LOS were wound infection and partially dependent functional status, with a c-index of 0.656. Intraoperative factors included operative time (5 to 5:59 hours) and transfusion of one or more units of blood, with a c-index of 0.687. The postoperative factors associated with a prolonged LOS were return to the operating room and number of complications (two, three or more). The factors generating the highest OR were return to the operating room (OR 8.2, 95% CI 6.1 to 10.9) and three or more complications (OR 6.5, 95% CI 3.3 to 12.7). The final c-index for the model with the inclusion of the postoperative variables was 0.823.
For carotid endarterectomy, preoperative factors associated with a prolonged LOS were ASA class 4, history of a cerebrovascular accident, and partially dependent functional status, with a c-index of 0.614. Intraoperative factors included operative time (4 to 4:59 hours, 5 to 5:59 hours) and transfusion of one or more units of blood, with a c-index of 0.641. Postoperative factors included two or more complications and return to the operating room, resulting in a c-index of 0.738. Factors associated with the highest OR were intraoperative blood transfusion (OR 6.7, 95% CI 2.8 to 16.0) and two or more complications (OR 10.2, 95% CI 5.6 to 18.5).
Predictive Validity
The discrimination (c-index) of the 11 models ranged from 0.62 to 0.83. Validation of the models using phase II data resulted in <0.06 degradation in the c-index for each model.
Deaths
The number of deaths in 30 days were as follows: TURP 23, radical prostatectomy 7, total knee replacement 8, total hip replacement 27, lumbar laminectomy 0, partial colectomy 64, open cholecystectomy 18, laparoscopic cholecystectomy 3, abdominal aortic aneurysm repair 23, femoral popliteal revascularization 19, and carotid endarterectomy 17. For all of the operations, most of the cases involving death had a prolonged LOS. The models were run with and without death included, and the variables did not change within the models. There were only minor changes in the OR for prolonged LOS for each factor with deaths included and then excluded from the models. Because of this, deaths were included in the final models.
DISCUSSION
For 11 common elective operations performed in VAMCs, prolonged LOS is associated with preoperative patient characteristics, intraoperative processes, and postoperative adverse occurrences. Preoperative patient characteristics predictive of prolonged LOS among the 11 operations were advanced age, diminished functional status, and ASA classes 3 and 4.
Preoperative patient characteristics were significant predictors of prolonged LOS, but they were not more predictive than intraoperative and postoperative factors. In several operations, preoperative factors generated a lower OR in association with a prolonged LOS than both intraoperative process of care and postoperative adverse events.
Intraoperative events statistically significantly associated with a prolonged LOS were transfusion of at least one unit of blood and operative time. Operative time was associated with a risk for prolonged LOS for TURP, partial colectomy, open cholecystectomy, laparoscopic cholecystectomy, radical prostatectomy, abdominal aortic aneurysm repair, femoral popliteal revascularization, and carotid endarterectomy. After adjusting for age, ASA class, and functional status, the magnitude of the association of operative time with prolonged LOS was high. This variable may be a marker for patient characteristics, the severity of the primary disease at the time of operation, the skill of the primary surgeon, or the experience of the surgical team.
In addition to the preoperative and intraoperative factors, postoperative complications and return to the operating room were associated with high risks for prolonged LOS for the 11 elective operations. A postoperative complication as a cause of prolonged LOS is not surprising clinically and has been shown in prior studies. 19 Although complications will occur, previous studies provide evidence of patients who are more likely to have complications 25–32 ; determining what puts patients at risk for these complications may help to reduce these adverse events. For postoperative pneumonia, a previous controlled clinical trial 33 has shown that the use of respiratory rehabilitation after elective abdominal surgery can reduce the incidence of postoperative pulmonary complications, including pneumonia. In our study, postoperative pneumonia was a factor for prolonged LOS for partial colectomy and abdominal aortic aneurysm repair. A study to determine the impact of aggressive pulmonary care in the immediate postoperative period for these operations may help to reduce this complication.
Length of stay is an important outcome as a marker for resource consumption, and prolonged LOS can provide insight into the process of care. 34–38 One study has shown that the greatest costs associated with elective surgery are incurred the day of surgery and the first postoperative day 39 ; this, however, does not take into account the development of complications. Other studies have shown that complications after major surgery increase hospital costs. 40 In our study, poor postoperative outcomes and intraoperative process of care are associated with a prolonged LOS and, by inference, greater hospital costs. If the intraoperative process of care can be improved while maintaining the quality of care, and postoperative adverse events can be minimized, then the number of patients with a prolonged LOS can be reduced, decreasing resource consumption. In our study, the intraoperative process of care variables associated with a prolonged LOS were operative time and red blood cell transfusions administered during surgery. These summary variables reflect the overall intraoperative process of care; additional research and an in-depth assessment of surgical process of care in the operating room are needed to determine optimal techniques that may reduce complications and prolonged LOS.
The limitations of this study include the patient population. A study of older men may not apply to younger patients or women, thus limiting generalizability. Operation, subspecialty, and disease-specific variables were not collected; this may have limited the ability to define for each operation which preoperative, intraoperative, and postoperative variables were most associated with a prolonged LOS and could also reduce the explanatory power (c-index) of each model. Patient vital signs and some preoperative assessment tools such as electrocardiograms could not be collected consistently across sites and were not included.
The purpose of the NSQIP is to collect data and build predictive models that permit the VHA to use risk-adjusted surgical outcomes as a means to compare the quality of surgical care among the various VAMCs. 20 Previous studies have highlighted that variations in LOS are affected by many factors, including patient, physician, and hospital characteristics. 37 This study of the predictors of prolonged LOS indicates that intraoperative process of care and postoperative adverse events have a greater association with prolonged postoperative LOS than preoperative patient characteristics. Differences among surgical services in postoperative LOS may be relatively insensitive to adjustment for patient characteristics.
Footnotes
Correspondence: Tracie Collins, MD, MPH, Department of Veterans Affairs, 2002 Holcombe Blvd. (152), Houston, TX 77030.
The National Veterans Affairs Surgical Risk Study was funded by the Office of Quality Management, Patient Care Services, and the Health Services Research and Development Service of the Department of Veterans Affairs.
At the time this research was conducted, Dr. Collins was a Harvard General Medicine Fellow at the Brockton/West Roxbury VA Medical Center, and Dr. Daley was a Senior Research Associate in the Career Development Award Program in Health Services Research and Development.
Accepted for publication February 4, 1999.
References
- 1.Angus AC, Linde-Zwirble WT, Sirio CA, et al. The effect of managed care on ICU length of stay implications for Medicare. JAMA 1996; 276: 1075–1082. [PubMed] [Google Scholar]
- 2.Luft HS, Hunt SS. Evaluating individual hospital quality through outcome statistics. JAMA 1986; 255: 2780. [PubMed] [Google Scholar]
- 3.Hebel JR, Kessler II, Mabuchi K, McCarter RJ. Assessment of hospital performance by use of death rates: A recent case history. JAMA 1982; 248: 3131–3135. [PubMed] [Google Scholar]
- 4.McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA 1994; 272: 859–866. [PubMed] [Google Scholar]
- 5.Daley J. Validity of risk adjustment methods. In: Iezzoni LI, ed. Risk Adjustment for Measuring Health Care Outcomes. Ann Arbor, MI: Health Administration Press; 1997: 239–262.
- 6.Iezzoni LI. Risk adjustment and current health policy debates. In: Iezzoni LI, ed. Risk Adjustment for Measuring Health Care Outcomes, 2d ed. Ann Arbor, MI: Health Administration Press; 1997: 357.
- 7.Kalish RL, Daley J, Duncan CC, Davis RB, Coffman GA, Iezzoni LI. Costs of potential complications of care for major surgery patients. Am J Med Quality 1995; 10: 48–54. [DOI] [PubMed] [Google Scholar]
- 8.Daley J, Jencks S, Draper D, Lenhart G, Thomas N, Walker J. Predicting hospital-associated mortality for Medicare patients. JAMA 1988; 260: 3617–3624. [DOI] [PubMed] [Google Scholar]
- 9.Roberts AJ, Woodhall DD, Conti CR, et al. Mortality, morbidity, and cost accounting related to coronary artery bypass surgery in the elderly. Ann Thorac Surg 1985; 39: 426–432. [DOI] [PubMed] [Google Scholar]
- 10.Montague NT, Kouchoukos NT, Wilson TAS, et al. Morbidity and mortality of coronary artery bypass grafting in patients 70 years of age or older. Ann Thorac Surg 1985; 39: 552–557. [DOI] [PubMed] [Google Scholar]
- 11.Grover FL, Hammermeister KE, Burchfiel C. Initial report of the Veterans Administration Preoperative Risk Assessment Study for Cardiac Surgery. Ann Thorac Surg 1990; 50: 12–28. [DOI] [PubMed] [Google Scholar]
- 12.Hammermeister KE, Burchfiel C, Johnson R, and Grover FL for the VA Surgeons and Cardiologists. Identification of patients at greatest risk for developing major complications at cardiac surgery. Circulation 1990; 82(Suppl 4): 380–389. [PubMed] [Google Scholar]
- 13.Grover FL, Johnson RR, Hammermeister KE and the VA Cardiac Surgeons. Factors predictive of operative mortality among coronary artery bypass subsets. Ann Thorac Surg 1993; 56: 1296–1307. [DOI] [PubMed] [Google Scholar]
- 14.Grover FL, Johnson RR, Shrover AL, et al. The Veterans Affairs Continuous Improvement in Cardiac Surgery Study. Ann Thorac Surg 1994; 58: 1845–1851. [DOI] [PubMed] [Google Scholar]
- 15.Hammermeister KE, Johnson R, Marshall G, Grover FL. Continuous assessment and improvement in quality of care. A model from the Department of Veterans Affairs. Ann Surg 1994; 219: 281–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Macario A, Vitez TS, Dunn B, McDonald T, Brown B. Hospital costs and severity of illness in three types of elective surgery. Anesthesiology 1997; 86: 92–100. [DOI] [PubMed] [Google Scholar]
- 17.Cleary PD, Greenfield S, Mulley AG, et al. Variations in length of stay and outcomes for six medical and surgical conditions in Massachusetts and California. JAMA 1991; 266: 73–79. [PubMed] [Google Scholar]
- 18.Greenfield S, Apolone G, McNeil BJ, Cleary PD. The importance of co-existent disease in the occurrence of postoperative complications and one-year recovery in patients undergoing total hip replacement. Med Care 1993; 31: 141–154. [DOI] [PubMed] [Google Scholar]
- 19.McAleese P, Odling-Smee W. The effect of complications on length of stay. Ann Surg 1994; 220: 740–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khuri SF, Daley J, Henderson WG, et al. The National Veterans Administration Surgical Risk Study: Risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg 1995; 180: 519–609. [PubMed] [Google Scholar]
- 21.Khuri SF, Daley J, Henderson WG, et al. Risk adjustment of the postoperative mortality rate for the comparative assessment of the quality of surgical care: Results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg 1997; 185: 315–327. [PubMed] [Google Scholar]
- 22.Daley J, Khuri SK, Henderson WH, et al. Comparative assessment of thirty-day morbidity following major surgery: Results of the National VA Surgical Risk Study. J Am Coll Surg 1997; 185: 328–340. [PubMed] [Google Scholar]
- 23.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. Am J Infection Control 1988; 16: 128–140. [DOI] [PubMed] [Google Scholar]
- 24.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982; 143: 29–36. [DOI] [PubMed] [Google Scholar]
- 25.Goldman K, Caldera D, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977; 297: 845–850. [DOI] [PubMed] [Google Scholar]
- 26.Goldman L. Cardiac risks and complications of noncardiac surgery. Ann Intern Med 1983; 98: 504–513. [DOI] [PubMed] [Google Scholar]
- 27.Jewell ER, Perrson AV. Preoperative evaluation of the high-risk patient. Surg Clin North Am 1985; 65: 3–19. [DOI] [PubMed] [Google Scholar]
- 28.Roberts AJ, Woodhall DD, Conti CR, et al. Mortality, morbidity, and cost-accounting related to coronary artery bypass graft surgery in the elderly. Ann Thoracic Surg 1985; 39: 426–432. [DOI] [PubMed] [Google Scholar]
- 29.Detsky AS, Abrams HB, McLaughlin JR, et al. Predicting cardiac complications in patients undergoing non-cardiac surgery. J Gen Intern Med 1986; 1: 211–219. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke MK. Preoperative evaluation: The assessment and management of surgical risk. J Gen Intern Med 1987; 2: 257–269. [DOI] [PubMed] [Google Scholar]
- 31.Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg [Br] 1995; 77: 250–253. [PubMed] [Google Scholar]
- 32.Lotke PA, Faralli VJ, Orenstein EM, Ecker ML. Blood loss after total knee replacement: Effects of tourniquet release and continuous passive motion. J Bone Joint Surg [Am] 1991; 73: 1037–1040. [PubMed] [Google Scholar]
- 33.Soledad C, Ponce JL, Delgado F, Viciano V, Mateu M. Prevention of postoperative pulmonary complications through respiratory rehabilitation: A controlled clinical study. Arch Phys Med Rehabil 1998; 79: 5–9. [DOI] [PubMed] [Google Scholar]
- 34.Cullen DJ, Giovanni A, Greenfield S, et al. ASA physical status and age predict morbidity after three surgical procedures. Ann Surg 1994; 220: 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magdi KM. Length of postoperative hospital stay after transurethral resection of the prostate. Ann R Coll Surg Engl 1997; 79: 284–288. [PMC free article] [PubMed] [Google Scholar]
- 36.Katz NM, Ahmed SW, Clark BK, Wallace RB. Predictors of length of hospitalization after cardiac surgery. Ann Thorac Surg 1985; 45: 656–660. [DOI] [PubMed] [Google Scholar]
- 37.Burns LR, Wholey DR. The effects of patient, hospital, and physician characteristics on length of stay and mortality. Med Care 1991; 29: 251–271. [DOI] [PubMed] [Google Scholar]
- 38.Evans JH, Hwang Y, Nagarajan N. Physicians’ response to length-of-stay profiling. Med Care 1995; 33: 1106–1119. [DOI] [PubMed] [Google Scholar]
- 39.Marrin CAS, Johnson LC, Beggs VL, Batalden PB. Clinical process cost analysis. Ann Thorac Surg 1997; 64: 690–694. [DOI] [PubMed] [Google Scholar]
- 40.Munoz E, Bartholomew JT, Jaker M, Sakmyster M, Kanofsky P. Surgical resource consumption in an academic health consortium. Surgery 1994; 115: 411–416. [PubMed] [Google Scholar]