Abstract
Objective
To investigate risk factors associated with aneurysm rupture using patients randomized into the U.K. Small Aneurysm Trial (n = 1090) or monitored for aneurysm growth in the associated study (n = 1167).
Summary Background Data
The U.K. Small Aneurysm Trial has shown that ultrasound surveillance is a safe management option for patients with small abdominal aortic aneurysms (4.0 to 5.5 cm in diameter), with an annual rupture rate of 1%.
Methods
In the cohort of 2257 patients (79% male), aged 59 to 77 years, 103 instances of abdominal aortic aneurysm rupture were identified during the 7-year period of follow-up (1991–1998). Almost all patients (98%) had initial aneurysm diameters in the range of 3 to 6 cm, and the majority of ruptures (76%) occurred in patients with aneurysms ≥5 cm in diameter. Kaplan-Meier survival and Cox regression analysis were used to identify baseline risk factors associated with aneurysm rupture.
Results
After 3 years, the annual rate of aneurysm rupture was 2.2% (95% confidence interval 1.7 to 2.8). The risk of rupture was independently and significantly associated with female sex (p < 0.001), larger initial aneurysm diameter (p < 0.001), lower FEV1 (p = 0.004), current smoking (p = 0.01), and higher mean blood pressure (p = 0.01). Age, body mass index, serum cholesterol concentration, and ankle/brachial pressure index were not associated with an increased risk of aneurysm rupture.
Conclusions
Within this cohort of patients, women had a threefold higher risk of aneurysm rupture than men. Effective control of blood pressure and cessation of smoking are likely to diminish the risk of rupture.
Rupture of an abdominal aortic aneurysm (AAA) is a catastrophic event. Many patients die without reaching the operating table, and only 50% of those undergoing surgical repair survive beyond 30 days. 1,2 Therefore, most surgeons offer elective repair to fit patients with an asymptomatic AAA. The benefits of such a strategy for patients with a small aneurysm (4.0 to 5.5 cm in diameter) have been challenged recently: the U.K. Small Aneurysm Trial showed that early elective surgery conferred no long-term survival benefit. 3 Uncertainty concerning the risk of rupture of AAAs of different sizes and the absence of appropriate evidence compound the difficulties of decision making, particularly for patients of marginal fitness. 4 Autopsy studies have indicated that aneurysm diameter is an important determinant of rupture, with larger aneurysms having the greatest risk. 5,6 However, diameter as measured at autopsy does not reflect diameter in vivo. 7 Studies in living patients also may suffer from the poor reproducibility of measuring aneurysm diameter by different scanning modalities, 8 particularly for retrospective data. A further complicating issue is the confirmation of AAA rupture in patient or population studies. Not surprisingly, the rupture rates reported for aneurysms <5.0 cm in diameter vary widely, from 0% 7 or 1% per annum 3,9,10 to as high as 6% per annum. 11 The data for larger aneurysms are even more difficult to interpret, although modeling studies have suggested that the risk of rupture is 9% and 12.5% per annum for AAAs with diameters of 6.5 and 7.5 cm, respectively. 12 Size apart, other factors such as hypertension may influence the risk of aneurysm rupture. 11 Knowledge of these other factors should allow a more informed approach to management, particularly in patients of marginal fitness.
The U.K. Small Aneurysm Trial and the associated study, for patients ineligible or refusing randomization, 13 provided the opportunity to investigate prospectively, in a large cohort (n = 2257) of carefully monitored patients, the parameters that influence rupture of AAAs.
METHODS
The methods have been described elsewhere. 3,13 Briefly, patients (age 60–76 years) were entered into either the U.K. Small Aneurysm Trial or the Small Aneurysm Study from 93 hospitals across Britain. Fit patients who consented to randomization in the trial had an AAA 4.0 to 5.5 cm in diameter. In total, 1090 patients were randomized in the 4-year period from September 1991, and 527 of these were allocated to serial ultrasonographic surveillance. 3 The 563 patients randomized to surgery were included up to the time of surgery. These 563 patients may have been followed since before the aneurysm reached 4.0 cm (the Small Aneurysm Study), or had to wait several months before elective surgery, contributing 706 person-years of follow-up. In addition, the trial coordinators followed the progress of a further 1167 patients who were ineligible for randomization for the following reasons: the aortic diameter was <4.0 cm (n = 507) or >5.5 cm (n = 100), the patient refused randomization (n = 122), the patient was considered unfit for surgery (n = 340), or other reason, such as with a long wait before elective surgery (n = 98). All these patients were monitored at regular intervals by the trial coordinators, who measured the AAA diameter with an Aloka SSD500 scanner equipped with a 3.5-MHz transducer (Keymed, Southend, United Kingdom). The repeatability of measurement of aneurysm diameter was ±0.2 cm. All patients were flagged at the Office of National Statistics to enable us to receive automatic notification of emigration, death, place of death, underlying cause of death, and whether an autopsy was performed. For this study, our primary end-point was rupture of the AAA; this was ascertained either from the death certificate or from imaging and surgical details.
Statistical analysis was undertaken according to a predefined plan. Patients were censored at June 30, 1998 (the end of the trial), or if the earlier events of emigration, aneurysm repair, aneurysm rupture, or death had occurred. Kaplan-Meier survival curves for time from initial AAA diameter were used to evaluate rupture rates. We used Cox’s proportional hazards regression to estimate hazard ratios and to adjust these for age, sex, and initial aneurysm diameter. Aneurysm growth rates were calculated by linear regression analysis.
To investigate how the risk of aneurysm rupture varied with aortic diameter, we used measurements obtained within the 12 months preceding rupture (available for 82/103 [80%] of the ruptures). For the further 21 patients who died from aneurysm rupture, we estimated an aneurysm diameter at the time of rupture based on the last measurement (>1 year previously) and the aneurysm growth rate in that patient. This estimated diameter was used to allocate these 21 patients to the size categories used for analysis. For the 2154 patients not known to have AAA rupture, the person-years of follow-up were calculated to the time of censorship (AAA repair, cessation of follow-up, or death).
RESULTS
Rupture Rates According to Baseline Variables
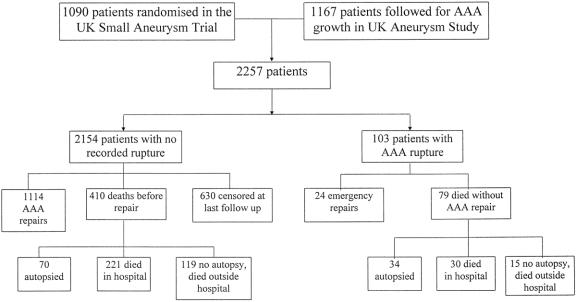
Among the 1090 randomized patients, there were 25 recorded AAA ruptures. In 8 patients the event was verified at surgical repair, and 17 died without surgical repair and the event was recorded on the death certificate (including 10 autopsies). To increase the number of events (AAA rupture) identified, we included 1167 nonrandomized patients, among whom there was a higher proportion of ruptures (78/1167). This yielded a cohort of 2257 patients (Fig. 1) with 103 recorded aneurysm ruptures. Twenty-four ruptures were confirmed at surgical repair, 34 were confirmed by autopsy, a further 30 patients died in the hospital from aneurysm rupture, and 15 of the deaths attributed to ruptured aneurysm occurred outside the hospital without an autopsy. Of the 103 patients with AAA rupture, 26 (25%) patients died without ever reaching the hospital, 53 (51%) died in the hospital without undergoing surgery, 13 (13%) died within 30 days of surgery (46% operative mortality rate), and 11 (11%) survived beyond 30 days. In total, 502 deaths (occurring before June 30, 1998) were recorded. Ruptured AAA was the underlying cause of death in 92 patients (18%), including 13 who did not survive emergency surgical repair. The autopsy rate was 21%. A further 51% of these patients died in the hospital, and the remainder died elsewhere without evidence of an autopsy being performed. The progress of patients is shown in Figure 1. Altogether, there were 4102 patient-years of follow-up.
Figure 1. Profile of patients with respect to rupture of abdominal aortic aneurysm (AAA).
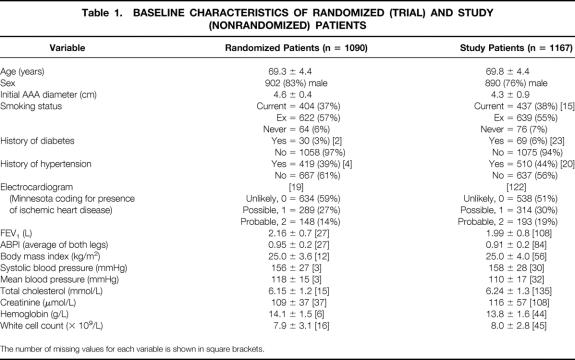
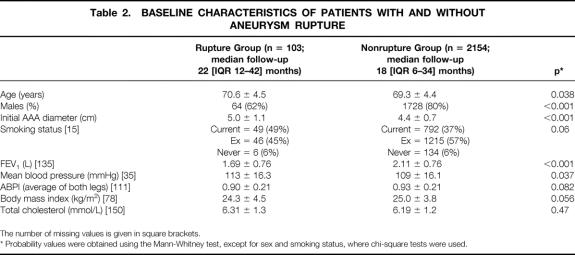
The baseline characteristics of the trial and study patients are compared in Table 1 and the baseline characteristics of the patients with and without aneurysm rupture in Table 2. The study group was in many respects similar to the trial group, although there was an increased proportion of women and the study group was slightly older, had smaller aneurysms, and, as might be expected, had poorer lung and renal function (see Table 1). The mean initial AAA diameter was higher among the patients with rupture, and this group had a high proportion of women (38%) and current smokers (49%) (see Table 2). The mean blood pressure also was higher in the patients with aneurysm rupture. The other variables in Table 2 all had a moderate number of missing values. There was no association between use of aspirin or beta-blockers and AAA rupture. Ruptures occurred during every month of the year, but with a seasonal nadir in September and October.
Table 1. BASELINE CHARACTERISTICS OF RANDOMIZED (TRIAL) AND STUDY (NONRANDOMIZED) PATIENTS
The number of missing values for each variable is shown in square brackets.
Table 2. BASELINE CHARACTERISTICS OF PATIENTS WITH AND WITHOUT ANEURYSM RUPTURE
The number of missing values is given in square brackets.
* Probability values were obtained using the Mann-Whitney test, except for sex and smoking status, where chi-square tests were used.
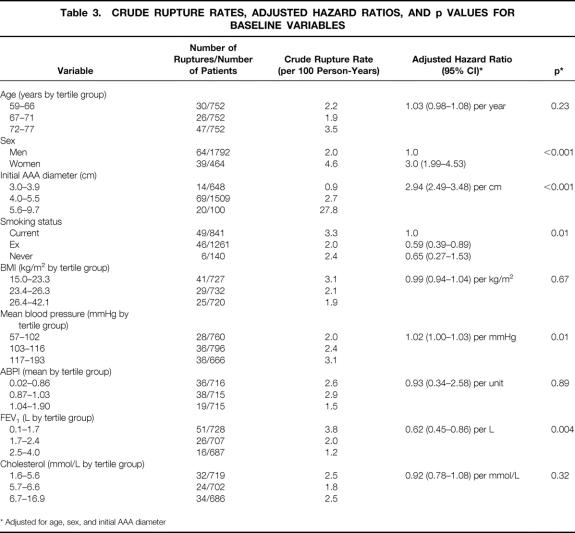
The overall survival without AAA rupture in this cohort of 2257 patients is shown in Figure 2. In the first 3 years, the annual rupture rate was 2.2% (95% confidence interval 1.7 to 2.8). The estimated hazard ratios identified the possibility that female sex, higher mean arterial blood pressure, current smoking, and FEV1, in addition to initial AAA diameter, increased the risk of aneurysm rupture (Table 3). Although height was inversely associated with the risk of rupture in univariate analysis, after adjustment for age and sex the association was no longer significant. The fitness status (electrocardiogram, creatinine measurement) of men and women was similar, but the mean diameter preceding rupture was smaller in women (5.0 ± 0.8 cm) than men (6.0 ± 1.4 cm) (p = 0.001). The Kaplan-Meier curves comparing rupture-free survival in men and women (Fig. 3) also clearly indicate the threefold increased risk of AAA rupture in women (log rank test, p < 0.001).
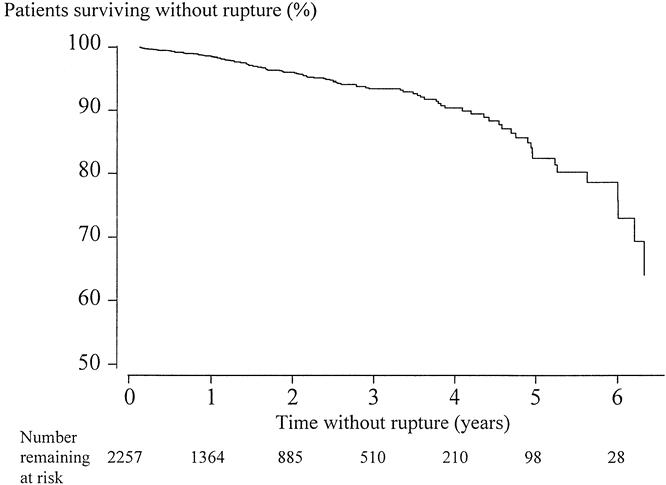
Figure 2. Overall survival without abdominal aortic aneurysm rupture. Kaplan-Meier estimate; patients were censored at death, aneurysm repair, or last follow-up.
Table 3. CRUDE RUPTURE RATES, ADJUSTED HAZARD RATIOS, AND p VALUES FOR BASELINE VARIABLES
* Adjusted for age, sex, and initial AAA diameter
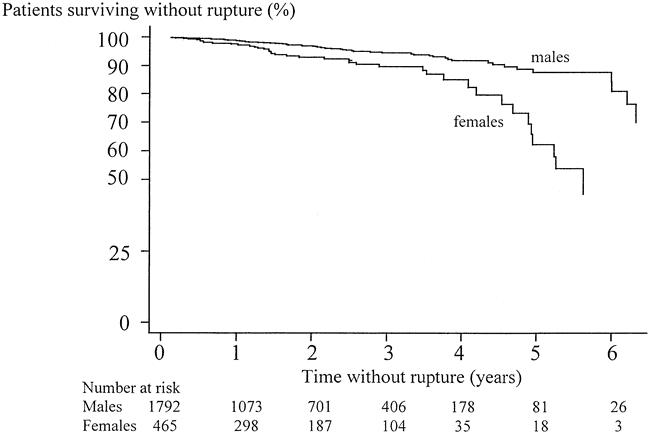
Figure 3. Overall survival without AAA rupture by gender. Kaplan-Meier estimates; patients were censored at death, aneurysm repair, or last follow-up. Log rank values, p < 0.001.
The large cohort of 2257 patients included significant proportions of patients whose AAA diameter never exceeded 4.0 cm or who, although the AAA diameter exceeded 5.5 cm, were considered unfit or refused surgery. The inclusion of these patients could have biased the results. Therefore, we repeated the analysis using only the more homogenous group of 1090 fit patients with AAAs 4.0 to 5.5 cm in diameter randomized in the U.K. Small Aneurysm Trial (with 25 known ruptures). This analysis of trial patients identified current smoking as having borderline significance, with initial AAA diameter, female sex, and higher mean blood pressure being independently and significantly associated with aneurysm rupture (Table 4). We have long suspected that self-reporting of smoking status may be inaccurate. Baseline plasma cotinine (a long-lived metabolite of nicotine) was measured in the 1090 trial patients. When cotinine instead of self-reported smoking status was used as the index of smoking habit, the clear significance of smoking was observed (p = 0.045).
Table 4. VARIABLES ASSOCIATED WITH ANEURYSM RUPTURE IN 1090 RANDOMIZED TRIAL PATIENTS
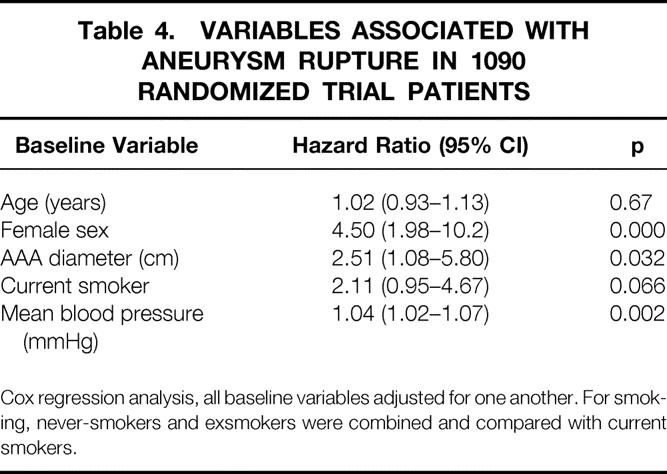
Cox regression analysis, all baseline variables adjusted for one another. For smoking, never-smokers and exsmokers were combined and compared with current smokers.
Risk of Rupture and Last AAA Diameter
To obtain further insight into how the risk of rupture varied according to the most recent aortic diameter, patients were categorized into four groups with diameters of ≤3.9 cm, 4.0 to 4.9 cm, 5.0 to 5.9 cm, and ≥6.0 cm. In 82/103 patients with AAA rupture, the aortic diameter had been measured within the preceding 12 months. An estimate of AAA diameter at rupture, based on last known diameter and individual growth rate, was made for the remaining 21 cases. Based on known (known + estimated) diameter at rupture, there were 2 (3), 18 (24), 33 (40), and 29 (36) ruptures in diameter categories ≤3.9 cm, 4.0 to 4.9 cm, 5.0 to 5.9 cm, and ≥6.0 cm, respectively. The total number of person-years in each size range was calculated from the first AAA diameter measurement in that size range to the first measurement recorded in the next size range. The number of ruptures per 100 patient-years increased from 0.3 for AAA ≤3.9 cm to 1.5 and 6.5 for patients with AAAs in the diameter ranges 4.0 to 4.9 cm and 5.0 to 5.9 cm, respectively. The person-years of follow-up for patients with AAAs ≥6.0 cm was so restricted by censorship at surgery that no estimate of rupture rate was calculated, although the rate of rupture appeared very high. The alternate analysis displaying survival without AAA rupture from the last measurement of aortic diameter up to the time of aneurysm repair, death, AAA rupture, or cessation of follow-up 9 is shown in Figure 4. This analysis does not provide an estimate of rupture rates but allows assessment of how the risk of rupture varies with the last known AAA diameter. The much-higher risk of rupture in patients with aneurysms ≥6.0 cm is shown clearly.
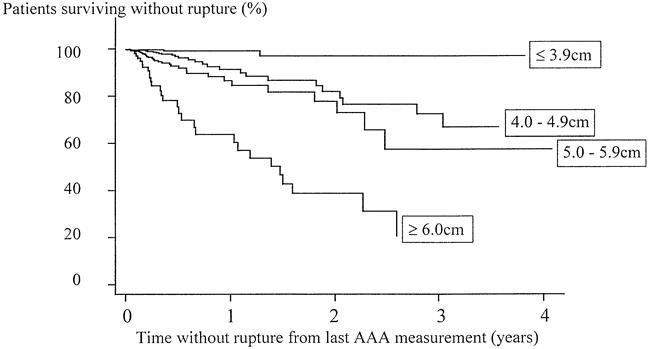
Figure 4. Survival without abdominal aortic aneurysm (AAA) rupture by size category of last measured aortic diameter.
DISCUSSION
The prognosis of AAA has been uncertain, mostly because it has remained difficult to predict which aneurysms, in a given size range, are at highest risk of rupture. Our study shows that even very small aneurysms may rupture, but the risk and rate of rupture is very low. Previous cohort and population studies, like the present study, have been complicated by the uncertainty of diagnosis: no study has a full autopsy rate. Imaging and operative details and autopsy all permit an accurate diagnosis of rupture. The diagnosis of ruptured AAA, unconfirmed by these modalities, after a hospital death can be viewed with confidence but is less secure. In this study, a large number of deaths occurred outside the hospital, 15 in the rupture arm and 119 in the nonrupture arm (see Fig. 1); in these patients, the diagnosis of aneurysm rupture is insecure, providing the possibility of significant amounts of both false-positive and false-negative information. However, this study has the advantages of being prospective, based on very reproducible physiologic measurements (including AAA diameter), and providing accurate censorship at the time of AAA repair. This latter event may be difficult to ascertain in large population studies.
Screening studies have shown that the prevalence of AAA is much lower in women than men. 10 Women form only a small proportion of the surgical caseload for this condition. One of the most important and surprising findings of our study is that the rate of aneurysm rupture was three times higher in women than in men (see Fig. 3). This difference remained after adjustment for age, initial AAA diameter, and body mass index or height. The mean AAA diameter at rupture was 5 cm in women and 6 cm in men. There is evidence to indicate that women have smaller-diameter, more compliant aortas than men. 14 This might suggest that the ratio of infrarenal/suprarenal diameter is the important determinant of AAA stability or rupture, although suprarenal diameters cannot be measured reproducibly by ultrasonography. 8
Higher mean blood pressure and current smoking (associated with a low FEV1) are the risk factors for AAA rupture that can be altered. Previously, we have shown that small aneurysms appeared to grow faster in smokers, 15 and others have indicated that poor lung function and increased diastolic blood pressure are associated with AAA rupture. 11 Mean blood pressure reflects the continuing hemodynamic burden on the aortic wall, always present to weaken the aneurysmal section. Among the cohort of patients we studied, there was a very significant correlation between current smoking habit and lung function: both were associated with AAA rupture. The data on smoking habit were more complete than lung function measurements. Moreover, poor lung function is a valid reason to declare a patient unfit for surgery, providing potential bias, whereas current smoking habit is not. It has been known for a long time that smoking is the most important risk factor for the development of AAA. 16,17 Now, for the first time, we have shown that current smoking also increases the risk of AAA rupture. These findings indicate that for patients of marginal fitness, those who refuse surgery, or those in whom a wait before surgery is anticipated, the surgeons and physicians should collaborate to provide adequate control of blood pressure and counseling and replacement therapy to help the patient stop smoking.
Surgeons would like to know how to stratify the risk of rupture according to aneurysm diameter and growth rate. All previous studies have indicated that the risk of rupture escalates as the aortic diameter increases. 5,6,9,10 In the cohort studied here, the paucity of data for larger AAAs (≥6 cm) is mainly attributable to surgery and makes it difficult to provide accurate information. The highest proportion of ruptures occurred in those who were unfit for surgery or refused surgery. For these reasons, the figures we provide for ruptures per 100 patient-years and rupture-free survival after the last measurement of aortic diameter must be interpreted cautiously. Although small AAAs do rupture, the risk for an aneurysm smaller than 5 cm in diameter is very low. The risk for AAAs 5.0 to 5.9 cm in diameter also is low but appears to escalate sharply for aneurysms ≥6 cm in diameter. Unfortunately, the annual rate of rupture for these large aneurysms cannot be estimated, because the length of follow-up was very limited. The analysis of factors associated with AAA growth and whether rapid aneurysm growth predicts rupture will be the focus of a separate analysis.
This study has shed new light on the risk factors associated with the rupture of AAAs, particularly smaller aneurysms. Recently, endovascular repair has become a management option for patients considered unfit for open repair, but it is not known how this will influence rupture rates in such patients. Whether or not marginally fit patients are treated by endovascular repair, we shall need to know whether smoking cessation and improved blood pressure control will diminish the risk of rupture. Our data also suggest that when considering the indications for aneurysm repair, different thresholds should apply to women than men.
U.K. Small Aneurysm Trial
Steering Committee: Prof. RM Greenhalgh (Chairman); Prof. JT Powell (Imperial College at Charing Cross); Prof. FGR Fowkes, Dr. JF Forbes, Prof. CV Ruckley (University of Edinburgh).
Writing Committee: Prof. JT Powell (Chair); LC Brown, Prof. RM Greenhalgh, Prof. FGR Fowkes, Prof. CV Ruckley.
Monitoring Committee: Prof. PA Poole-Wilson (Chair); Sir N. Browse, Prof. CJ Bulpitt, Prof. K. Burnand, Dr. EC Coles, Dr. A. Fletcher.
Trial Coordinators: Sue Blair, Rebecca Clark, Carol Devine, Karen Ferguson, Sheila Hearn, Eileen Kerracher, Sarah Logan, Anna McCabe, Razia Meer-Baloch, Michelle Mossa, Anna Rattray, Katie Wilson.
ECG Coding: Mrs. N. Keen, Mrs. C. Rose.
Blood Analysis: R. Mir Hassaine.
TRIAL PARTICIPANTS (number of randomized patients recruited in brackets)
S.W. ENGLAND AND SOUTH WALES—Prof. M. Horrocks, Regional Trial Director: Royal United Hospital: Mr. J. Budd (6), Prof. M. Horrocks (23); Bristol Royal Infirmary: Mr. RN Baird (12), Mr. P Lamont (10); Derriford Hospital: Mr. DC Wilkins (6), Mr. S Ashley (3); Dorset County Hospital: Mr. K. Flowerdew (9); Frenchay Hospital: Mr. A. Baker (7); Gloucester Royal Infirmary: Mr. J. Earnshaw (4), Mr. B. Heather (3); Morriston Hospital: Mr. C. Gibbons (14); Neville Hall Hospital: Mr. RL Blackett (8); New Royal Bournemouth General Hospital: Mr. SD Parvin (30); North Devon District General Hospital: Mr. DR Harvey (1); Princess of Wales Hospital: Mr. R. Hedges (1); Princess Margaret Hospital: Mr. D. Finch (6), Mr. DB Hocken (2); Southampton General Hospital: Mr. GE Morris (1), Mr. CP Shearman (4); Southmead Hospital: Mr. P. Lear (4); Torbay Hospital: Mr. P. Lewis (5); Yeovil District General Hospital: Mr. RJ Clarke (5).
SCOTLAND & N.E. ENGLAND—Prof. CV Ruckley, Regional Trial Director: Edinburgh R.I.: Mr. AM Jenkins (1), Prof. CV Ruckley (28); Aberdeen R.I.: Mr. GG Cooper (18), Mr. J. Engeset (38), Mr. R. Naylor (1); Ayr Hospital: Mr. G. Stewart (16); Dryburn Hospital, Durham: Mr. J. Cumming (10); Dumfries & Galloway Royal Infirmary: Mr. J. McCormick (8); Dunfermline & West Fife Hospital: Miss A. Howd (9), Mr. A. Turner (6); Falkirk & District Infirmary: Mr. DR Harper (5), Mr. RC Smith (6); Freeman Hospital: Mr. J. Chamberlain (10), Mr. AG Jones (12), Mr. MG Wyatt (2); Gartnavel General Hospital: Mr. AJ McKay (13); Ninewells Hospital: Mr. JC Forrester (3), Mr. P. McCollum (30), Mr. PA Stonebridge (3); Perth Royal Infirmary: Mr. AIG Davidson (2); Queen Elizabeth Hospital: Mr. R. Baker (4); Royal Victoria Infirmary: Mr. JLR Forsythe (1), Mr. D. Lambert (8); Royal Northern Infirmary: Mr. JL Duncan (11).
THE MIDLANDS—Prof. PRF Bell, Regional Trial Director: Leicester Royal Infirmary: Prof. PRF Bell (25), Mr. D. Ratliff (1); Derbyshire Royal Infirmary: Mr. KG Callum (16), Mr. JR Nash (17); Glenfield General Hospital: Mr. DS McPherson (7); Kettering & General District Hospital: Mr. RE Jenner (4), Mr. R. Stewart (5); Kidderminster General Hospital: Mr. PR Armitstead (8); Leicester General Hospital: Mr. WW Barrie (5); Northampton General Hospital: Mr. DB Hamer (6), Mr. S. Powis (5); Northern General Hospital: Mr. LD Coen (2); Mr. J. Michaels (4), Mr. CL Welsh (3); Nottingham Queen’s Medical Centre: Mr. BR Hopkinson (5), Mr. PW Wenham (14); Royal Hallamshire Hospital: Mr. J. Beard (25); Sandwell District General Hospital: Mr. A. Auckland (3); Worcester Royal Infirmary: Mr. J. Black (7), Mr. R. Downing (6); Worcester Royal Infirmary: Mr. NC Hickey (3).
LONDON & S.E. ENGLAND—Prof. RM Greenhalgh, Regional Trial Director: Charing Cross Hospital: Mr. AH Davies (2), Prof. RM Greenhalgh (39), Mr. D. Nott (5); Colchester General Hospital: Mr. ARL May (33); Epsom District Hospital: Mr. R. McFarland (11); Guy’s Hospital: Mr. P. Taylor (15); Hillingdon Hospital: Mr. JWP Bradley (3), Mr. T. Paes (9); Ipswich Hospital: Mr. AEP Cameron (7); Joyce Green Hospital: Mr. A. McIrvine (18); Lewisham Hospital: Mr. D. Negus (4), Mr. PR Taylor (10); Medway Hospital: Mr. CM Butler (2), Mr. RW Hoile (1); Newham General Hospital: Mr. B. Pardy (11); Princess Alexandra Hospital: Miss J. Ackroyd (9); Royal Free Hospital: Mr. G. Hamilton (4); Royal Hampshire County Hospital: Mr. R. Lane (1); Royal Surrey County Hospital: Mr. AEB Giddings (21); St. Georges’s Hospital: Mr. J. Dormandy (5), Mr. R. Taylor (9); St. Peter’s Hospital: Mr. M. Thomas (18); St. Thomas’ Hospital: Mr. KJ Burnand (7); University College Hospital: Mr. M. Adiseshiah (3); West Middlesex Hospital: Mr. P. Pattison (1); West Norwich Hospital: Mr. J. Clarke (8), Mr. J. Colin (9); Wexham Park Hospital: Mr. P. Rutter (4); Whipps Cross Hospital: Mr. S. Brearley (14), Mr. M. Pietroni (1).
N. ENGLAND AND NORTH WALES—Prof. CN McCollum, Regional Trial Director: University Hospital South Manchester: Prof. CN McCollum (12); Arrowe Park Hospital: Mr. MG Greaney (2), Mr. D. Reilly (7); Blackburn Royal Infirmary: Mr. WG Paley (1); Blackpool, Victoria Hospital: Mr. M. Lambert (16); Burnley General Hospital: Mr. R. Hughes (16); Clatterbridge Hospital: Mr. S. Blair (2); Cumberland Infirmary: Mr. JEG Shand (1); Grimsby District General Hospital: Mr. LA Donaldson (1); Hull Royal Infirmary: Mr. JMD Galloway (2), Mr. AR Wilkinson (21); Leeds District General Hospital: Mr. M. Gough (16); Leigh Infirmary: Mr. J. Mosley (1); Macclesfield General Hospital: Mr. DM Matheson (19); Manchester Royal Infirmary: Mr. M. Walker (4); Oldham Royal Hospital: Mr. N. Hulton (4); Pontefract General Infirmary: Mr. MI Aldoori (4), Mr. CK Yeung (1); Royal Preston Hospital: Mr. AR Hearn (6); Royal Lancaster Infirmary: Mr. J. Kelly (18); Stafford General Hospital: Mr. D. Durrans (2), Mr. B. Gwynn (3); Stoke City General Hospital: Mr. GB Hopkinson (13); Telford General Hospital: Mr. RGM Duffield (18); The Infirmary Rochdale: Mr. IG Schraibman (3); York District Hospital: Mr. R. Hall (3), Mr. SH Leveson (4); Glan Clwyd Hospital, Rhyl: Mr. J. Clark (3), Mr. O. Klimach (23).
Discussion
Dr. Frank J. Veith (New York, New York): I congratulate Professor Greenhalgh and his colleagues in the United Kingdom Small Aneurysm Study for providing us with solid data to support our long-standing prejudice that not all aortic aneurysms in the 4.0- to 5.5-cm range have to be fixed urgently. These lesions are not “ticking time bombs,” as some surgeons mistakenly tell their patients. Professor Greenhalgh’s data now provide firm support for continuing to observe many of these patients, as we have done for many years.
I also congratulate Professor Greenhalgh on his presentation today and I thank him too for letting me review his excellent manuscript that brings us new data showing which patients with small aneurysms have a greater risk of rupture. However, I remain unclear on exactly how we should use this information in the management of individual patients. Perhaps Professor Greenhalgh can tell us which patients who have a 4.0- to 5.5-cm aneurysm and who are female, hypertensive, still smoking, or have chronic lung disease should be subjected to treatment and which ones should be observed.
As many of you may know, we have been heavily involved in endovascular grafting for the past 7 years and have now used 414 of these grafts to treat 256 patients. There are two relevant points to be made from our endovascular graft experience.
First, we have used these grafts to treat 130 high-risk aortoiliac aneurysm patients untreatable by standard surgery. All these high-risk patients had aneurysms over 5.5 cm in diameter, with some as large as 8.5 cm. For various reasons, logistic and regulatory, there was a delay between the time we first saw these patients and the time we could fix these aneurysms. This delay averaged over 4 months, and in several cases was over 4 years. Yet not one of these 130 patients had rupture of their aneurysm. This lends support to the principle that one can safely be deliberate in the evaluation and treatment of aneurysm patients, even with some of those who have aneurysms over 5.5 cm in diameter.
The second point is that we have now treated by endovascular grafting 17 patients with ruptured aortoiliac aneurysms (Ohki T, Veith FJ, Sanchez LA, et al. Endovascular repair of ruptured aortoiliac aneurysms. J Am Coll Surg 1999 [in press]). Some of these patients had contained ruptures, but several had no containment and were in shock when treated. Yet 15 of these 17 patients survived.
We therefore believe that endovascular grafting has the potential for lowering the unacceptably high mortality for standard surgical treatment of ruptured aortic aneurysms. However, this remains to be proven.
Presenter Dr. Roger M. Greenhalgh (London, England): Dr. Veith, you asked which operation should we perform in aneurysms less than 5.5 cm. Well, certainly we must examine more carefully which females might benefit. And in this regard, I draw our attention to the unreliability of ultrasound to measure the suprarenal diameter.
It would perhaps be sensible to use the ratio of infrarenal to suprarenal ratio, but we have to do that by another modality than ultrasound. I believe that will point the way forward to show which females should be operated upon. But I am sure there will be a new threshold. But I will comment to you that even females could be persuaded to stop smoking and have their blood pressure controlled also.
Dr. William C. Krupski (Denver, Colorado): Professor Greenhalgh, I enjoyed your presentation very much. On several occasions you mentioned the marginally fit patient. I would like to address this issue.
As you know, the ADAM trial is the U.S. equivalent of the U.K. Small Aneurysm Trial, and although the final results of that trial remain to be analyzed, several of us have noted that during the course of watchful waiting many patients have become very high-risk patients. They have developed congestive heart failure, their FEV1s have decreased, etcetera.
I wonder if you have analyzed this in the watchful waiting group? Because many of the patients who were originally good candidates for surgery have become unacceptable candidates during the watchful waiting period in certain U.S. centers in the ADAM trial.
Dr. Greenlhalgh: Thank you, Dr. Krupski, for your comments. We all eagerly await the ADAM trial results.
I would say to you that we set up the U.K. Small Aneurysm Trial with the supposition that it was obviously more sensible to operate upon younger patients with small aneurysms at an earlier stage in the natural history. All I can say to you is our data did not support that expectation. And the results that I have shown you of surgeons performing aortic aneurysm surgery from all over our country produced the results which I have shown you, which I believe does not support an early intervention. That, therefore, means that despite the fact that some patients will get older and less fit, nevertheless, those are the data, which I think are very robust.
Dr. Jack L. Cronenwett (Lebanon, New Hampshire): Professor Greenhalgh, this is an extremely important paper because it helps us to apply the overall results of your initial U.K. Small Aneurysm Study to the individual patient.
The question that I have for you relates to a long-standing interest in the impact of chronic pulmonary disease on aneurysms. In the U.K. study I believe that you showed COPD was an important risk factor for poor outcome from surgery. So I wondered if you have analyzed the relative risk of chronic pulmonary disease on operative risk versus aneurysm rupture risk, and you can tell us on which side of the equation the majority of risk falls?
Dr. Greenhalgh: Dr. Cronenwett, it is good to hear you at the microphone, and we have taken great note of your writings and findings.
We did find in our study a strong correlation between pulmonary function and current smoking habits. So they went together. As we summated the study with the trial, we were concerned that there may be problems with all of that. So we re-ran the analysis on the trial alone. And for everything but lung function, all of the independent variables showed up. Smoking didn’t show up. But then we have been reminded from our earlier work that smokers in Britain are sometimes economical with the truth. So we performed cotinine analyses. Then assessing smoking by marker, even in the trial smoking did relate as an independent variable, even within those small trial patients, did relate to rupture. So I think that throughout, the smoking certainly and as that relates to lung function, we think that is a very robust endpoint.
Yes, there is a risk of increased mortality performing surgery from lung function. We haven’t been able to analyze the effect of that and relate it in the way that you would like.
Dr. Rodney A. White (Torrance, California): Did you look at growth rate as an independent factor? This has been found to be predictive in the past.
Dr. Greenhalgh: By regression analysis we are looking at growth rates. But that will be the subject of a further analysis and presentation and publication in due course. We are finding—the analysts and statisticians are finding—the analysis of growth rate a tricky one. It has always been programmed that we should do it, but it is taking a lot of effort to get that done very accurately. But we will return to growth rate in due course.
Dr. Lazar J. Greenfield (Ann Arbor, Michigan): One of the variables that has been talked about in this country is the presence of thrombus in the aneurysm as being associated with a perhaps slightly higher risk. Was that analyzed?
Dr. Greenhalgh: Not as such.
Footnotes
Correspondence: Janet T. Powell, MD, Dept. of Vascular Surgery, Imperial College at Charing Cross, St. Dunstan’s Road, London W6 8RP, United Kingdom.
Presented by Roger M. Greenhalgh, MD, at the 119th Annual Meeting of the American Surgical Association, April 15–17, 1999, Hyatt Regency Hotel, San Diego, California.
The U.K. Small Aneurysm Trial was supported by the Medical Research Council, the British Heart Foundation, and the Camelia Botnar Foundation.
Reprints will not be available from the authors.
Accepted for publication April 1999.
References
- 1.Bradbury AW, Makhdoomi KR, Adam DJ, et al. Twelve-year experience of the management of ruptured abdominal aortic aneurysm. Br J Surg 1997; 84: 1705–1707. [PubMed] [Google Scholar]
- 2.Johnson KW. Ruptured abdominal aortic aneurysm. 6-year follow-up results of a multicenter prospective study. J Vasc Surg 1994; 19: 888–900. [DOI] [PubMed] [Google Scholar]
- 3.U.K. Small Aneurysm Trial Participants. Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet 1998; 352: 1649–1655. [PubMed] [Google Scholar]
- 4.Lederle FA. Risk of rupture of large abdominal aortic aneurysm. Arch Intern Med 1996; 156: 1007–1009. [PubMed] [Google Scholar]
- 5.Darling RC. Ruptured arteriosclerotic abdominal aortic aneurysms: a pathologic and clinical study. Am J Surg 1970; 119: 397–401. [DOI] [PubMed] [Google Scholar]
- 6.Turk KAD. The post-mortem incidence of abdominal aortic aneurysm. Proc Roy Soc Med 1965; 58: 869–870. [PMC free article] [PubMed] [Google Scholar]
- 7.Nevitt MP, Ballard DJ, Hallett JW. Prognosis of abdominal aortic aneurysms: a population-based study. N Engl J Med 1989; 321: 1009–1014. [DOI] [PubMed] [Google Scholar]
- 8.Ellis M, Powell JT, Greenhalgh RM. The limitations of ultrasonography in surveillance of abdominal aortic aneurysms. Br J Surg 1991; 78: 614–616. [DOI] [PubMed] [Google Scholar]
- 9.Reed WW, Hallett JW, Damiano MA, Ballard DJ. Learning from the last ultrasound. A population-based study of patients with abdominal aortic aneurysm. Arch Intern Med 1997; 157: 2064–2068. [DOI] [PubMed] [Google Scholar]
- 10.Scott RA, Tisi PV, Ashton MA, Allen DR. Abdominal aortic aneurysm rupture rates: a 7-year follow-up of the entire abdominal aortic aneurysm population detected by screening. J Vasc Surg 1998; 28: 124–128. [DOI] [PubMed] [Google Scholar]
- 11.Cronenwett JL, Murphy TF, Zelenock GB, et al. Actuarial analysis of variables associated with rupture of small abdominal aortic aneurysms. Surgery 1985; 98: 472–483. [PubMed] [Google Scholar]
- 12.Michaels JA. The management of small abdominal aortic aneurysms: a computer simulation using Monte Carlo methods. Eur J Vasc Surg 1992; 6: 551–557. [DOI] [PubMed] [Google Scholar]
- 13.U.K. Small Aneurysm Trial Participants. The U.K. Small Aneurysm Trial: design, methods and progress. Eur J Vasc Endovasc Surg 1995; 9: 42–48. [DOI] [PubMed] [Google Scholar]
- 14.Sonesson B, Hansen F, Stale H, Lanne T. Compliance and diameter in the human abdominal aorta—the influence of age and sex. Eur J Vasc Surg 1993; 7: 690–697. [DOI] [PubMed] [Google Scholar]
- 15.MacSweeney STR, Ellis M, Worrell PC, Greenhalgh RM, Powell JT. Smoking and growth rate of small abdominal aortic aneurysms. Lancet 1994; 344: 651–652. [DOI] [PubMed] [Google Scholar]
- 16.Hammond EC, Garfinkel L. Coronary heart disease, stroke and abdominal aortic aneurysm. Arch Environ Health 1967; 19: 167–182. [PubMed] [Google Scholar]
- 17.Strachan DP. Predictors of death from aortic aneurysm among middle-aged men: the Whitehall Study. Br J Surg 1991; 78: 401–404. [DOI] [PubMed] [Google Scholar]