Abstract
Objective
To propose a simple and minimally invasive approach for parathyroid surgery.
Summary Background Data
Minimally invasive approaches to the parathyroid glands may involve preoperative morphologic explorations, perioperative biologic controls, or videocervicoscopy, a new method.
Methods
The authors describe 597 patients who underwent parathyroidectomy through an original bilateral oblique approach between 1976 and 1997. None underwent morphologic exploration or biologic perioperative monitoring. In primary hyperparathyroidism, the four glands are controlled and it is possible to check their abnormalities of location or number. In secondary hyperparathyroidism and multiple endocrine neoplasia (MEN), a total or subtotal parathyroidectomy is performed.
Results
The results and vocal morbidity are the same as that from authors using transverse cervicotomy, but this approach is more comfortable for the patient and allows total exploration of the location through short incisions without bleeding, visceral contusions, or muscle lesion.
Conclusions
This cervicotomy is easy and secure even if the surgeon is not trained in this approach because it uses and respects the anatomy of the cervical fasciae. It can be used without preoperative localization, intraoperative monitoring, or specialized material. But this approach could be also proposed for unilateral exploration guided by these methods and for surgical treatment of recurrent hyperparathyroidism after a transverse cervicotomy.
Since Cope in 1941, the surgical approach to the parathyroid glands has generally used the same transverse low cervicotomy used for cervical endocrine surgery. 1 Exposure of the dorsal part of the thyroid lobe is difficult during this dissection because of the adhesions between the infrahyoid muscles and the capsule of the thyroid gland. Esselstyn 2 and Chigot 3 transversally cut these muscles; Edis, 4 Proye, 5, and Demard 6 opened the linea alba of the neck and separated the left and right muscles. In 1975, Dubost proposed to go around the lateral edge for reoperations in hyperparathyroidism. 7 Stevens proposed it for all surgical approaches to parathyroid glands. 8 Chapuis performed a unilateral approach under local anesthesia, guided by preoperative localization and intraoperative biologic monitoring; this approach requires a transverse or oblique skin incision and a transverse incision of the infrahyoid muscles. 9 More recently, endoscopic procedures have been introduced with or without carbon dioxide insufflation to perform the same unilateral exploration. 10,11 Only a few authors perform videocervicoscopy for this indication; the results of these preliminary studies and initial experience are presented here.
It is possible to avoid infrahyoid dissection by using a double lateral approach that gives direct, specific, and bloodless access. We have used this technique since 1976, and it has been applied since 1978 to all the operations for hyperparathyroidism in the Service de Chirurgie Generale et Thoracique. We describe here the surgical technique of a minimally invasive parathyroidectomy with a complete neck exploration and its anatomic basis as an alternative method of the endoscopic approach.
OPERATIVE TECHNIQUE
The patient is placed in a supine position with the upper limbs in adduction. The surgeon stands on the side to be explored, in front of the assistant. They reverse places for the exploration of the second side of neck. The cervical column is placed in a neutral position without any rotation or extension.
The bilateral cervicotomy requires two symmetrical incisions, each starting 2 cm above and outside the medial joint of the clavicle. The incisions ascend in an oblique upward direction to cross the medial ledge of sternocleidomastoid muscle, and are 3 or 4 cm in length on the bisector between the medial edge of sternocleidomastoid muscle and the upper edge of the clavicle. They resemble the lateral extensions of a classic low transverse cervicotomy (Fig. 1).
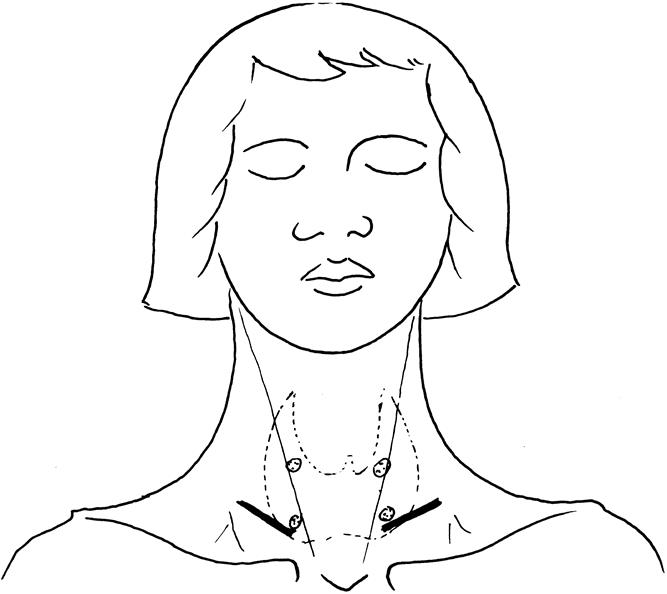
Figure 1. Bilateral oblique cervicotomy needs two symmetrical incisions and dissections.
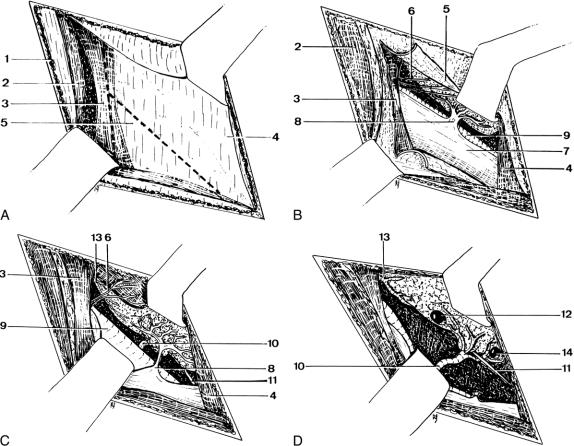
The skin, superficial fascia of the neck, and platysma are cut without any elevation. The investing layer of the deep cervical fascia is incised on the medial ledge of the sternocleidomastoid muscle, which is pulled out with a retractor; the omohyoid muscle appears through the posterior layer of the fascia superficialis (Fig. 2A). The operative field shows only the superior belly or the intermediate tendon of the omohyoid muscle. The internal jugular vein is visible through the pretracheal layer of the deep cervical fascia tightened by this muscle, and its transparency often shows the efferent nerves of the ansa cervicalis.
Figure 2. Operative technique on the right side of the neck: (A) the omohyoid and infrahyoid muscles appear through the fascia superficialis; (B) incision of the deep cervical fascia (fascia pretrachealis); (C) opening of the visceral sheath; (D) exploration of the parathyroid glands after ligation and section of a middle thyroid vein. 1, platysma; 2, sternocleidomastoid muscle; 3, omohyoid muscle; 4, infrahyoid muscles; 5, fascia cervicalis pretrachealis; 6, efferent nerves of the ansa cervicalis; 7, internal jugular vein; 8, middle thyroid vein; 9, common carotid artery; 10, inferior thyroid artery; 11, recurrent laryngeal nerve; 12, parathyroid gland PIV; 13, superior thyroid artery; 14, parathyroid gland PIII.
The pretracheal layer of the deep cervical fascia is incised on the omohyoid muscle, in a parallel direction with its inferior ledge. This incision then goes on in a T form to the lower and medial part of the fascia, in a direction parallel with the carotid sheath (Fig. 2B).
The two divergent retractors separate the carotid sheath from the infrahyoid muscles and their motor nerves and so protect them. The ansa cervicalis is generally hidden above and behind the omohyoid muscle itself, but when it appears and crosses the operative field, the retractor brings it nearer and under the omohyoid muscle. The exposure may be restricted by a middle thyroid vein, which is often tight between the internal jugular vein and the thyroid gland. It is sometimes necessary to link and to cut it; this would then be the only hemostasis in this approach.
The visceral sheath is opened close to the thyroid gland, and the medial retractor lifts the lobe to expose its posterior side (Fig. 2C). The inferior thyroid artery crosses the background of the operative field through the opened tissue plane. It can be stretched by a vessel loop close to the common carotid artery to expose the recurrent laryngeal nerve (Fig. 2D). In this space, it is possible to explore the inferior arterial pedicle, the superior pedicle, the thyroid capsule of the entire lobe, and also the thymus, the esophagus, and the carotid sheath, but only by traction and countertraction using the two retractors. A thymectomy can be performed after ligation of the thymic veins under the left brachiocephalic vein. A hemithyroidectomy can also be performed because the pedicles and the recurrent laryngeal nerve are exposed.
If necessary, a suction drain can be left close to the vascular sheath at the end of the exploration. Then only the platysma and the skin are sutured.
In our experience of hyperparathyroidism, both sides are systematically explored to control the four glands and to be able to check their abnormalities of location or number. An intraoperative histopathologic examination of the resected tissue was systematically used. For secondary hyperparathyroidism or multiple endocrine neoplasia (MEN) and for all the cases of hyperplasia, a subtotal parathyroidectomy with cervical thymectomy and cryopreservation of resected parathyroid tissue was performed.
MATERIAL AND METHOD
Between 1976 and 1997, 597 parathyroidectomies were performed in our department through this bilateral oblique approach. Four hundred thirty patients were treated for primary hyperparathyroidism (range 15–99 years, average 57); MEN types of hyperparathyroidism occurred in 13 of these patients. One hundred sixty-seven patients were treated for secondary or tertiary hyperparathyroidism (range 13–84 years, average 49). One patient simultaneously underwent treatment of primary hyperparathyroidism and a diverticulum of the cervical esophagus.
Two patients high-risk but cooperative patients with severe hypercalcemia underwent unilateral exploration under local anesthesia. In these cases only, the side of the cervicotomy was guided by a preoperative ultrasonography, with successful results.
Bilateral suction drainage was systematically used during the first 10 years of our experience (1976–1987). During the last 10 years (1987–1997), drainage was always bilateral but used only in cases of hemorrhage in the field of a difficult cervical thymectomy or if the patient had hemostasis abnormalities. This drainage was removed on the second postoperative day.
RESULTS
Mean operative time was 62 minutes for primary hyperparathyroidism, 87 minutes for secondary hyperparathyroidism, and 74.4 minutes for hyperparathyroidism. Bilateral drainage was used in 157 cases (26.3%). Mean postoperative hospital stay was 2.8 days. Table 1 summarizes the results and the operative mortality and morbidity. Recurrent laryngeal nerve paralysis was demonstrated by laryngoscopy; a second laryngoscopy 1 month after operation separated definitive from transitory paralysis. The nine patients with postoperative hematoma needed neither reoperation nor drainage; one of the three suppurations concerned the patient who underwent resection of an esophageal diverticulum. None of the suppurations required reoperation.
Table 1. RESULTS AND MORBIDITY OF INTERVENTIONS FOR HYPERPARATHYROIDISM*
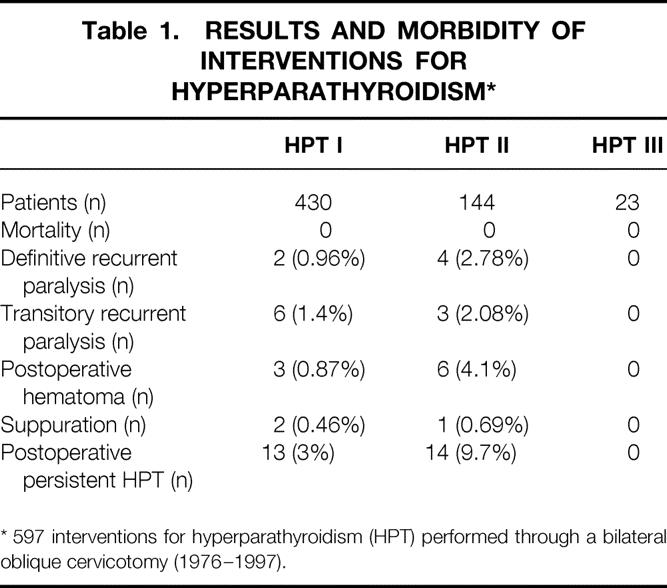
* 597 interventions for hyperparathyroidism (HPT) performed through a bilateral oblique cervicotomy (1976–1997).
Single parathyroid adenomas were found in 357 patients (83%), double adenomas in 13 patients (3.01%; bilateral adenomas in 8 cases), and parathyroid hyperplasia in 60 patients (13.9%). Finally, a bilateral lesion of the parathyroid glands was found in 68 patients (15.8%) including MEN (13 cases).
Two adenomas were found in a thyroid lobe (0.46%). They were very large tumors (3 g and 4 g) suspected through the thyroid tissue at the end of the exploration. They were resected by lobectomy to avoid capsular rupture. Twelve adenomas were found in the thymus (2.8%). One adenoma was found in the retroesophageal space in the mediastinum.
DISCUSSION
Works on parathyroid surgery are numerous, but they deal mainly with the difficulties presented by the morphologic and topographic variations of these glands. The chosen approach is rarely discussed, and is often not even mentioned because the transverse cervicotomy common with thyroid surgery has imposed itself on parathyroid surgery.
Once under the superficial aponeurosis, it is possible to follow the linea alba and to separate the left and right infrahyoid muscles in order to mobilize the whole of the thyroid gland, but it is also possible to reach the visceral lodge of the neck outside the infrahyoid muscles. Only a few authors, for unilateral approaches, seem to use oblique incisions borrowed from surgery of the carotid artery. We are not aware of other publications describing precisely this bilateral oblique approach to the parathyroid glands in its spaces of clivage and relationships.
We have used this cervicotomy in our department since 1976 and it has been performed systematically for all parathyroid surgery since 1978. 12 Our exploration systematically researches the four parathyroid glands, whatever the information given by preoperative imagery (which is not ordered in our department if the patient has not previously undergone cervicotomy). The choice of this bilateral exploration is principally guided by the high rate of bilateral lesions. The literature shows a wide range of prevalence of multiple adenomas and hyperplasia, averaging respectively 2.2% and 14% in the analysis of Duh et al, 13 and 3.01% and 13.9% in our series. This choice is also guided by the morbidity of reoperations for persistent hyperparathyroidism. Because the rate of recurrent nerve palsy in these reoperations is 3% to 10%, 14,15 we prefer the most complete surgical exploration the first time.
This approach provides a direct opening on the sites of research for parathyroid glands. It enables an exploration of the unusual locations of parathyroid glands: retroesophageal or posterior mediastinal glands, glands included in the jugulocarotid sheath, and intrathymic or intrathyroidian glands. A thyroidian lobectomy is, in fact, easy to perform through this approach because the superior and inferior pedicles are exposed along with the recurrent laryngeal nerve. When the patient is short or has a short rachidian extension, the exposition is modified by the depth of the operative field, whatever the chosen approach, but we think that a lateral approach is less dependent on the gnathosternal distance than a classic approach. This method without rachidian extension may improve the comfort of the patient if local anesthesia is used, and it reduces postoperative nuchal rigidity in all cases. Our results show that the bilateral oblique approach gives the same wide exploration of the neck as a large transverse cervicotomy. For primary hyperparathyroidism, our results are very similar to those reported in the literature. The surgical procedure is successful in 90% to 98% of cases in the literature, and in 97% in our series. 16,17 The frequency of multiple adenomas is about 2.2% for Duh et al and 3.01% in our series. 13 For secondary hyperparathyroidism, we consider only the early postoperative result of the subtotal parathyroidectomy: the frequency of the persistent hyperparathyroidism is 6.6% for the total parathyroidectomy and 5.8% for the subtotal parathyroidectomy in the analysis of Rothmund, and 9.7% in our series. 18
This approach is cosmetically acceptable because the incisions are short and symmetrical, placed on supple and mobile skin far from prominent margins of bone. They are parallel to the cleavage lines of the skin and the scars are almost invisible 1 month after surgery.
The approach is bloodless as all the parathyroid surgery must be. Here more than anywhere else, the dissection uses the color of living tissue to bring the parathyroid glands into evidence. The technique follows the fibrous spaces of the neck without detachment. Ligation of a middle thyroid vein is the only hemostasis that is sometimes necessary, if the vein is too short or is placed in the center of the operative space. For primary hyperparathyroidism, significant wound hematomas or infections occur in 0% to 3% of cases in the literature, and in 1.33% in our series. 16,17 This hemostasis problem is even greater in case of thymectomy for secondary hyperparathyroidism because chronic renal insufficiency always accompanies defects of platelet aggregation. In our series of secondary hyperparathyroidism, these hematomas are found in 4.1% of cases. This rate seems higher than expected, but we have been unable to find other results in the literature about secondary hyperparathyroidism. Kerby reports 2.6% of wound separation for 38 cases of tertiary hyperparathyroidism. 19
The approach causes little trauma because it uses the fibrous sheaths of the neck while respecting their content. The jugular and carotid vessels are easily observed while remaining protected in their sheath and are not subjected to strong traction by the retractors. The thyroid gland also remains in its sheath, undissected, except in cases where the parathyroid gland is included in the parenchyma or under the capsule. Further thyroid surgery can then be performed without difficulty through a classic transverse cervicotomy free of adherences. During the search for the parathyroid glands themselves, this cervicotomy enables a better control of the inferior thyroid artery and the recurrent laryngeal nerve than does an anterior approach. The nerve is exactly checked before any upward or downward extension. The lateral approach does not seem to modify the rate of vocal cord paralysis: definitive recurrent paralysis in the surgical treatment of the primary hyperparathyroidism occurs in 0% to 1.5% in the literature, and in 0.96% in our series. 16,17 To the contrary, the frequency of paralysis in our series of secondary hyperparathyroidism seems rather high (2.78%) but to our knowledge, this rate is not given in the literature. Kerby reported 2.6% vocal cord hemiparesis for 38 cases of tertiary hyperparathyroidism. 19 Complete dissection and resection of the thymus and the four glands is more aggressive than a simple exploration, so surgical complications are probably the same for secondary or tertiary hyperparathyroidism.
Only the ansa cervicalis and its motor nerves aimed at the infrahyoid muscles appear particularly endangered by this technique. If that was the case, the lesions would be even more serious when there is a bilateral and symmetrical approach. Following Liguoro’s conclusions about the anatomic basis of the anterior cervical spine approach, respect for the motoricity of the infrahyoid muscles is necessary, not only because they are accessory breathing muscles but also because of their part in phonation: they modify the ring of the voice by lowering the larynx. 20 A unilateral paralysis of the infrahyoid muscles remains discreet or inaudible, but it is different if the lesion is bilateral or if the patient’s profession depends on the use of his or her voice (e.g., singers). In a series of 80 dissections of the cervical plexus, Caliot showed that the apex of the ansa cervicalis is above or behind the omohyoid muscle in 85% of cases. 21 A long ansa is noted in 15% of cases but always close to the inferior border of the muscle. Chhetri reported the same results in a recent review of the literature. 22 Caliot described a symmetrical appearance of the ansa cervicalis in only 12% of cases. 21 These anatomic results lead to following conclusions:
• A T-shaped incision of the pretracheal layer of fascia is generally more caudal than the apex of the loop.
• If the ansa cervicalis is a long one, it will be perfectly shown and protected by this incision.
• The retractor that lifts the thyroid lobe inwardly and forward protects the nerve branches aimed at the sternohyoid and sternothyroid muscles.
These comments demonstrate that the oblique approach is an easy and secure method of neck exploration for all cases of hyperparathyroidism. Our minimally invasive technique must also be compared with videocervicoscopy, a new field of interest for surgery of the neck. This method is performed currently by only a few authors, with or without gas insufflation. 23–26 The literature about cervicoscopy shows that it is a feasible and effective procedure, but also that gas insufflation sometimes creates a massive subcutaneous emphysema or hypercarbia. 27 The morbidity of the gasless approach seems to be the same as in the classic approach, but the authors report only short series of primary hyperparathyroidism. Patients are generally selected on the basis of the following criteria: no goiter, no prior neck operations, and preoperative localization of an adenoma. 10 Cougard reported 17 cases of primary hyperparathyroidism who underwent cervicoscopy after preoperative localization. 25 In seven cases, a horizontal cervicotomy had to be performed: four failures of exploration, one hyperplasia of the four glands, one bleeding anterior jugular vein, and one thyroid cancer discovered incidentally during the operation. Contrary to the endoscopic approach, our method does not require expensive surgical materials or specialized training. It can be proposed for all cases of primary and secondary hyperparathyroidism. But these two methods are not really opposite: the anatomic basis described for our method could be used in the video-assisted technique for a lateral dissection of the working space.
CONCLUSION
Between 1976 and 1997, 597 parathyroidectomies were performed in our department with this bilateral oblique approach, a principle in primary hyperparathyroidism because it is necessary to control the four glands and be able to check their abnormalities of location or number. The bilateral approach is necessary in secondary hyperparathyroidism and MEN to perform a total or subtotal parathyroidectomy. Results and morbidity are the same as those of authors using the transverse cervicotomy, but this approach is comfortable for the patient and allows total exploration of the location through short incisions without bleeding, visceral contusions, or muscle lesion. It is an easy and secure procedure even if the surgeon is not trained for this approach because it uses and respects the anatomy of the cervical fasciae. It can be used without preoperative localization and intraoperative monitoring. But this approach could be also proposed for an unilateral exploration guided by these methods and for the surgical treatment of the recurrent hyperparathyroidism after a transverse cervicotomy.
Footnotes
Correspondence: Philippe C.J. Chaffanjon, MD, Service de Chirurgie Générale et Thoracique, Centre Hospitalier et Universitaire de Grenoble, BP217, 38043 Grenoble Cedex, France.
Accepted for publication July 26, 1999.
References
- 1.Cope O. Surgery of hyperparathyroidism: the occurrence of parathyroids in the anterior mediastinum and the division of the operation into two stages. Ann Surg 1941; 114:706–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esselstyn CB Jr, Levin HS. A technique for parathyroid surgery. Surg Clin North Am 1975; 55:1047–1063. [DOI] [PubMed] [Google Scholar]
- 3.Chigot PL. Chirurgie de l’hyperparathyroidisme. J Chir 1967; 93:579–596. [PubMed] [Google Scholar]
- 4.Edis AJ. Surgical anatomy and technique of neck exploration for primary hyperparathyroidism. Surg Clin North Am 1977; 57:495–504. [DOI] [PubMed] [Google Scholar]
- 5.Proye C. Exploration parathyroidienne pour hyperparathyroidie. J Chir 1978; 115:101–106. [PubMed] [Google Scholar]
- 6.Demard F, Santini J, Serra C, et al. Traitement chirurgical de l’hyperparathyroïdie primaire. J Fr Otorhinolaryngol 1990; 39:27–35. [Google Scholar]
- 7.Dubost C. Hyperparathyroidie. Les reinterventions. J Chir 1975; 110:179–192. [PubMed] [Google Scholar]
- 8.Stevens JC. Lateral approach for exploration of the parathyroid gland. Surg Gynecol Obstet 1979; 148:431–432. [PubMed] [Google Scholar]
- 9.Chapuis Y, Ycard P, Fulla Y, et al. Parathyroid adenomectomy under local anesthesia with intraoperative monitoring of UcAMP and/or 1-84 PTH. World J Surg 1992; 16:570–575. [DOI] [PubMed] [Google Scholar]
- 10.Miccoli P, Bendinelli C, Vignali E, et al. Endoscopic parathyroidectomy: report of an initial experience. Surgery 1998; 124:1077–1080. [DOI] [PubMed] [Google Scholar]
- 11.Brunt LM, Jones DB, Wu JS, Quasebarth MA, Meininger T, Soper NJ. Experimental development of an endoscopic approach to neck exploration and parathyroidectomy. Surgery 1997; 122:893–901. [DOI] [PubMed] [Google Scholar]
- 12.Sarrazin R, Chaffanjon PCJ, Brichon PY, Eymard P. Voie d’abord latérale oblique des glandes parathyroides. Lyon Chir 1996; 92:380–382. [Google Scholar]
- 13.Duh QY, Udén P, Clark OH. Unilateral neck exploration for primary hyperparathyroidism: analysis of a controversy using a mathematical model. World J Surg 1992; 16:654–662. [DOI] [PubMed] [Google Scholar]
- 14.Grant CS, van Heerden JA, Charbonean IW, James EM, Reading CC. Clinical management of persistent and/or recurrent primary hyperparathyroidism. World J Surg 1986; 10:555–565. [DOI] [PubMed] [Google Scholar]
- 15.Patow CA, Norton JA, Brennan MF. Vocal cord paralysis and reoperative parathyroidectomy. Ann Surg 1986; 203:282–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg 1991; 15:688–692. [DOI] [PubMed] [Google Scholar]
- 17.Henry JF, Denizot A. Cervicotomie premiere pour hyperparathyroidisme primaire. In: Barbier H, Henry JF. L’hyperparathyroidisme primaire. Rapport present au 93e Congres Français de Chirurgie. Paris: Springer-Verlag; 1991: 75–98.
- 18.Rothmund M, Wagner PK, Schark C. Subtotal parathyroidectomy versus total parathyroidectomy and autotransplantation in secondary hyperparathyroidism: a randomized trial. World J Surg 1991; 15:745–750. [DOI] [PubMed] [Google Scholar]
- 19.Kerby JD, Rue LW, Blair H, Hudson S, Sellers MT, Diethlem AG. Operative treatment of tertiary hyperparathyroidism: a single-center experience. Ann Surg 1998; 227:878–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liguoro D, Vital JM, Guerin J, Senegas J. Anatomical basis of the anterior cervical spine approach: topographic study of the nerve structure. Surg Radiol Anat 1992; 14:203–208. [DOI] [PubMed] [Google Scholar]
- 21.Caliot P, Dumont D, Bousquet V, Midy D. A note on the anastomoses between the hypoglossal nerve and the cervical plexus. Surg Radiol Anat 1986; 8:75–79. [DOI] [PubMed] [Google Scholar]
- 22.Chhetri DK, Berke GS. Ansa cervicalis nerve: review of the topographic anatomy and morphology. Laryngoscope 1997; 107:1366–1372. [DOI] [PubMed] [Google Scholar]
- 23.Miccoli P, Bendinelli C, Conte M, Pinchera A, Marcocci C. Endoscopic parathyroidectomy by a gasless approach. J Laparoendosc Adv Surg Tech A 1998; 8:189–194. [DOI] [PubMed] [Google Scholar]
- 24.Yeung GH. Endoscopic surgery of the neck: a new frontier. Surg Laparosc Endosc 1998; 8:227–232. [PubMed] [Google Scholar]
- 25.Cougard P, Goudet P, Osmak L, Ferrand L, Letourneau B, Brun JM. Videocervicoscopy in surgery of primary hyperparathyroidism: preliminary study of 19 patients. Ann Chir 1998; 52:885–889. [PubMed] [Google Scholar]
- 26.Naitoh T, Gagner M, Garcia Ruiz A, Heniford BT. Endoscopic endocrine surgery in the neck: an initial report of endoscopic subtotal parathyroidectomy. Surg Endosc 1998; 12:202–206. [DOI] [PubMed] [Google Scholar]
- 27.Gottlieb A, Sprung J, Zheng XM, Gagner M. Massive subcutaneous emphysema and severe hypercarbia in a patient during endoscopic transcervical parathyroidectomy using carbon dioxide insufflation. Anesth Analg 1997; 84:1154–1156. [DOI] [PubMed] [Google Scholar]