Abstract
Objective
In this randomized trial, the authors sought to determine whether eradication of Helicobacter pylori could reduce the risk of ulcer recurrence after simple closure of perforated duodenal ulcer.
Background Data
Immediate acid-reduction surgery has been strongly advocated for perforated duodenal ulcers because of the high incidence of ulcer relapse after simple patch repair. Although H. pylori eradication is now the standard treatment of uncomplicated and bleeding peptic ulcers, its role in perforation remains controversial. Recently a high prevalence of H. pylori infection has been reported in patients with perforations of duodenal ulcer. It is unclear whether eradication of the bacterium confers prolonged ulcer remission after simple repair and hence obviates the need for an immediate definitive operation.
Methods
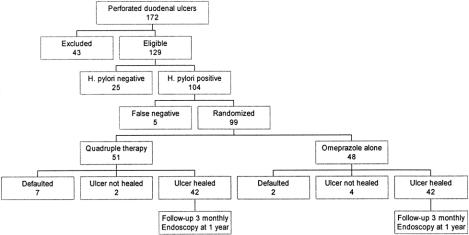
Of 129 patients with perforated duodenal ulcers, 104 (81%) were shown to be infected by H. pylori. Ninety-nine H. pylori-positive patients were randomized to receive either a course of quadruple anti-helicobacter therapy or a 4-week course of omeprazole alone. Follow-up endoscopy was performed 8 weeks, 16 weeks (if the ulcer did not heal at 8 weeks), and 1 year after hospital discharge for surveillance of ulcer healing and determination of H. pylori status. The endpoints were initial ulcer healing and ulcer relapse rate after 1 year.
Results
Fifty-one patients were assigned to the anti-Helicobacter therapy and 48 to omeprazole alone. Nine patients did not undergo the first follow-up endoscopy. Of the 90 patients who did undergo follow-up endoscopy, 43 of the 44 patients in the anti-Helicobacter group and 8 of the 46 in the omeprazole alone group had H. pylori eradicated; initial ulcer healing rates were similar in the two groups (82% vs. 87%). After 1 year, ulcer relapse was significantly less common in patients treated with anti-Helicobacter therapy than in those who received omeprazole alone (4.8% vs. 38.1%).
Conclusions
Eradication of H. pylori prevents ulcer recurrence in patients with H. pylori-associated perforated duodenal ulcers. Immediate acid-reduction surgery in the presence of generalized peritonitis is unnecessary.
The long-term results of omental patch repair for perforated duodenal ulcer are unsatisfactory; a high incidence of ulcer recurrence has been repeatedly reported. 1–4 Some advocate immediate acid-reduction procedures in addition to repair of the ulcer as a preventive measure against subsequent ulcer relapse. 5,6 Immediate definitive surgery in selected patients is safe, without increasing the rate of perioperative complications or death. 7 However, with recent advances in antiulcer medical therapy, fewer surgeons have acquired sufficient expertise in performing the definitive operation. Moreover, because perforated peptic ulcer isoften an “out of hours” emergency, a simpler life-saving procedure such as omental patch repair is an attractive option in many centers.
The recent rediscovery of Helicobacter pylori has revolutionized the therapeutic approach to peptic ulcer disease. Eradication of H. pylori heals most uncomplicated peptic ulcers and prevents relapse. 8–10 In the case of bleeding peptic ulcers, a short course of antibiotics eradicating H. pylori is as efficacious as maintenance acid-reduction medication in preventing recurrent ulcer hemorrhage. 11 Both the National Institute of Health Consensus Meeting and the Maastricht Meeting of the European Helicobacter pylori Study Group have recommended eradication of H. pylori as the standard treatment for uncomplicated and bleeding peptic ulcers. 12,13
However, the association between H. pylori and perforated duodenal ulcer is less well defined. The reported infection rates range widely, from 47% by serologic testing 14 to more than 80% in two recent biopsy-based studies. 15,16 Whether there is a causal relation between the bacterium and duodenal ulcer perforation is controversial. We therefore performed a prospective randomized trial to determine whether eradication of H. pylori could lead to sustained ulcer remission in patients who underwent only simple repair for duodenal ulcer perforation.
METHODS
Patients
Patients with clinical or radiologic signs of perforated peptic ulcers were considered for inclusion in the study. The study was approved by the Ethics Committee of the Faculty of Medicine, The Chinese University of Hong Kong. Informed consent was obtained for surgical exploration, intraoperative per oral gastroscopy, and possible enrollment into the study if infected with H. pylori. Exclusion criteria were age younger than 16 or older than 75 years, use of antibiotics or acid-suppressing medications within 4 weeks before admission, previous gastrectomy or vagotomy, pregnancy, sealed-off perforation, and inpatients in whom ulcer perforation developed while receiving treatment for other medical conditions.
Procedures
All patients received fluid resuscitation. Parenteral analgesics were prescribed for pain relief after the decision for surgical intervention was made. Informed consent was obtained for surgical exploration and possible enrollment into the study. Intravenous cefuroxime (1.5 g) was administered during induction of anesthesia. No other antibiotics or acid-suppressing medications were prescribed before surgery.
When duodenal ulcer perforation was confirmed by laparoscopy or laparotomy, intraoperative flexible gastroscopy (Q20, Olympus, Tokyo, Japan) was performed to obtain biopsy samples of the gastric antrum. Seven samples were obtained: one for rapid urease test (Campylobacter-Like Organism test [CLOtest], Delta West, West Australia), three in brain–heart–infusion medium for subsequent Gram stain and culture, and three in 10% buffered formalin for histologic examination.
Definition of H. pylori Status
Patients were considered to be H. pylori positive if any one of the following criteria was fulfilled: a positive culture, a positive CLOtest result plus gram-negative helical bacteria in the smear, or a positive CLOtest result plus helical microorganisms in histologic section of the gastric biopsy samples.
Surgery
Perforations less than 1 cm in diameter were repaired using the conventional open method or the laparoscopic technique, based on the surgeon’s discretion. Gastrectomy or other definitive acid-reduction procedures were considered only if patients had a large perforation (>1 cm in diameter) not amenable to simple omental patch repair or a perforation concomitant with hemorrhage or obstruction. After closure of the perforation, thorough peritoneal lavage with warm normal saline was performed before closure of the abdominal incision. After surgery, patients were cared for in designated surgical wards. Intravenous cefuroxime (750 mg) was continued every 8 hours for 3 days, and intravenous omeprazole (40 mg/day) was given until the patient resumed eating an oral diet.
Random Assignment to Treatment Groups
Only H. pylori-positive patients who had undergone patch repair were eligible for the randomization trial. After resuming an oral diet, patients were randomly assigned to one of the two treatment options by opening sealed envelopes that contained treatment options previously determined from a list of computer-generated random numbers. For the eradication group, a 1-week course of oral antibacterial treatment (bismuth subcitrate 120 mg, tetracycline 500 mg, and metronidazole 400 mg four times daily) plus 4 weeks of omeprazole (20 mg twice daily) was prescribed. Patients assigned to the control group were given a 4-week course of omeprazole alone. Compliance with treatment was monitored by phone inquiry and tablet count on follow-up by research nurses.
Follow-Up and Endoscopy
Endoscopy was scheduled 8 weeks after randomization and was performed by an endoscopist masked to the assigned treatment. Biopsy samples were again obtained from the gastric antrum to determine the patient’s H. pylori status. Additional biopsy samples were collected from body of the stomach to avoid false-negative results secondary to proximal migration of the bacterium after therapy. All patients with complete ulcer healing confirmed on scheduled endoscopy were then interviewed every 3 months by research nurses. Maintenance acid-suppression agents were not prescribed during the follow-up period. Repeat endoscopic examination was performed whenever patients were symptomatic. All patients were invited for a follow-up endoscopy at 1 year for ulcer surveillance and determination of H. pylori status.
For patients whose ulcers had not healed at 8 weeks, another 4-week course of omeprazole (20 mg twice daily) was prescribed, and a second endoscopy was scheduled at 16 weeks. Primary treatment failure was considered to be present if patients had persistent nonhealing ulcers at that point.
Sample Size and Statistical Analysis
There are few data regarding the effect of H. pylori eradication in perforated ulcer disease. Based on studies of uncomplicated ulcers, we estimated that ulcers would relapse in fewer than 5% of the patients with perforated duodenal ulcers after eradication of H. pylori. 8–10 Studies before the era of H. pylori revealed a median ulcer recurrence rate of 40% if only simple repair was performed for duodenal ulcer perforation. 2–4 To show a 35% difference of ulcer recurrence with a 5% type I error risk and a power of 0.8 in a two-sided model, a minimum of 43 patients in each arm was required. Anticipating a default rate of 10%, we decided to recruit at least 48 patients into each treatment group. The differences in initial ulcer healing and ulcer recurrence between the two groups of patients were studied by intention-to-treat analyses. Patients who did not appear for follow-up were contacted by phone to ask about symptoms. Those who were symptomatic but refused to undergo endoscopy and those who could not be contacted were considered as treatment failures. All statistical analyses were performed with GraphPad Prism version 2 (GraphPad Software, Inc., San Diego, CA). Chi-square with Yates correction and Fisher’s exact test were used to compare proportions when appropriate; continuous normally distributed numeric data were compared using the Student t test.
RESULTS
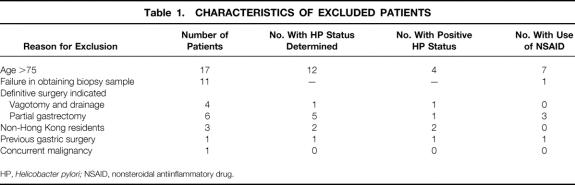
From September 1994 to January 1997, 172 patients (138 men and 34 women) with a mean age of 52.2 years (S.D. = 18.1) were confirmed to have duodenal ulcer perforation by laparoscopy or laparotomy (Fig. 1). Forty-three patients were not eligible for the study: 17 were older than 75 years, 10 required definitive operation, 7 failed endoscopic examination (equipment failure occurred with 5 patients, and the endoscopist could not pass the flexible endoscope through the cricopharyngeus when the other 2 patients were intubated), 4 refused to undergo intraoperative endoscopy, 3 did not live in Hong Kong (so long-term follow-up was not possible), 1 had disseminated malignancy, and 1 had a previous vagotomy (Table 1). Of the remaining 129 patients, 104 (80.6%) were infected with H. pylori. Five patients were not enrolled into the randomization study because the initial urease test and histology results were falsely negative. These five patients were prescribed a full course of eradication therapy on follow-up and were not included in the trial.
Figure 1. Trial profile.
Table 1. CHARACTERISTICS OF EXCLUDED PATIENTS
HP, Helicobacter pylori; NSAID, nonsteroidal antiinflammatory drug.
Of the remaining 99 patients, 51 were assigned to anti-Helicobacter therapy and 48 to omeprazole alone (see Fig. 1). The two groups were comparable in age, sex ratio, smoking habit, use of nonsteroidal antiinflammatory drugs (NSAIDs), previous ulcer history, size of perforation, severity of peritoneal contamination, and method of repair (Table 2). Ninety patients returned for follow-up endoscopy at 8 weeks. The dropout rate of the anti-Helicobacter group (seven patients: three had major side effects from the medication and four could not be contacted) exceeded that of the omeprazole group (two patients lost to follow-up), but the difference did not reach statistical significance (P = .16).
Table 2. CHARACTERISTICS OF PATIENTS
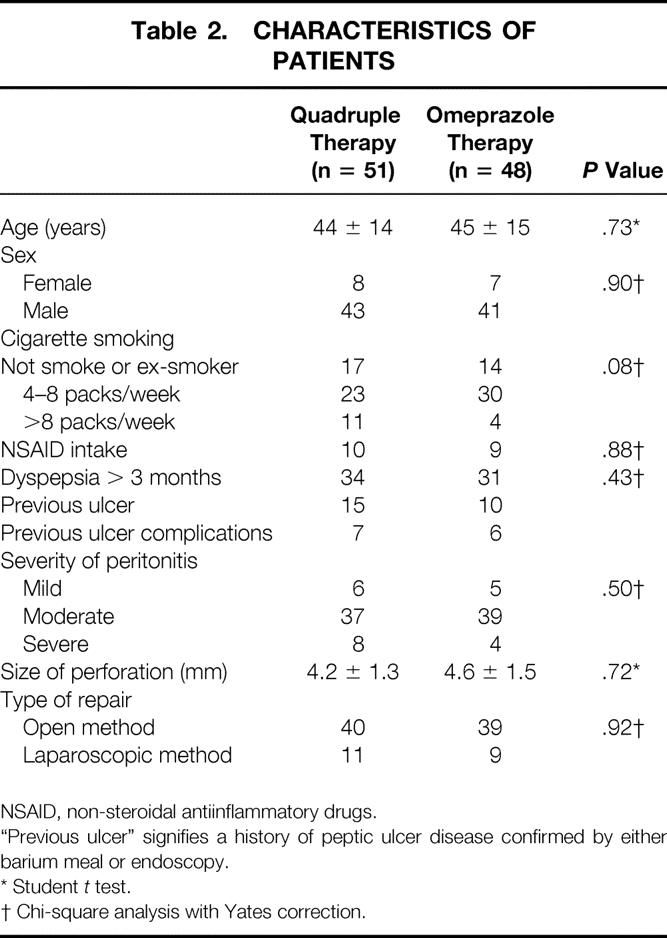
NSAID, non-steroidal antiinflammatory drugs.
“Previous ulcer” signifies a history of peptic ulcer disease confirmed by either barium meal or endoscopy.
* Student t test.
† Chi-square analysis with Yates correction.
As expected, the H. pylori eradication rate of the anti-Helicobacter treatment group was significantly higher than that of the omeprazole alone group (84.3% vs. 16.7%, P < .001). Eight patients in the omeprazole alone group had inadvertent eradication of H. pylori (Table 3). When case records were reviewed, seven of these eight patients had received extra antibiotics, including ampicillin or metronidazole (both are effective antibiotics for eradication of H. pylori) in the early postoperative period because of persistent fever or other septic conditions.
Table 3. EARLY OUTCOMES
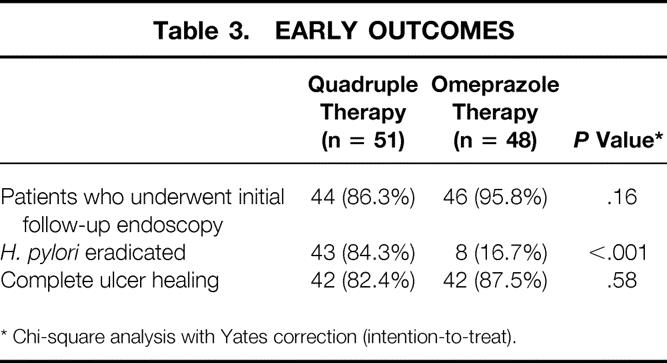
* Chi-square analysis with Yates correction (intention-to-treat).
Initial healing of ulcers was comparable between the two groups (see Table 3). There were six nonhealing ulcers despite repeated courses of omeprazole, two in the anti-Helicobacter group and four in the omeprazole group. Complete ulcer healing was documented in 42 patients in each arm (P = .58). Patients with documented ulcer healing were scheduled for follow-up according to the study protocol.
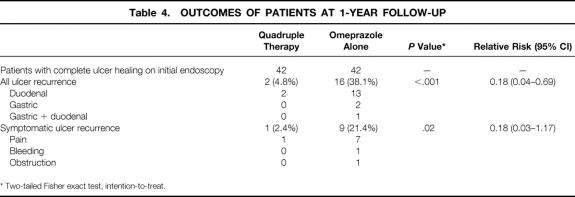
After 1 year, two patients in the anti-Helicobacter group and four in the omeprazole group were lost to follow-up (Table 4). They reported no significant dyspeptic symptoms and refused to undergo further endoscopic examination when contacted by phone. Of the remaining 78 patients who followed the study protocol strictly, 18 had ulcer recurrence (see Table 4).
Table 4. OUTCOMES OF PATIENTS AT 1-YEAR FOLLOW-UP
* Two-tailed Fisher exact test, intention-to-treat.
Two patients in the anti-Helicobacter group had ulcer relapse: one patient had profound duodenal ulcer bleeding 7 months after the index perforation and was subsequently found to have recurrent H. pylori infection; the other one was asymptomatic and had recurrent ulcer diagnosed at the scheduled 1-year endoscopy. Of the 16 patients with ulcer recurrence in the omeprazole alone group, 9 were symptomatic. Four patients returned before the scheduled endoscopy at 1 year: two with severe ulcer pain, one with bleeding, and one with gastric outlet obstruction. The difference in ulcer recurrence between the anti-Helicobacter group and the control group was statistically significant (4.8% vs. 38.1%, P = .0001, intention-to-treat) with a relative risk of 0.18 (95% confidence interval 0.04–0.69). Fifteen of these 18 ulcer recurrences were associated with persistent H. pylori infection: 14 in the omeprazole group and 1 in the anti-Helicobacter group (see Fig. 1).
DISCUSSION
The optimal surgical treatment for perforated duodenal ulcer has been controversial. Simple repair has been the most commonly performed procedure since its popularization by Graham in 1937. 17 However, long-term follow-up of patients who underwent simple repair reveals a high incidence of ulcer relapse. 1–4 In a prospective series by Bornman et al, 18 48 of 131 patients (42.5%) had recurrent ulcer disease after simple closure of duodenal perforation over a median follow-up of 42 months; 30% of them required further surgery for intractable symptoms or recurrent ulcer complications. Because of the unsatisfactory result of simple repair, immediate acid-reduction procedures have been strongly advocated. In the 1980s, several prospective randomized studies reported significantly fewer ulcer recurrences by adding immediate proximal gastric vagotomy to patch repair of ulcer perforation. 7,19–21 Although the procedure has been shown to be safe, without increasing the rate of perioperative complications, it is technically demanding and requires prolonged operation time. With the recent rapid decline in the number of elective peptic ulcer operations, immediate proximal gastric vagotomy is unlikely to be a practical procedure for most surgical residents, the front-line personnel managing patients with duodenal ulcer perforation.
The recent rapid development in laparoscopic surgery has complicated the issue. Since the first successful laparoscopic repair performed by Mouret et al 22 in 1990, several minimal-access techniques have been described for repair of perforated peptic ulcers. 23–25 Nevertheless, reservations about the use of laparoscopic repair still exist. The inability to perform a concomitant acid-reduction procedure must be weighed against the analgesic and cosmetic advantages of laparoscopic repair. Although laparoscopic vagotomy has been reported as an elective procedure for chronic duodenal ulcer, 26 the procedure is likely to be time-consuming, and its use in patients with peritonitis from a perforated duodenal ulcer is probably limited.
Our study was designed to determine whether perforated duodenal ulcer is causally related to H. pylori infection. Anti-Helicobacter therapy would be a more desirable option than definitive surgery if eradication of the bacterium confers prolonged ulcer remission after simple closure of the perforation. In our early 27 and the present series of consecutive patients with perforated duodenal ulcers, H. pylori infection rates exceeded 80%. This figure is much higher than that reported by Reinbach et al 14 but is consistent with that of Sebastian et al 15 and Matsukura et al, 16 suggesting an association between H. pylori infection and duodenal ulcer perforation.
In contrast to the high consumption rate of NSAIDs in most Western series, 28,29 only 26 of 129 patients (20%) in the present series reported a history of use of these agents. This could partly be attributed to the younger age of the patients in our study. Although perforated peptic ulcers have been related to the use of NSAIDs, the association was shown mainly in the elderly patients who took these drugs on a long-term basis. 30H. pylori infection, as a risk factor, appears to be more relevant in younger patients, in whom acid-reduction surgery with its attendant complications is most undesirable.
To the best of our knowledge, this is the first randomized study examining the effect of H. pylori eradication in patients with perforated duodenal ulcers. After H. pylori eradication and without maintenance acid-suppression agents, 95% of patients remained ulcer-free at 1-year follow-up. The remission rate is similar to those previously reported in uncomplicated ulcers after H. pylori eradication 8,9 and is comparable to that achieved by immediate proximal gastric vagotomy during emergency laparotomy. 5–7 In light of the high prevalence of H. pylori infection and the few recurrences after eradication, the bacterium is likely to be causally related to the strong ulcer diathesis in patients with duodenal ulcer perforation. Simple repair, either conventional or laparoscopic, is the procedure of choice for duodenal ulcer perforation, especially in younger patients. H. pylori status should be determined when the patients recover from the acute episode, by either endoscopic biopsy or serology, and the bacterium should be eradicated in those who were infected. Immediate acid-reduction surgery is unnecessary unless there are other concurrent ulcer complications, such as hemorrhage or obstruction.
Footnotes
Correspondence: S.C. Sydney Chung, MD, Dept. of Surgery, Prince of Wales Hospital, Shatin, N.T., Hong Kong.
Part of the article was presented at the meeting of the American Gastroenterology Association, New Orleans, Louisiana, May 1998.
Accepted for publication January 22, 1999.
References
- 1.Boey J, Wong J. Perforated duodenal ulcers. World J Surg 1987; 11:319. [DOI] [PubMed] [Google Scholar]
- 2.Drury JK, McKay AJ, Hutchison JS, Joffe SN. Natural history of perforated duodenal ulcers treated by suture closure. Lancet 1978; 2 (8093):749–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin GE, Organ CH. The natural history of the perforated duodenal ulcer treated by suture plication. Ann Surg 1976; 183:382–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sawyers JL, Herrington JL, Mulherin JO, Whitehead WA, Moby B, Marsh J. Acute perforated ulcer. An evaluation of surgical management. Arch Surg 1975; 110:527–530. [DOI] [PubMed] [Google Scholar]
- 5.Jordan PH, Thornby J. Perforated pyloroduodenal ulcers: long-term results with omental patch closure and parietal cell vagotomy. Ann Surg 1995; 221:479–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sawyers JL, Herrington JL Jr. Perforated duodenal ulcer managed by proximal gastric vagotomy and suture plication. Ann Surg 1977; 185:656–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hay JM, Lacaine F, Kohlmann G, Fingerhut A. Immediate definitive surgery for perforated duodenal ulcer does not increase operative mortality: a prospective controlled trial. World J Surg 1988; 12:705–709. [DOI] [PubMed] [Google Scholar]
- 8.Graham DY, Lew GM, Klein PD, et al. Effect of treatment of Helicobacter pylori infection on the long-term recurrence of gastric or duodenal ulcer: a randomized, controlled study. Ann Intern Med 1992; 116:705–708. [DOI] [PubMed] [Google Scholar]
- 9.Van der Hulst RW, Rauws EA, Koycu B, et al. Prevention of ulcer recurrence after eradication of Helicobacter pylori : a prospective long-term follow-up study. Gastroenterol 1997; 113:1082–1086. [DOI] [PubMed] [Google Scholar]
- 10.Hosking SW, Ling TK, Chung SC, et al. Duodenal ulcer healing by eradication of Helicobacter pylori without anti-acid treatment: randomized controlled trial. Lancet 1994; 343:508–510. [DOI] [PubMed] [Google Scholar]
- 11.Sung JJ, Leung WK, Suen R, et al. One-week antibiotics versus maintenance acid suppression therapy for Helicobacter pylori-associated peptic ulcer bleeding. Dig Dis Sci 1997; 42:2524–2528. [DOI] [PubMed] [Google Scholar]
- 12.Helicobacter pylori in peptic ulcer disease. NIH Consensus Statement 1994; 12:1–23. [PubMed]
- 13.The European Helicobacter Pylori Study Group. Current European concepts in management of Helicobacter pylori infection. The Maastricht Consensus report. Gut 1997; 41:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reinbach DH, Cruickshank G, McColl KE. Acute perforated duodenal ulcer is not associated with Helicobacter pylori infection. Gut 1993; 34:1344–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sebastian M, Chandran VP, Elashaal YI, Sim AJ. Helicobacter pylori infection in perforated peptic ulcer disease. Br J Surg 1995; 82:360–362. [DOI] [PubMed] [Google Scholar]
- 16.Matsukura N, Onda M, Tokunaga A, et al. Role of Helicobacter pylori infection in perforation of peptic ulcer: an age- and gender-matched case-control study. J Clin Gastroenterol 1997; 25:S235–S239. [DOI] [PubMed] [Google Scholar]
- 17.Graham RR. The treatment of perforated duodenal ulcers. Surg Gynecol Obstet 1937; 64:235. [Google Scholar]
- 18.Bornman PC, Theodorou NA, Jeffery PC, et al. Simple closure of perforated duodenal ulcer: a prospective evaluation of a conservative management policy. Br J Surg 1990; 77:73–75. [DOI] [PubMed] [Google Scholar]
- 19.Boey J, Branicki FJ, Alagartnam TT, et al. Proximal gastric vago-tomy—the preferred operation for perforations in acute duodenal ulcer. Ann Surg 1988; 208:169–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Christiansen J, Andersen OB, Bonnesen T, Baekgaard N. Perforated duodenal ulcer managed by simple closure versus closure and proximal gastric vagotomy. Br J Surg 1987; 74:286–287. [DOI] [PubMed] [Google Scholar]
- 21.Ceneviva R, de Castro e Silva Jr O, Castelfranchi PL, Modnea JLP, Santos RF. Simple closure with or without proximal gastric vagotomy for perforated duodenal ulcer. Br J Surg 1986; 73:427–430. [DOI] [PubMed] [Google Scholar]
- 22.Mouret P, Francois Y, Vignal J, Barth X, Lombard-Platet R. Laparoscopic treatment of perforated peptic ulcer. Br J Surg 1990; 77:1006. [DOI] [PubMed] [Google Scholar]
- 23.Lau WY, Leung KL, Kwong KH, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg 1996; 224:131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Costalat G, Alquier Y. Combined laparoscopic and endoscopic treatment of perforated gastroduodenal ulcer using the ligamentum teres hepatis (LTH). Surg Endosc 1995; 9:677–679. [DOI] [PubMed] [Google Scholar]
- 25.Matsuda M, Nishiyama M, Hanai T, Saeki S, Watanabe T. Laparoscopic omental patch repair for perforated peptic ulcer. Ann Surg 1995; 221:236–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Awad W, Csendes A, Braghetto I, et al. Laparoscopic highly selective vagotomy: technical considerations and preliminary results in 119 patients with duodenal ulcer or gastroesophageal reflux disease. World J Surg 1997; 21:261–268. [DOI] [PubMed] [Google Scholar]
- 27.Ng EK, Chung SC, Sung JJ, et al. High prevalence of Helicobacter pylori infection in duodenal ulcer perforations not caused by non-steroidal anti-inflammatory drugs. Br J Surg 1996; 83:1779–1781. [DOI] [PubMed] [Google Scholar]
- 28.Thompson MR. Indomethacin and perforated duodenal ulcer. Br Med J 1980; 280:448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collier D St J, Pain JA. Non-steroidal anti-inflammatory drugs and peptic ulcer perforation. Gut 1985; 26:359–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walt R, Katchinski B, Logan R, Ashley J, Langman MJS. Rising frequency of peptic ulcer perforation in elderly people in the United Kingdom. Lancet 1986; 1:489–492. [DOI] [PubMed] [Google Scholar]