Abstract
Background and Objective
The ideal suture for abdominal fascial closure has yet to be determined. Surgical practice continues to rely largely on tradition rather than high-quality level I evidence. The authors conducted a systematic review and meta-analysis of randomized controlled trials to determine which suture material and technique reduces the odds of incisional hernia.
Methods
MEDLINE and Cochrane Library databases were searched for articles in English published from 1966 to 1998 using the keywords “suture,” “abdomen/surgery,” and “randomized controlled trials.” Randomized controlled trials, trials of adult patients, and trials with a Jadad Quality Score of more than 3, comparing suture materials, technique, or both, were included. Two independent reviewers critically appraised study quality and extracted data. The reviewers were masked to the study site, authors, journal, and date to minimize bias. The primary outcome was postoperative incisional hernia. Secondary outcomes included wound dehiscence, infection, wound pain, and suture sinus formation.
Results
The occurrence of incisional hernia was significantly lower when nonabsorbable sutures were used. Suture technique favored nonabsorbable continuous closure. Suture sinuses and wound pain were significantly lower when absorbable sutures were used. There were no differences in the incidence of wound dehiscence or wound infection with respect to suture material or method of closure. Subgroup analyses of individual sutures showed no significant difference in incisional hernia rates between polydioxanone and polypropylene. Polyglactin showed an increased wound failure rate.
Conclusions
Abdominal fascial closure with a continuous nonabsorbable suture had a significantly lower rate of incisional hernia. The ideal suture is nonabsorbable, and the ideal technique is continuous.
The ideal suture for closing abdominal fascia has yet to be determined. Surgical tradition, prejudice, familiarity, and personal conviction tend to dictate surgical procedures rather than evidence-based medicine. The reported cumulative incidence of incisional hernia varies from 9% to 19%. 1–3 Incisional hernias often require repair, with postoperative recurrence rates as high as 45%, 4 further contributing to complications.
Previous randomized controlled trials of abdominal fascial closure have failed to determine the best technique and the ideal suture. Many of these trials had small sample sizes and lacked sufficient power to show significant treatment differences. Results were often conflicting and have left many surgeons uncertain about the ideal suture and technique for abdominal fascial closure.
A meta-analysis is a statistical compilation of studies performed to address a treatment effect. 5 It attempts to summarize knowledge by rigorous and explicit methodology. 6 A recent meta-analysis by Weiland et al 7 attempted to address the question of fascial closure. Unfortunately, it contained numerous omissions and raised methodologic concerns; it should therefore be interpreted with caution. A more thorough and rigorous meta-analysis to determine the ideal suture is warranted.
METHODS
Literature Search
Computer searches of MEDLINE for the years 1966 to 1998 and the Cochrane Library (1998, vol. IV) database were performed using the keywords “abdominal surgery,” “sutures,” and “randomized clinical trials.” A manual search of the bibliographies of the identified papers was carried out to identify any additional trials. Finally, expert academic surgeons in Ontario, Canada, were asked whether they knew about any important unpublished data.
Inclusion and Exclusion Criteria
All randomized clinical trials comparing at least two different suture materials or techniques for abdominal fascial closure were included. Trials using vertical midline, paramedian, oblique, or transverse incisions were included. Other criteria included patients older than 15 years and a Jadad Quality Score of more than 3. 8 Gynecologic surgery trials and trials of children younger than 15 years were excluded. Trials comparing two sutures of the same category (i.e., absorbable vs. absorbable) and with the same technique were excluded because relevant comparisons could not be applied to our clinical question.
Data Extraction
Two reviewers masked to journal, authors, and publication dates performed independent data extraction. Study quality was assessed using the Jadad Quality Scale. 8 Discrepancies were resolved by discussion and consensus.
Analyses
The primary outcome was postoperative incisional hernia. Definitions of incisional hernia, wound dehiscence, wound infection, wound pain, and suture sinus were accepted as reported. Based on a priori criteria, the primary comparison was nonabsorbable versus absorbable sutures and continuous versus interrupted techniques. Further comparisons included continuous nonabsorbable versus continuous absorbable and interrupted nonabsorbable versus interrupted absorbable. Studies were assessed for homogeneity both qualitatively and quantitatively. Statistical homogeneity of the study data was confirmed using the chi-square test of heterogeneity. 9 All analyses were conducted using Review Manager 3.1 (Software Update, the Cochrane Collaboration, Oxford, UK).
The Mantel-Haenszel 9 fixed-effects method was used to summarize dichotomous outcomes of pooled studies. The odds ratio (OR) was used as the summary statistic, with 95% confidence intervals (CI). Absolute risk reduction (ARR), relative risk reduction (RRR), and number needed to treat (NNT) were also calculated. Sensitivity analyses were performed by serially omitting each trial and omitting trials with follow-up periods of less than 1 year. Comparisons of trials using only midline incisions were also carried out. A reanalysis using the random-effects model was also performed to assess the robustness of the results.
Subgroup analyses of individual suture types (i.e., polydioxanone [PDS] vs. polypropylene [Prolene]) were also conducted.
RESULTS
Thirty-two studies that evaluated suture material or technique for abdominal fascial closure were identified. Nineteen trials were excluded for the following reasons: poor quality, 10–19 gynecologic surgery only, 20,21 pediatric trial, 22 nonrandomized trials, 23–26 and comparison exclusions (i.e., studies assessing absorbable vs. absorbable sutures). 2,27,28 Study characteristics are displayed in Table 1. No unpublished data were identified. Data extraction revealed no interobserver variation, with 100% agreement between the two reviewers for all outcomes.
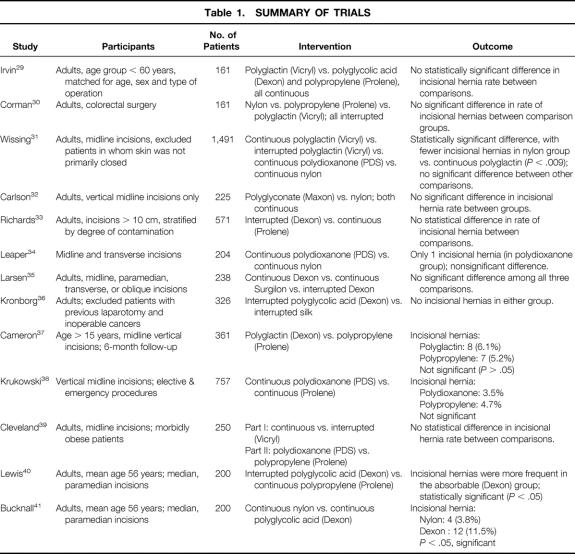
Table 1. SUMMARY OF TRIALS
Nonabsorbable Versus Absorbable
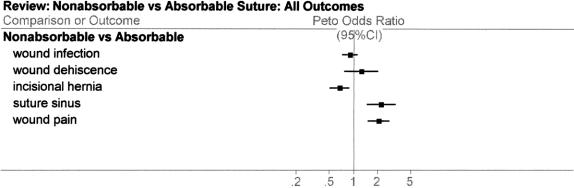
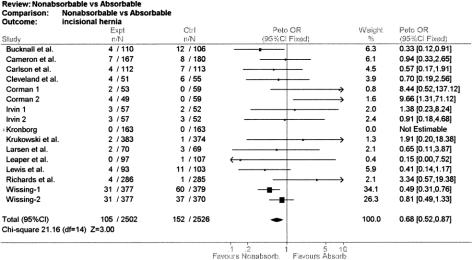
The clinical homogeneity of included trials was confirmed, with the possible exception of one trial that compared polydioxanone and polypropylene in morbidly obese patients. 29 The test for heterogeneity was not significant (chi-square = 21.16, P > .05), indicating that the studies were homogenous and statistical combination was appropriate. The pooled OR for all outcomes comparing nonabsorbable versus absorbable sutures (13 studies) 28–41 are summarized in Figure 1. An OR less than 1 favors nonabsorbable and an OR more than 1 favors absorbable. For the primary outcome, incisional hernia, the OR was 0.68 (95% CI 0.52–0.87;Fig. 2). This means that the odds of incisional hernia were significantly lower in the nonabsorbable group, by 32%. The calculated cumulative incidence of incisional hernias across all studies was 5%.
Figure 1. Meta-analysis of all outcomes comparing absorbable versus nonabsorbable sutures. Squares indicate point estimates of odds ratio, and horizontal bars signify 95% confidence intervals. Values less than 1 favor the nonabsorbable group and values more than 1 favor the absorbable group. Point estimates are significant at the P < .05 level if their confidence intervals exclude the vertical line at 1 (“no effect”).
Figure 2. Pooled estimates of risk of incisional hernia comparing absorbable versus nonabsorbable. The weight attributed to a particular study is represented by the size of the square on the point estimate of each odds ratio; the width of the horizontal bars reflects the 95% confidence interval. Point estimates crossing the vertical bar represent statistically nonsignificant results, with 95% confidence intervals that include 1. An odds ratio of less than 1 favors nonabsorbable suture; an odds ratio of more than 1 favors absorbable suture.
The OR of wound infection in the nonabsorbable group versus the absorbable group was 0.90 (95% CI 0.73–1.12) and the OR of wound dehiscence was 1.25 (95% CI 0.78–2.01). Neither was statistically significant. Suture sinuses and wound pain were significantly more frequent in the nonabsorbable group (OR 2.18, 95% CI 1.48–3.22, and OR 2.05, 95% CI 1.52–2.77, respectively).
Continuous Versus Interrupted
In the six trials comparing continuous versus interrupted technique (irrespective of suture type), the OR for incisional hernia was significant, favoring continuous closure (OR 0.73, 95% CI 0.55–0.99;Fig. 3). There was no statistical difference in the rate of wound infection or wound dehiscence.
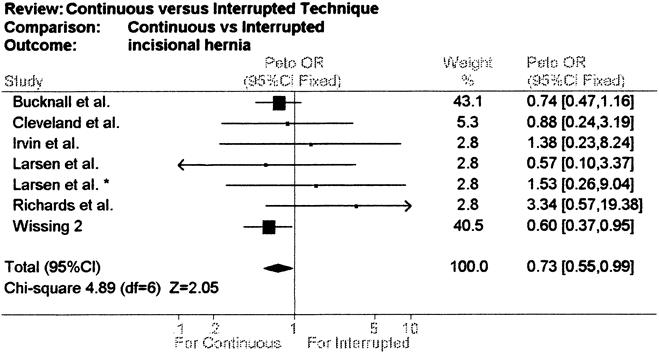
Figure 3. Pooled estimates of continuous versus interrupted suture technique. Squares indicate point estimates of odds ratios, and horizontal bars represent 95% confidence intervals. Values less than 1 favor the continuous group and values more than 1 favor the interrupted group.
Continuous Nonabsorbable Versus Continuous Absorbable
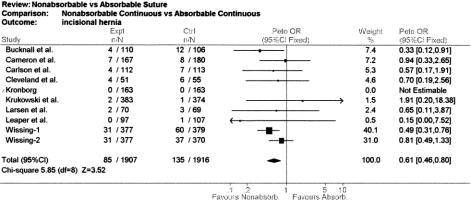
In the nine trials comparing continuous nonabsorbable versus continuous absorbable suture technique (Fig. 4), incisional hernias were significantly less common in the continuous nonabsorbable group (OR 0.61, 95% CI 0.46–0.80;Table 2).
Figure 4. Pooled estimates of incisional hernia comparing continuous nonabsorbable versus continuous absorbable closure. Squares indicate point estimates of odds ratios, with the size of the square representing the weight of each study. Horizontal bars signify 95% confidence intervals. The summary odds ratio is represented by the diamond; values to the left of the vertical bar favor the continuous nonabsorbable group and values to the right favor continuous absorbable.
Table 2. CLINICAL OUTCOME MEASURES OF INCISIONAL HERNIA ACROSS COMPARISON GROUPS
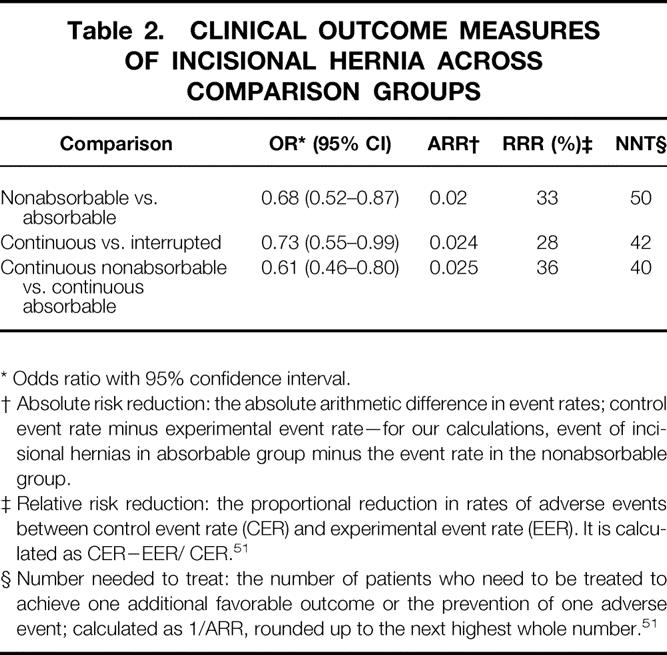
* Odds ratio with 95% confidence interval.
† Absolute risk reduction: the absolute arithmetic difference in event rates; control event rate minus experimental event rate—for our calculations, event of incisional hernias in absorbable group minus the event rate in the nonabsorbable group.
‡ Relative risk reduction: the proportional reduction in rates of adverse events between control event rate (CER) and experimental event rate (EER). It is calculated as CER−EER/ CER. 51
§ Number needed to treat: the number of patients who need to be treated to achieve one additional favorable outcome or the prevention of one adverse event; calculated as 1/ARR, rounded up to the next highest whole number. 51
Interrupted Nonabsorbable Versus Interrupted Absorbable
There was no significant difference in incisional hernia rates between these two trials.
Sensitivity Analyses
A reanalysis of only the trials using vertical midline incisions (omitting trials using paramedian, transverse incisions) found that the rate of incisional hernia was still significantly lower in the nonabsorbable group (OR 0.64, 95% CI 0.48–0.86). Further sensitivity analyses included reanalyzing the data using the random-effects model, including poor-quality trials, including gynecologic trials, excluding small trials, excluding the obesity trial, and omitting all trials with less than 1 year of follow-up. These analyses did not substantially change the summary statistic.
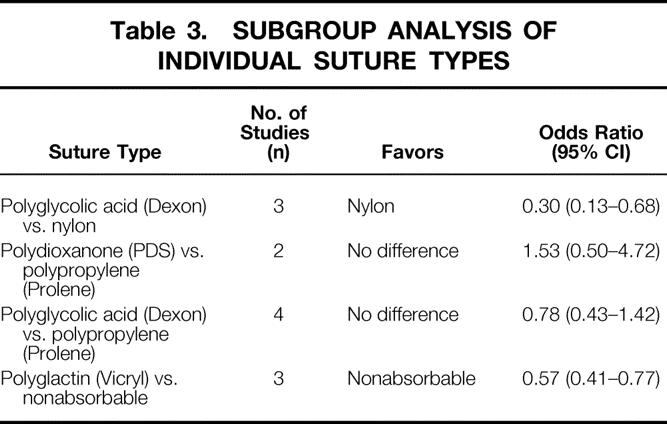
Subgroup Analyses
The subgroup analyses are summarized in Table 3. Polydioxanone (PDS) compared with polypropylene (Prolene) did not have an increased risk of incisional hernia (OR 1.53, CI 0.50–4.72). In contrast, use of polyglactin (Vicryl) compared with nonabsorbable sutures resulted in an increased rate of wound failure. Nylon compared with polyglycolic acid (Dexon) demonstrated a lower rate of incisional hernia (OR 0.30, 95% CI 0.13–0.68). There was no statistical difference between polyglycolic acid (Dexon) and polypropylene (Prolene).
Table 3. SUBGROUP ANALYSIS OF INDIVIDUAL SUTURE TYPES
DISCUSSION
Incisional hernias contribute significantly to the complication rate and once repaired have a high recurrence rate. 4 Wound dehiscence, infection, pain, and suture sinus formation are also important contributors to postoperative complications.
A meta-analysis, when it includes a series of satisfactory trials and when it is rigorously performed, provides high-quality level I evidence. The recent meta-analysis by Weiland et al 7 failed to meet most of the methodologic requirements supported by a recent consensus. 6 The search strategy was less than explicit, nonrandomized trials, and poor-quality studies were included in their analyses, decreasing the validity of their results. The quality of the randomized controlled trials included in their analysis was not assessed. Interpretation of their results was difficult because individual study characteristics were not described. There was an absence of clinically useful outcome measures: OR, NNT, and RRR figures were not reported. The method of combining probability values used in their report has two important drawbacks: it does not weigh the studies according to their uncertainties or sample sizes, and it does not give estimates of the magnitude of the effects. For these reasons, combining probability values is seldom used as a metanalytic tool. 42
Poor-quality surgical trials appear to be common. 43 A recent meta-analysis of drainage of colorectal anastomoses also reported overall poor quality of the surgical trials included in their analyses. 44 The Jadad Quality Scale 8 is the only validated instrument available to assess the quality of randomized controlled trials. Incorporation of poor-quality trials into a meta-analysis has been shown to increase the estimate of benefit by 34% and may produce discordant results. 45 In our review, 10 trials (31%) were excluded for poor quality (Jadad score <3) to assess adequately any benefit of intervention.
In our review, qualitative and quantitative homogeneity was confirmed and statistical combination was appropriate. Multiple sensitivity analyses confirmed the robustness of our summary statistic. Inclusion or exclusion of the morbidly obese trial 39 did not alter the results. Gynecologic trials 20,21 were omitted to focus results to a general surgical practice, and inclusion of these trials did not appreciably change the summary statistic.
The pooled OR for incisional hernia in the nonabsorbable versus absorbable suture groups, the primary outcome for this study, was 0.68 (95% CI 0.52–0.87). The fact that the point estimate was less than 1 favored the nonabsorbable group (Fig. 2), a statistically significant result. Clearly, the evidence supports a significant benefit in using nonabsorbable suture. With an RRR of 32%, using a nonabsorbable suture lowers the risk of incisional hernia formation by 32%. A more clinically useful measure is NNT: the NNT was 50, which means only 50 patients need to undergo nonabsorbable fascial closure to prevent one incisional hernia.
For continuous nonabsorbable versus continuous absorbable, the RRR was even greater (36%), and the NNT was 40 patients. These results are also biologically plausible: nonabsorbable sutures retain tensile strength for the duration of fascial healing. 4 Continuous suture technique also has the added benefit of being easier and less time-consuming. 33
A potential benefit of meta-analysis is the ability to perform subgroup analyses. 46,47 Our subgroup analyses demonstrated that polydioxanone (PDS), unlike all other absorbable sutures, did not have an increased risk of incisional hernia. Polyglactin (Vicryl) appeared to have a significant risk of incisional hernia when compared with nonabsorbable sutures.
Our meta-analysis is limited by the absence of unpublished literature and possibly other sources of heterogeneity. Unpublished studies are more likely to have “negative results”; therefore, a meta-analysis of only published studies may have some publication bias. A survey of experts in Ontario yielded no unpublished data. Extraction bias was minimized by masking reviewers to publication date, authors, and journal. Other sources of heterogeneity include patient factors (malignancy, steroid use, pulmonary disease, obesity, age), local factors (emergency surgery, degree of contamination, antibiotic prophylaxis), and technical factors (surgical experience, type of incision). These factors may theoretically have been unequally distributed between treatment groups or between studies. Type of incision may be instrumental in incisional hernia formation. A prospective study described lower incisional hernia rates in paramedian incisions versus midline incisions. 28 Studies of transverse incisions have been inconclusive. 47–50 The randomized trials included in this study did not stratify based on type of incision. For example, no direct comparisons of midline versus transverse incisions were done. The question of the role of incision type in the development of incisional hernias is therefore impossible to answer by this meta-analysis.
The follow-up of patients for individual studies was highly variable: only seven (54%) studies followed patients for 1 year or more. This may explain why our cumulative incidence of incisional hernia across studies was only 5%. This incisional hernia rate at 1 year does not reflect the true incidence of this outcome. Mudge and Hughes 1 followed up a cohort of patients prospectively for 10 years and noted that 35% of all incisional hernias occurred after 3 years.
This meta-analysis serves to synthesize some of the information on the effect of suture choice on wound failure. It is hypothesis-generating in that, given the high number of poor-quality trials, short follow-up, and variable patient factors, a large definitive trial of nonabsorbable continuous closure versus the current surgical practice with a longer follow-up period is warranted. Because incisional hernia is an infrequent outcome, very large sample sizes are required to determine a difference between suture materials (nonabsorbable vs. absorbable) or technique (continuous vs. interrupted). If we assume an incisional hernia rate of 10% in a control group and we would like to reduce this rate to 8% (20% RRR) in the intervention group with 80% power and a significance level of 5%, we would require 3,206 patients in each treatment arm in a traditional randomized controlled trial. Such a trial seems improbable and supports doing this meta-analysis of current trials.
In conclusion, we report high-quality level I evidence that the ideal suture in reducing incisional hernia rates is a nonabsorbable suture material and a continuous technique.
Footnotes
Correspondence: R.A. Malthaner, MSc, MD, FACS, Department of Thoracic Surgery, London Health Sciences Centre, 375 South St. Suite 3N345, Victoria Campus, London, Ontario N6A 4G5, Canada.
Accepted for publication June 25, 1999.
References
- 1.Mudge M, Hughes LE. Incisional hernia; a 10-year prospective study of incidence and attitudes. Br J Surg 1985; 72:70–71. [DOI] [PubMed] [Google Scholar]
- 2.Israelsson LA, Jonsson T. Incisional hernia after midline laparotomy: a prospective study. Eur J Surg 1996; 162:125–129. [PubMed] [Google Scholar]
- 3.Osther PJ, Gjode P, Mortensen BB, et al. Randomized comparison of polyglycolic acid and polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. Br J Surg 1995; 82:1080–1082. [DOI] [PubMed] [Google Scholar]
- 4.Gecin E, Kocak S, Erscz S. Recurrence after incisional hernia repair: results and risk factors. Surg Today 1996; 26:607–609. [DOI] [PubMed] [Google Scholar]
- 5.Petitti DB, Kelsey J, Marmot MG, Stolley PD, Vessey MP, eds. Meta-Analysis, Decision Analysis, and Cost-Effectiveness Analysis. 1st ed. New York: Oxford University Press; 1994.
- 6.Cook DJ, Sackett DL, Spitzer WO. Methodological guidelines for systematic reviews of randomized control trials in healthcare from the Potsdam consultation on meta-analysis. J Clin Epidemiol 1995; 48:167–171. [DOI] [PubMed] [Google Scholar]
- 7.Weiland DE, Bay C, Del Sordi S. Choosing the best abdominal closure by meta-analysis. Am J Surg 1998; 176:666–670. [DOI] [PubMed] [Google Scholar]
- 8.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clin Trials 1996; 17:1–12. [DOI] [PubMed] [Google Scholar]
- 9.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959; 22:719–748. [PubMed] [Google Scholar]
- 10.Tiwari VS, Agarwal A. Evaluation of synthetic absorbable sutures in abdominal closure. J Indian Med Assoc 1982; 78:37–39. [PubMed] [Google Scholar]
- 11.McNeill PM, Sugarman HJ. Continuous absorbable vs interrupted nonabsorbable fascial closure. Arch Surg 1986; 121:238–243. [DOI] [PubMed] [Google Scholar]
- 12.Savolainen H, Ristkari S, Mokka R. Early laparotomy wound dehiscence: a randomized comparison of three suture materials and two methods of fascial closure. Ann Chir Gynaecol 1988; 77:111–113. [PubMed] [Google Scholar]
- 13.Deitel M, Alhindawi R, Yamen M, et al. Dexon plus Maxon fascial closure in morbid obesity: a prospective randomized comparison. Can J Surg 1990; 33:302–304. [PubMed] [Google Scholar]
- 14.Askew AR. A comparison of upper abdominal wound closure with monofilament and polyglycolic acid. Aust NZ J Surg 1983; 53:353–356. [DOI] [PubMed] [Google Scholar]
- 15.Cameron AEP, Parker CJ, Field ES, et al. A randomized comparison of polydioxanone and polypropylene for abdominal wound closure. Ann Roy Coll Surg Eng 1985; 67:273–275. [Google Scholar]
- 16.Taylor TV. The use of polydioxanone suture in midline incisions. J Roy Coll Surg Ed 1985; 30:191–192. [PubMed] [Google Scholar]
- 17.Brolin RE. Prospective, randomized evaluation of midline fascial closure in gastric bariatric operations. Am J Surg 1996; 172:328–331. [DOI] [PubMed] [Google Scholar]
- 18.Fagniez PL, Hay JM, Lacaine F et al. Abdominal midline incision closure. Arch Surg 1985; 120:1351–1353. [DOI] [PubMed] [Google Scholar]
- 19.Gys T, Hubens A. A prospective comparative clinical study between monofilament absorbable and non-absorbable sutures for abdominal wall closure. Acta Chir Belg 1989; 89:265–270. [PubMed] [Google Scholar]
- 20.Orr JW, Orr PF, Barret JM, et al. Continuous or interrupted fascial closure: a prospective evaluation of no. 1 Maxon suture in 402 gynecologic procedures. Am J Obstet Gynecol 1990; 163:1485–1489. [DOI] [PubMed] [Google Scholar]
- 21.Trimbos JB, Smit IB, Holm JP, et al. A randomized clinical trial comparing two methods of fascia closure following midline laparotomy. Arch Surg 1992; 127:1232–1353. [DOI] [PubMed] [Google Scholar]
- 22.Chana RS, Sexena VC, Agarwal A. A prospective study of closure technique of abdominal incisions in infants and children. J Indian Med Assoc 1980; 88:359–369. [PubMed] [Google Scholar]
- 23.Kiely EM, Spitz I. Layered vs mass closure of abdominal wounds infants and children. Br J Surg 1985; 72:739–740. [DOI] [PubMed] [Google Scholar]
- 24.Israelsson LA, Jonsson T. Closure of midline laparotomy incisions with polydioxanone and nylon: the importance of suture technique. Br J Surg 1994; 81:1606–1608. [DOI] [PubMed] [Google Scholar]
- 25.Leese T, Ellis H. Abdominal wound closure—a comparison of monofilament nylon and polydioxanone. Surgery 1984; 95:125–126. [PubMed] [Google Scholar]
- 26.Gallitano AL, Kondi ES. The superiority of polyglycolic acid suture for closure of abdominal incisions. Surg Gynecol Obstet 1973; 137:794–796. [PubMed] [Google Scholar]
- 27.Gammelgaard N, Jensen J. Wound complications after closure of abdominal incisions with Dexon or Vicryl. Acta Chir Scan 1983; 149:505–508. [PubMed] [Google Scholar]
- 28.Kendall SWH, Brennan TG, Gillou PJ. Suture length to wound length ratio and integrity of midline and paramedian incisions. Br J Surg 1991; 78:705–707. [DOI] [PubMed] [Google Scholar]
- 29.Irvin TT, Koffman CG, Duthie HL. Layer closure of laparotomy wounds with absorbable and non-absorbable suture materials. Br J Surg 1976; 63:793–796. [DOI] [PubMed] [Google Scholar]
- 30.Corman ML, Veidenheimer MC, Coller JA. Controlled clinical trial of three suture materials for abdominal wall closure after bowel operations. Am J Surg 1981; 141:510–513. [DOI] [PubMed] [Google Scholar]
- 31.Wissing J, van Vroohoven JMV, Efteneck M, et al. Fascia closure after midline laparotomy: results of a randomized trial. Br J Surg 1987; 74:738–741. [DOI] [PubMed] [Google Scholar]
- 32.Carlson MA, Condon RE. Polyglyconate (Maxon) versus nylon suture in midline abdominal incision closure: a prospective randomized trial. Ann Surg 1995; 61:980–983 [PubMed] [Google Scholar]
- 33.Richards PC, Balcj CM, Aldrette JA. A randomized prospective study of 571 patients comparing continuous vs. interrupted suture techniques. Ann Surg 1983; 197:238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leaper DJ, Arthur A, Roy EM, et al. Abdominal wound closure: a controlled trial of polyamide (nylon) and polydioxanone suture (PDS). Ann Roy Coll Surg Eng 1985; 67:273–275. [PMC free article] [PubMed] [Google Scholar]
- 35.Larsen PN, Nielsen K, Schultz A, et al. Closure of the abdominal fascia after clean and clean-contaminated laparotomy. Acta Chir Scand 1989; 155:461–464. [PubMed] [Google Scholar]
- 36.Kronborg O. Polyglycolic acid (Dexon) vs silk for fascial closure of abdominal incisions. Acta Chir Scand 1976; 142:9–12. [PubMed] [Google Scholar]
- 37.Cameron AEP, Gray RCF, Talbot RW, Wyatt AP. Abdominal wound closure: a trial of Prolene and Dexon. Br J Surg 1980; 67:487–488. [DOI] [PubMed] [Google Scholar]
- 38.Krukowski ZH, Cusick EL, Engeset J. Polydioxanone or polypropylene for closure of midline abdominal incisions: a prospective comparative clinical trial. Br J Surg 1980; 67:487–488. [DOI] [PubMed] [Google Scholar]
- 39.Cleveland RD, Zitsch RP, Laws HL. Incisional closure in morbidly obese patients. Am Surg 1989; 55:61–64. [PubMed] [Google Scholar]
- 40.Lewis RT, Wiegand FM. Natural history of vertical abdominal parietal closure: Prolene versus Dexon. Can J Surg 1989; 32:196–199. [PubMed] [Google Scholar]
- 41.Bucknall TE, Ellis H. Abdominal wound closure—a comparison of monofilament nylon and polyglycolic acid. Surgery 1981;672–677. [PubMed] [Google Scholar]
- 42.Hasselblad V, McCrory DC. Meta-analytic tools for medical decision making: a practical guide. Med Decis Making 1995; 15:81–96. [DOI] [PubMed] [Google Scholar]
- 43.Solomon MJ, McLeod RS. Clinical studies in surgical journals; have we improved? Dis Colon Rectum 1993; 36:43–44. [DOI] [PubMed] [Google Scholar]
- 44.Urbach DR, Kennedy ED, Cohen MM. Colon and rectal anastomoses do not require routine drainage. Ann Surg 1999; 229:174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moher D, Pham B, Jones A, et al. Does the quality of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998; 352:609–613. [DOI] [PubMed] [Google Scholar]
- 46.Oxman AD, Guyatt GH. A consumer’s guide to subgroup analyses. Ann Intern Med 1992; 116:78–84. [DOI] [PubMed] [Google Scholar]
- 47.Berlin JA, Antman EM. Advantages and limitations of meta-analytic regressions of clinical trials data. Online J Curr Clin Trials 1994; doc#134. [DOI] [PubMed]
- 48.Lord RS, Crozier JA, Snell JI, Meek AC. Transverse abdominal incisions compared with midline incisions for elective infrarenal aortic reconstruction: predisposition to incisional hernia in patients with increased intraoperative blood loss. J Vasc Surg 1994; 20:27–33. [DOI] [PubMed] [Google Scholar]
- 49.Ellis H, Coleridge-Smith PD, Joyce AD. Abdominal incisions—vertical or transverse? Postgrad Med J 1984; 60:407–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stone HH, Hoefling SJ, Strom PR, et al. Abdominal incisions: transverse vs vertical placement and continuous and interrupted closure. South Med J 1983; 76:1106–1108. [PubMed] [Google Scholar]
- 51.Sackett DL, Haynes RB, Guyatt GH, et al. Clinical Epidemiology: A Basic Science for Clinical Medicine. Boston: Little, Brown and Company; 1991.