Abstract
Objective
To compare the first 20 patients who underwent minimally invasive radioguided parathyroidectomies (MIRPs) performed at the authors’ institution with 20 similar patients who underwent a more conventional surgical approach for primary hyperparathyroidism.
Summary Background Data
The technique of parathyroidectomy has traditionally involved a bilateral exploration of the neck with the intent of visualizing four parathyroid glands and resecting enlarged parathyroid glands. Parathyroid scanning using radioisotopes has evolved and now can localize adenomas in 80% to 90% of patients. MIRP combines parathyroid scanning with a hand-held intraoperative detector that guides the surgeon to the adenoma.
Methods
Forty patients with documented primary hyperparathyroidism who underwent surgery by a single surgeon between January 1998 and May 1999 were included in this study. Twenty of these patients underwent MIRP. The technique involved injecting 20 mCi technetium-99m sestamibi 2 hours before surgery and performing a parathyroid scan. If the scan was considered positive for a single adenoma, patients were taken to the operating room and given the choice of either general anesthesia or intravenous sedation with local anesthesia. Using an incision of 4 cm or less, the dissection down to the adenoma was guided by the Navigator miniature hand-held probe. An additional 20 patients who underwent more conventional bilateral or unilateral neck exploration were chosen to match the MIRP patient population. Both groups included four patients undergoing repeat surgery for persistent or recurrent primary hyperparathyroidism and one patient with multiple endocrine neoplasia type 1 syndrome. Patient demographics, preoperative calcium and parathyroid hormone levels, operative time, total time in the operating room, time in the recovery room, complications, hospital charges for the operating room, and total hospital charges were analyzed.
Results
There were no differences in patient demographics, presenting symptoms, or preoperative calcium level between patients undergoing the standard procedure versus MIRP. Operative time, total time in the operating room, operative charges, and total hospital charges were significantly reduced in the MIRP group. All 40 patients were cured of primary hyperparathyroidism. There were no recurrent laryngeal nerve injures in either group. The mean length of stay in the standard group was 1.35 days; in the MIRP group, 65% of patients were discharged within 5 hours after surgery.
Conclusions
The MIRP technique resulted in excellent cure rates for primary hyperparathyroidism while simultaneously decreasing operative time and hospital stays. These resulted in significant cost reductions without compromising patient safety. The technique may significantly change the management of primary hyperparathyroidism.
Primary hyperparathyroidism can be a subtle yet devastating disease process. The prevalence may be as high as 4 per 1,000. 1 Its incidence is greater in women, and it increases with age; the estimated incidence in persons aged 60 and older is 154/100,000. 2,3 Causes include parathyroid adenoma, multiglandular hyperplasia of a primary or secondary nature, and rarely parathyroid cancer. \. The traditional surgical approach, honed during the past 70 years, has involved carefully exploring both sides of the central neck with the intent of identifying all four parathyroid glands. General endotracheal anesthesia has been the preferred and usually necessary modality. Enlarged parathyroid glands that were identified were considered pathologic and were then removed; however, surgical judgment and experience played a major role in the assessment and management of these presumably abnormal glands. Experienced surgeons have reported 97% to 99% cure rates using this standard approach. 4,5
Before 1992, preoperative parathyroid localization using noninvasive imaging techniques had poor sensitivity rates and significant false-positive rates. 6 However, the technetium-99m sestamibi parathyroid scan, developed in 1992, has increased the sensitivity of detecting parathyroid adenomas to 91%, with a specificity of 98.8%. 7 In 1997, Norman and Chheda 8 reported their results using minimally invasive radioguided parathyroidectomy (MIRP). This procedure, predicated on a positive sestamibi scan, makes use of a hand-held gamma probe to guide the surgeon to the parathyroid adenoma.
The purpose of this study was to compare the first 20 patients who underwent MIRPs at our institution with 20 similar patients who underwent a more conventional surgical approach for primary hyperparathyroidism.
METHODS
Twenty patients with primary hyperparathyroidism underwent MIRP between July 1998 and May 1999. These 20 patients were the first patients to undergo this procedure at our institution. For the purposes of this study, these patients were compared with 20 additional patients with primary hyperparathyroidism who underwent more conventional bilateral or unilateral neck exploration between January 1998 and May 1999. The 20 patients in the standard group were selected to match the MIRP patients closely. As such, both groups included four patients undergoing repeat surgery for persistent or recurrent primary hyperparathyroidism and one patient with multiple endocrine neoplasia type 1 (MEN1) syndrome. All procedures were performed by the same surgeon.
The diagnosis of primary hyperparathyroidism was based on hypercalcemia documented on at least two occasions and an elevated intact parathyroid hormone level (iPTH). A confirmatory 24-hour urinary calcium excretion was also obtained in more than 50% of the patients.
The MIRP technique was developed by Norman et al 8,9 in 1997. Patients underwent sestamibi parathyroid scanning on the morning of surgery. Two hours before the operation was scheduled to start, patients received an intravenous injection of 20 mCi sestamibi. Planar images were acquired using a low-energy high-resolution collimator positioned 8 cm from the neck in a 128 × 128 matrix with a 1.6 zoom and an energy window of 140 keV ± 10%. The initial image was acquired for a minimum of 5 minutes and at least 500,000 counts; subsequent images was acquired for identical times. Four early images were obtained beginning 15 minutes after injection, including anterior views with and without markers and right and left anterior oblique views. All views included the thorax down to the inferior aspect of the heart. Similar views were obtained starting 60 minutes after injection (delayed images). If the initial images were thought to be unequivocally positive for a parathyroid adenoma, the delayed images were not obtained (Figs. 1 and 2).
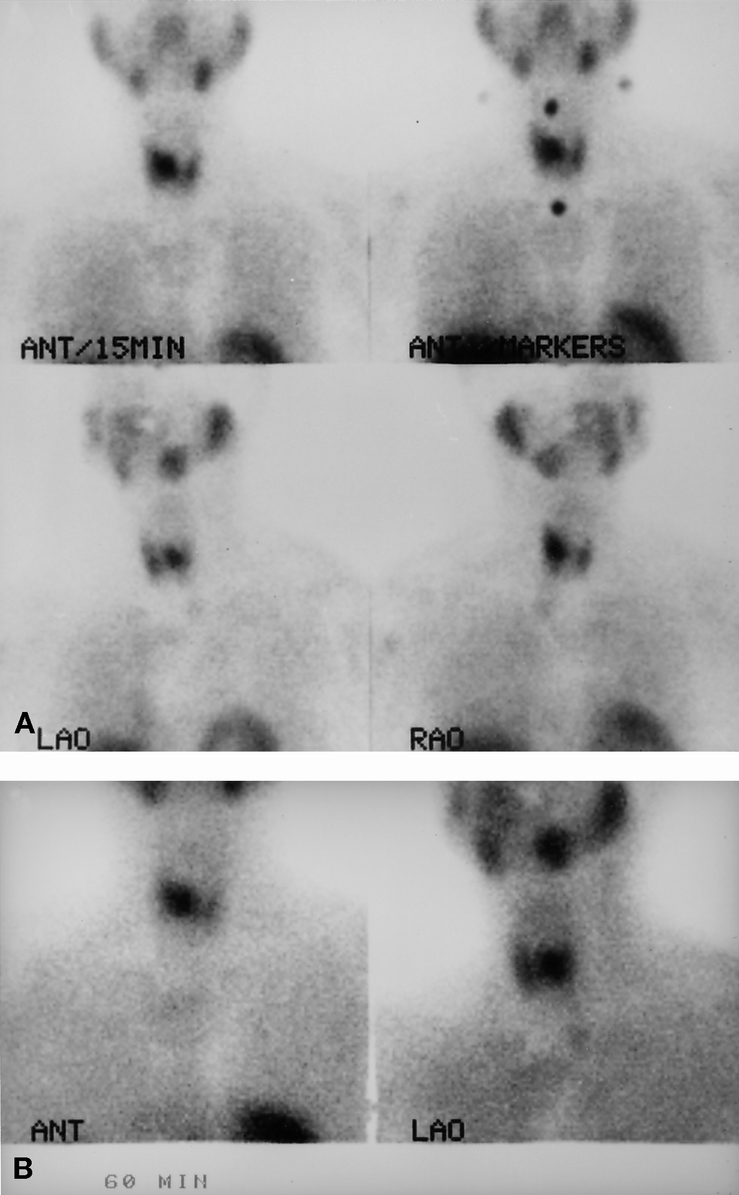
Figure 1. Initial (A) and delayed (B) parathyroid scans demonstrating a large right parathyroid adenoma. The use of anterior, left anterior oblique, and right anterior oblique views helped to demonstrate that the adenoma lay quite posterior and medial relative to the right thyroid lobe.
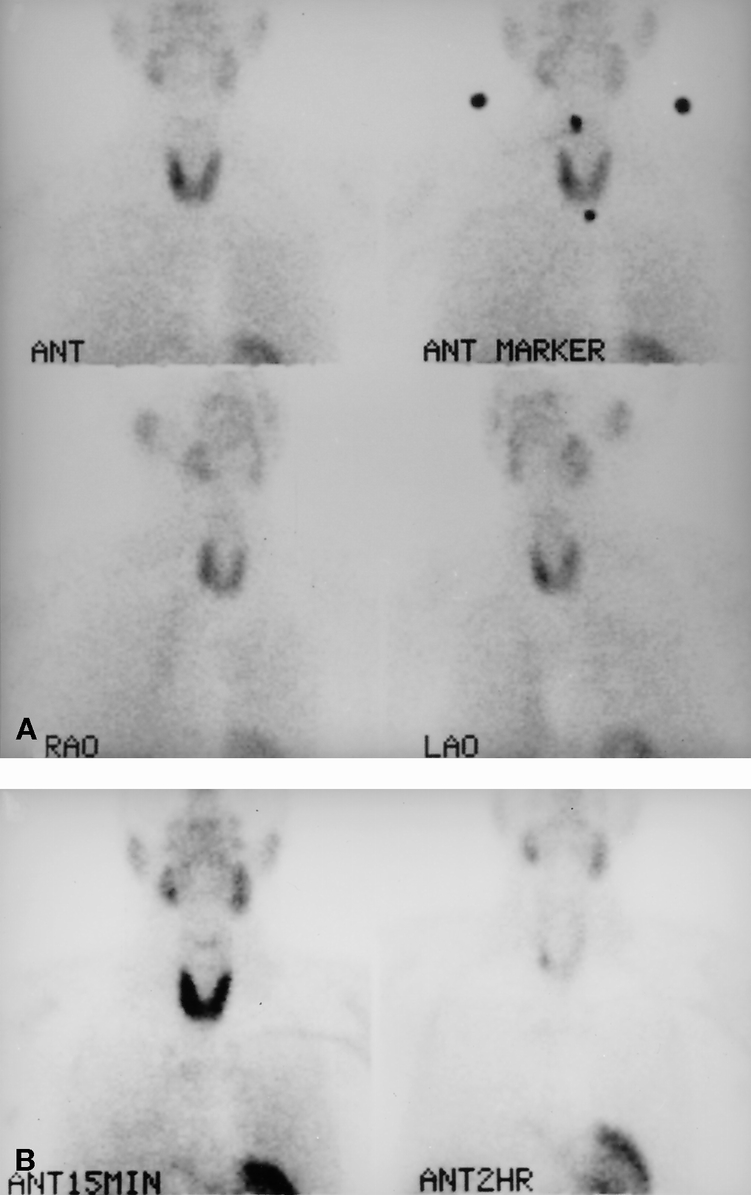
Figure 2. Initial (A) and delayed (B) parathyroid scans demonstrating a small right-sided parathyroid adenoma. This patient was referred after having undergone two previous unsuccessful neck explorations. The use of anterior, left anterior oblique, and right anterior oblique views helped to demonstrate that the adenoma was either close to the right thyroid lobe or was an intrathyroidal adenoma. The adenoma was, in fact, completely intrathyroidal.
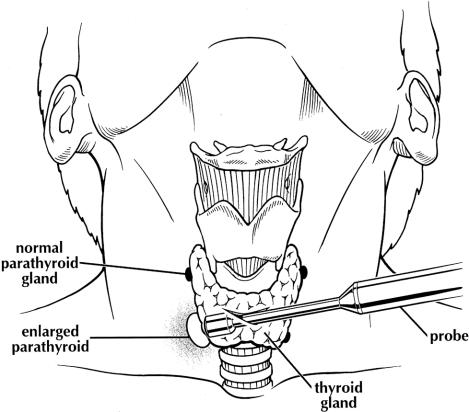
The MIRP technique is predicated on a positive parathyroid scan. If the preoperative scan localizes a solitary parathyroid adenoma, the incision should be made no later than 2.5 hours after injection. 8 Patients were given the choice of intravenous sedation (monitored anesthesia care [MAC]) or general endotracheal anesthesia. Intravenous sedation consisted of midazolam and propofol plus a local application of lidocaine with 10% sodium bicarbonate into the subcutaneous tissues of the anterior lower neck. A 2.5- to 4.0-cm incision was made in a transverse direction two fingerbreadths above the sternal notch. Minimal subplatysmal planes were created, and the strap muscles were divided in the midline and then dissected off the inferior aspect of the thyroid lobe on the side of the parathyroid adenoma. The dissection down to the adenoma was guided from this point by the use of a hand-held gamma probe (Navigator; U.S. Surgical, Inc., Norwalk, CT) (Fig. 3). Recently, U.S. Surgical released a probe designed for parathyroid surgery. Once the adenoma was identified, it was dissected using bipolar scissors. Care was taken to look for the recurrent laryngeal nerve; however, given the very directed dissection, the nerve was identified less than half the time.
Figure 3. A minimally invasive radioguided parathyroidectomy (MIRP). Through a small incision, the hand-held gamma probe helps to determine the line of dissection down to the right inferior parathyroid adenoma.
Once the targeted gland was removed, the radioactivity of the adenoma was measured ex vivo (with the probe directed away from the patient) and compared with the radioactivity obtained by slowly tracking the probe over the thyroid gland. If the ex vivo radioactivity totaled at least 20% of the remaining background counts, 10 the procedure was deemed successful and the incision site was closed without a drain. Frozen sections were generally unnecessary. 8 Norman and Chheda 8 reported that the radioactivity in the adenoma was low enough to allow the cryostat to be used without contamination if frozen-section analysis was requested.
The patient can be discharged once sufficient recovery has occurred. Patients were discharged with one bottle of calcium carbonate (1,250 mg) tablets and asked to take two or three tablets daily. Patients were counseled on signs and symptoms of hypocalcemia. Most patients required only acetaminophen or nonsteroidal antiinflammatories for pain control.
The standard surgical approach consisted of exploring at least one side of the neck under general endotracheal anesthesia. If patients had positive preoperative scans, unilateral exploration with excision of the adenoma and visual confirmation of a normal parathyroid gland was considered an option.
Data were obtained by reviewing hospital records and charge sheets. All sestamibi scans in the MIRP group were reviewed and interpreted before surgery by both the surgeon and the radiologist. The charge for the preoperative scan was included in the total hospital charge for patients in the MIRP group. Follow-up information was obtained through patient visits or phone contact with patients and their primary care physicians.
Means between groups were compared using nonpaired t tests. Data are reported as means ± standard error of the mean.
RESULTS
Demographics
The MIRP group consisted of 20 patients with an average age of 57 ± 3 years; 80% were women. One patient had MEN1, two patients had a family history of benign thyroid disease, and two patients had concurrent benign thyroid disease. No patients had undergone previous thyroid surgery, but four patients had undergone previous unsuccessful parathyroid surgery. No patients had significant radiation exposure.
The standard group consisted of 20 patients with an average age of 55 ± 3 years; 70% were women. One patient had MEN1, one patient had a family history of benign thyroid disease, and one patient had concurrent benign thyroid disease. No patients had undergone previous thyroid surgery, but four patients had undergone previous unsuccessful parathyroid surgery. One patient had significant radiation exposure.
There was no statistical difference in demographics between the groups.
Diagnosis
The average preoperative serum calcium level in the MIRP group was 11.1 ± 0.2 mg/dL, the iPTH level was 109 ± 9 pg/mL, and the 24-hour urinary calcium excretion was 301 ± 23 mg. For the standard group, these figures were, respectively, 11.3 ± 0.2 mg/dL (P = NS), 140 ± 23 pg/mL (P = NS), and 308 ± 29 mg (P = NS). By definition, all patients in the MIRP group had a positive sestamibi scan. Ten of 20 patients (50%) were referred with a positive scan. Two patients also had a computed tomography scan, and one patient underwent neck ultrasonography. In the standard group, 13 of 20 (65%) had a preoperative sestamibi scan, of which 9 were positive. Five of these patients also had a computed tomography scan of the neck; four were positive. Additional studies included ultrasonography in three patients, magnetic resonance imaging in two patients, and venous sampling in one patient.
Symptoms
The signs and symptoms that patients in the two groups noted are listed in Table 1. Despite the relatively mild hypercalcemia in both groups, only 10% of patients in the MIRP group and only 15% in the standard group were considered asymptomatic. The three most common presentations in both groups were fatigue (60% in the MIRP group, 50% in the standard group), renal stones (30% MIRP, 30% standard) and decreased bone density (30% MIRP, 55% standard).
Table 1. SYMPTOMS ASSOCIATED WITH PRIMARY HYPERPARATHYROIDISM
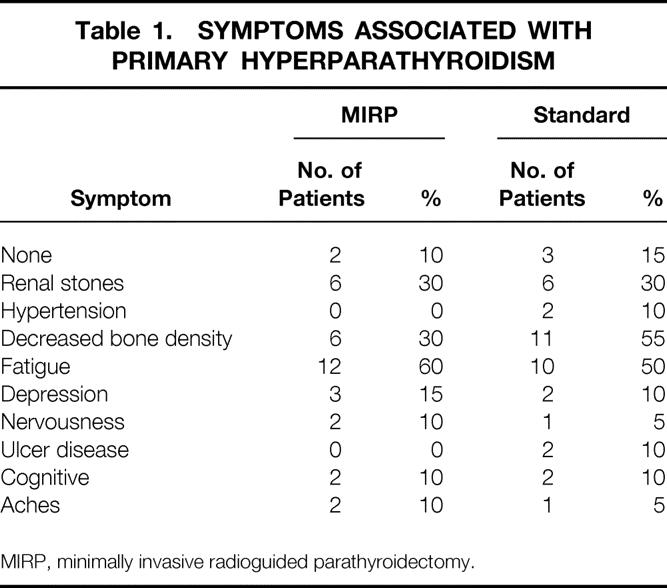
MIRP, minimally invasive radioguided parathyroidectomy.
Surgical Data
Of the 20 patients who underwent MIRP, MAC was successful in 13 (65%) and general endotracheal anesthesia was used in 7. One patient was converted from MAC to general endotracheal anesthesia because of inability to remain immobile. All 20 patients in the standard group received general endotracheal anesthesia. Twelve patients underwent a bilateral neck exploration and eight underwent unilateral neck exploration; all of the latter patients had some preoperative imaging performed. Operative and recovery room times are listed in Table 2. Operative time, total time in the operating room, and time in the recovery room were all significantly decreased in the MIRP group. In addition, although frozen-section confirmation was obtained in all 20 patients in the standard group, it was obtained in only 9 of the 20 patients in the MIRP group.
Table 2. OPERATIVE DATA
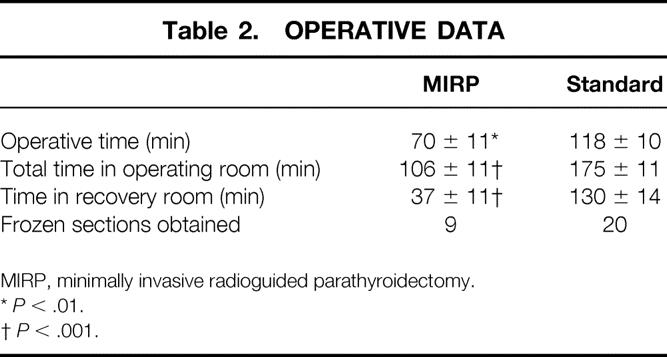
MIRP, minimally invasive radioguided parathyroidectomy.
*P < .01.
†P < .001.
Sestamibi Scans
In the MIRP group, 19 of 20 patients had a preoperative sestamibi scan 2 to 3 hours before surgery (the remaining patient was injected only). The radiologist interpreted 10 of the scans as positive for a right-sided adenoma and 9 as positive for a left-sided adenoma. There was 100% correlation between these readings and the surgical findings. The radiologist also interpreted the scan as suggesting an inferior adenoma in 18 patients and a superior adenoma in 1 patient. However, at surgery, four of the “inferior adenomas” were superior adenomas that tracked down behind the corresponding lobe of the thyroid. After surgery, the scans were reinterpreted by two masked, independent nuclear medicine physicians with 100% concurrence with the preoperative interpretation.
Pathology and Postoperative Results
Final pathology was consistent with parathyroid adenoma in 19 of 20 patients in each group. The mean weight of the adenoma was 1,989 ± 722 (range 280–11,700) mg in the MIRP group and 1,070 ± 313 (range 240–5990) mg in the standard group. One patient in each group had hyperplasia consistent with known MEN1 syndrome. Hypercalcemia was corrected in all 40 patients. The mean postoperative calcium level at 2-week follow-up was 9.3 ± 0.2 mg/dL in the standard group and 9.1 ± 0.2 mg/dL in the MIRP group (P = NS). No patients in either group have had recurrent hypercalcemia.
Complications
There were no temporary or permanent recurrent laryngeal nerve injuries in either group. In the standard group, the one patient with MEN1 syndrome underwent a total parathyroidectomy with autotransplantation complicated by temporary hypocalcemia. One additional patient had two episodes of atrial fibrillation after surgery with no sequelae, and there was one case of cellulitis. In the MIRP group, one patient had mild transient hypocalcemia after surgery, predominately as a result of significant bone hunger.
Length of Stay
The average length of stay was 1.35 ± 0.22 (range 1–4) days in the standard group; in the MIRP group, 13 of 20 patients (65%) were discharged within 5 hours after surgery. Two patients stayed 2 days: one was the first patient, and the second was kept because of concern for possible bone hunger after resection of an 11.7-g adenoma.
Costs
Hospital charges for the operating room, recovery room, and total hospital charges are shown in Table 3. Operating room charges were $4,944 ± 271 in the standard group and $2,590 ± 308 in the MIRP group (P < .001). Recovery room charges were $436 ± 10 in the standard group and $201 ± 51 in the MIRP group (P < .001). Total hospital charges were $7,187 ± 400 in the standard group and $3,782 ± 426 in the MIRP group (P < .001).
Table 3. OPERATIVE AND HOSPITAL CHARGE DATA
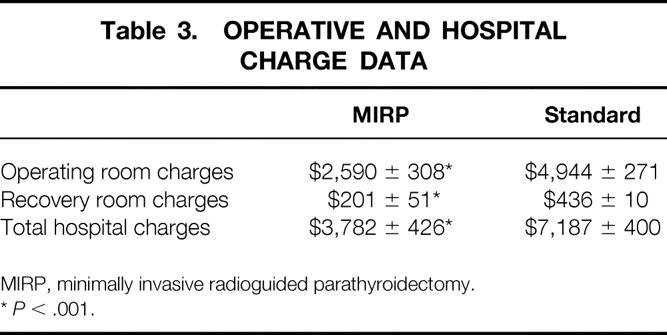
MIRP, minimally invasive radioguided parathyroidectomy.
*P < .001.
DISCUSSION
The MIRP technique as a curative procedure for primary hyperparathyroidism has been championed by Norman et al 7–10 during the past 3 years. The technique was initiated at our institution in July 1998. There are two dominant features of the technique that would at first glance appear contrary to traditional surgical teachings. The first is that one makes no attempt to locate and identify all four of the parathyroid glands. The second is that most patients are discharged from the hospital the same day as the surgical procedure. The latter is possible because most of these procedures are performed using MAC.
The purpose of this study was to review the first 20 consecutive MIRP procedures performed at our institution and to compare them with an equal number of patients who underwent more traditional parathyroidectomies. Our primary findings were as follows:
• Sestamibi scintigraphy has a high degree of accuracy, thus enabling MIRP.
• MIRP can be performed safely, and most patients tolerated conscious sedation extremely well, leading to a significantly reduced hospital length of stay.
• The commercially available probe could guide the line of dissection, allowing the procedure to be done expediently and with cure.
• MIRP reduced operative and hospital charges by almost 50%.
It has generally been believed that in 80% of cases, primary hyperparathyroidism was due to a parathyroid adenoma of one of the four glands. 11 Ten percent to 15% of the time, four-gland hyperplasia was the cause. In the remaining instances, a double or triple adenoma was the cause. Recently, Denham and Norman 7 performed a meta-analysis based on 50 reports in the literature encompassing 6,331 patients with primary hyperparathyroidism: 87% had a single adenoma, 9% had four-gland hyperplasia, and fewer than 3% had double or triple adenomas. Thus, if one excludes patients with a known family history of primary hyperparathyroidism or MEN, probably more than 90% of patients will have single-gland disease.
Since the days of Captain Martell, parathyroid glands have been notorious for being located in aberrant locations. 12–15 Hence, locating these glands can be the most significant challenge of the procedure. Failure to locate the adenoma generally leads to persistent primary hyperparathyroidism. Although no large series have reported a 100% cure rate, initial cure rates of 97% to 99% have been reported by highly experienced surgical teams. 4,5 Despite the general intent to identify all four glands, four glands were identified 44% of the time and three glands were identified in an additional 37% of the patients. 5 Thus, even in bilateral explorations for primary hyperparathyroidism by experienced parathyroid surgeons, all four glands are often not routinely identified.
Failed parathyroidectomy resulting in persistent primary hyperparathyroidism can lead to a multitude of additional tests—nuclear medicine imaging, ultrasound, computed tomography and magnetic resonance imaging scans, venous sampling, and arteriography—in an attempt to locate the missing gland. 6,12,16 Costs are significantly greater than for the initial procedure, 17 and the complication rate is also not insignificant. Carty and Norton 12 reported a 95% success rate at reoperation, with a 6.6% rate of recurrent laryngeal nerve injury and an 8.3% rate of postoperative hypocalcemia. Thompson et al 18 recently reported an 88% cure rate at reoperation, with a 13% rate of hypocalcemia and a 0.8% incidence of nerve injury. In interpreting reoperative results, we must remember that the hypoparathyroidism is most likely secondary to injury or removal of normal parathyroid glands at the initial procedure rather than to injury to normal glands at reoperation.
Imaging of parathyroid glands before an initial neck exploration was given little weight before the mid-1990s. 15 Noninvasive imaging methods, including scintigraphy, had sensitivities of less than 80% and significant false-positive rates. 6 A 1991 NIH Consensus Development Conference 19 concluded that noninvasive imaging methods were unreliable, with a 15% false-positive rate and only a 60% true-positive rate. The conference statement concluded that preoperative imaging failed to reduce the operative time, the cost, or the complication rate and did not prevent failed operations.
During the past decade, the potential for unilateral neck exploration begin to be reexamined seriously. Beginning in 1992, scintigraphy advanced with the use of 99mTc-sestamibi. 20 Sestamibi is distributed in proportion to blood flow and is sequestered intracellularly in the mitochondria. The large number of mitochondria present in the cells of most parathyroid adenomas may be responsible for the high uptake and slow washout seen with parathyroid adenomas compared with surrounding thyroid tissue. Imaging has been performed either as a subtraction scan 21 or using a dual-phase technique in which initial and then delayed images are obtained. 20 In general, the delayed images are obtained approximately 2.5 to 3 hours after injection.
Using the sestamibi scan, investigators have reported greatly improved sensitivities for the detection of adenomas. 22,23 Denham and Norman 7 performed a meta-analysis of reported sestamibi scan results. Of 784 patients with primary hyperparathyroidism undergoing an initial operation, the scan had sensitivities of 80% to 100% (average 91%) and an average specificity of 98.8%. The authors calculated that 78% of patients with primary hyperparathyroidism would be candidates for unilateral exploration, and that such exploration would be cost-effective.
Unilateral exploration had been proposed in 1982 by Tibblin et al 24 and again in 1993 by Worsey et al, 25 but it was not until the development of the sestamibi scan that the idea began to generate interest. In 1997, Norman and Chheda 8 published their results using the MIRP procedure in 15 patients. The smaller incision and the more directed approach allowed the procedure to be performed with intravenous sedation and local anesthesia in 10 of the 15 patients; all were cured, and the average operative time was 48 minutes. This experience has been expanded, and Norman et al 26 recently reported on 250 consecutive patients successfully cured after undergoing radioguided parathyroidectomy.
To obtain as much information as possible from the scan, Norman and Chheda 8 have advocated anterior views along with right and left anterior oblique views. Although the oblique views are not necessary to determine the side of the adenoma, they provide information about the relation of the adenoma to the thyroid. Two of the 20 patients in the current series had intrathyroidal adenomas that were suspected from the scan (see Fig. 2). Right or left superior adenomas that have enlarged and tracked down along the posterior aspect of the respective thyroid lobe may be misinterpreted as inferior adenomas. However, this is of no consequence, because the probe guides the dissection toward the adenoma regardless of the anatomical origin.
Although Norman and Denham 10 have reported no false-positive scans to date, Thompson et al 18 have reported a fairly significant false-positive rate in a relatively small sample of patients being evaluated for repeat parathyroid surgery. We have seen only one false-positive scan (not in this series). Thus, although the incidence of a false-positive scan is unlikely to be zero, its overall incidence is low. In terms of double and triple adenomas, we have had one patient whose scan detected only one of two adenomas (again, not in this series). This was identified through a planned bilateral exploration yielding a cure. Thus, although Norman et al 26 report very high cure rates, it is unlikely that any technique will yield 100% cure rates in large series in which patients are followed up for years.
Another recent development that has affected parathyroid surgery is the quick PTH assay, 27 which yields a PTH determination in approximately 15 minutes. Combined with the short half-life of PTH, this allows the drop in PTH to be assessed during surgery after resection of the adenoma. Combining the scan with the assay, Irvin et al 28 and Carty et al 29 performed unilateral explorations based on a positive scan. Intraoperative PTH determinations were used to confirm the completeness of the procedure. However, recent data from Garner and Leight 30 and Gordon et al 31 suggest that the intraoperative PTH assay will not eliminate failure, despite this sophisticated approach.
We use the intraoperative PTH assay in most repeat parathyroidectomies. The upshot is generally that the cause of the failed initial parathyroidectomy was a failure to find the single enlarged adenoma rather than failing to understand the pathophysiology. 16,18 Thus, the challenge is to find the adenoma. In our experience, the quick PTH assay primarily serves to confirm that the parathyroid adenoma had been correctly located before surgery and removed. A recent report from the Mayo Clinic analyzing the impact of sestamibi scanning and the intraoperative PTH assay on repeat parathyroid surgery found that neither cure rates nor surgical complication rates were significantly altered by the changes in technology. 18 Persistent multigland disease was the major cause of reoperative failure in these patients. Norman and Denham 10 recently reported on the use of MIRP for repeat parathyroid surgery. Although the series was small, the technique was highly successful and reduced the number of preoperative imaging studies obtained.
Thus, two central questions are whether the cure rates of 97% to 99%4,5 observed with careful bilateral exploration by highly experienced surgeons can be improved on, and whether such a goal should be the major focus of our efforts. Although it is unlikely that either the MIRP or the quick PTH techniques will yield 100% cure rates in multiple large series, it is also true that cure rates of 97% to 99% probably do not reflect parathyroid surgery across the country. Thus, although a successful surgical procedure is paramount, the primary drive for unilateral exploration ultimately may center around patient convenience, perception, and costs. In the current series, 13 of 20 patients (including 8 of the last 10) underwent successful surgery with only intravenous sedation and local anesthesia, and 65% of the patients could be safely discharged from the hospital within 5 hours after surgery. The early discharge reflects the relative comfort these patients have as a result of to the smaller incision, the decreased degree of dissection, and the avoidance of general anesthesia. These numbers may improve with experience.
The logistics of coordinating these procedures may seem complicated, but Figure 4 shows a protocol that works well at our institution. Patients do not need to have a scan before the day of surgery. However, if the patient has not been scanned, there needs to be the understanding that a standard bilateral exploration will be performed under general endotracheal anesthesia if the scan does not localize a solitary adenoma.
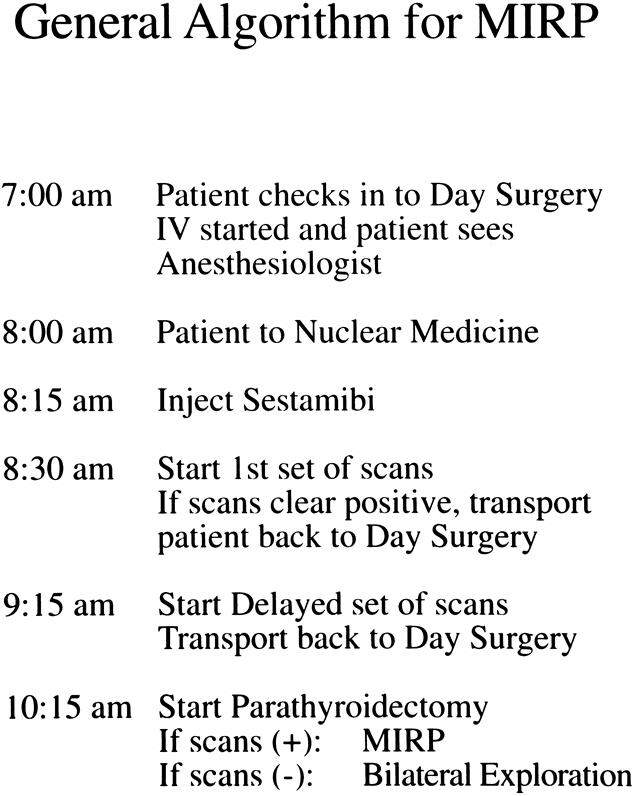
Figure 4. Algorithm followed by patients scheduled to undergo minimally invasive radioguided parathyroidectomy (MIRP).
Cost and charge data are often subject to considerable criticism. However, both groups in our study underwent their procedures during a similar time period, at a single institution, by a single surgeon. Thus, broad comparisons should be valid. As such, patients undergoing MIRP had operative and total hospital charges that were only 52% of the charges submitted for patients undergoing more standard parathyroidectomy.
Some patients with a positive parathyroid scan may not be ideal candidates for MIRP. Such patients may be candidates for what one might term a radioguided-assisted parathyroidectomy. Figure 5 depicts a scan from one such patient. This patient had MEN1 syndrome and 20 years ago had undergone bilateral exploration. Both inferior parathyroid glands were identified and removed, but neither superior parathyroid gland was identified. The sestamibi parathyroid scan identified both superior parathyroids. Bilateral exploration under general endotracheal anesthesia was performed. One hour before the procedure, sestamibi was injected. During the procedure, the hand-held gamma probe was used to direct the dissection through considerable scar, and both superior glands were easily identified. A subtotal parathyroid resection was performed and the hypercalcemia was corrected.
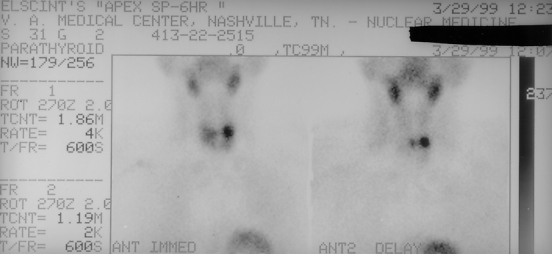
Figure 5. Sestamibi parathyroid scan from a patient with MEN1 syndrome. Twenty years ago, only the two inferior parathyroid glands were identified and removed. The scan identified the location of the two missed superior parathyroid glands.
In summary, MIRP appears to be both safe and efficacious. The issue of whether cure rates will be increased will be answered only with multiple large series. However, the convenience of the procedure may convince many primary care physicians and endocrinologists to refer for parathyroidectomy patients with what is perceived to be minimal to moderate disease. In addition, elderly patients with primary hyperparathyroidism and symptoms such as fatigue, depression, or cognitive changes may benefit from parathyroidectomy and may be more willing to undergo such a procedure if general endotracheal anesthesia can be avoided. In any event, during the next few years, more directed approaches for parathyroid disease appear inevitable. The MIRP technique may significantly change the management of primary hyperparathyroidism.
Acknowledgment
The authors thank Paul Gross for the illustration.
Discussion
Dr. Jeffrey F. Moley (St. Louis, Missouri): Virtually all the experienced parathyroid surgeons I know are routinely using some form of minimally invasive parathyroid surgery, either incorporating sestamibi scanning or intraoperative parathyroid hormone monitoring, and often are doing this in an outpatient setting under local or regional anesthesia.
These techniques do have reported failures, both false-positives and false-negatives; our own experience at Washington University has confirmed this. Despite Dr. Goldstein’s perfect results in his initial 20 patients, I am sure that he will eventually encounter patients with persistent hyperparathyroidism that will require additional procedures. Ultimately, however, this approach is patient-driven, and patients are accepting of the small risk of persistent hyperparathyroidism and a subsequent need for additional procedure because the vast majority will be cured in a single operation with a small incision, often in an outpatient setting.
I have a question about the need for a handheld probe in the operating room. It is often difficult to orchestrate this procedure, that is, using the radioguided technique intraoperatively because it requires that nuclear medicine, the operating room staff, and the surgeon all be on board and on the same timetable. This is difficult to orchestrate. Do we really need to use a handheld probe intraoperatively for parathyroid adenomas in the usual location? If the scan shows an adenoma on the right or left side of the neck, an experienced parathyroid surgeon should be able to find that adenoma quickly and easily, even under local anesthesia or regional anesthesia, without the use of a cumbersome handheld probe.
Dr. Arnold G. Diethelm (Birmingham, Alabama): Very simply, an accurate diagnosis in parathyroid surgery is essential. There needs to be an elevated calcium, an elevated parathyroid hormone, and preferably, a 24-hour urine collection. Then the surgeon has to find the gland and be certain that the operation performed is appropriate. Is it a four-gland problem, i.e., hyperplasia, or is it a one-gland problem, i.e., an adenoma? The use of the technique today showed us a relatively simple approach to localization of the offending gland. In turn, this approach shortens the operative time and the costs, and allows the procedure occasionally to be performed under local anesthesia.
I have a few questions for Dr. Goldstein.
First, what do you do if the preoperative sestamibi scan is negative?
Second, do you use intraoperative PTH assay to confirm that the operation is complete? Again, one has to be absolutely certain that when you finish the operation, as best you can tell, you don’t have to return at another time.
And third, can you locate normal glands with the probe, and is there any gland size that is too small to locate with the probe that could be a small adenoma, a weight of 150 or 160 mg?
I think this is an important contribution, and if it will save time, improve accuracy, and eliminate the need, in some instances, for general anesthesia, then it’s going to be a very important part of the future.
Dr. J. Kenneth Jacobs (Nashville, Tennessee): During a similar 20-month period in 1998 and 1999 at St. Thomas Hospital, also in Nashville, I have operated, with the same surgical residents as Dr. Goldstein uses, on 53 patients with primary hyperparathyroidism. We do not use preoperative sestamibi scans or any other type of localization studies for these patients with primary hyperparathyroidism unless they have undergone previous neck exploration. As the reagents for intraoperative PTH assay are stable for only 8 hours and cost the hospital $600, we have not done any intraoperative PTH assay determinations.
We have used a bilateral standard operative technique with an attempt made to identify all parathyroid glands in the neck. [Slide] An average of 3.4 glands were found in these patients. There were no recurrent laryngeal nerve injuries, and all patients’ calcium levels returned to normal values. The average operative time was 74 minutes, with extremes of 45 to 124 minutes, the latter occurring in a patient who also had a substernal goiter removed.
Only recently have we converted from our traditional 2-day postoperative length of stay. Except in two patients, one who had bone hunger and another with a compression fracture due to bone disease, hospitalizations longer than 48 hours have not been necessary.
Forty-four patients had a single adenoma, three patients had hyperplasia, six patients had a double adenoma. The smaller of the six patients with double adenoma was 426 mg, with the extremes of the second adenoma being anywhere from 150 mg to 1350 mg.
I am concerned about the six patients, 11% of this group, with double adenomas. My question for Dr. Goldstein is, had bilateral exploration not been performed on these patients, would they have had a persistence of their hypercalcemia or a recurrence of their hyperparathyroidism at a later date?
Dr. James G. Chandler (Boulder, Colorado): Thank you for letting me be an add-on. I’m an add-on because when I saw your picture of the incision, it looked like it was in the front, and it seems to me that if you want to take the most direct route to a parathyroid, the front is the hard way to go. You really have to approach it posteriolateral if you could, and you can do that by going behind the sternocleidomastoid muscle. If you have the advantage of good imaging so you can free yourself from the fetters of your forefathers, you don’t have to go in front anymore—you can sneak through the back and be home sooner.
Dr. Richard E. Goldstein (Closing Discussion): First, taking the comments by Dr. Moley, do we really need the probe? As we all know, quite a number of times one makes a small incision, looks in the area where we expect it to be based on the scan, and there it is. But there clearly have been several patients where the probe has been extremely helpful. In addition, the probe allows a little bit less extensive dissection to get down to that adenoma and, therefore, I think the patients do experience less postoperative discomfort.
His second point deals with the concept of failures. I think realistically, with any technique used by surgeons, there will be some operative failures—that’s the nature of this beast. But I think that most patients have single adenomas that can be cured by a very directed approach, and they can go home on the same day.
Putting it into some perspective, I think most patients can come in, have a 40-minute procedure, and go home that day. One or two of those patients out of 100 potentially could be operative failures and need to come back for a more formal approach under a general anesthesia. I think patients are quite willing to take that risk, and I think surgeons are willing to take that risk.
Dr. Diethelm had some very nice comments. What we are now doing is not asking patients to have a scan prior to the day of their operative procedure, but we do tell them that they will have a scan that morning. If that scan is negative or we are not comfortable with it, then we will explore both sides of the neck under general anesthesia. I think, as in any surgical field, surgical judgment continues to play a very important role.
Do we use the FAST parathyroid assay? Occasionally. We did not use it on these 40 patients. We do have it available, and we have used it in the past, largely for reoperative necks. But generally, my feeling is that most operative failures are due to a failure to find the offending adenoma in these patients, and that if in fact you do identify and it clearly appears to be adenoma, that the overwhelming high probability is that those patients will, at that point, be cured.
There was a question as to whether there is a certain size that is too small to identify. I’m really not sure. I think that approximately 10% of the parathyroid scans are still negative, when we know that they have primary hyperparathyroidism. One of the future directions may be ways to try to make that scan more sensitive.
Dr. Jacobs, you have been both a mentor and a friend to me, and you are well known for your long interest in parathyroid surgery as well as your excellent operative results. As far as your six patients out of 53 with the double adenoma, first, that is a very high rate. I think most accepted rates would be somewhere between 2% to 4%. Second, if the parathyroid scan does truly have a 90% sensitivity of imaging and adenoma, and there is a 2% to 4% probability of a double adenoma, that essentially one out of 100 patients will have a failed operation based on the scan missing it.
I also want to emphasize that there is absolutely nothing wrong with exploring both sides of the neck—that really needs to be borne in mind. However, I think that the drum for unilateral surgery has started. I don’t think it’s going to be silenced, and the real question is not “if” but “when” and “how.”
Dr. Chandler’s comment on exploring from a more lateral approach is certainly very valid. We have not approached from a more lateral approach, although I think some other groups have. I actually find that we are able to approach the inferior adenomas extremely well from a small transverse incision. As far as approaching the superior adenomas, what we do is free up the inferior aspect of the thyroid lobe and then tunnel under the lobe up toward the adenoma, and that has actually worked very well.
Footnotes
Correspondence: Richard E. Goldstein, MD, PhD, D-5217 MCN, Vanderbilt University, Nashville, TN 37232.
Presented at the 111th Annual Meeting of the Southern Surgical Association, December 5–8, 1999, The Homestead, Hot Springs, Virginia.
E-mail: Richard.Goldstein@mcmail.vanderbilt.edu
Accepted for publication December 1999.
References
- 1.Melton LJ III. Epidemiology of primary hyperparathyroidism. J Bone Min Res 1991; 6:S25–S29. [DOI] [PubMed] [Google Scholar]
- 2.Heath H III, Hodgson SF, Kenneday MA. Primary hyperparathyroidism: incidence, morbidity, and potential economic impact in a community. N Engl J Med 1980 302:189–193. [DOI] [PubMed] [Google Scholar]
- 3.Ljunghall S, Hellman P, Rastad J, Akerstrom G. Primary hyperparathyroidism: epidemiology, diagnosis and clinical picture. World J Surg 1991; 15:681–687. [DOI] [PubMed] [Google Scholar]
- 4.Auguste L-J, Attie JN, Schnaap D. Initial failure of surgical exploration in patients with primary hyperparathyroidism. Am J Surg 1990; 160:333–336. [DOI] [PubMed] [Google Scholar]
- 5.van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg 1991; 15:688–692. [DOI] [PubMed] [Google Scholar]
- 6.Miller DL. Pre-operative localization and interventional treatment of parathyroid tumors: when and how? World J Surg 1991; 15:706–715. [DOI] [PubMed] [Google Scholar]
- 7.Denham DW, Norman J. Cost-effectiveness of preoperative sestamibi scan for primary hyperparathyroidism is dependent solely upon the surgeon’s choice of operative procedure. J Am Coll Surg 1998; 186:293–305. [DOI] [PubMed] [Google Scholar]
- 8.Norman J, Chheda H. Minimally invasive parathyroidectomy facilitated by intraoperative nuclear mapping. Surgery 1997; 122:998–1004. [DOI] [PubMed] [Google Scholar]
- 9.Norman J, Chheda H, Farrell C. Minimally invasive parathyroidectomy for primary hyperparathyroidism: decreasing operative time and potential complications while improving cosmetic results. Am Surg 1998; 64:391–395. [PubMed] [Google Scholar]
- 10.Norman J, Denham D. Minimally invasive radio-guided parathyroidectomy in the reoperative neck. Surgery 1998; 124:1088–1093. [DOI] [PubMed] [Google Scholar]
- 11.Thompson NW, Eckhauser FE, Harness JK. The anatomy of primary hyperparathyroidism. Surgery 1982; 92:814. [PubMed] [Google Scholar]
- 12.Carty SE, Norton JA. Management of patients with persistent or recurrent primary hyperparathyroidism. World J Surg 1991; 15:716–723. [DOI] [PubMed] [Google Scholar]
- 13.Thompson NW. The history of hyperparathyroidism. Acta Chir Scand 1990; 156:5–21. [PubMed] [Google Scholar]
- 14.Wang CA. The anatomic basis of parathyroid surgery. Ann Surg 1976; 183:271–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaplan EL, Yashiro T, Salti G. Primary hyperparathyroidism in the 1990s. Ann Surg 1992; 215:300–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peeler BB, Martin WH, Sandler MP, Goldstein RE. Sestamibi parathyroid scanning and preoperative localization studies for patients with recurrent/persistent hyperparathyroidism or significant comorbid conditions: development of an optimal localization strategy. Am Surg 1997; 63:37–46. [PubMed] [Google Scholar]
- 17.Doherty GM, Weber B, Norton JA. Cost of unsuccessful surgery for primary hyperparathyroidism. Surgery 1994; 116:954–958. [PubMed] [Google Scholar]
- 18.Thompson G, Grant C, Perrier N, et al. Reoperative parathyroid surgery in the era of sestamibi scanning and intraoperative parathyroid hormone monitoring. Arch Surg 1999; 134:699–705. [DOI] [PubMed] [Google Scholar]
- 19.Consensus development conference statement. J Bone Min Res 1991; 6:S9–S13. [DOI] [PubMed]
- 20.O’Doherty MJ, Kettle AG, Wells P, Collins REC, Coakley AJ. Parathyroid imaging with technetium-99m-sestamibi: preoperative localization and tissue uptake studies. J Nucl Med 1992; 33:313–318. [PubMed] [Google Scholar]
- 21.Casas AT, Burke GJ, Mansberger AR, Wei JP. Impact of technetium-99m sestamibi localization on operative time and success of operations for primary hyperparathyroidism. Am Surg 1994; 60:12–17. [PubMed] [Google Scholar]
- 22.Wei JP, Burke GJ, Mansberger AR. Prospective evaluation of the efficacy of technetium-99m sestamibi and iodine-123 radionuclide imaging of abnormal parathyroid glands. Surgery 1992; 112:111–117. [PubMed] [Google Scholar]
- 23.Carter WB, Sarfati MR, Fox KA, Patton DD. Preoperative detection of sporadic parathyroid adenomas using technetium-99m sestamibi: what role in clinical practice? Am Surg 1997; 63:317–321. [PubMed] [Google Scholar]
- 24.Tibblin S, Bondeson A-G, Ljungberg O. Unilateral parathyroidectomy in hyperparathyroidism due to single adenoma. Ann Surg 1982; 195:245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Worsey MJ, Carty S, Watson C. Success of unilateral neck exploration for sporadic primary hyperparathyroidism. Surgery 1993; 114:1024–1030. [PubMed] [Google Scholar]
- 26.Murphy C, Farrell C, Norman J. The 20% rule: a simple, instantaneous radioactivity measurement defines cure and allows elimination of frozen sections and hormone assays during parathyroidectomy. Surgery 1999; 126:1023–1029. [DOI] [PubMed] [Google Scholar]
- 27.Irvin GL III, Dembrow VD, Prudhomme DL. Operative monitoring of parathyroid gland hyperfunction. Am J Surg 1991; 162:299–302. [DOI] [PubMed] [Google Scholar]
- 28.Irvin GL, Prudhomme DL, Deriso GT, Stakianakis G, Chandarlapaty SKC. A new approach to parathyroidectomy. Ann Surg 1994; 219:574–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carty SE, Worsey J, Virgi MA, Brown ML, Watson CG. Concise parathyroidectomy: the impact of preoperative SPECT 99m-Tc sestamibi scanning and intraoperative quick parathormone assay. Surgery 1997; 122:1107–1116. [DOI] [PubMed] [Google Scholar]
- 30.Garner SC, Leight GS Jr. Initial experience with intraoperative PTH determinations in the surgical management of 130 consecutive cases of primary hyperparathyroidism. Surgery 1999; 126:1132–1137. [DOI] [PubMed] [Google Scholar]
- 31.Gordon LL, Snyder WH, Wians F Jr, Nwariaku F, Kim LT. The validity of quick intraoperative parathyroid hormone assay: an evaluation in 72 patients based on gross morphologic criteria. Surgery 1999; 126:1030–1035. [DOI] [PubMed] [Google Scholar]