Abstract
Objective
To investigate the feasibility of a 48-hour postoperative stay program after colonic resection.
Summary Background Data
Postoperative hospital stay after colonic resection is usually 6 to 12 days, with a complication rate of 10% to 20%. Limiting factors for early recovery include stress-induced organ dysfunction, paralytic ileus, pain, and fatigue. It has been hypothesized that an accelerated multimodal rehabilitation program with optimal pain relief, stress reduction with regional anesthesia, early enteral nutrition, and early mobilization may enhance recovery and reduce the complication rate.
Methods
Sixty consecutive patients undergoing elective colonic resection were prospectively studied using a well-defined postoperative care program including continuous thoracic epidural analgesia and enforced early mobilization and enteral nutrition, and a planned 48-hour postoperative hospital stay. Postoperative follow-up was scheduled at 8 and 30 days.
Results
Median age was 74 years, with 20 patients in ASA group III-IV. Normal gastrointestinal function (defecation) occurred within 48 hours in 57 patients, and the median hospital stay was 2 days, with 32 patients staying 2 days after surgery. There were no cardiopulmonary complications. The readmission rate was 15%, including two patients with anastomotic dehiscence (one treated conservatively, one with colostomy); other readmissions required only short-term observation.
Conclusion
A multimodal rehabilitation program may significantly reduce the postoperative hospital stay in high-risk patients undergoing colonic resection. Such a program may also reduce postoperative ileus and cardiopulmonary complications. These results may have important implications for the care of patients after colonic surgery and in the future assessment of open versus laparoscopic colonic resection.
The postoperative hospital stay after colonic resection is usually 6 to 12 days, 1–6 with a complication rate of 10% to 20%, because many patients are elderly and at high risk. The recent introduction of multimodal postoperative rehabilitation regimens including epidural analgesia, early enteral nutrition, and early mobilization and revision of the surgical care program have reduced the hospital stay to approximately 5 days. 7–9 The introduction of laparoscopic-assisted colonic surgery has also reduced the hospital stay to approximately 4 to 6 days. 6,10,11 However, in studies on the effect of laparoscopic-assisted colonic resection, there has rarely been a focus on revising perioperative care programs and on including optimal analgesia, early mobilization, and early enteral nutrition. A combination of laparoscopic-assisted colonic resection in high-risk patients with epidural analgesia, early enteral nutrition, and early mobilization resulted in a postoperative hospital stay of 2 to 3 days. 12
The potential for further improvement of the postoperative course, the length of hospital stay, and the complication rate after open colonic resection has not been evaluated, except for our preliminary findings in 16 patients undergoing sigmoidectomy, where early recovery and a median hospital stay of 2 days were achieved. 13 After these initial and hypothesis-generating findings, an accelerated multimodal care program was introduced as a routine in our department of surgical gastroenterology from January 1, 1998. Here we report our accumulated results in the first 60 consecutive patients.
METHODS
Subjects
This study was a prospective investigation of 60 consecutive patients scheduled for elective colonic resection (excluding planned low anterior resection and rectum extirpation, and patients undergoing surgery for inflammatory bowel disease). The results include the initial 16 patients 13 and the next 44 patients from January to October 1998. The study was approved by the local ethical committee.
Study Design
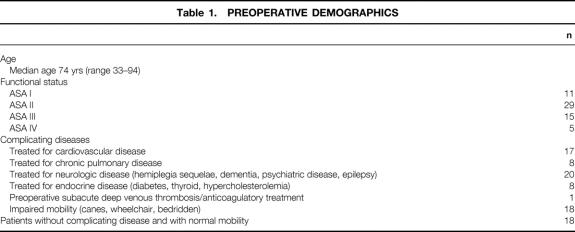
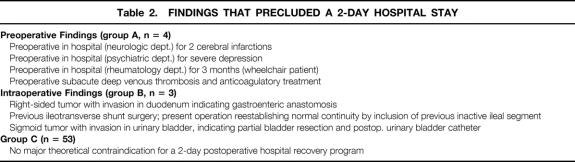
When the indication for surgery was established, the patient was informed by the research team about the accelerated rehabilitation program involving a planned 48-hour postoperative hospital stay, presuming that all organ functions had returned to normal. Patients were assessed before surgery with a detailed description of concurrent diseases (Table 1) and American Society of Anesthesiologists’ (ASA) classification. Group A comprised patients with special factors that precluded a 2-day hospital stay that were identified before surgery (Table 2). Group B comprised patients whose precluding factors were identified during surgery. The remaining patients (group C) had no precluding factors, despite the presence of severe complicating diseases.
Table 1. PREOPERATIVE DEMOGRAPHICS
Table 2. FINDINGS THAT PRECLUDED A 2-DAY HOSPITAL STAY
Anesthesia and Analgesia
No premedication was administered. Before surgery, a thoracic epidural catheter was inserted at T6–7 for right hemicolectomy and at T8–10 for left-sided and sigmoid resection. It was tested with 3 mL 2% lidocaine with epinephrine, followed by 6 + 6 mL 0.5% bupivacaine. A bolus of epidural morphine (2 mg) was given in patients 70 years or younger; 1 mg was given in older patients. During surgery, an additional 4 mL 0.5% bupivacaine was administered hourly, and a continuous infusion of 0.25% bupivacaine with morphine (0.05 mg/mL) was initiated at a fixed rate of 4 mL per hour. After preoperative assessment of the epidural block, general anesthesia was introduced with propofol (2–3 mg/kg), remifentanil (1–2 mg), and cisatracurium (0.15 mg/kg) and maintained with propofol (2–4 mg/kg/hr) and remifentanil (1 μg/kg/min). The first 16 patients received additional intrathecal anesthesia with lidocaine. 13 Intraoperative fluid administration was standardized to 1,500 mL isotonic saline + 500 mL 6% hydroxyethyl starch. Additional fluid therapy or transfusion required discussion between the anesthesiologist and the surgeon, if blood loss exceeded 500 mL. Thirty minutes before termination of anesthesia, ketorolac (30 mg) and ondansetron (4–8 mg) were given intravenously. At the end of surgery, 20 mL 0.25% bupivacaine was given subfascially or intramuscularly in the incision. Intraoperative normothermia was maintained with a Bair-Hugger (Augustine Medical, Eden Prairie, MN). After surgery, continuous epidural analgesia with bupivacaine and morphine was maintained for 48 hours. Acetaminophen tablets were administered after surgery (2 g every 12 hours). If pain relief was insufficient, either ibuprofen (600 mg orally) or additional epidural 0.125% bupivacaine (6 mL) was given.
Surgical Procedure
Right-sided hemicolectomy was performed with a horizontal incision 2 to 3 cm above the umbilicus, resection of the transverse colon with a transverse incision cephalad to the umbilicus, and left-sided hemicolectomy and sigmoid resection with a curved incision in the left iliac fossa extended up toward the curvature when necessary. All anastomoses were hand-sewn.
Postoperative Regimen
Gastrointestinal tubes were not used. Postoperative mobilization and oral intake followed a well-defined nursing care program (Table 3). Additional cisapride (20 mg) was given every 12 hours and 1 g magnesium oxide was given every 12 hours from the evening of the day of surgery. The bladder catheter was removed routinely 24 hours after surgery; the epidural catheter was removed routinely on the morning of the second day (approximately 44 hours after surgery). The plan was discharge after lunch approximately 4 to 6 hours after removal of the epidural catheter, provided that all organ functions had returned to normal and pain could be managed with oral analgesics. At discharge, the patients were provided with acetaminophen (2 g every 12 hours) and ibuprofen (600 mg every 8 hours) for pain relief and a few morphine tablets (10 mg) for rescue analgesia. The patients were seen in the outpatient clinic for removal of stitches and information about histology on day 8, and a final postoperative checkup was scheduled for day 30.
Table 3. NURSING CARE PROGRAM AND GOALS AFTER ELECTIVE COLONIC RESECTION
RESULTS
Patient Characteristics and Surgical Findings
The patients consisted of a high-risk group with a median age of 74 years, 20 patients belonging to ASA group III-IV. Eighteen patients had preoperative impaired mobilization, and most had complicating extracolonic diseases. Only 18 patients had no complicating disease and had normal preoperative mobility.
Four patients were classified before surgery as impossible to discharge from the hospital 2 days after surgery (group A): one patient had two previous cerebral infarctions and one myocardial infarction and was admitted to the neurology department; one patient was admitted to the psychiatry department for severe depression and had indications for further inpatient care; one patient was transferred from the rheumatology department after a 3-month stay in a severely deteriorated condition (wheelchair-dependent); and one patient had had a femoral venous thrombosis 10 days before surgery, which had been treated with anticoagulants requiring close postoperative monitoring.
Three patients were classified during surgery as impossible to discharge from the hospital 2 days after surgery (group B): one patient had a tumor invading the duodenum, requiring a gastroenteric anastomosis; one patient had a previous ileotransverse shunt, and the present operation included reestablishing normal intestinal continuity, including the atrophic segment; and one patient had tumor invasion in the urinary bladder wall, requiring a partial bladder resection and postoperative urinary bladder drainage.
In the remaining 53 patients (group C), although most had complicating diseases, no pre- and intraoperative findings precluded a postoperative hospital stay of 2 days. This group, for instance, included one patient with severe pulmonary disease (FEV1 = 0.56 L/min) and one patient with acute uremia and severe hypoalbuminemia (396 mmol/L). This group also included patients who underwent the following procedures in addition to the colonic resection: one patient with a ureter–ureter anastomosis because of intraoperative ureter transection during dissection of a large retroperitoneal inflammatory mass; one resection of the omentum because of severe carcinosis and malignant ascites; two small bowel resections because of tumor invasion; one salpingo-oophorectomy; and one cholecystectomy.
The colonic resections included 23 right-sided hemicolectomies, 2 resections of the colon transversum, and 34 sigmoid resections or left hemicolectomies, and 1 subtotal colectomy. Median duration of surgery was 120 minutes (range 70–360). Median intraoperative blood loss was 100 mL (range 50–2,450). Underlying colonic disease was cancer in 42 patients (Dukes’ A, 4; Dukes’ B, 22; Dukes’ C, 11; Dukes’ D, 5), lymphoma in 1 patient, and benign colonic diseases, mostly chronic diverticulitis, in 17 patients.
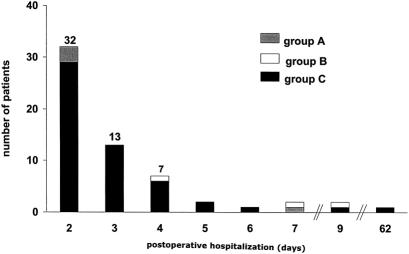
Postoperative Hospital Stay
The duration of hospital stay in the 60 patients is shown in Figure 1. Of the four group A patients, the actual stay was 2 days in three patients, because the preoperative condition was attained during this period (all were transferred back to the hospital department where they were staying before surgery). The remaining patient stayed 7 days for management of anticoagulation therapy related to the preoperative deep vein thrombosis. In the three group B patients, the lengths of stay were 4, 7, and 9 days. In the remaining patients (group C), the median postoperative hospital stay was 2 days. Three patients needed to stay more than 5 days. One patient had a stay of 6 days because of chronic joint pain with difficult mobilization, One patient had a stay of 9 days after resection of a large tumor invading the anterior abdominal wall that was partially resected but with subsequent wound dehiscence, acute reoperation, and death on day 9. One patient had a 62-day hospital stay after reoperation on day 2 because of a 15-cm-long infarction of the ileum, 15 cm away from an intact ileotransversostomy after right-sided hemicolectomy. After surgery, an intensive care stay was necessary because of multiple organ dysfunction, but the patient survived. Of the 22 patients who required a stay of 2 to 5 days, the reasons were psychosocial factors (9 patients), delayed operation (1 patient), dizziness and fatigue (4 patients), delayed return of gastrointestinal function (7 patients, see below), and unconfirmed suspicion of pneumonia (1 patient). Pain was not a limiting factor for discharge, and only approximately 10% of the patients received supplementary doses of epidural bupivacaine or systemic morphine (10–20 mg) during the hospital stay.
Figure 1. Postoperative hospital stay, including the day of surgery, in 60 patients undergoing elective colonic resection with multimodal rehabilitation.
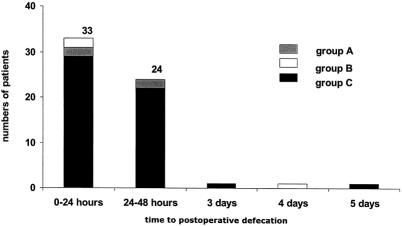
Gastrointestinal Function
Clinically, the patients tolerated early enteral nutrition, and 57 patients had defecation in the first 48 hours (Fig. 2). Defecation in the remaining patients occurred on days 3, 4, and 5. Four patients were kept in the hospital more than 2 days because of nausea or small-quantity, intermittent vomiting despite defecation.
Figure 2. Reestablishment of gastrointestinal function (defecation) in 60 patients undergoing elective colonic resection with multimodal rehabilitation.
Postoperative Complications
There were two deaths (3.3%) and an additional five patients had one complication (Tables 4 and 5). Seven patients had urinary retention requiring a single bladder catheterization between day 1 and 2. Serious complications (anastomotic leakage, small bowel infarction, wound dehiscence, or death) occurred in only five patients (8.3%). No cardiopulmonary complications were observed in the 58 survivors despite the high incidence of coexisting cardiopulmonary disease. Reasons for readmission and duration of hospital stay are detailed in Table 5. The accumulated number of days of repeat admission was 56 days, primarily from the two patients with anastomotic leakage. No complications or readmissions could be attributed to the shorter length of stay.
Table 4. DEATH AND COMPLICATIONS IN 60 PATIENTS UNDERGOING ELECTIVE COLONIC RESECTION
Table 5. READMISSIONS AMONG 60 PATIENTS UNDERGOING ELECTIVE COLONIC RESECTION
In summary, the hospital stay was 193 days for the primary operation and 56 days for readmission—in total, 249 days. Thus, for the total 60-patient population, including all high-risk groups and patients with special intraoperative findings, the median postoperative hospital stay was 3 days (range 2–62).
During the 30 days of follow-up, 73% of the patients were satisfied with the postoperative care, but 27% believed they had been discharged too early, because of feeling insecure or “fatigued.” However, at the 8- and 30-day checkups, patients were somatically and socially functioning normally or rapidly recovering. No patient’s condition deteriorated after discharge, except those mentioned above (complications or readmission).
DISCUSSION
The aim of this study was to investigate whether a multimodal rehabilitation program could enhance the recovery of organ function after elective colonic resection. The initial results of this prospective, hypothesis-generating investigation were that return of gastrointestinal function seems feasible in 2 to 3 days in more than 90% of patients with a combination of early enteral nutrition and continuous thoracic epidural analgesia including local anesthetics for 48 hours. The reduction of the conventional postoperative paralytic ileus response represents a clinical relevant achievement, because early institution of enteral nutrition may reduce postoperative infectious complications and the catabolic response to surgery. The results also support the well-established finding that continuous epidural analgesia with local anesthetics is necessary to reduce ileus, especially when compared with opioid analgesic techniques. 8,15
The finding of a median postoperative hospital stay of 2 days suggests that implementation of an early rehabilitation program may reduce or prevent the conventional impairment of different organ functions that follows elective colonic surgery. The very high-risk nature of our patients further suggests that the usual medical complications such as cardiopulmonary complications may be avoided. Important contributing factors to this finding may include early mobilization and optimal pain relief. The patients in our study averaged approximately 10 years older than those in other studies. 6,8,9,11 Among the 60 patients studied, 16 were 80 years or older, but they had a median postoperative hospital stay of 3 days, despite the fact that 5 were in high-risk group A or B. These findings are in sharp contrast to the higher complication rate reported previously after colonic resection in octogenarians. 14
In this initial study, we excluded low anterior resection from the protocol because of the well-known higher risk of anastomotic dehiscence (and thereby potential gross contamination) when combined with very early feeding. Future studies must clarify the optimal regimen for low anterior resection.
The routine use of a urinary bladder catheter with removal after 24 hours did not cause complication, even though 11% needed a single recatheterization. No patient had sequelae of cystitis or bladder dysfunction requiring a hospital stay of more than 48 hours after surgery.
The surgical complications in this high-risk patient group included one superficial wound infection treated in the outpatient clinic, a case of incisional wound bleeding treated with local suturing, and one case of wound dehiscence in a patient with tumor invasion in the abdominal wall. Two anastomotic leakages occurred after discharge, but both were diagnosed and managed early because of the occurrence of pain (one was conservatively treated; the other was treated with a colostomy). Because of the nonrandomized nature of this investigation, the potential of the multimodal rehabilitation regimen to either reduce or increase the risk of surgical complications cannot be answered, but the results suggest that the overall complication rate may be reduced, given the patient demographics.
Previous attempts to enhance postoperative recovery after open colonic resection have led to a hospital stay of approximately 5 days, 7–9 probably because the care program was designed to achieve recovery within that period. In recent years the role of laparoscopic-assisted colonic resection to enhance recovery and reduce complications has been discussed. 6,10,11 In these and other studies, the duration of hospital stay after laparoscopic resection has usually been approximately 5 days, no different from studies with multimodal rehabilitation in open resection. 7–9 We have previously demonstrated that a combination of the multimodal rehabilitation program and the laparoscopic-assisted technique could reduce hospital stay in high-risk patients to 2 to 3 days. 12 Interestingly, the present study achieved the same results with open colonic resection, suggesting that postoperative recovery may depend more on other factors such as optimal pain relief, early nutrition, and early mobilization and omission of recovery-inhibiting regimens (e.g., gastrointestinal tubes, prolonged urinary catheter drainage, drains) 15,16 than the choice of surgical technique itself (laparoscopic vs. open). Based on these findings, it may therefore be timely to perform a masked, randomized controlled trial of open versus laparoscopic-assisted colonic resection where both groups receive a multimodal rehabilitation program (with sufficient wound dressing to secure patient and nurse masking) to demonstrate the true differences between the two surgical techniques.
The relative importance of the individual components of the multimodal rehabilitation program to improve recovery has not been clearly evaluated. Thus, single-modality treatment with pain relief, 17 enteral nutrition, 15 and cisapride 18 has had only limited effects on outcome in randomized trials. The individual effects of mobilization 15 and changes in perioperative care (e.g., tubes, drains, feeding restrictions) 15,16,19 on outcome has not been established either, although several studies have demonstrated tubes, drains, and feeding restrictions to be unnecessary and to limit recovery. 15,16,19 Therefore, the multimodal effect seems rational and probably necessary to achieve major outcome effects, as observed in preliminary nonrandomized studies. 7–9,12,13
An important question is whether it is safe to discharge elderly, high-risk patients 2 days after open colonic resection. In the present study, however, no patient had acute life-threatening complications after discharge, and the few complications that did occur, including the two anastomotic leakages, were diagnosed within few hours and treated before any deterioration of the overall condition or specific organ complications developed. All patients received detailed pre- and postoperative information about calling the surgical department if any signs of complications occurred, and they were allowed to be seen in the outpatient clinic if symptoms appeared. Our findings do not support the common fear of an increased risk of anastomotic leakage or other complications with early enteral nutrition and early discharge. Although experience from larger case series obviously is necessary, our preliminary findings do not suggest that early discharge is medically inappropriate and unsafe, provided that proximity to the hospital allows readmission within a few hours if signs of complications occur.
Patient satisfaction was acceptable, although approximately 25% mentioned that they felt fatigued and insecure. This would probably not improve with a hospital stay of several more days. 15 It is our impression from the follow-up on postoperative day 8 that patients included in a multimodal rehabilitation program achieve much earlier return to normal of daily functions, and with less fatigue than in previous studies. 13,15 Obviously, more detailed studies are necessary, especially regarding the importance of educating patients and relatives, who usually expect a 5- to 10-day stay after such procedures and therefore may feel socially insecure with the early discharge.
In summary, our results suggest that a multimodal intervention with revision of traditional surgical care programs (e.g., tubes, drains, bladder catheter) combined with optimal pain relief with continuous thoracic epidural analgesia with local anesthetics and opioids, early enteral nutrition, and enforced mobilization may enhance recovery after elective colonic resection. The results bring into question the proposed advantages of laparoscopic-assisted colonic resections and call for a well-designed, masked assessment of laparoscopic versus open colonic resection in which both groups receive multimodal rehabilitation treatment. Further studies are required to document the safety of the early rehabilitation regimen and to determine whether the incidence of medical complications may be reduced.
Footnotes
Correspondence: Linda Basse, MD, Dept. of Surgical Gastroenterology 435, Hvidovre University Hospital, DK-2650 Hvidovre, Denmark.
Dr. Basse and Ms. Jakobsen are supported by a grant from Apotekerfonden 1991, and Dr. Kehlet is supported in part by grant 28809 from the Danish Research Council.
Reprints will not be available from the authors.
E-mail: L.Basse@dadlnet.dk
Accepted for publication November 19, 1999.
References
- 1.Retchen SM, Penberthy L, Desch C, et al. Perioperative management of colonic cancer under Medicare risk programs. Arch Intern Med 1997; 157:1878–1884. [PubMed] [Google Scholar]
- 2.Schoetz DJ, Bockler M, Rosenblat MS, et al. “Ideal” length of stay after colectomy: whose ideal? Dis Colon Rectum 1997; 40:806–810. [DOI] [PubMed] [Google Scholar]
- 3.Bokey EL, Chapuis PH, Fung C, et al. Postoperative morbidity and mortality following resection of the colon and rectum cancer. Dis Colon Rectum 1995; 38:480–487. [DOI] [PubMed] [Google Scholar]
- 4.Rutledge R. An Analysis of 25 Milliman and Robertson guidelines of surgery. Ann Surg 1998; 228:579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marcario A, Vitez TS, Dunn B, et al. Hospital costs and severity of illness in three types of elective surgery. Anesthesiology 1997; 86:92–100. [DOI] [PubMed] [Google Scholar]
- 6.Chen HH, Wexner SD, Weiss EG, et al. Laparoscopic colectomy for benign colorectal disease is associated with a significant reduction in disability as compared with laparotomy. Surg Endosc 1998; 12:1397–1400. [DOI] [PubMed] [Google Scholar]
- 7.Möiniche S, Bülow S, Hesselfeldt P, et al. Convalescence and hospital stay with balanced analgesia, early oral feeding and enforced mobilisation. Eur J Surg 1995; 161:283–288. [PubMed] [Google Scholar]
- 8.Liu SS, Carpenter RL, Mackey DC, et al. Effects of perioperative analgesic technique on rate of recovery after colon surgery. Anesthesiology 1995; 83:757–765. [DOI] [PubMed] [Google Scholar]
- 9.Bradshaw BGG, Liu SS, Thirlby RC. Standard perioperative care protocols and reduced length of stay after colon surgery. J Am Coll Surg 1998; 186:501–506. [DOI] [PubMed] [Google Scholar]
- 10.Bokey EL, Morre JWE, Ahapuis PH, et al. Morbidity and mortality following laparoscopic-assisted right hemicolectomy for cancer. Dis Colon Rectum 1996; 39:S24–S28. [DOI] [PubMed] [Google Scholar]
- 11.Milson JW, Böhm B, Hammerhofer KA, et al. A prospective randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 1998; 187:46–57. [DOI] [PubMed] [Google Scholar]
- 12.Bardram L, Funch-Jensen PM, Jensen P, et al. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet 1995; 345:763–764. [DOI] [PubMed] [Google Scholar]
- 13.Kehlet H, Mogensen T. Two-day hospital stay after open sigmoidectomy with a multi-modal rehabilitation program. Br J Surg 1999; 86:227–230. [DOI] [PubMed] [Google Scholar]
- 14.Spivak H, Van de Maele O, Friedman I, Nussbaum M. Colorectal surgery in octogenarians. J Am Coll Surg 1996; 183:46–50. [PubMed] [Google Scholar]
- 15.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997; 78:606–617. [DOI] [PubMed] [Google Scholar]
- 16.Wexner SD. Standardized perioperative care protocols and reduced lengths of stay after colon surgery. J Am Coll Surg 1998; 186:589–593. [DOI] [PubMed] [Google Scholar]
- 17.Kehlet H. Acute pain control and accelerated postoperative surgical recovery. Surg Clin North Am 1999; 79:431–443. [DOI] [PubMed] [Google Scholar]
- 18.Brown TA, McDonald J, Williard W, Washington T. A prospective, randomized, double-blinded placebo-controlled trial of cisapride after colorectal surgery. Am J Surg 1999; 117:399–401. [DOI] [PubMed] [Google Scholar]
- 19.Urbach DR, Kennedy ED, Cohen MM. Colon and rectal anastomoses do not require routine drainage. A systemic review and meta-analysis. Ann Surg 1999; 229:174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]