Abstract
Objective
To determine the negative predictive value of cranial computed tomography (CT) scanning in a prospective series of patients and whether hospital admission for observation is mandatory after a negative diagnostic evaluation after minimal head injury (MHI).
Summary Background Data
Hospital admission for observation is a current standard of practice for patients who have sustained MHI, despite having undergone diagnostic studies that exclude the presence of an intracranial injury. The reasons for this practice are multifactorial and include the perceived false-negative rate of all standard diagnostic tests, the belief that admission will allow prompt diagnosis of occult injuries, and medicolegal considerations about the risk of early discharge.
Methods
In a prospective, multiinstitutional study during a 22-month period at four level I trauma centers, all patients with MHI were evaluated using the following protocol: a standardized physical and neurologic examination in the emergency department, cranial CT scanning, and then admission for observation. MHI was defined as either a documented loss of consciousness or evidence of posttraumatic amnesia and an emergency department Glasgow Coma Scale score of 14 or 15. Outcomes were measured at 20 hours and at discharge and included clinical deterioration, need for craniotomy, and death.
Results
Two thousand one hundred fifty-two consecutive patients fulfilled the study protocol. The CT was interpreted as negative for intracranial injury in 1,788, positive in 217, and equivocal in 119. Five patients with CT scans initially interpreted as negative required intervention. There was one craniotomy in a patient whose CT scan was initially interpreted as negative. This patient had facial fractures that required surgical intervention and elevation of depressed intracranial fracture fragments. The negative predictive power of a cranial CT scan based on the preliminary reading of the CT scan and defined by the subsequent need for neurosurgical intervention in the population fully satisfying the protocol was 99.70%.
Conclusions
Patients with a cranial CT scan, obtained on a helical CT scanner, that shows no intracerebral injury and who do not have other body system injuries or a persistence of any neurologic finding can be safely discharged from the emergency department without a period of either inpatient or outpatient observation. Implementation of this practice could result in a potential decrease of more than 500,000 hospital admissions annually.
Head injury remains one of the most common reasons for seeking medical attention after injury: it is been estimated that more than 1.5 million people are treated for head injuries annually in the United States. 1 The vast majority of head injuries are minor, but the optimal evaluation and treatment protocol of this large group of patients remains controversial. 2–16 Recommendations on the use of cranial computed tomography (CT) scanning vary from mandatory scanning in all patients to more selective use based on a constellation of findings on the history and physical examination. Hospital admission or prolonged supervised observation remains a current standard of practice for patients who have sustained a loss of consciousness (LOC) even though diagnostic studies have excluded an intracranial injury. 3,7,12 The major reason for this practice is the perception that there is an important but undefined false-negative rate in these patients, despite the absence of abnormalities on physical examination, skull radiography, and cranial CT. Case reports on patients who “talked and then deteriorated” have also contributed to this practice. 2,17 It is also believed that even if no significant injury is discovered when a patient is first evaluated, inpatient observation is the best means to identify any missed injury and would allow rapid treatment to be instituted. Finally, medicolegal considerations may cause medical providers to err on the side of caution and admit such patients to the hospital, because there are no prospectively collected data defining the risk of subsequent injury when patients with minimal head injury (MHI) are sent home after a negative evaluation.
The purpose of this study was to evaluate prospectively the incidence of intracranial injury in patients who sustained MHI and the practice of mandatory hospital admission or supervised observation of patients after MHI, particularly when a CT scan was interpreted as negative for intracranial injury.
METHODS
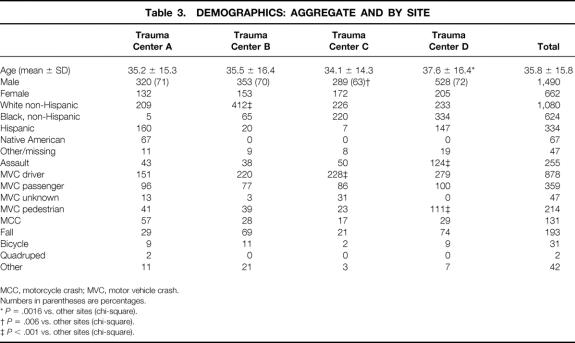
All patients 16 years and older with suspected blunt head trauma admitted to four level I trauma centers (University Hospital, Newark, NJ; MetroHealth Medical Center, Cleveland, OH; Presley Regional Trauma Center, Memphis, TN; and University of New Mexico Medical Center, Albuquerque, NM) between November 4, 1995, and September 1, 1996, were prospectively screened for study eligibility (Table 1). A patient with MHI was defined as one who came to the emergency department (ED) with a Glasgow Coma Scale (GCS) score of 14 or 15 and had sustained an LOC or posttraumatic amnesia.
Table 1. REASONS PATIENTS WERE SCREENED BUT WERE NOT ELIGIBLE
CT, computed tomography; GCS, Glasgow Coma Scale score; LOC, loss of consciousness.
All patients underwent a standardized neurologic examination, created by the investigators and taught to all participants, that included level of consciousness, orientation, pupillary findings, and the presence of focal neurologic deficits. The timing of all neurologic examinations, the level of experience of the examiner, and the diagnostic tests performed after admission were recorded.
Eligible patients underwent a noncontrast cranial CT scan using a helical CT scanner following a standardized protocol. The results were considered preliminary if the CT scan was interpreted by a radiology resident or trauma surgeon. The typed radiology report, as signed off by an attending radiologist, was considered the final reading. Any changes in the CT interpretation between the preliminary and final readings were noted.
A CT scan was considered positive only if an intracranial injury was demonstrated. The presence of any extracranial injury was noted, but a CT scan demonstrating only an extracranial injury was considered negative. Studies were considered equivocal when they could neither exclude nor determine the presence of an intracranial injury. Patients who had equivocal CT examinations were analyzed with respect to the subsequent therapeutic decisions of the supervising physicians. The need for intervention in a patient with a positive cranial CT was determined by the treating neurosurgeons.
After the CT study, patients were admitted and observed for any deterioration in their neurologic examination and the treatment of any other injuries. The standardized neurologic examination was repeated 4 to 8 hours after arrival to the ED. Patients were also assessed 20 hours after admission and at discharge for the major study outcomes: neurologic deterioration, neurosurgical intervention, and death. Deterioration was defined as a decrease of two or more points on the GCS, the development of a focal neurologic abnormality, a loss of orientation to person or place, the need to move the patient to an intensive care unit (ICU) because of the head injury, and the need for any neurosurgical intervention. Neurosurgical intervention was defined as the need for endotracheal intubation and mechanical ventilation, the use of anticonvulsants in patients without a history of seizures, the use of medications to treat cerebral edema, the need for intracranial pressure monitoring, or the need for a craniotomy.
Data were collected prospectively by experienced study coordinators using a manual to ensure uniform coding and were entered into a customized database (Paradox 4.5; Borland International, Scotts Valley, CA). All records were reviewed by one of the authors (R.L.) for completeness, accuracy, and consistency. Queries were sent to the coordinators to request missing data or to clarify apparently invalid or inconsistent data. Only when records were 100% complete were they incorporated into the database.
Sample Size
Calculation of the sample size needed to achieve the projected end points was based on the following assumptions. Because the goal of this study was to define the components of a diagnostic evaluation with sufficiently high negative predictive value (NPV) that patients could be safely discharged from the ED after a concussion, we believed that physicians would be willing to change clinical practice only if the NPV was convincingly greater than 99%. Second, we estimated that the actual NPV of an intracranial injury workup would be 99.6% or more. 8,13,15 Third, from previous reports, we assumed that approximately 15% of patients with MHI would have a positive CT scan and 85% would not. Therefore, we calculated that enrollment of 2,100 subjects would result in a total of 1,700 patients free of intracranial injury. Using these assumptions, a diagnostic evaluation with an NPV of 99.6% should result in 10 or fewer false-negative results out of 1,700 apparently negative patients 91.5% of the time. The 95% lower confidence bound on the NPV would be 0.990%. Thus, 91.5% of the time we would be able to report with 95% confidence that the NPV of the workup exceeds 99%.
Data Analysis
Descriptive analyses were performed initially to provide summaries of demographic information and baseline clinical status for both aggregate and site-specific data to determine whether there were any center effects or significant practice pattern variations between the sites. Baseline frequencies of the findings on physical examination and abnormalities on cranial CT studies were computed. Also, the surgical reports and clinical course of all patients who required neurosurgical intervention after a negative cranial CT were reviewed.
The predictive value of negative results for each component of the diagnostic workup separately and in combination was calculated. The NPV was defined by the true-negative results/(true-negative results + false-negative results). Lower 95% and 99% confidence limits were obtained for NPVs using the binomial probability distribution.
This study was reviewed and approved by the institutional review boards at the four participating institutions.
RESULTS
Six thousand four hundred nine consecutive patients with blunt injury were screened by the four trauma centers during the 22 months of the study, of whom 4,568 had signs of head trauma. One thousand nine hundred ninety-nine were excluded by protocol (see Table 1). Only 31 patients were excluded in error; the remaining 2,569 patients were enrolled (98.8% eligibility). Enrollment during the course of the study remained constant, and there were no differences in accrual between any of the four sites.
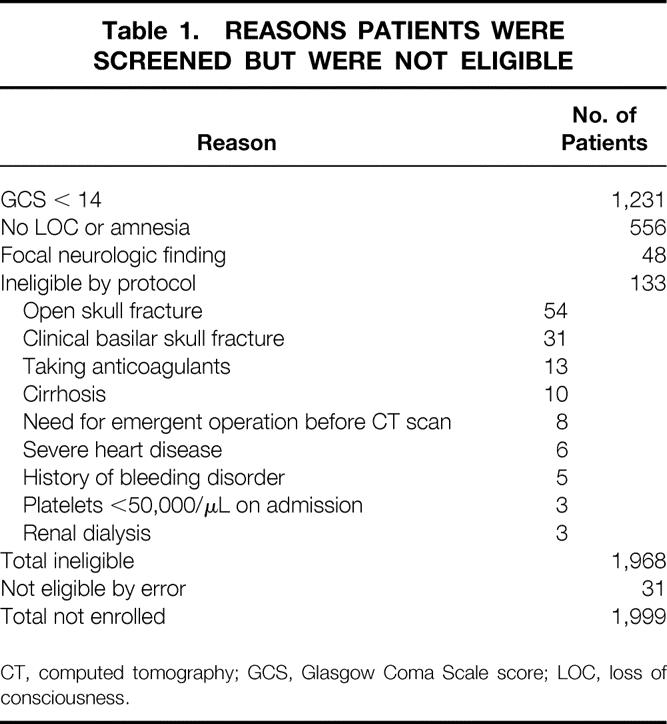
Four hundred seventeen of the 2,569 enrolled patients were subsequently excluded from the analysis. The reasons for exclusion are listed in Table 2. The remaining 2,152 patients who underwent both a physical examination and a cranial CT scan within 12 hours of admission formed the study group. All patients (n = 2,569) who were enrolled before exclusion were followed up for the primary outcome measures and form an intent-to-treat group.
Table 2. REASONS FOR EXCLUSION AFTER ENROLLMENT
CT, computed tomography.
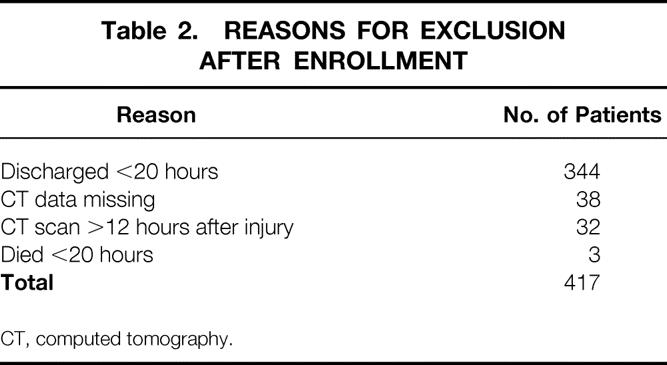
Clinically unimportant differences were found in age, gender, and mechanism of injury between some of the sites (Table 3). The mean Injury Severity Score for the entire population was 10.6 (95% CI 10.4–10.9, median 9). There were no differences in Injury Severity Score between centers. Associated injuries were present in 2,482 (97%) patients and are shown in Table 4.
Table 3. DEMOGRAPHICS: AGGREGATE AND BY SITE
MCC, motorcycle crash; MVC, motor vehicle crash.
Numbers in parentheses are percentages.
*P = .0016 vs. other sites (chi-square).
†P = .006 vs. other sites (chi-square).
‡P < .001 vs. other sites (chi-square).
Table 4. ASSOCIATED INJURIES
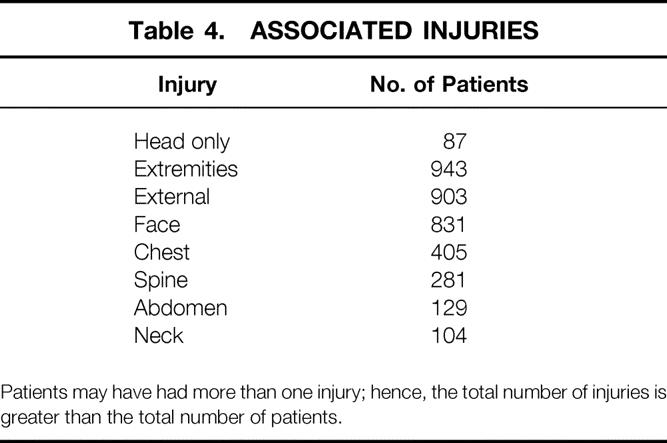
Patients may have had more than one injury; hence, the total number of injuries is greater than the total number of patients.
Eight hundred two patients had a documented LOC and were amnestic to the event. Six hundred fifty-seven did not have a documented or witnessed LOC but were amnestic. The remaining patients had a witnessed LOC but were not recorded as having significant posttraumatic amnesia. A history of posttraumatic seizure was reported in 44 (2%) patients. Six hundred ninety-eight patients had an abnormality on their admission neurologic examination. Only 19% (135/698) of patients with an abnormal finding on their neurologic examination also had an abnormal CT study, whereas 14% (201/1,454) of patients had a positive CT study with no abnormal neurologic findings.
Demographic variables and findings on neurologic examination were subjected to contingency analysis and logistic regression. Patients with a GCS of 14, those injured by interpersonal assault, and victims of motor vehicle trauma were more likely to have a positive CT study. Nonetheless, no variable alone or in combination could reliably discriminate between patients who would have a negative or positive CT study.
The final interpretation of the cranial CT study was negative in 1,788, positive in 217, and equivocal in 119. Twenty-eight final CT reports could not be located. The agreement matrix between the preliminary and the final readings is shown in Table 5. Both diagnostic interpretations were available for 1,987 (92%) CT studies. There was agreement between all the initial and final interpretations in 1,836 (92%), upgrading in 66 (3%), and downgrading in 85 (4%). There was 97% agreement in the interpretation of a negative CT scan. The kappa statistic for agreement between the preliminary and final reading was 0.79 (95% CI 0.76–0.83). The intracranial injuries for the positive CT scans are listed in Table 6.
Table 5. PRELIMINARY AND FINAL CT SCAN READINGS FOR INTRACRANIAL INJURIES
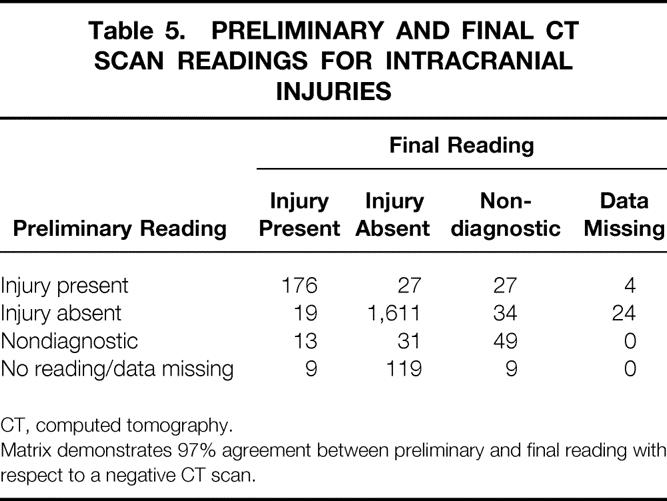
CT, computed tomography.
Matrix demonstrates 97% agreement between preliminary and final reading with respect to a negative CT scan.
Table 6. INTRACRANIAL INJURIES ON CRANIAL CT SCANS
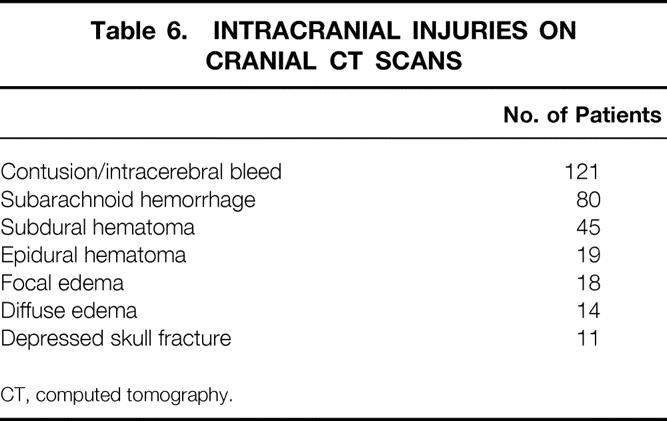
CT, computed tomography.
Thirty-three patients with a negative preliminary CT interpretation had an intervention: ICU admission in 32, endotracheal intubation and mechanical ventilation in 10, anticonvulsant administration in 8, and antiedema medication in 2. Of the eight patients treated with anticonvulsants, six had seizures before admission, one had a seizure after admission, and one was treated for unknown reasons. All patients who underwent endotracheal intubation met the inclusion criteria for the study. None deteriorated under observation, but all had positive findings on their initial neurologic examination, and the treating physicians believed they were too combative to undergo CT scanning safely. Six patients in this group had a seizure before admission, and six had an admitting GCS of 14. All intubations and treatment with anticonvulsant medication occurred in the ED before obtaining the CT scan. The remaining patients either had additional injuries or persistent neurologic findings that required ICU admission for observation. Thus, we believe these interventions were made on clinical grounds and not based on the CT findings. No patient who required intubation needed a craniotomy, and all recovered without neurologic sequelae. The final interpretation of the CT study in only three of the patients in this group was changed to positive.
The interpretation of the CT study in 34 patients was changed from negative to equivocal. In 28 of these, no further action was taken by the treating physicians. Six patients had another CT scan; the results were negative in three and positive in three (small contusions in two and subdural hematoma in one). Two patients had an increase in neurologic monitoring. No patient had neurologic deterioration, and all recovered without sequelae.
Nineteen patients (1.1%; 19/1,664) had their CT interpretations changed from negative to positive. The final readings in this group were contusions in 12, subarachnoid hemorrhage in 3, subdural hematoma in 2, epidural hematoma in 1, and diffuse edema in 1. Two patients deteriorated. One patient with a subarachnoid hemorrhage had a decreased level of consciousness and developed a focal neurologic finding, prompting ICU admission for monitoring and treatment with anticonvulsants. No other intervention was performed. The other patient had a cerebral contusion and was transferred to the ICU and treated with both anticonvulsant and antiedema medications after a seizure. Both recovered without further intervention. Only one patient with a negative CT scan required craniotomy. This patient was the victim of an assault that resulted in displaced facial fractures. During the surgical repair, the patient was noted to have depressed calvarial fracture fragments, requiring craniotomy for elevation. This patient had no neurologic deterioration and was discharged.
Five patients (0.3%; 5/1,664) had missed injuries on the preliminary reading and required neurosurgical intervention based on those injuries. The five interventions were listed above and comprised two patients who had an increase in neurologic monitoring, two patients who underwent ICU admission and treatment with anticonvulsants or antiedema medications, and the one patient who underwent a craniotomy. All recovered without sequelae. The NPV of the cranial CT scan based on the preliminary interpretation was 99.70% (lower 95% and 99% confidence bounds of 99.38% and 99.23%, respectively), as defined by the ultimate presence of an injury in patients who deteriorated and required any intervention in the population fully satisfying the protocol. An analysis using the intent-to-treat group did not alter these results. The NPV defined by the need for a craniotomy was 99.94% (lower 95% and 99% confidence bounds of 99.72% and 99.61%, respectively).
DISCUSSION
Despite more than two decades of debate and study, the optimal evaluation of patients with MHI remains controversial. 2–16 The data presented here clearly indicate that a cranial CT scan is necessary for patients who sustained either an LOC or posttraumatic amnesia, because no constellation of variables can predict which patients will have a positive CT study. Further, patients with a cranial CT scan, obtained on a helical CT scanner, that shows no intracerebral injury and who do not have other body system injuries or a persistence of any neurologic finding can safely be discharged from the ED, thus reducing the need for hospital admission in this large group of patients.
Varying definitions and terms have hampered the assessment of the data on MHI. This study defined MHI to include only patients with an admission GCS score of 14 or 15 and a history of a reported LOC or posttraumatic amnesia (or both). First, we wished to evaluate patients who could be potentially discharged from the ED with respect to their head injury. Hence, we specifically excluded patients with lower GCS scores, because the incidence of an intracranial injury in this group has been reported to exceed 30%. 2,4,13–15 We have also chosen to call these injuries MHI instead of concussions. The American Academy of Neurology recently separated concussions into three grades, with grades 1 and 2 being defined as transient confusion and/or disorientation without an LOC 18; only grade 3 concussions are associated with an LOC. Thus, per that definition, this study was restricted to only grade 3 concussions. The term MHI has been associated with scalp lacerations and other head injuries without an LOC. 19 We believe the use of the term MHI conveys that these patients have a real incidence of neurologic injury and a small but defined need for neurosurgical intervention.
The 13% positive rate for cranial CT scans in this population is within the range of previous investigations. 2,4,5,7,8,12–15,20 Most importantly, we were unable to predict from history and neurologic examination which patients would have a positive CT. This is similar to the data in other studies 7,12 and confirms the fact that patients with MHI must undergo mandatory CT scanning. Although both a documented LOC and posttraumatic amnesia were associated with an increased incidence of a positive scan, 10% of patients with either finding alone had a positive CT study. A similar pattern was observed in the incidence of a positive CT study in patients with or without abnormalities on their neurologic examination. Our data do not support attempts to limit the use of cranial CT scan only for patients with a constellation of certain findings, and this practice would most likely increase the death and complication rates from undiagnosed intracranial injuries. 21 Further, because patients without other significant body system injuries or a persistently abnormal mental status and a normal CT scan can be promptly discharged from the ED, we believe the use of CT in this population would reduce unnecessary hospital admissions.
The range of recommendations about the management of patients with MHI and the variability in the frequency of positive CT findings are confusing. In patients with a GCS of 15 and a history of an LOC or amnesia, the reported incidence of a positive CT scan is 3% to 19% and the need for neurosurgical intervention is 0.08% to 3.3%. 2,4,5,7,8,10,12,13,15,20,22 This wide range of results is likely due to undetected differences and biases between these series in the types of patients studied, the selection criteria for inclusion, and the intent of the study. This variability also may be accounted for in the definition of MHI as outlined above, the physician’s threshold for obtaining a CT scan, and whether the study was retrospective or prospective. Although a positive LOC is an undisputed indication for obtaining a cranial CT scan, the definition of posttraumatic amnesia in the absence of a documented LOC is more subjective. Stiell et al, 23 in a study of cranial CT use in MHI, found extreme variability in CT ordering and positive CT rates between Canadian institutions and even between attending ED physicians in a given institution.
Some have suggested that improvements in resource utilization could be accomplished by admitting all patients with MHI and using cranial CT scanning more selectively. The problems inherent in the selective use of CT scanning are outlined above. Hospital admission also assumes that patients will be observed properly in the hospital; that observation will uncover a reasonable percentage of occult injuries not found on diagnostic testing amenable to prompt intervention, thereby reducing complications and death; and that the incidence and consequences of adverse events from hospital admission are less than those of a missed injury. Livingston et al, 8 in a study of observation for MHI, noted that only 50% of patients admitted to non-ICU beds had documented neurologic observation. In a retrospective multicenter review of MHI, documented observation was missing in more than one third of patients. 13 With continual reinforcement as part of the study protocol, we were able to increase the frequency of a second neurologic examination to 87%. This percentage accurately reflects clinical practice in busy trauma centers and raises further doubts about the value of hospital admission for observation. Klauber et al 21 found that patients with minimal rather than severe brain injury had an increased risk of dying from the injury. They postulated that this was due to a delay in diagnosis among patients who were initially thought not to have an injury, based on the absence of abnormal neurologic findings.
At the outset of this study, we hypothesized that to alter the practice of hospital admission for observation after MHI, we would have to demonstrate that early emergent CT is necessary in this patient population and that the NPV was sufficiently high to allow prompt discharge from the ED. Overall, the false-negative rate was 0.3%, with only one patient with a negative CT requiring a craniotomy. Thus, the NPV of a cranial CT scan in patients requiring a craniotomy was 99.94%. Because this patient had known complex facial fractures, we believe that present CT scanning is accurate enough to exclude significant intracranial injuries in this patient population. Whether the improvement in the observed accuracy of CT in this study is due to the recent improvements in CT technology or increasing experience with this modality is not known from this study. These data conclusively demonstrate that patients with a cranial CT scan, obtained on a helical CT scanner, that shows no intracerebral injury and who do not have other body system injuries or a persistence of any neurologic finding can be safely discharged from the ED without a period of either inpatient or outpatient observation. Implementation of this practice could result in a potential decrease of more than 500,000 hospital admissions annually.
Footnotes
Correspondence: David H. Livingston, MD, University Hospital E-245, 150 Bergen St., Newark, NJ 07103.
Supported by Agency for Health Care Policy Research grant RO1-HS07336.
E-mail: livingst@umdnj.edu
Accepted for publication October 8, 1999.
References
- 1.Sosin DM, Sniezek JE, Thurman DJ. Incidence of mild and moderate brain injury in the United States, 1991. Brain Inj 1996; 10:47–54. [DOI] [PubMed] [Google Scholar]
- 2.Borczuk P. Predictors of intracranial injury in patients with mild ahead trauma. Ann Emerg Med 1995; 25:731–736. [DOI] [PubMed] [Google Scholar]
- 3.Dacey RGJ, Alves WM, Rimmel RW. Neurosurgical complications after apparently minor head injury. J Neurosurg 1986; 65:203–210. [DOI] [PubMed] [Google Scholar]
- 4.Dunham CM, Coates S, Cooper C. Compelling evidence for discretionary brain computed tomographic imaging in those patients with mild cognitive impairment after blunt trauma. J Trauma 1996; 41:679–686. [DOI] [PubMed] [Google Scholar]
- 5.Feuerman T, Wackym P, Gade G, Becker D. Value of skull radiography, head computed tomographic scanning, and admission for observation in cases of minor head injury. Neurosurgery 1988; 22:449–453. [DOI] [PubMed] [Google Scholar]
- 6.Holmes JF, Baier ME, Derlet RW. Failure of the Miller criteria to predict significant intracranial injury in patients with a Glasgow Coma Scale score of 14 after minor head injury. Acad Emerg Med 1997; 4:788–792. [DOI] [PubMed] [Google Scholar]
- 7.Jeret J, Mandell M, Anziska B, et al. Clinical predictors of abnormality disclosed by computed tomography after mild head injury. Neurosurgery 1993; 32:9–16. [DOI] [PubMed] [Google Scholar]
- 8.Livingston D, Loder P, Koziol J, Hunt C. The use of CT scanning to triage patients requiring admission following minimal head injury. J Trauma 1991; 31:483–489. [PubMed] [Google Scholar]
- 9.Mendelow AD, Campbell, DA, Jeffrey RR, et al. Admission after mild head injury: benefits and costs. Br Med J 1982; 285:1530–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mikhail MG, Levitt A, Christopher TA, Sutton MC. Intracranial injury following minor head injury. Am J Emerg Med 1992; 10:24–28. [DOI] [PubMed] [Google Scholar]
- 11.Moran SG, Mccarthy MC, Uddin DE, Poelstra RJ. Predictors of positive CT scans in the trauma patient with minor head injury. Am Surg 1994; 60:533–536. [PubMed] [Google Scholar]
- 12.Harad F, Kerstein M. Inadequacy of bedside clinical indicators in identifying significant intracranial injury in trauma patients. J Trauma 1992; 32:359–363. [DOI] [PubMed] [Google Scholar]
- 13.Shackford SR, Wald SL, Ross SE, et al. The utility of CT scanning and neurologic examination in the management of patients with minor head injuries. J Trauma 1992; 33:385–394. [DOI] [PubMed] [Google Scholar]
- 14.Snoey ER, Levitt MA. Delayed diagnosis of subdural hematoma following normal computed tomography scan. Ann Emerg Med 1994; 23:1127–1131. [DOI] [PubMed] [Google Scholar]
- 15.Stein S, Ross S. Mild head injury: a plea for routine early CT scanning. J Trauma 1992; 33:11–13. [PubMed] [Google Scholar]
- 16.Taheri PA, Karamanoukian H, Gibbons K, et al. Can patients with minor head injuries be safely discharged home? Arch Surg 1993; 128:289–292. [DOI] [PubMed] [Google Scholar]
- 17.Ratanalert S, Phuenpathom P. Management of head injury patients who talk and deteriorate. Surg Neurol 1990; 34:27–29. [DOI] [PubMed] [Google Scholar]
- 18.Neurology Quality Standards Subcommittee, American Academy of Neurology. Practice parameter: the management of concussion in sports. Neurology 1997; 48:581–585. [DOI] [PubMed] [Google Scholar]
- 19.Masters SJ, McClean PM, Argarese JS, et al. Skull x-ray examinations after head injury: recommendations by a multidisciplinary panel and validation study. N Engl J Med 1987; 316:84–91. [DOI] [PubMed] [Google Scholar]
- 20.Schynoll W, Overton D, Krome R, et al. A prospective study to identify high-yield criteria associated with acute intracranial computed tomography findings in head-injured patients. Am J Emerg Med 1993; 11:321–326. [DOI] [PubMed] [Google Scholar]
- 21.Klauber MR, Marshall LF, Luerssen TG, Frankowski R. Determinants of head injury mortality: importance of the low-risk patient. Neurosurgery 1989; 24:31–36. [DOI] [PubMed] [Google Scholar]
- 22.Miller EC, Derlet RW, Kinser D. Minor head injury: is computed tomography always necessary? Ann Emerg Med 1996; 27:290–294. [DOI] [PubMed] [Google Scholar]
- 23.Stiell IG, Wells GA, Vandemheen K, et al. Variations in ED use of computed tomography for patients with minor head injury. Ann Emerg Med 1997; 30:14–22. [DOI] [PubMed] [Google Scholar]