Abstract
Objective
To review the surgical and clinical results of minimally invasive resection of intrathoracic neurogenic tumors using a video-assisted thoracoscopic technique.
Summary Background Data
Thoracoscopy has emerged as a possible means for diagnosing and managing various intrathoracic disorders. Benign intrathoracic tumors often are ideal lesions for resection using a video-assisted technique. The authors report on their combined experience with the thoracoscopic resection of 143 intrathoracic neurogenic tumors.
Methods
Between March 1992 and February 1999, 143 patients with intrathoracic neurogenic tumors were diagnosed and underwent resection using video-assisted thoracoscopic techniques in three teaching centers. Case selection, surgical technique, and clinical results were reviewed.
Results
The average age of the patients was 40.8 years; 57.3% were male. Thirty-eight patients (27%) had symptoms attributable to the masses. Seventy-two masses were neurofibromas, 33 were neurilemmomas, 7 were paragangliomas, and 31 were ganglioneuromas. All but seven tumors were located in the posterior mediastinum. The masses were on average 3.5 cm in greatest diameter. The mean surgical time was 40 minutes, and the average hospital stay was 4.1 days. There were no major postoperative complications or recurrences to date. Nine patients reported paresthesias over the chest wall during a mean follow-up of 29 months.
Conclusions
Resection of intrathoracic neurogenic tumors using a thoracoscopic technique based on standard surgical indications would seem to be appropriate. Most of these masses are benign and readily removed. For dumbbell tumors, a combined thoracic and neurosurgical approach is mandatory.
Intrathoracic neurogenic tumors are neoplasms that arise from any of the neural elements in the thorax. These tumors are derived from the various neural elements (nerve sheath, ganglion, or neurite) of the peripheral, autonomic, or paraganglionic nervous systems. Nerves and ganglia of both the somatic and autonomic nervous systems are found throughout the thorax but are concentrated in the paravertebral sulcus region, commonly designated as the posterior mediastinum. Intercostal nerve rami and the sympathetic chain found in this region account for 95% of intrathoracic neurogenic tumors. 1 Before the advent of video-thoracoscopy, most nerve sheath and autonomic system tumors were best approached by a standard posterolateral thoracotomy. 2–6 More recently, attempts have been made to resect these tumors thoracoscopically in a minimally invasive manner. 7–9 Given the advantages shown by the efficacy of these techniques and their less invasive nature, we have chosen video-thoracoscopy as the procedure of choice to remove intrathoracic neurogenic tumors in recent years. This report reviews our combined experiences and clinical results.
METHODS
The medical records of 143 patients undergoing surgical removal of intrathoracic neurogenic tumors between March 1992 and February 1999 were reviewed in three medical centers (Prince of Wales Hospital, Hong Kong; First School of Clinical Medicine, Beijing Medical University, Beijing, China; and Chang Gung Memorial Hospital, Taiwan). The average age of the patients was 40.8 years (range 11–72 years), and 82 (57.3%) were male. Tumors that were large (>8 cm in diameter) or obviously malignant were excluded from the video-assisted approach.
Preoperative evaluation included routine chest radiography, electrocardiography, and laboratory evaluation, including complete blood counts and serum chemistries. None of our patients were suspected of having hormonally active tumors; therefore, catecholamine and vanillylmandelic acid levels were not routinely obtained. Computed tomography scans were obtained routinely to image the lesions (Fig. 1A). Patients with suspected intraspinal extension of a tumor underwent magnetic resonance imaging studies and neurosurgical consultation.
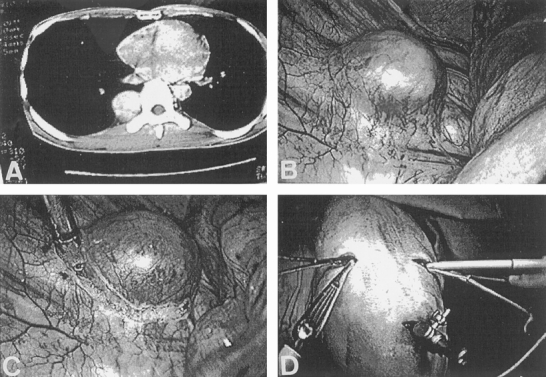
Figure 1. (A) Computed tomography showing right posterior mediastinal mass. (B) Neurogenic tumor was identified thoracoscopically. (C) Parietal pleura overlying the tumor was incised and tumor dissection was carried out along its border. (D) Conventional instruments were used to enucleate the tumor.
All procedures were carried out under general anesthesia with a double-lumen endotracheal tube. Patients were positioned and draped as for a standard posterolateral thoracotomy. We used a 10-mm 0° lens. The camera was introduced into the pleural cavity through a 2-cm incision through the fifth to seventh intercostal space in the midaxillary line. This was done after a digital exploration of the proposed initial trocar site to ensure that free pleural space was present. Depending on the tumor site and the planned procedure, two additional incisions were created to allow the introduction of conventional instruments into the thoracic cavity. We seldom used endoscopic instruments or disposable trocars. 10 It was often necessary for the surgeon to change from one side of the table to the other to target the tumor site. Long conventional instruments such as the sponge-holding forceps were especially useful in manipulating the tumor during dissection.
Once the tumor had been identified (Fig. 1B), the parietal pleura overlying the tumor was incised (Fig. 1C). With careful dissection, the well-circumscribed tumor was easily freed. Usually the dissection was simple and straightforward. The tumor could be enucleated using conventional instruments without significant difficulty (Fig. 1D). Adjacent intercostal and vertebral vessels were ligated with hemoclips or directly cauterized. The tumor was extracted through one of the incisions. Placement of the tumor in a surgical glove was preferred to avoid the use of an expensive disposable specimen bag and to avoid direct wound contamination. If hemostasis was ensured, a chest tube was usually not necessary, and the lung was reinflated under video vision. Wounds were closed while the anesthesiologist maintained positive pleural pressure. For patients with dumbbell tumors, routinely the neurosurgical team was called on to perform a laminectomy for a posterior approach to the spinal cord (a two-stage approach).
RESULTS
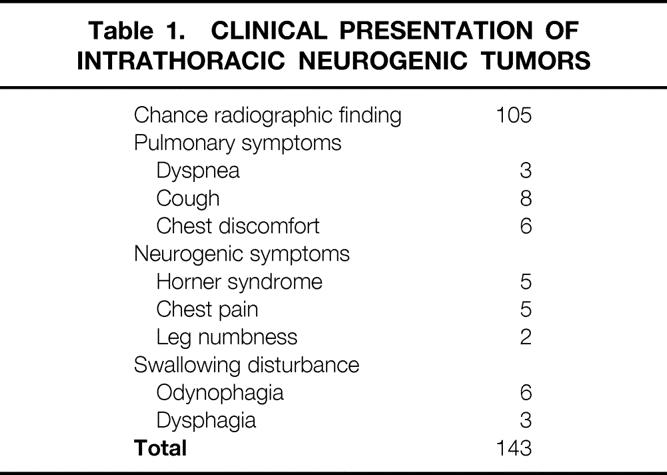
All 143 patients underwent successful thoracoscopic resection of their intrathoracic neurogenic tumors. Fourteen patients had tumors larger than 5 cm, which required wound extension to 6 cm for retrieval of specimens. None of our patients needed conversion to full thoracotomy. Fifty-four tumors were located in the superior mediastinum, 47 lesions in the middle portion of the posterior mediastinum, and 35 lesions in the lower part of the posterior mediastinum. Seven patients had tumors located in a lateral aspect of the chest wall cavity. Fourteen patients underwent magnetic resonance imaging. Esophagography was performed in nine patients who had a swallowing disturbance at the time of diagnosis. Of all the patients, 73% were asymptomatic and their tumors were a chance finding on routine chest radiography. Thirty-eight patients had pressure-related symptoms at the time of diagnosis (Table 1).
Table 1. CLINICAL PRESENTATION OF INTRATHORACIC NEUROGENIC TUMORS
The objective of complete tumor removal was attained in all of our patients; in all patients, the resection involved the division of one or more nerves from which tumors had originated. There were 105 patients (73.3%) with benign nerve sheath tumors, 72 (50.3%) neurofibromas and 33 (23%) neurilemmomas. The remainder included 7 patients with paragangliomas and 31 with nerve cell tumors (ganglioneuromas). Four patients had dumbbell tumors with intraspinal involvement. The diameter of all the tumors excised ranged from 1.5 to 8 cm (average 3.5 cm). The average surgical time for the video-thoracoscopic approach was 40 minutes (range 15–110 minutes). Blood loss was negligible (mean <50 mL). The average hospital stay was 4.1 days (range 1–11 days).
Of the 143 patients whose tumors were thoracoscopically excised, none had in-hospital or postoperative major complications attributable to the surgical technique. Five patients, however, had a nerve sheath tumor excised from the superior mediastinum at the thoracic inlet producing Horner syndrome, which had already occurred before surgery. One of the seven patients with a lateral chest wall neurofibroma developed a loculated empyema that required conservative treatment with local drainage and antibiotics. He remained well without sequelae during follow-up. Nine patients reported paresthesias over the chest wall in the dermatomal distribution of the fifth intercostal nerve 6 months after surgery. At subsequent follow-up, most of these patients were free of symptoms, with only two patients noting wound discomfort related to weather changes.
Four patients with dumbbell tumors were noted to have limited intraspinal involvement. Combined excision of the tumors was carried out with our neurosurgical colleagues. Three of the four patients first underwent neurosurgery and had a neural canal approach, followed by thoracoscopic removal of the intrapleural tumor. In all four, the tumors were completely removed and the patients were discharged uneventfully. No recurrence of the tumors was seen during a mean follow-up of 29 months.
DISCUSSION
Intrathoracic neural tumors are uncommon but account for about 75% of tumors of the posterior mediastinum. A benign tumor arising from Schwann cells is called a neurilemmoma; that arising from the nerve sheath is called a neurofibroma. Ganglioneuromas are tumors of nerve cell origin, most of which arise from the autonomic nervous system. 1 Because of doubt about the diagnosis, the increasing size of the tumor, and the possibility of malignancy, early surgical exploration and resection is a frequently accepted policy. Most patients clearly present little problem if this objective is achieved—the asymptomatic patient, usually a young adult with a typical posterior mediastinal opacity, will have this tumor completely excised and its nature confirmed by a pathologist. 1 Expectant observation of mediastinal masses is rarely justified because both benign and malignant lesions may be asymptomatic. Essentially all isolated mediastinal neurogenic tumors are amenable to primary surgical therapy, with the best therapeutic outcomes following complete surgical excision. 2–6
Most nerve sheath and autonomic system tumors, as well as paragangliomas, arise in the posterior mediastinum and are best approached by a standard posterolateral thoracotomy one or two interspaces above or below the lesion to avoid direct injury to the neoplasm. However, classical standard thoracic surgery has often required large and painful incisions. Video-assisted thoracic surgery minimizes access trauma and is appropriate for diagnosing and resecting masses in all of the mediastinal compartments. The reported benefits of video-thoracoscopy specifically related to its being minimally invasive include fewer postoperative pulmonary complications, a more rapid return of respiratory function, a shorter postoperative hospital stay, decreased hospital cost, less postoperative pain and disability, better cosmesis, and a more rapid return to work. 7–10 It has emerged as a possible method for the diagnosis and management of various mediastinal and spinal disorders. 11–16 Benign mediastinal masses such as neurogenic tumors often represent ideal lesions for resection using this minimally invasive technique. 17–19 Our experiences in resecting intrathoracic neurogenic tumors using video-thoracoscopy have proved to be straightforward and without complications.
The standard indications for surgical resection of intrathoracic neurogenic tumors have been either when symptoms exist or when there is a possibility of malignancy in children or adults. Our policy has always been that all patients with suspected intrathoracic neurogenic masses should have the tumor removed because of doubt about the diagnosis and the possibility of malignancy. It is clear that as a mass enlarges, it will produce a pressure effect on surrounding structures, which may necessitate its excision. In recent years, the introduction of advanced video-thoracoscopic techniques has allowed evaluation of the mediastinum and assessment of the local spread of malignancy. The entire mediastinum can be approached with thoracoscopic techniques. Under video vision, the neurogenic tumor covered by pleura is easily identified. The lung parenchyma is not usually adherent to it. The tumor is usually well encapsulated and can be easily mobilized from the surrounding structures if necessary. Division of the nerve or nerves of origin must be carried out, and division of intercostal vessels may also be required using endoclips under video vision. In most benign neurogenic masses, there is an easily developed plane between the tumor and adjacent tissue that lends itself well to total thoracoscopic excision. Unless the mass is large and suspicious of malignancy, the procedure rarely requires conversion to open thoracotomy. Video-thoracoscopy usually offers the ideal surgical approach for mediastinal tumor excision if combined with the use of conventional lung thoracic instruments. Our experience confirms the preference for using conventional instruments to perform video-thoracoscopy resection in a cost-effective manner. 9–13
Four of our patients with dumbbell tumors required a combined neurosurgical and thoracic approach. All the tumors were completely removed. Serious postoperative complications were not encountered by either our team or the neurosurgical groups. According to Grillo et al, 3 approximately 8% of the posterior mediastinal neurogenic tumors are dumbbell-shaped and are often without cord symptoms. The unexpected intraoperative finding of extension of a tumor through the spinal foramen complicates a thoracic approach. Undue traction on this extension under video-thoracoscopy may lead to spinal cord damage. Hemorrhage at the vertebral foramen may be difficult to control using minimally invasive techniques. There is also a risk that removal of just the intrathoracic portion may be followed by paraplegia or other sequelae of permanent spinal cord injury. In these situations, therefore, it is important to make the diagnosis of intraspinal extension before planning the surgical procedure. Radiography of the thoracic spine and computed tomography of the appropriate region should be done. If there is any suggestion of intervertebral involvement, magnetic resonance imaging or myelography is indicated. Once the diagnosis of a dumbbell tumor has been established, careful planning of a combined neurosurgical and thoracic procedure is required. 3,6 We believe that the thoracic approach using video-thoracoscopy provides better visualization of the pathologic involvement as well as procedures for dealing with the anterior spinal approach. 14–19
Benign neurogenic tumors of the mediastinum are among the most common mediastinal tumors. After complete resection, no additional therapy is required. The incidence of local recurrence of these benign lesions is negligible, regardless of the histologic type. Survival approaches 100% after excision of these lesions. Thus, resection of the tumors based on standard surgical indications would seem to be an ideal setting for the use of video-assisted thoracoscopic techniques. We have demonstrated that these techniques can be performed safely and effectively with a short hospital stay and few complications. For the dumbbell variety of neurogenic tumors with extension into the spinal canal, a combined video-thoracoscopic and neurosurgical approach is mandatory.
Footnotes
Correspondence: Hui-Ping Liu, MD, Division of Thoracic & Cardiovascular Surgery, Chang Gung Memorial Hospital, 199 Tun-Hwa N Rd., Taipei, Taiwan 105.
E-mail: hpliu125@ms21.hinet.net
Accepted for publication January 19, 2000.
References
- 1.Davidson KG, Walbaum PR, McCormack RJM. Intrathoracic neural tumors. Thorax 1978; 33: 359–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blegvad S, Lippert H, Simper LB, Dybdahl H. Mediastinal tumors: a report of 129 cases. Scan J Thorac Cardiovasc Surg 1990; 24: 39–42. [DOI] [PubMed] [Google Scholar]
- 3.Grillo HC, Ojemann RG, Scannell JG, Zervas NT. Combined approach to “dumbbell” intrathoracic and intraspinal neurogenic tumors. Ann Thorac Surg 1983; 36: 402–407. [DOI] [PubMed] [Google Scholar]
- 4.Ricci C, Rendina EA, Venuta F, et al. Diagnostic imaging and surgical treatment of dumbbell tumor of the mediastinum. Ann Thorac Surg 1990; 50: 586–589. [DOI] [PubMed] [Google Scholar]
- 5.Shields TW, Reynolds M. Neurogenic tumors of the thorax. Surg Clin North Am 1988; 68: 645–668. [DOI] [PubMed] [Google Scholar]
- 6.Shields TW. Benign and malignant neurogenic tumors of the mediastinum in adults. In: Shields TW, ed. Mediastinal Surgery. Philadelphia: Lea & Febiger; 1992: 241–253.
- 7.Landreneau RJ, Dowling RD, Ferson PF. Thoracoscopic resection of a posterior mediastinal neurogenic tumor. Chest 1992; 102: 1288–1290. [DOI] [PubMed] [Google Scholar]
- 8.Naunheim K. Video thoracoscopy for masses of the posterior mediastinum. Ann Thorac Surg 1993; 56: 657–658. [DOI] [PubMed] [Google Scholar]
- 9.Yim APC. Minimizing chest wall trauma in video-assisted thoracic surgery. J Thorac Cardiovasc Surg 1995; 109: 1255–1256. [DOI] [PubMed] [Google Scholar]
- 10.Liu HP, Lin PJ, Chang CH, Chang JP. Video-assisted thoracic surgery: manipulation without trocar in 112 consecutive procedures. Chest 1993; 104: 1452–1454. [DOI] [PubMed] [Google Scholar]
- 11.Hang TJ, Hsu RWW, Liu HP, et al. Technique of video-assisted thoracoscopic surgery for the spine: new approach. World J Surg 1997; 21: 358–362. [DOI] [PubMed] [Google Scholar]
- 12.Yim APC, Ko KM, Chau WS, Ma CC, Ho JKS. Video-assisted thoracic anatomical lung resections. The initial Hong Kong experience. Chest 1996; 109: 13–17. [DOI] [PubMed] [Google Scholar]
- 13.Liu HP, Chang CH, Lin PJ, et al. Video-assisted thoracic surgery: the Chang Gung experience. J Thorac Cardiovasc Surg 1994; 108: 834–840. [PubMed] [Google Scholar]
- 14.Dickman CA, Rosenthal D, Karahalios DG, et al. Thoracic vertebrectomy and reconstruction using a microsurgical thoracoscopic approach. Neurosurgery 1996; 38: 270–293. [DOI] [PubMed] [Google Scholar]
- 15.Mack MJ, Regan JJ, Bobechdo WP, Acuff TE. Application of thoracoscopy for diseases of the spine. Ann Thorac Surg 1993; 57: 736–738. [DOI] [PubMed] [Google Scholar]
- 16.McAfee PC, Regan JJ, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery: a prospective multicenter study comprising the first 100 consecutive cases. Spine 1995; 14: 1624–1632. [DOI] [PubMed] [Google Scholar]
- 17.Heltzer JM, Krasna MJ, Aldrich F, McLaughlin JS. Thoracoscopic excision of a posterior mediastinal “dumbbell” tumor using a combined approach. Ann Thorac Surg 1995; 60: 431–433. [DOI] [PubMed] [Google Scholar]
- 18.Bousamra M, Hoasler GB, Patterson GA, Roper CL. A comparative study of thoracoscopic vs. open removal of benign neurogenic mediastinal tumors. Chest 1996; 109: 1461–1465. [DOI] [PubMed] [Google Scholar]
- 19.Strollo DC, Rosado-de-Christerson ML, Jett JR. Tumors of the middle and posterior mediastinum. Chest 1997; 112: 1344–1357. [DOI] [PubMed] [Google Scholar]


