Abstract
Objective
To evaluate the authors’ experience with periduodenal perforations to define a systematic management approach.
Summary Background Data
Traditionally, traumatic and atraumatic duodenal perforations have been managed surgically; however, in the last decade, management has shifted toward a more selective approach. Some authors advocate routine nonsurgical management, but the reported death rate of medical treatment failures is almost 50%. Others advocate mandatory surgical exploration. Those who favor a selective approach have not elaborated distinct management guidelines.
Methods
A retrospective chart review at the authors’ medical center from June 1993 to June 1998 identified 14 instances of periduodenal perforation related to endoscopic retrograde cholangiopancreatography (ERCP), a rate of 1.0%. Charts were reviewed for the following parameters: ERCP findings, clinical presentation of perforation, diagnostic methods, time to diagnosis, radiographic extent and location of duodenal leak, methods of management, surgical procedures, complications, length of stay, and outcome.
Results
Fourteen patients had a periduodenal perforation. Eight patients were initially managed conservatively. Five of the eight patients recovered without incident. Three patients failed nonsurgical management and required extensive procedures with long hospital stays and one death. Six patients were managed initially by surgery, with one death. Each injury was evaluated for location and radiographic extent of leak and classified into types I through IV.
Conclusions
Clinical and radiographic features of ERCP-related periduodenal perforations can be used to stratify patients into surgical or nonsurgical cohorts. A selective management scheme is proposed based on the features of each type.
Endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy is commonly used in the treatment of common bile duct stones. It is widely regarded as a safe procedure, but the major complication rate approaches 10%. Common complications include pancreatitis, bleeding, cholangitis, and perforation. Overall, the procedure carries a death rate of 1.0% to 1.5%. 1,2
ERCP-related perforations occur in about 1% of patients, and the injury carries a death rate of 16% to 18%. 1,3 Traditionally, traumatic and atraumatic duodenal perforations have been managed surgically 4; however, in the past decade, management of limited and contained esophageal, 5 colonic, 6 and even duodenal perforations 7 has evolved toward a more selective approach.
Arguments have been made for both surgical 8–10 and nonsurgical management 3,11 of ERCP-related duodenal perforations, but consensus is lacking. In this study, we report the largest published series from a single center and define a management strategy for ERCP-related perforations based on clinical and radiographic features at presentation, anatomical details of the perforation, and treatment outcomes.
METHODS
Between June 1993 and June 1998, 1,413 ERCP procedures with and without sphincterotomy were performed at the Los Angeles County/University of Southern California Medical Center. Fourteen patients (1%) had duodenal perforations during ERCP. The median age of these patients was 48.5 years. There were 10 women and 4 men. The indications for ERCP in these patients were choledocholithiasis before cholecystectomy (n = 10), cholangitis with associated choledocholithiasis (n = 2), retained stone after laparoscopic cholecystectomy (n = 1) and cholecystoenteric fistula (n = 1).
Data were collected retrospectively on 14 patients with documented duodenal perforations during ERCP. Charts were reviewed for the following information: ERCP findings, clinical presentation of perforation, diagnostic methods, time to diagnosis and surgery, radiographic location and extent of duodenal leak, methods of management, surgical procedures, complications, length of stay, and outcomes. Generally, patients were managed medically in the presence of the following parameters: benign abdominal examination, absence of sepsis, minimal leak demonstrated on a follow-up upper gastrointestinal study (UGI), and absence of retroperitoneal fluid collections. Patients were managed surgically if any of the following was present: extensive contrast extravasation on ERCP/UGI, extra- or intraperitoneal fluid collection on computed tomography, retained hardware, documented perforation with retained stones, or massive subcutaneous emphysema. Fever and leukocytosis alone were not considered justification for surgery.
RESULTS
All Patients
ERCP Findings
Cannulation of the ampulla was considered difficult by the endoscopist in 10 of 14 patients. Three cannulations were considered easy, and one procedure was terminated before cannulation. Three patients (21%) erroneously thought to have duodenal diverticula were later discovered to have large perforations. In 6 of the 14 patients, the sphincterotome was the presumed source of injury (all 6 underwent sphincterotomy); in the remaining 8 patients, the mechanism of injury was presumably related to the endoscope (n = 5; 1 of 5 underwent sphincterotomy) or guidewire (n = 3; 2 of 3 underwent sphincterotomy). These conclusions were reached through extensive discussions with both the endoscopist and the operating surgeon in each case.
Diagnosis of Perforation
In 11 of 14 cases (78%), the diagnosis was either made or suspected during ERCP. Demonstration of a perforation during ERCP was accomplished by a limited contrast study through the endoscope. In the remaining patients, the diagnosis was established by chest radiography demonstrating free air under the diaphragm, massive subcutaneous emphysema with a tension pneumothorax during ERCP, and clinical sepsis, which occurred 72 hours after ERCP.
When perforation was suspected but not proven at ERCP, a formal gastrograffin UGI was performed. Four patients (28%) underwent UGI; two had extensive contrast extravasation and two had none.
Clinical Presentation
The clinical presentation of ERCP perforation was variable but frequently mild. Ten patients (71%) had mild abdominal tenderness. Four patients (29%) developed generalized peritonitis between 2 and 72 hours (median 6 hours) after ERCP perforation. Four patients (29%) had temperatures greater than 101°F, four had low-grade fevers, and six remained afebrile.
Four patients did not have white blood cell determinations because of early surgical intervention, but leukocytosis was present in 9 of 10 patients in whom white blood cell counts were performed. Only one HIV-positive patient failed to mount a white blood cell response to ERCP perforation.
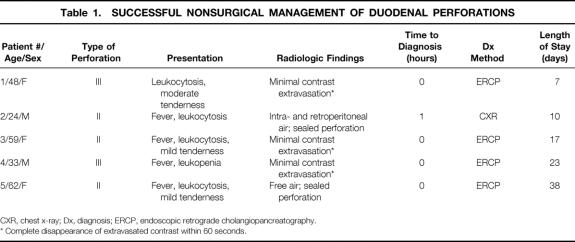
Nonsurgical Management
Of the eight patients who were initially managed without surgery, seven were managed intentionally; one was unintentional and due to a delay in diagnosis. Five of the eight were successfully managed with antibiotics and observation (Table 1) . Their clinical course was characterized by minimal abdominal tenderness, absence of sepsis, a small leak at ERCP with contrast dissipating rapidly on follow-up plain film, no leak demonstrated on follow-up UGI within 4 hours of the injury, and absence of fluid collections on computed tomography. The median length of stay for this group was 17 days (range 7–38).
Table 1. SUCCESSFUL NONSURGICAL MANAGEMENT OF DUODENAL PERFORATIONS
CXR, chest x-ray; Dx, diagnosis; ERCP, endoscopic retrograde cholangiopancreatography.
* Complete disappearance of extravasated contrast within 60 seconds.
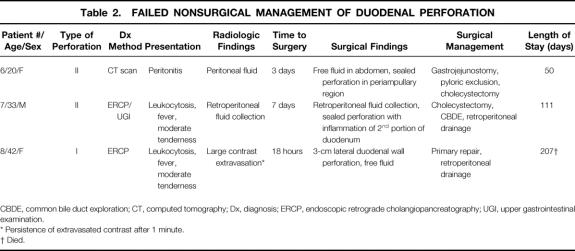
Three patients (Table 2) failed to respond to nonsurgical management. Patients 7 and 8 required salvage operations. Both had initially had minimal abdominal tenderness but progressed to septic peritonitis. Patient 6 had a delay in diagnosis and was managed nonsurgically until she was diagnosed with septic peritonitis after 3 days. At surgery, she had a sealed perforation with a large retroperitoneal abscess. One of three patients died. The median length of stay for the three nonsurgical treatment failures was 111 days.
Table 2. FAILED NONSURGICAL MANAGEMENT OF DUODENAL PERFORATION
CBDE, common bile duct exploration; CT, computed tomography; Dx, diagnosis; ERCP, endoscopic retrograde cholangiopancreatography; UGI, upper gastrointestinal examination.
* Persistence of extravasated contrast after 1 minute.
† Died.
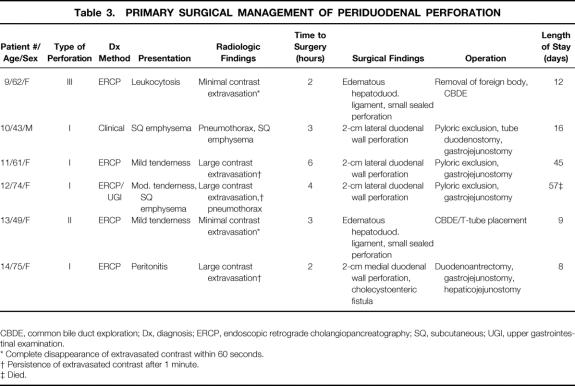
Surgical Management
Indications for surgery in this group of patients included any of the following findings: large contrast extravasation on ERCP/UGI, contrast-enhanced computed tomography scans showing intra- or retroperitoneal fluid collection, massive subcutaneous emphysema, or suspected perforation in association with retained material (i.e., stones, ERCP basket/wire). The time interval to surgery was less than 4 hours in all six patients (Table 3).
Table 3. PRIMARY SURGICAL MANAGEMENT OF PERIDUODENAL PERFORATION
CBDE, common bile duct exploration; Dx, diagnosis; ERCP, endoscopic retrograde cholangiopancreatography; SQ, subcutaneous; UGI, upper gastrointestinal examination.
* Complete disappearance of extravasated contrast within 60 seconds.
† Persistence of extravasated contrast after 1 minute.
‡ Died.
The development (within 18 hours to 7 days) of septic peritonitis with large intraabdominal or retroperitoneal fluid collections led to a delayed surgical procedure in the three patients in whom conservative management failed.
Surgical Findings
In the patients treated primarily by surgery, four patients had 1- to 2-cm duodenal wall perforations (three lateral, one medial) that appeared to be caused by the endoscope. Two of these four patients were erroneously thought to have duodenal diverticula at the time of ERCP. The patient with the medial wall perforation was also found to have a cholecystoenteric fistula. Four patients had large duodenal leaks with retroperitoneal or intraabdominal fluid collections.
Patients 9 and 13 had edema and contrast within the hepatoduodenal ligament but no free or retroperitoneal fluid collections. These two patients would have been managed nonsurgically except for the presence of a retained stone basket in one patient and retained stones in the other.
Three patients underwent delayed surgical treatment. One patient had a large duodenal perforation on the lateral aspect of the duodenum with a large amount of fluid in the retroperitoneum and abdomen. The injury appeared to be caused by the endoscope. This patient was also thought to have a duodenal diverticulum at ERCP that was not demonstrated at surgery. The other two patients had large retroperitoneal or intraabdominal fluid collections with sealed leaks.
Surgical Procedures and Outcomes
Surgical procedures included gastrojejunostomy with pyloric exclusion and retroperitoneal drainage (n = 4), CBDE and T-tube placement (n = 3), duodenoantrectomy (n = 1), and primary duodenal repair and drainage (n = 1).
None of the six patients treated by primary surgical management required reoperation for duodenal leakage. Two patients developed a retroperitoneal abscess; it required open drainage in one patient. Five patients recovered with a median length of stay of 14 days, and one patient, a 74-year-old woman, died of sepsis at 57 days.
Three patients underwent delayed surgical treatment and multiple reoperations (mean 3.6 per patient). In two of the three patients, the duodenum healed, but leakage of a duodenal repair from the third led to sepsis and death. The median length of stay for this group with failed nonsurgical management was 111 days, and there was one death in a previously healthy 42-year-old woman.
DISCUSSION
ERCP sphincterotomy is standard therapy for the diagnosis and treatment of pancreaticobiliary pathology. Associated duodenal injuries have historically been managed surgically, but during the past decade management has shifted toward a more selective approach. Although some authors have recommended routine nonsurgical management, 1,3,11 the reported death rate of those failures was almost 50%. 3 Consequently, others advocate mandatory surgical exploration. 8–10 We reviewed our single-center experience with ERCP-related duodenal perforations to identify clinical and radiographic features that would permit safe nonsurgical management and those that would dictate surgical intervention.
The diagnosis of a duodenal perforation is usually made at ERCP by a limited contrast study through the endoscope. Eleven of our fourteen perforations (79%) were suspected at the time of ERCP. A similar frequency has been reported by others. 2,9 If there was doubt about a perforation at ERCP, an immediate contrast UGI was obtained. Free or retroperitoneal air alone were occasionally present and led to confirmatory UGI.
Inflammation, but not necessarily peritonitis, was a common early feature of duodenal perforation. Leukocytosis and fever were often present early but were not useful to distinguish a management approach. Likewise, abdominal examination was not helpful in determining who should undergo surgery within the first few hours. Most patients requiring surgery did eventually experience peritonitis; however, this was often a late finding and as such was related to a poor outcome. Early peritonitis should dictate surgery, but the retroperitoneal nature of the injuries may mask the severity; therefore, negative findings on an abdominal examination should not exclude surgery.
Our experience with duodenal perforations led to the proposal of the classification scheme shown in Figure 1. These four classes of duodenal perforations, in descending order of severity, relate to the mechanism, anatomical location, and severity of the injury and may predict the need for surgery. We found that the mechanism of injury correlated well with the radiologic findings; considered together, these were the best guide for surgery.
Figure 1. Classification of duodenal perforations into types I through IV based on anatomical location and mechanism of injury (type IV not shown).
Lateral or medial wall perforations (type I) are caused by the endoscope, tend to be large and remote from the ampulla, and require immediate surgery (Fig. 2). Type I lesions often cause large, persistent contrast leaks in the retroperitoneal or intraperitoneal space (Fig. 3). Type II or peri-Vaterian injuries varied in severity but usually were more discrete and less likely (43% of patients in our series) to require surgery. Oral contrast UGI or computed tomography can be used for initial confirmation of the leak and for repeat interval evaluation. Type III injuries probably represent distal bile duct injuries related to wire or basket instrumentation near an obstructing entity (e.g., stone) and are often small (Fig. 4). Retroperitoneal air alone (type IV) is probably related to the use of compressed air to maintain patency of a lumen 12; as such, it is not a true perforation and thus does not require surgical intervention.
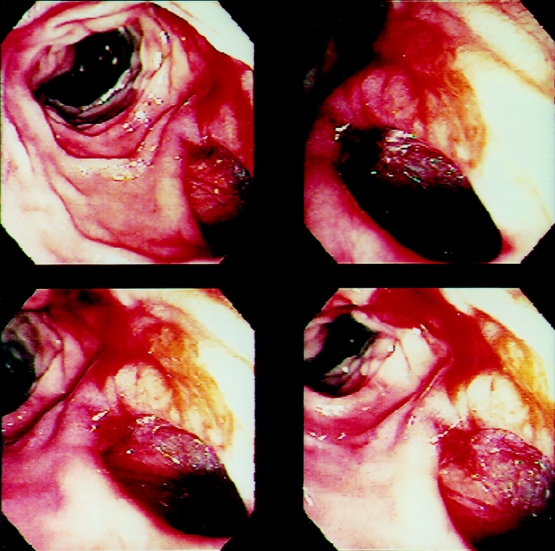
Figure 2. Endoscopic view of a type I duodenal perforation (patient 10).
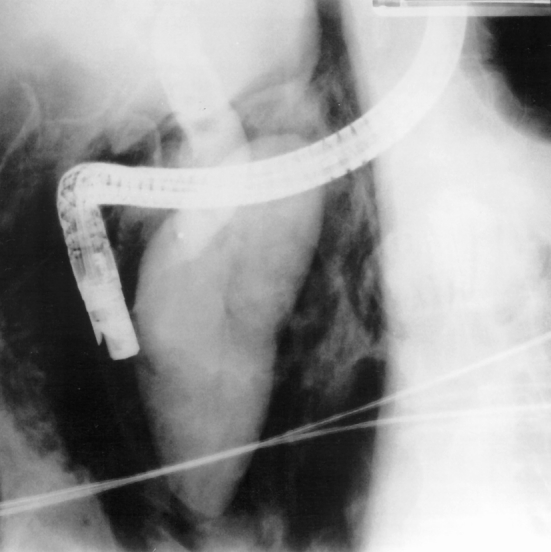
Figure 3. Plain film demonstrating a large leak (type I) after a duodenal perforation related to endoscopic retrograde cholangiopancreatography (patient 11).
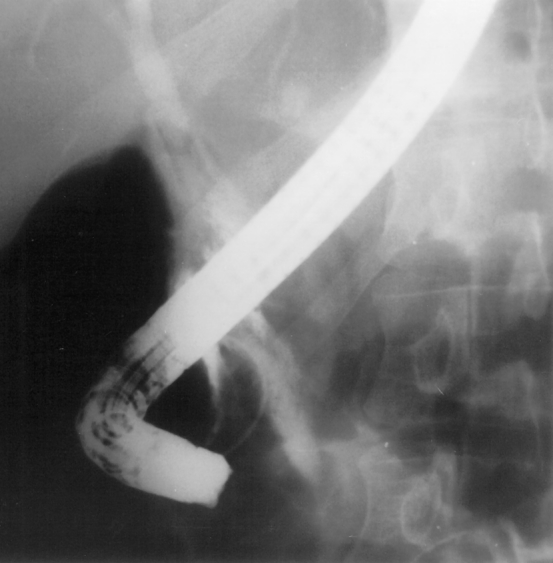
Figure 4. Plain film demonstrating a minimal contrast leak (type III) with papillotomy caused by a wire perforation (patient 4).
Type II and III injuries tend to seal spontaneously and thus lend themselves to nonsurgical management. However, surgical indications may still exist in association with type II and III lesions if large free or retroperitoneal fluid collections exist or if there are retained stones or hardware. Nonsurgical management was successful in five patients with type II or III lesions (62%).
Failed nonsurgical management (three of eight patients [38%]) was associated with high rates of death, complications, and reoperation and a longer hospital stay. During the study, an analysis of our nonsurgical treatment failures led to a revision of our surgical indications (Table 4). Two of these patients had type II injuries and had apparently sealed perforations on UGI or computed tomography, but both had large fluid collections—one intra- and one retroperitoneal (Fig. 5). Extensive retropancreatic drainage, which could not have been accomplished percutaneously, was required in both patients. In addition, two of three patients were diagnosed at ERCP and were immediately started on antibiotics and nasogastric suction, which produced no significant improvement and possibly delayed definitive management.
Table 4. SURGICAL INDICATIONS AFTER ERCP-RELATED DUODENAL PERFORATION
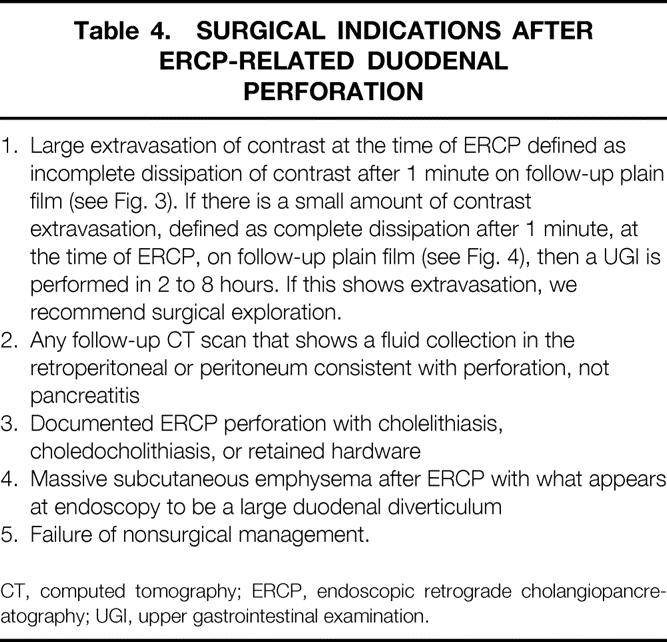
CT, computed tomography; ERCP, endoscopic retrograde cholangiopancreatography; UGI, upper gastrointestinal examination.

Figure 5. Periduodenal fluid collection after a duodenal perforation related to endoscopic retrograde cholangiopancreatography (patient 6).
The magnitude of the surgical procedure was proportionate to the degree of injury. Type I lesions and patients with failed nonsurgical management often required pyloric exclusion, gastrojejunostomy, tube duodenostomy, and extensive drainage or débridement. Reoperation was common in patients with failed conservative management. However, patients with surgical indications for type II and III lesions needed only stone or foreign body removal, biliary diversion, and drainage of the periduodenal spaces.
Based on our experience, we recommend that all patients with type I injuries undergo surgery immediately. Nonsurgical management for type II and III injuries is acceptable if an early contrast study demonstrates minimal extravasation or a sealed perforation without associated fluid collections. Patients with retroperitoneal air alone (type IV) probably need no additional treatment or workup if the findings of the abdominal examination are normal and there is no evidence or suspicion of contrast extravasation at ERCP. Type II, III, or IV injuries with retained stones and unrelieved bile obstruction or foreign bodies should be explored in the absence of other indications. If an initial study demonstrates minimal contrast extravasation and a conservative approach is chosen, a UGI study should be repeated within 8 hours to confirm the initial impression. In addition, a double-contrast computed tomography scan should be performed at 8 hours and at 48 hours to confirm that the leak remains sealed and to exclude the development of fluid collections. These studies should be repeated regularly until clinical recovery appears certain.
The decision to manage patients without surgery is a dynamic one and should undergo frequent reevaluation whenever the clinical circumstances demonstrate even the slightest untoward development.
CONCLUSION
The diagnosis of duodenal perforation is usually made at ERCP. Characteristics on ERCP/UGI may be used to classify injuries into types I, II, III, or IV. Type I injuries are usually large and require immediate surgery. Type II and III injuries with minimal contrast leak and no associated fluid collections may be managed nonsurgically with close surveillance. Type IV injuries are due to the use of compressed air to maintain the patency of a lumen; they are therefore not true perforations and do not require surgical intervention. Patients who have late recognition of a duodenal perforation and nonsurgical treatment failures have a high complication rate, with a potentially fatal outcome.
Footnotes
Correspondence: Rick Selby, MD, Dept. of Surgery, LAC+USC Medical Center, 1200 N. State St., Rm. 9900, Los Angeles, CA 90033.
E-mail: rselby@surgery.usc.edu
Accepted for publication November 11, 1999.
References
- 1.Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endoscopy 1991; 37: 383–393. [DOI] [PubMed] [Google Scholar]
- 2.Dunham F, Bourgeouis N, Gelin M, et al. Retroperitoneal perforations following endoscopic sphincterotomy: clinical course and management. Endoscopy 1982; 14: 92–96. [DOI] [PubMed] [Google Scholar]
- 3.Elder JB. Surgical treatment of duodenal ulcer. Postgrad Med J 1988; 64 (Suppl 1): 54–59. [PubMed] [Google Scholar]
- 4.Cameron J, Kieffer R, Baker R, et al. Selective nonoperative management of contained intrathoracic esophageal disruptions. Ann Thorac Surg 1979; 27: 404–408. [DOI] [PubMed] [Google Scholar]
- 5.Cobb L, Vinnocur C, Wagner C, Weintraub W. Intestinal perforation due to blunt trauma in children in an era of increased nonoperative treatment. J Trauma 1986; 26: 461–463. [DOI] [PubMed] [Google Scholar]
- 6.Berne T, Donovan A. Nonoperative treatment of perforated duodenal ulcer. Arch Surg 1989; 124: 830–832. [DOI] [PubMed] [Google Scholar]
- 7.Booth FV McL, Doerr RJ, Khalafi RS, et al. Surgical management of complications of endoscopic sphincterotomy with precut papillotomy. Am J Surg 1990; 159: 132–136. [DOI] [PubMed] [Google Scholar]
- 8.Sarr MG, Fishman EK, Milligan FD, Siefelman SS, Cameron JL. Pancreatitis or duodenal perforation after peri-Vaterian therapeutic endoscopic procedures: diagnosis, differentiation, and management. Surgery 1987; 100: 461–466. [PubMed] [Google Scholar]
- 9.Bell RCW, Van Stiegmann G, Goff J, et al. Decision for surgical management of perforation following endoscopic sphincterotomy. Am Surgeon 1991; 57: 237–240. [PubMed] [Google Scholar]
- 10.Martin DF, Tweedle DEF. Retroperitoneal perforation during ERCP and endoscopic sphincterotomy: causes, clinical features and management. Endoscopy 1990; 22: 174–175. [DOI] [PubMed] [Google Scholar]
- 11.Scarlett PY, Falk GL. The management of perforation of the duodenum following endoscopic sphincterotomy: a proposal for selective therapy. Aust NZ J Surg 1994; 64: 843–846. [DOI] [PubMed] [Google Scholar]
- 12.Genzlinger JL, McPhee MS, Helzberg JH, et al. Significance of retroperitoneal air after endoscopic retrograde cholangiopancreatography with sphincterotomy. Am J Gastroenterol 1999; 94: 1267–1270. [DOI] [PubMed] [Google Scholar]