Abstract
Objective
To define the changes in demographics of liver injury during the past 25 years and to document the impact of treatment changes on death rates.
Summary Background Data
No study has presented a long-term review of a large series of hepatic injuries, documenting the effect of treatment changes on outcome. A 25-year review from a concurrently collected database of liver injuries documented changes in treatment and outcome.
Methods
A database of hepatic injuries from 1975 to 1999 was studied for changes in demographics, treatment patterns, and outcome. Factors potentially responsible for outcome differences were examined.
Results
A total of 1,842 liver injuries were treated. Blunt injuries have dramatically increased; the proportion of major injuries is approximately 16% annually. Nonsurgical therapy is now used in more than 80% of blunt injuries. The death rates from both blunt and penetrating trauma have improved significantly through each successive decade of the study. The improved death rates are due to decreased death from hemorrhage. Factors responsible include fewer major venous injuries requiring surgery, improved outcome with vein injuries, better results with packing, and effective arterial hemorrhage control with arteriographic embolization.
Conclusions
The treatment and outcome of liver injuries have changed dramatically in 25 years. Multiple modes of therapy are available for hemorrhage control, which has improved outcome.
The management of liver injuries has changed dramatically during the past three decades, particularly for blunt trauma. Although most reports have shown dramatic treatment changes for liver injuries during the past decade, often associated with improved survival rates, few if any studies have presented a long-term consecutive patient series examining the impact of treatment changes on outcome. We studied a database of consecutive hepatic injuries treated from 1975 to June 1999. Factors examined included demographic changes, treatment patterns, alterations in death rates, and possible mechanisms for outcome changes.
METHODS
In 1976, two authors (JDR and LMF) developed a database of liver injuries beginning in 1975 and including all liver injuries treated through June 1999. The cases were collected concurrently and entered into the database at least quarterly. Information collected included demographic data, mechanism of injury, grade of hepatic injury, 1,2 associated injuries, treatment of liver injuries, and outcome. Hepatic-related deaths, categorized as deaths directly related to the liver injury, were determined. Some treatment comparisons used annual data; others examined results during three 5-year periods (1975–1979, 1985–1989, and 1995 to June 1999).
RESULTS
The University of Louisville Trauma Unit treated 1,842 liver injuries from January 1975 through June 1999. The annual distribution of injuries treated is shown in Figure 1, including those resulting from blunt and penetrating mechanisms. The total number of injuries increased over time, with a steady rise in the number of patients treated, particularly in the last 12 years of the study. The number of patients with penetrating injuries remained relatively stable during the 25-year period. In the initial 5 years of the review, the percentage of patients with blunt injuries was 48%. The increase in total liver injuries treated occurred primarily as a result of an increase in blunt injuries. From 1985 to 1989, the percentage of blunt injuries increased to 61%; for a corresponding 5-year period in the late 1990s, the figure was 74%.
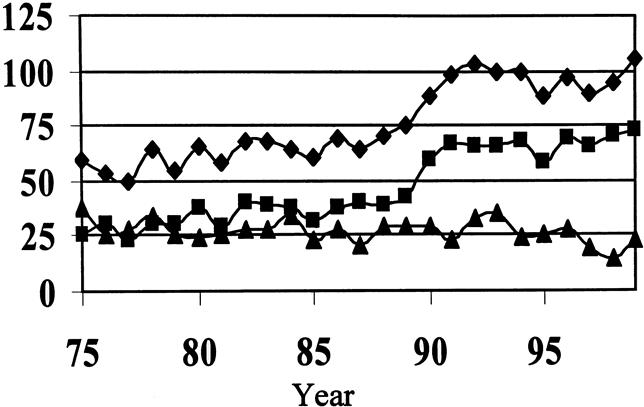
Figure 1. Annual distribution of hepatic injuries by mechanism: ♦, total; ▪, blunt injuries; ▴, penetrating injuries). The increase in the total number of liver injuries treated in the last 12 years was due to an increase in blunt injuries.
The gender distribution for patients with penetrating injuries did not change significantly during the study period: fewer than 5% of those injured were women. There was a steady rise in women with blunt injuries in successive 5-year intervals, from 20% in 1975 to 1979 to 31% and 46% in 1985 to 1989 and 1995 to 1999, respectively.
The occurrence of major hepatic injuries was relatively stable during the study period, ranging from 15% to 12% (Fig. 2), with a mean of 16.8% of the total group having an injury grade of IV or greater. As the number of injuries increased, the percentage of severe injuries increased concomitantly.
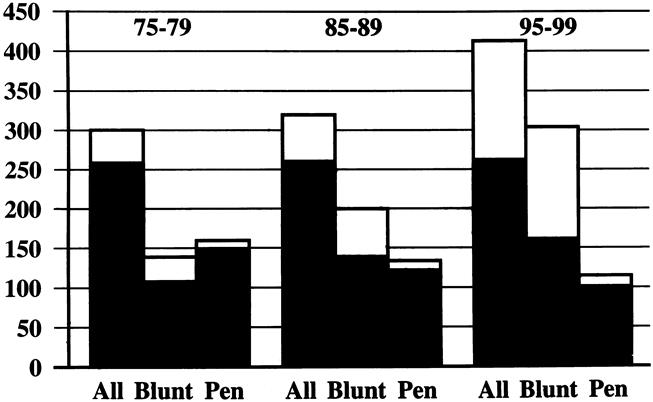
Figure 2. The total number of injuries (♦) per year increased during the past 12-year period. The percentage of severe (grade IV or greater) injuries remained stable (▪).
Treatment of Liver Injuries
The treatment of hepatic trauma changed greatly. The percentages of various forms of surgical treatment used are shown in Table 1 and are divided into the 5-year intervals as described. Selective hepatic artery ligation (SHAL) was used extensively in the early and mid-1970s and still represented 13% of all patients treated in the 5-year period of the late 1970s. In successive decades, SHAL use declined to less than 1% of patients treated.
Table 1. EVOLUTION OF SURGICAL TREATMENT*
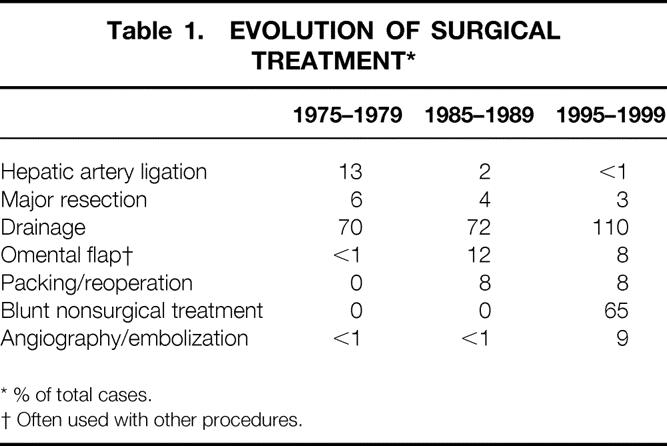
* % of total cases.
† Often used with other procedures.
Major resection was used to control extensive laceration or large segments of devitalized liver tissue in each of the three periods examined, but the percentage declined from 6% to 3%. Drainage as the only treatment used dramatically decreased.
Omental flaps were rarely used before the mid-1980s but were used in approximately 10% of patients treated since then, often in combination with other treatments. Individual vessel suture ligation, minor resectional débridement, tractotomy, hepatic mattress sutures, and other techniques have been used alone or in combination throughout the 25-year interval, but there were no consistent changes in treatment patterns.
In the late 1970s, there were virtually no patients treated by packing and planned reoperation. In the latter two time periods, 8% of patients were treated by packing and planned reoperation as a part of a “damage control” strategy.
Nonsurgical therapy was not used to treat liver injuries with any regularity until the mid-1990s. From 1995 to 1999, two thirds of blunt injury patients were treated without surgery; in the last 2 years, more than 80% did not undergo surgery. Patients with penetrating injuries were still treated surgically. With the advent of nonsurgical therapy, the use of angiography and embolization for hemorrhage control has increased from less than 1% to 9%.
Changes in Death Rates
There was a marked decline in death rates during the 25-year period. Table 2 shows the decrease in both total death rates and death rates ascribed to the liver injury itself. Total death rates declined from 19% to 9%. Liver-related deaths from penetrating injuries declined from 12% to 5%, and death secondary to blunt injury was between 8% and 2% during the 5-year intervals studied.
Table 2. DEATH RATES FROM HEPATIC TRAUMA (TOTAL AND LIVER-RELATED)
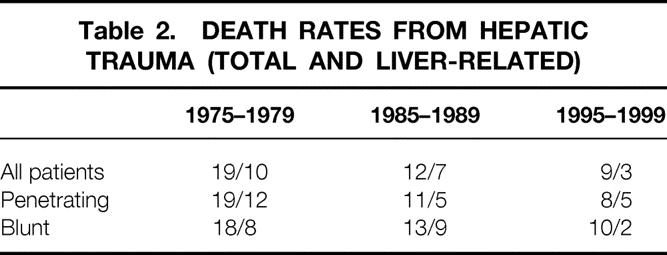
The annual death rates, as percentages, are shown in Figure 3. The steady and dramatic decline in the late 1980s remained in the 3% to 5% range in the past decade.
Figure 3. Both total (▪, left panel) and liver-related (▴, right panel) death rates consistently decreased during the 25-year review (expressed as a percentage of all injuries).
Death unrelated to liver injury showed little change during the 25-year interval. Nonhepatic deaths were related to associated injuries and multiple organ failure. Deaths related to the liver injury itself were due to hemorrhage in more than 85% of patients throughout the study. Improvement in death rates clearly resulted from a decrease in deaths from hemorrhage. Figure 4 demonstrates a consistent decline in the percentage of deaths related to hemorrhage. Four major trends appeared to decrease deaths from hemorrhage: a decrease in major venous injuries requiring surgery, improved management of major venous injuries, improved results with packing and reoperation, and improved arterial bleeding control with arteriography and embolization compared with previous strategies.
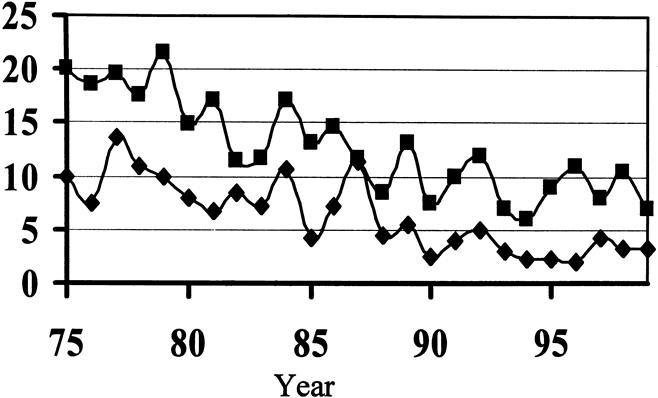
Figure 4. The death rate from hemorrhage consistently declined during the 25-year period (▪, blunt; ♦, penetrating).
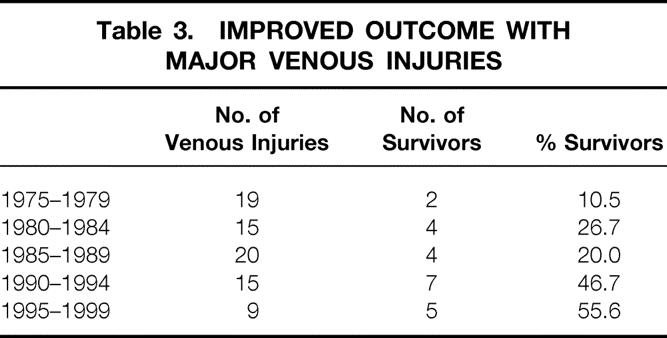
One of the major improvements in death rates is clearly related to improved outcome with major venous injuries (Table 3). Major venous injuries were examined for each 5-year interval from 1975 to 1999. The number of injuries diagnosed and directly treated remained relatively stable for the first 20 years of the review. However, in the last 5 years, the number of patients with major venous injuries declined by 50% over comparable periods. Because the number of total injuries has increased dramatically and the percentage of major liver injuries has remained constant, this suggests that nonsurgical treatment has allowed major venous injuries to be managed without surgery. Five of the nine injured patients treated in the past 5 years have survived. There was a progressive increase in survival rates with each successive 5-year interval.
Table 3. IMPROVED OUTCOME WITH MAJOR VENOUS INJURIES
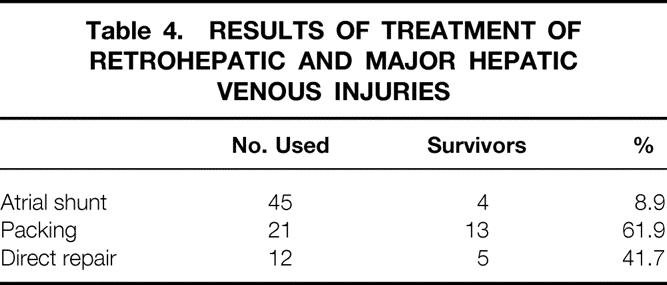
Seventy-eight major juxtahepatic venous injuries were treated involving either the retrohepatic vena cava or the confluence of the major hepatic veins near the cava. Atriocaval shunt was used as the primary mode of therapy in 45 of these patients; only 4 patients survived. The use of atriocaval shunting declined in recent years as packing and direct approaches increased. As opposed to atriocaval shunting, packing combined with direct approaches to the venous injury itself resulted in markedly improved survival rates. Packing led to survival in more than 60% of the patients in which it was used and direct repair in 40%; the shunting survival rate was only 8.9% (Table 4).
Table 4. RESULTS OF TREATMENT OF RETROHEPATIC AND MAJOR HEPATIC VENOUS INJURIES
The death rate associated with packing significantly decreased in the past 5 years compared with reports from two earlier periods from our institution. 3,4 From 1983 to 1989, packing of liver injuries was associated with a 52% death rate. In the succeeding 5-year period, the death rate actually increased to 68% as its use was expanded. From 1995 to 1999, the death rate decreased to 34.5% (P ≤ .05). Analysis of the improved death rates showed that the severity of injuries did not change during the three time periods. The major difference in the latter time period was that packing was performed earlier, with an average blood loss of 6.8 units received before packing, as opposed to 15 units in the earlier series.
The final difference in practice in the last 5 years was in the use of angiography and embolization to control bleeding. Thirty-six patients underwent angiography for hepatic injuries, with bleeding identified in 28 patients. Hemorrhage control was accomplished in 24 of the patients (85%).
DISCUSSION
In the past 25 years, the annual number of injuries increased consistently, probably reflecting the continued increase in total trauma volume. The grade of severe injuries has not changed. The incidence of grades IV and V injuries was 15% to 20% through the years, similar to the 14% reported by Pachter et al. 5 Because the percentage of serious injuries was unchanged, it would be difficult to assert that the improvement in the survival rate was due to a lower severity of injuries.
Treatment patterns changed dramatically during the study. SHAL was developed at the University of Louisville and was used extensively in the early to mid-1970s 6,7; in retrospect, it was overused during this period. Flint and Polk 8 defined its use after several years’ experience, and the incidence of SHAL decreased dramatically since then. SHAL was used in 13% of patients from 1975 to 1979, but that rate then diminished greatly. When arterial bleeding is controlled by a Pringle maneuver, SHAL should still be considered. Cogbill et al 9 reported that SHAL was used in 10 of 210 severe liver injuries, and Asensio et al 10 noted its use in 1 of 22 cases of complex liver trauma in recent series. This rate of usage is consistent with that in our unit.
Major resection is usually necessitated by extensive injuries when devitalized liver is present. Segmentectomy and lobectomy were used in 18 and 12 patients respectively in a series of 210 cases. 9 In 22 patients with grades IV and V injuries, half had nonanatomical resection or lobectomy. 10
Feliciano et al 11 noted that major resection was used in 3.6 of 1,000 cases; this rate was similar to our findings.
The high complication rate associated with liver packing in the middle of the 20th century led to its abandonment. 12 Multiple reports 3,4,13–18 from the mid-1980s outlined the value of packing, and this modality became an important part of the armamentarium in the management of major hepatic injuries. The death rate varied from 40% to 80% in these reports. In our initial report on packing in 1990, the death rate was 53%. 3 We noted that many severe physiologic derangements were present on admission and that early packing was critical if this technique were to have optimal benefit. Earlier use of packing decreased the death rate to roughly one third of the patients treated in the most recent 5-year period.
Multiple reports 19–24 have outlined the efficacy of nonsurgical treatment and its relative safety in hemodynamically stable patients. The Memphis group 25 recently reported that 85% of their blunt trauma patients had nonsurgical treatment, and they have referred to the recent emergence of nonsurgical therapy as the treatment of choice for blunt trauma as a “paradigm shift.” Our data and those of others validate that assertion. Although the initial attraction to nonsurgical treatment is the avoidance of surgery, our data suggest that nonsurgical treatment may contribute to a decrease in death. Despite an increased volume of liver injuries treated and a fairly constant rate of major injuries encountered each year, the number of major venous injuries requiring surgery declined by 50% in the past 5 years compared with previous time periods. Also, the survival rate of these patients with major venous injuries has improved. Through the years, many experienced trauma surgeons anecdotally related accounts of stable patients operated on in whom little bleeding was initially encountered; however, manipulation of venous injuries resulted in massive hemorrhage that resulted in the patient’s death. Because venous injuries occur in low-pressure systems, we contend that many venous injuries heal without the need for surgery. Several retrohepatic caval injuries were encountered that initially had little bleeding but in which massive hemorrhage developed with manipulation. Avoidance of surgery may actually benefit this patient group as well. Thus, we believe that nonsurgical treatment not only avoids surgery but may actually have a positive impact on survival.
The use of nonsurgical treatment has created problems that had not been encountered before. 10,26 Angiography, laparoscopy, endoscopic sphincterectomy, and biliary stent placement have played an important role in this group of patients, as we have previously reported. 26,27
The most striking observation of our 25-year review was the dramatic decrease in the death rate. The major reason is a reduction in deaths from liver hemorrhage.
Above we noted four factors related to decreased deaths from bleeding. Table 4 shows the results of treating major venous injuries with three types of treatment: atriocaval shunting, packing, and direct repair of the venous injuries. Atriocaval shunting was reported by Shrock et al 28 in 1968 and has remained the mainstay of treatment, at least in the literature. However, the death rate from atriocaval shunting procedures is extraordinarily high, ranging from 80% to 100%. 9,29,30 Although the notion of venous isolation with a shunt is theoretically appealing, there are numerous practical barriers to its widespread success. It is rarely performed, and it requires a sternotomy, with the potential of hypothermia attendant with a second open body cavity. We believe it should not be the primary method of controlling major hepatic venous or caval injuries. Judicious early use of packing has resulted in numerous survivors who we believe would have died with attempted atriocaval shunting.
In 1986, Pachter et al 31 suggested that a direct approach to the hepatic veins might be preferable to atriocaval shunting. They noted that all four patients treated with atriocaval shunting died and that the five patients treated with direct repair using finger fracture survived, with exposure of the injured vein and repair of the injury. This notion has been slow to gain acceptance, but several recent reports have outlined excellent results with direct methods of dealing with hepatic vein or retrohepatic caval injuries without atriocaval shunting. Carrillo et al, 32 from our institution, reported on the use of a direct clamping technique to control major juxtahepatic venous injuries with excellent results, given the devastating nature of this injury. Several other reports have demonstrated improved survival with pending or direct repair of venous injuries. 10,33,34
The term “hepatic injury” is a misnomer, for it implies a homogeneous pattern of trauma to the liver that simply does not exist. Whether blunt or penetrating, bleeding or nonbleeding, hemorrhage from veins or arteries, wounds with deep crevasses or major vein injuries, it is apparent that myriad injury patterns may be encountered. With modern computed tomography, most blunt injuries may be managed without surgery; however, complex liver injuries still require surgery. Numerous surgical and intervention techniques (e.g., angiography and endoscopic retrograde cholangiopancreatography) are required to manage these difficult injuries. 10,26
Discussion
Dr. H. Leon Pachter (New York, New York): This is certainly a landmark paper. The changing patterns in the management of complex hepatic injuries, what has been referred to as a paradigm shift, is certainly not unique in itself but is a phenomenon that is prevalent from coast to coast. The single greatest advance in the management of hepatic trauma in the last decade has been the nonoperative management of blunt hepatic injuries. And this can be done, as Dr. Richardson delineated, and I am not surprised, in 80% of their patients during the last 2 years, with a success rate over 90%.
In the past, these patients would have probably been operated on based on a positive DPL despite the fact that they were hemodynamically stable, only to find injuries, as Dr. Richardson referred to, that were “stirred up” and then bleeding occurred which could subsequently not be controlled.
The prevalence of nonoperative management has really been delineated in the February issue of Journal of the American College of Surgeons in “What’s New in Surgery,” when Mary McCarthy described only the nonoperative management of hepatic injuries, without mention of penetrating injuries whatsoever (J Am Coll Surg 2000; 190:232–243).
The other factors identified and delineated by Dr. Richardson that have played a significant role in decreasing the overall mortality to 3%—which is certainly an enviable number—include: 1) damage control “packing” and planned reexploration (I would stress, as Dr. Richardson has stressed, that this be done early; when packing is done as a last desperate maneuver, the chances of salvage are virtually zero); 2) packing of hepatic venous injuries, which you have a 62% survival rate, as opposed to an atrial caval shunt, where the survival rate is only 9%.
I believe that atrial caval shunting has been virtually abandoned in this country. There are 188 published cases in the literature, with only 56 survivors (29%). When that was broken down and stratified to shunting, only 23% survived, and in those that were nonshunted, 52% survived.
Angioembolization, as you identified, Dr. Richardson, certainly played a major role both in the initial blush on CT scan and in the postoperative period.
The multidisciplinary approach concept in the treatment of complex hepatic trauma is rapidly becoming the standard.
I would like to ask Dr. Richardson questions on some of the new horizons such as the nonselective, nonoperative management of some penetrating injuries. Additionally, what is the role of hepatic resection for trauma? Finally, do you have any experience with the use of endovascular stents?
Presenter Dr. J. David Richardson (Louisville, Kentucky): Dr. Pachter, we operate on gunshot wounds in Louisville virtually all the time, but do observe some stab wounds. Our transplant team is heavily involved in their transplant activities. We think we have learned a great deal from our liver transplant team, but we can’t get them to take trauma call.
Dr. Timothy C. Fabian (Memphis, Tennessee): This study encompasses a tremendous clinical effort and the lessons which were learned over time. The authors describe the experience as an evolution. Indeed, the management schemes have mutated to the point that a markedly different phenotype of hepatic trauma management has resulted from 1975 to today. Hepatic artery ligation was a novel approach in the mid-1970s and accounted for 13% of their management, but it is rarely applied today. Similarly, atrial caval shunting has become a vestigial appendage among the operative strategies.
What has taken their place over time? While gauze packing was anathema 25 years ago, the authors have well demonstrated that it can be a valuable lifesaving technique that is applied in nearly 10% of their recent cases; omental packing similarly from zero to 10%.
Perhaps the most significant change has been in the adoption of nonoperative management with blunt injury. While essentially never being chosen until the past decade, it remarkably now accounts for over 80% of the management of blunt hepatic trauma.
We recently reported a 10-year experience with approximately 1,000 blunt liver injuries from Memphis at the Southern Surgical (Ann Surg, June 20), and that experience is remarkably similar to that reported by Dr. Richardson today from Louisville.
I would like to ask four brief questions. One, do you have specific physiologic criteria established for choosing nonoperative management? Similarly, are there any specific CT criteria, such as liver injury grade or volume of hemoperitoneum, which mitigate against nonoperative management in the stable patient? Three, we experienced a 7.5% failure rate with nonoperative management, equally divided between liver-related and nonliver-related failures—i.e., missed small bowel, pancreas, or other organ injuries. What was your experience with nonoperative management failures?
We too have adopted a “don’t poke a skunk” approach, and have noted significant improvements in outcomes, including lower transfusion requirements and decreased abdominal infections and lengths of stay comparing nonoperative to operative management. Did you note similar outcome differences beyond mortality?
Dr. Richardson: We use specific physiologic criteria. If we can make a patient stable with 4 units of blood, then we proceed with a nonoperative approach. If we get beyond that in terms of transfusion requirements or if they become unstable, then we think about operating on them fairly quickly. We do not use CT criteria as indication for operation since CTs of the liver can look terrible in patients who do well. The amount of fluid in the abdomen is not relied upon as a need for operation in and of itself. We have about a 5% failure rate.
We often use a laparoscopic technique for delayed washout of the abdomen, which allows us to get rid of bile and blood combination which often has the patient in SIRS state. We think that bile and blood evactuation is a useful thing to do.
Finally, I am convinced that the biggest advantage in nonoperative management is not the avoidance of operation, but that in some patients you don’t stir up bleeding which ultimately kills them.
Dr. John Terblanche (Cape Town, South Africa): It has taken some time for people to recognize the importance of the use of conservative management for hepatic trauma. About 2 decades ago, our pediatric surgeons were the first to start with conservative management (J Paed Surg 1985; 20:14–18). We commenced in adults about 11/2 decades ago, initially with blunt trauma, then with knife wounds, and today with low-velocity gun missile wounds as well.
A tremendously important point about packing is that with therapeutic packing, where the patient has been closed and gone back to intensive care, very often when one reoperates to remove the packs, the bleeding has stopped. We even have documented evidence of hepatic vein injury that doesn’t bleed when you take the packs out. Have you had similar experience? Certainly very often when the packs come out, we do not need to do anything else.
Dr. Richardson: Prof. Terblanche, we have had the same experience. Dr. Carrillo, one of my colleagues, and I described a small series of patients in which we have actually put a vascular clamp on the front wall of the retrohepatic cava down behind the liver, left the clamp, and packed things around it. The following day the clamps were then removed. Bleeding has not occurred in these patients. We now have extended that to a series of about four or five patients. Interestingly, all of them have survived. And we have seen the same thing with packing alone as you have noted.
Dr. Donald D. Trunkey (Portland, Oregon): I have some concern about overenthusiasm for the nonoperative approach to liver injuries, and because of this, I went to our registry and pulled my personal experience over the last 11 years.
I had 74 patients with liver injuries. In 24, I made a decision not to operate based on the CT scan and the physiologic response of the patient. I had 25 patients, though, that I operated on primarily for associated injuries. You did not discuss the importance of associated injuries in your paper, and I want you to comment on that. In my 25 patients, 19 had bleeding or hollow viscus injury that required surgery. I had 25 patients that I operated on primarily because of the liver injury. Four I treated with packing, and in 11 patients I either repaired a retrohepatic caval injury or did a major resection.
In patients requiring surgery for their liver injuries, you are right, angiography does help with management, including embolization. But we are now identifying complications from this approach. We see liver necrosis from the embolization and we had had to operate and resect the dead liver. We are also seeing an increasing number of bilomas. I would like to have you comment and whether this is corroborated in your series.
Dr. Richardson: Absolutely. Again, 2 years ago at the AAST, Dr. Carrillo reported our experience, which I think was very similar to the recently reported L.A. County experience. If you are going to use nonoperative treatment—“nonoperative” in quotes, because I think at times it is early nonoperative treatment—you have to have other arrows in your quiver. You have to use the multidisciplinary approach to manage these patients. Drain of a biloma can be done percutaneously; sometimes we do it laparoscopically. Occasionally you have to do delayed operation to resect necrotic liver. But it has been our experience, Dr. Trunkey, that delayed operation can be done more safely because some of the other injuries are sorted out.
In terms of the associated injuries, it is my belief that if a patient has bleeding from multiple sources, those patients rarely are stabilized with 4 units of blood. And that is the group that usually in fact requires operation.
Footnotes
Correspondence: J. David Richardson, MD, Dept. of Surgery, University of Louisville, Louisville, KY 40292.
Presented at the 120th Annual Meeting of the American Surgical Association, April 6–8, 2000, The Marriott Hotel, Philadelphia, Pennsylvania.
E-mail: jdrich01@gwise.louisville.edu
Accepted for publication April 2000.
References
- 1.Flint LM, Mays ET, Aaron WS, et al. Selectivity in the management of hepatic trauma. Ann Surg 1977; 185: 613–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore EE, Shackford SR, Pachter HL, et al. Organ injury scaling: spleen, liver, kidney. J Trauma 1999; 29: 1664–1666. [PubMed] [Google Scholar]
- 3.Cue JI, Cryer HG, Miller FB, Richardson JD. Packing and planned re-exploration for hepatic and retroperitoneal hemorrhage: critical refinements of a useful technique. J Trauma 1990; 30: 1007–1013. [DOI] [PubMed] [Google Scholar]
- 4.Feliciano DV, Mattox KL, Burch JM, et al. Packing for control of hepatic hemorrhage. J Trauma 1986; 26: 738–743. [DOI] [PubMed] [Google Scholar]
- 5.Pachter HL, Spencer FC, Hofstetter SR, et al. Significant trends in the treatment of hepatic trauma: Experience with 411 injuries. Ann Surg 1992; 215: 492–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flint LM, Mays ET, Aaron WS, et al. Selectivity in the management of hepatic trauma. Ann Surg 1977; 185: 613–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aaron S, Fulton RL, Mays ET. Selective ligation of the hepatic artery for trauma of the liver. SGO 1975; 141: 187–189 [PubMed] [Google Scholar]
- 8.Flint LM, Polk HC. Selective hepatic artery ligation: limitations and failures. J Trauma 1979; 19: 319–323. [DOI] [PubMed] [Google Scholar]
- 9.Cogbill TH, Moore EE, Jurkovich GJ, et al. Severe hepatic trauma: a multicenter experience with 1,335 liver injuries. J Trauma 1988; 28: 1433. [PubMed] [Google Scholar]
- 10.Asensio JA, Demetriades D, Chawan S, et al. Approach to the management of complex hepatic injuries. J Trauma 2000; 48: 66–-69. [DOI] [PubMed] [Google Scholar]
- 11.Feliciano DV, Jordan GL, Bhondo CG, et al. Management of 1,000 consecutive cases of hepatic trauma (1979–1984). Ann Surg 1986; 204: 438–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madding GF, Kennedy PA. Trauma to the Liver. Philadelphia: WB Saunders, 1965.
- 13.Garrison JR, Richardson JD, Hilakos AS, et al. Predicting the need to pack early for severe intra-abdominal hemorrhage. J Trauma 1996; 40: 923–926. [DOI] [PubMed] [Google Scholar]
- 14.Rotondo MF, Schwab CW, McGonigal MD, et al. Damage control: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 1993; 35: 375. [PubMed] [Google Scholar]
- 15.Calmona RH, Peck DZ, Lim RC. The role of packing and planned reoperation in severe hepatic trauma. J Trauma 1984; 24: 779–784. [DOI] [PubMed] [Google Scholar]
- 16.Feliciano DV, Mattox KL, Burch JM, et al. Packing for control of hepatic hemorrhage. J Trauma 1986; 26: 738–743. [DOI] [PubMed] [Google Scholar]
- 17.Ivatury PR, Nallathambi M, Gundvz Y, et al. Liver packing for uncontrolled hemorrhage: a reappraisal. J Trauma 1986; 26: 744–753. [DOI] [PubMed] [Google Scholar]
- 18.Stone HH, Strom PR, Mullins RJ. Management of the major coagulopathy with onset during laparotomy. Ann Surg 1984; 197: 532–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meredith JW, Young JS, Bowling J, Robboussin D. Nonoperative management of blunt hepatic trauma: the exception or the rule? J Trauma 1994; 36: 529–535. [DOI] [PubMed] [Google Scholar]
- 20.Croce MA, Fabian TC, Menke PG, et al. Nonoperative management of blunt hepatic trauma is the treatment of choice for hemodynamically stable patients. Results of a prospective trial. Ann Surg 1995; 221: 744–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pachter HL, Hofstetter SR. The current status of nonoperative management of adult blunt hepatic injuries. Am J Surg 1995; 169: 442–454. [DOI] [PubMed] [Google Scholar]
- 22.Carrillo EH, Platz A, Miller FB, Richardson JD. Nonoperative treatment of blunt hepatic trauma. Br J Surg 1998; 85: 461–468. [DOI] [PubMed] [Google Scholar]
- 23.Farnell MB, Spencer MP, Thompson E, et al. Nonoperative management of blunt hepatic trauma in adults. Surgery 1988; 104: 748–756. [PubMed] [Google Scholar]
- 24.Knudson MM, Maull KI. Nonoperative management of solid organ injuries: past, present and future. Surg Clin North Am 1999; 79: 1357–1371. [DOI] [PubMed] [Google Scholar]
- 25.Malhotra AK, Fabian TC, Croce MA, et al. Blunt hepatic injury: a paradigm shift from operative to nonoperative management in the 1990s. Ann Surg 2000; 231: 804–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carrillo EH, Spain DA, Wohltmann CD, et al. Interventional techniques are useful adjuncts in nonoperative management of hepatic injuries. J Trauma 1999; 46: 619–624. [DOI] [PubMed] [Google Scholar]
- 27.Carrillo EH, Richardson JD. Delayed surgery and interventional procedures in complex liver injuries. J Trauma 1999; 46: 978. [DOI] [PubMed] [Google Scholar]
- 28.Shrock T, Blaisdell FW, Mathewson C Jr. Management of blunt trauma to the liver and hepatic veins. Arch Surg 1968; 96: 698–704. [DOI] [PubMed] [Google Scholar]
- 29.Kudsk KA, Sheldon GF, Lim RC Jr. Atriocaval shunting (ACS) after trauma. J Trauma 1982; 22: 81–85. [DOI] [PubMed] [Google Scholar]
- 30.Burch JM, Feliciano DV, Mattox KL. The atriocaval shunt: facts and fiction. Ann Surg 1988; 207–555. [DOI] [PMC free article] [PubMed]
- 31.Pachter HL, Spencer FC, Hofstetter SR, Liang HC, Coppa GF. The management of juxtahepatic venous injuries without an atriocaval shunt. Preliminary clinical observations. Surgery 1986; 99: 569–575. [PubMed] [Google Scholar]
- 32.Carrillo EH, Spain DA, Richardson JD, et al. Intrahepatic vascular clamping in complex hepatic vein injuries. J Trauma 1997; 43: 131–133. [DOI] [PubMed] [Google Scholar]
- 33.Beal SL. Fatal hepatic hemorrhage: an unresolved problem in the management of complex liver injuries. J Trauma 1990; 30: 163–169. [PubMed] [Google Scholar]
- 34.Klein SR, Baumgartner FJ, Bongard FS. Contemporary management strategy for major inferior vena caval injuries. J Trauma 1994; 37: 35–42. [DOI] [PubMed] [Google Scholar]