Abstract
Objective
To determine, in a series of patients with secondary and tertiary parathyroid hyperplasia, whether the type of parathyroidectomy (subtotal, total with autotransplantation, or total), the histologic pattern of the parathyroid tissue, or the proliferative index, as determined by Ki-67 analysis, could predispose patients to recurrent hyperparathyroidism.
Summary Background Data
Recurrent hyperparathyroidism appears in 10–70% of the patients undergoing surgery for secondary or tertiary hyperparathyroidism. The incidence could be related to the type of operation (Rothmund) but also depends on the histologic pattern of the glands removed (Niederle).
Methods
The retrospective investigation was performed on 446 patients undergoing parathyroid surgery. They were also studied in relation to the possibility of renal transplantation. In this population, two homogeneous groups were subsequently identified (23 patients with clear signs of recurrence and 27 patients apparently cured); they were studied from the histologic and immunohistochemical point of view using antibody to Ki-67 antigen.
Results
Subtotal parathyroidectomy, total parathyroidectomy with autotransplantation, and total parathyroidectomy produced similar results when considering the regression of osteodystrophy, pruritus, and ectopic calcification. As one could anticipate, tota1parathyroidectomy increased the incidence of hypoparathyroidism. The percentage of recurrence was 5% to 8% after subtotal parathyroidectomy, total parathyroidectomy with autotransplantation, and total parathyroidectomy, and only after incomplete parathyroidectomy did this percentage climb to 34.7%. In the recurrence group, the nodular form was more common and the proliferative fraction detected by Ki-67 was 1.9%; it was 0.81% in the control group.
Conclusions
Because more radical procedures were not more effective, the authors favor a less radical procedure such as subtotal parathyroidectomy. Histologic patterns and proliferative fraction could be useful indices of a recurrence, and these patients should be watched closely after surgery.
Most patients with chronic renal failure develop secondary hyperparathyroidism. The prevalence of this disease based on bone biopsies is approximately 67%. Only 5% of these patients require parathyroidectomy because most are treated pharmacologically using calcium and vitamin D, either orally or intravenously, with maintenance of adequate calcium levels during dialysis. Hyperphosphatemia is controlled by an appropriate diet and the administration of phosphorus chelating agents. 1–4 The incidence in patients in whom the disease appears or progresses after kidney transplantation (tertiary hyperparathyroidism) is 6% to 7%. 5,6
The indication for surgery is often failure of the pharmacologic therapy as a result of poor patient compliance during dialysis, with worsening of uremic osteodystrophy. Subperiosteal lesions of the hands and feet phalanges, acromioclavicular fractures, pubic symphysis diastasis, salt-and-pepper skull lesions, or vascular and ectopic calcifications and pruritus are diagnostic.
The most important biochemical findings include elevated levels of intact parathyroid hormone (400 pmol/L or more, normal range 10–65), osteocalcin, and serum alkaline phosphatase. The degree of hypercalcemia is not as important: it becomes relevant only when its concentration exceeds 10.5 mg%, indicating autonomous function of one or more glands. Obviously, patients with a low level of calcium must be treated with supplementary calcium and vitamin D, but in many cases the level of parathyroid hormone remains high. A calcium phosphate product of more than 70 is another main indication for parathyroidectomy. The situation differs for patients awaiting a kidney transplant: they should undergo surgical treatment before kidney transplantation if the intact parathyroid hormone level exceeds 400 pmol/L, despite adequate medical therapy, to avoid injury to the graft. 7
If hyperparathyroidism is not corrected, other lesions can appear related to the immunosuppressive and corticoid therapy. These include rupture of ligaments and tendons, metastatic calcifications, and calciphylaxis. 7,8 In these cases, the concentration of calcium is expected to be high.
A high S-phase fraction 9 and several histologic parameters such as total parenchymal mass, 10,11 nodular growth pattern, 1,12 absence of fat cells, and high mitotic index 12,13 have been proposed as markers of poor parathyroid suppressibility. In a recent study of parathyroid tumors (adenomas and carcinomas), we proposed that high proliferative activity, as detected by Ki-67 antigen expression, is an adjunct to the histopathologic diagnosis of parathyroid lesions that can be used to discriminate clinically aggressive from clinically indolent cases. 14
The aim of this paper is to determine, in a series of patients with secondary and tertiary parathyroid hyperplasia, whether the type of parathyroidectomy (subtotal, total with autotransplantation, or total), the histologic pattern of the parathyroid tissue, or the proliferative index, as determined by Ki-67 analysis, could predispose patients to recurrent hyperparathyroidism.
PATIENTS AND METHODS
Between January 1975 and July 1998, 446 patients (227 men, 219 women) with an average age of 47 years underwent surgery for complications of secondary and tertiary hyperparathyroidism after a mean of 7 years and 8 months of dialysis.
All patients were treated before surgery with supplementary calcium and vitamin D, orally or intravenously, for at least 2 years. Surgery was considered mandatory if the parathyroid hormone level increased to more than 400 pmol/L despite the therapy; ectopic and vascular calcification and the levels of calcium, phosphorus, alkaline phosphatase, and osteocalcin must be considered.
We performed 323 subtotal parathyroidectomies, 60 total parathyroidectomies with autotransplantation, 31 total parathyroidectomies alone, and 32 lesser procedures (fewer than three glands removed). We preferred to perform subtotal parathyroidectomy because of the shorter surgical time, avoiding the need for cryopreservation. In some instances (reoperation, difficulty to assess a well-vascularized remnant), we performed total parathyroidectomy with autotransplantation. Total parathyroidectomy was performed only at the beginning of our experience in patients older than 70 years.
Two groups were studied: 44 patients (23 men, 21 women; average age, 43 years) who underwent surgery after kidney transplantation (group 1), and 42 patients (27 men, 15 women; average age, 40 years) with a mean dialysis time of 7 years and 3 months who underwent kidney transplantation shortly after parathyroidectomy (group 2).
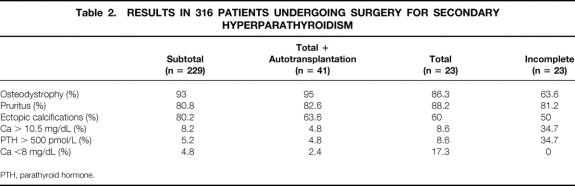
Two other groups were identified: 23 patients in whom hyperparathyroidism recurred after an initial successful surgical procedure, and 27 patients in whom it did not and who had a normal parathyroid hormone level, regression of osteodystrophy and ectopic calcifications, and no pruritus. These two groups were similar in age, degree of hypocalcemia and phosphatemia, parathyroid hormone levels, duration of dialysis, type of surgery, and total weight of glands removed (approximately 4 g) (Table 1).
Table 1. COMPARISON OF TWO GROUPS OF PATIENTS UNDERGOING SURGERY FOR SECONDARY HYPERPARATHYROIDISM
We used the immunohistochemical method of Abbona et al 14 involving antigen Ki-67 to evaluate the proliferative fraction by counting the number of positive nuclei in 1,000 cells per gland examined.
The results were analyzed in relation to the type of surgical procedure after adequate follow-up from 1975 to 1995. During that period, 341 patients underwent parathyroidectomy; 315 of them were followed up between 1 and 10 years.
RESULTS
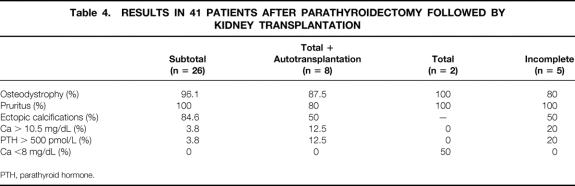
All surgical procedures caused regression of osteodystrophy, pruritus, and ectopic calcifications. The percentage of recurrence was 5% to 8% and did not differ among the various types of procedures. After total parathyroidectomy, 17.3% of patients had permanent hypocalcemia. Less satisfactory results were obtained after incomplete parathyroidectomy; when a gland was not found, the recurrence rate was 34.7% (Table 2). This group does not include recurrence resulting from a fifth parathyroid gland, which was present in 32 patients.
Table 2. RESULTS IN 316 PATIENTS UNDERGOING SURGERY FOR SECONDARY HYPERPARATHYROIDISM
PTH, parathyroid hormone.
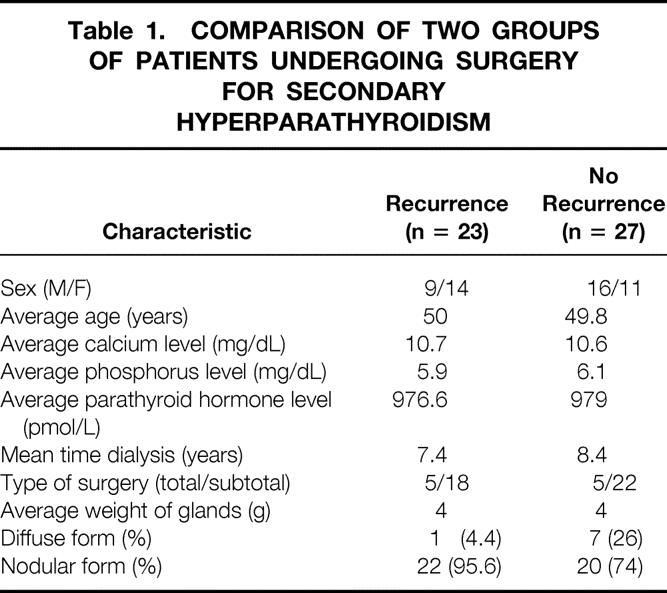
When we examined the patients who underwent surgery for tertiary hyperparathyroidism (hyperparathyroidism that develops after renal transplantation), we noted that the regression of osteodystrophy and ectopic calcifications was satisfactory after either subtotal or total parathyroidectomy and autotransplantation, with no recurrence and no hypocalcemia (Table 3).
Table 3. LONG-TERM RESULTS IN 29 PATIENTS UNDERGOING SURGERY FOR TERTIARY HYPERPARATHYROIDISM
PTH, parathyroid hormone.
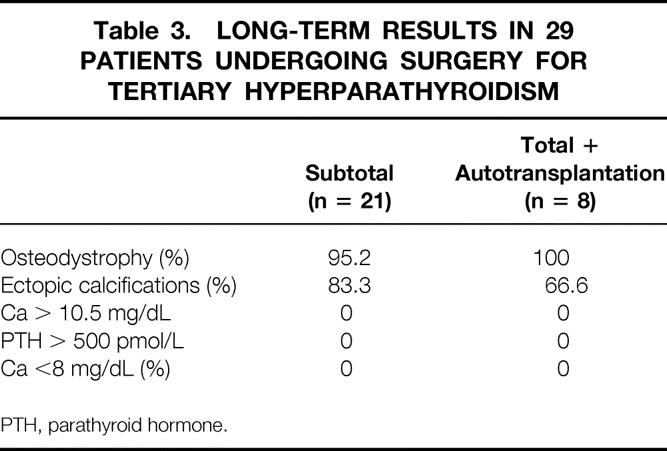
In the 42 patients in whom parathyroidectomy preceded renal transplantation, incomplete parathyroidectomy was associated with satisfactory results, with a recurrence rate of 20% as opposed to 35% in the other cases observed (P = .134). These results would confirm that kidney transplantation should be done soon after parathyroidectomy to avoid recurrence, particularly if only a gland was left behind (Table 4).
Table 4. RESULTS IN 41 PATIENTS AFTER PARATHYROIDECTOMY FOLLOWED BY KIDNEY TRANSPLANTATION
PTH, parathyroid hormone.
As to the influence of the macroscopic and microscopic characteristics of the gland left in the neck or transplanted on the evolution of the disease and the appearance of recurrence, macroscopically the results were favorable if the gland that was partially left in situ or transplanted was relatively small and surrounded by fat; histology and proliferative data confirm this statement. From a histologic standpoint, the diffuse form was seen in only a few patients; the nodular form was more often representative. The nodular form was found in 74% without recurrence, but in the recurrence group, 95.6% had the nodular form. This difference, although significant (P < .05), was not influenced by the surgical technique (subtotal parathyroidectomy vs. total parathyroidectomy with autotransplantation).
The histologic appearance consisted mostly of chief cells in 75% of cases, oxyphil cells in 20%, and clear cells in less than 4%. The unique difference (P < .03) was the presence of a large number of clear cells in the recurrent nodular form (4.3%) and in the control group (1%).
From the immunohistochemical standpoint, the proliferative fraction found with Ki-67, considering glands subtotally resected or autotransplanted, was 1.9% in the recurrence group and 0.8% in the control group (P = .001). In the recurrence group, the percentage of cells positive to Ki-67 was greater than in the control group (6.5% vs. 2%, P = .001) (Table 5).
Table 5. EVALUATION OF 50 PATIENTS BY Ki-67
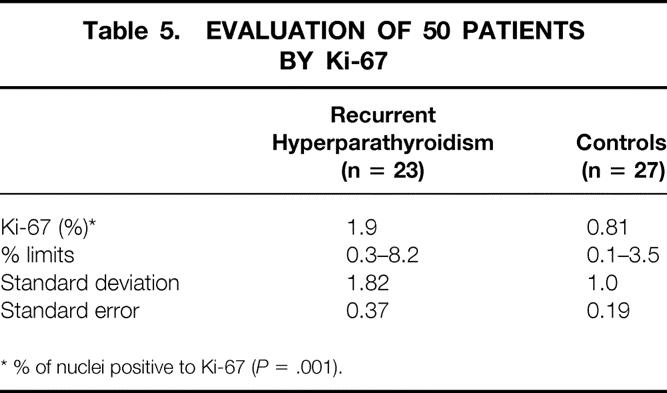
* % of nuclei positive to Ki-67 (P = .001).
In nodular hyperplasia, the proliferative fraction was calculated in every nodule. In the recurrence group, the highest density of cells positive to Ki-67 was found in 50% of the larger nodules. The same results were obtained in only 25% of the controls. Still, the central area of nodules contained many positive cells in both the recurrent and nonrecurrent group. It appears that the highest risk of recurrence occurs in the nodular forms where the proliferative fraction exceeds 1.5%.
The amount of well-vascularized parathyroid tissue left in the neck (40–50 mg), the autotransplantation technique (8 or 10 specimens transplanted in four pockets in the brachioradialis muscle of the nondominant arm), and the surgeon’s experience were similar in all procedures. The exploration of the anterosuperior mediastinum, as suggested by some authors, with partial removal of thymus to assess the presence of a fifth parathyroid gland, was performed in all the cases in the past 10 years; the percentage of cases in which a fifth parathyroid gland was found increased to 8% from only 3% in the previous experience. 15
DISCUSSION
When evaluating the results of all the types of surgical procedures, we found no significant difference in the recurrence rate between subtotal parathyroidectomy and total parathyroidectomy with autotransplantation, although there was a higher incidence of hypocalcemia after total parathyroidectomy. This restricts the use of total parathyroidectomy to a few, selected older patients who are not candidates for renal transplantation. Also, in the reoperative setting, total parathyroidectomy could be the first choice, but always with cryopreservation: it avoids the possibility of a third cervicotomy, so that autotransplantation could be performed later in case of hypocalcemia.
We performed autotransplantation after 3 months in three patients with satisfactory results. In one patient it was performed after 1 year of cryopreservation: histologic specimens were normal, but the transplant did not show any hormonal activity. The cryopreserved tissue may not function as well as primary autotransplanted parathyroid tissue, particularly after months of cryopreservation.
Less satisfactory results were obtained after incomplete parathyroidectomy, with a recurrence rate of 34.7% (8/23). In patients who underwent renal transplantation after parathyroidectomy, this percentage was reduced to 20%. Therefore, kidney transplantation is the principal objective after parathyroidectomy. High-risk patients should be referred for early renal transplantation after parathyroidectomy when possible. 7
From a macroscopic standpoint, the gland left in situ or transplanted should always be the smallest one and should have fatty tissue surrounding it. This was the case in all our patients who underwent surgery. The histologic characteristics of a portion of the gland left in situ or transplanted were studied morphologically and immunohistochemically. In the absence of definitive criteria to identify patients at risk of recurrence, we believe that some morphologic aspects (primarily diffuse vs. nodular enlargement, but also proliferative cellular activity) can be used to distinguish patients at increased risk. In the literature, the nodular form rather than the diffuse form is more frequently responsible for recurrence. 1,12,16 This is confirmed by our observations that the nodular form was present in 95% of recurrences and 74% of controls. The mean proliferative index as determined by the Ki-67 technique was significantly greater (1.9%) in the recurrent group than in the controls (0.81%, P = .001). In terms of the histologic characteristic of cells, the clear cells had a proliferative index activity greater than that of the chief cells.
Obviously, a missed supernumerary parathyroid gland could contribute to surgical failures: sometimes in these cases, glands are only remnants and after a period of good recovery the recurrence appears. The current opinion is that transcervical removal of thymic tissue is the best way to avoid this type of surgical failure. 15,17 Careful examination of the surgical site for supernumerary glands is also essential.
In contrast to other authors, 18 we did not routinely perform imaging procedures in secondary and tertiary hyperparathyroidism because of the poor results in identifying all parathyroid glands. Normally we use these procedures in reoperations and have found excellent sensitivity and specificity, especially for iodine-123/technetium-99m-sestamibi subtraction scintigraphy.
From our results and those of others, 19–25 we conclude that the nodular form is more frequent in recurrent hyperparathyroidism than the diffuse form (95.6% vs. 74%); the recurrences have a higher proliferative activity than the controls; a nodular form with an elevated proliferative index (>1.5–2%) indicates a high risk of recurrence; and the smallest normal-appearing gland responded best if left in situ or transplanted. Patients at risk of recurrence should be prioritized for kidney transplantation. In fact, recurrence after transplantation is lower even if one parathyroid was not found. Transplantation appears to have a favorable effect on cell proliferation even in the presence of high-risk baseline morphologic and proliferative findings. Finally, the type of surgical procedure does not influence the risk of recurrence. In summary, based on our experience, subtotal parathyroidectomy is the safest approach and should be the preferred procedure. Total parathyroidectomy with autotransplantation is the best procedure for treating recurrences, but the increased risk of hypoparathyroidism must be kept in mind. It is mandatory to cryopreserve some tissue to avoid the risk of hypocalcemia, particularly in patients who will need renal transplantation. Indeed, in the patients undergoing dialysis, metabolic acidosis compensates very well for hypocalcemia; we have never seen serious episodes of tetany, even with calcium levels of less than 7 mg%. Obviously the situation is different after kidney transplantation.
Footnotes
Correspondence: Guido Gasparri, MD, Dipartimento di Fisiopatologia Clinica, Sezione di Chirurgia Generale, Via Genova 3, 10126 Torino, Italy. E-mail: gasparri@molinette.unito.it
Accepted for publication March 14, 2000.
References
- 1.Mihai R, Farndon JR. Parathyroids: primary and secondary disease. In: Farndon JR,ed. Breast and endocrine surgery. London: Saunders Co. Ltd; 1997: 1–35.
- 2.Lee DB, Goodman WG, Coburn JW. Renal osteodystrophy: some new questions on an old disorder. Am J Kidney Dis 1988; 5: 365–376. [DOI] [PubMed] [Google Scholar]
- 3.Demeure MJ, McGee DC, Wilkes W,et al. Results of surgical treatment for hyperparathyroidism associated with renal disease. Am J Surg 1990; 160: 337–340. [DOI] [PubMed] [Google Scholar]
- 4.Chatterjee SN, Massry SG, Friedler RM,et al. The high incidence of persistent secondary hyperparathyroidism after renal homotransplantation. Surg Gynecol Obstet 1976; 143: 440–442. [PubMed] [Google Scholar]
- 5.D’Alessandro AM, Melzer JS, Pirsch JD,et al. Tertiary hyperparathyroidism after renal transplantation: operative indications. Surgery 1989; 106: 1049–1056. [PubMed] [Google Scholar]
- 6.Gasparri G, Camandona M, Jeantet A,et al. L’hyperparathyroidisme secondaire et tertiaire. Vingt ans d’experience. Lyon Chir 1994; 6: 403–408. [Google Scholar]
- 7.Gasparri G, Camandona M, Jeantet A,et al. Surgical treatment of tertiary hyperparathyroidism. Acta Chir Austriaca 1996; 28 (suppl 124): 48–50. [Google Scholar]
- 8.Duh QY, Lim RC, Clark OH. Calciphylaxis in secondary hyperparathyroidism. Diagnosis and parathyroidectomy. Arch Surg 1991; 126: 1213–1219. [DOI] [PubMed] [Google Scholar]
- 9.Tominaga Y, Tanaka Y, Sato K,et al. Recurrent renal hyperparathyroidism and DNA analysis of autografted parathyroid tissue. World J Surg 1992; 16: 595–603. [DOI] [PubMed] [Google Scholar]
- 10.Black WC, Slatopolsky E, Elkan I, Hoffsten P. Parathyroid morphology in suppressible and non suppressible renal hyperparathyroidism. Lab Invest 1976; 23: 497–509. [PubMed] [Google Scholar]
- 11.Hasleton PS, Ali HH. The parathyroid in chronic renal failure: a light and electron microscopical study. J Pathol 1980; 132: 307–323. [DOI] [PubMed] [Google Scholar]
- 12.Niederle B, Horandner H, Roka R, Woloszczuk W. Morphologic and functional studies to prevent graft dependent recurrence in renal osteodistrophy. Surgery 1989; 106: 1043–1048. [PubMed] [Google Scholar]
- 13.Ellis HA. Fate of long-term parathyroid autografts in patients with chronic renal failure treated by parathyroidectomy: a histopathological study of autografts, parathyroid glands and bone. Histopathology 1988; 13: 289–309. [DOI] [PubMed] [Google Scholar]
- 14.Abbona GC, Papotti M, Gasparri G, Bussolati G. Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining. Hum Pathol 1995; 26: 135–138. [DOI] [PubMed] [Google Scholar]
- 15.Proye C, Bizard JP, Carnaille B, Quievreux JL. La cinquieme glande en chirurgie parathyroidienne. Lyon Chir 1992; 88: 112–116. [Google Scholar]
- 16.Tominaga Y, Kohara S, Namii Y,et al. Clonal analysis of nodular parathyroid hyperplasia in renal hyperparathyroidism. World J Surg 1996; 20: 744–752. [DOI] [PubMed] [Google Scholar]
- 17.Numano M, Tominaga Y, Uchida K,et al. Surgical significance of supernumerary parathyroid glands in renal hyperparathyroidism. World J Surg 1998; 22: 1098–1103. [DOI] [PubMed] [Google Scholar]
- 18.Jeanguillaume C, Urena P, Hindie E,et al. Secondary hyperparathyroidism: detection with I-123-Tc-99m-sestamibi subtraction scintigraphy versus US. Radiology 1998; 207: 207–213. [DOI] [PubMed] [Google Scholar]
- 19.Dubost C, Kracht M, Assens P,et al. Reoperation for secondary hyperparathyroidism in hemodialysis patients. World J Surg 1986; 10: 654–660. [DOI] [PubMed] [Google Scholar]
- 20.Gagne ER, Urena P, Leite-Silva S,et al. Short- and long-term efficacy of total parathyroidectomy with immediate autografting compared with subtotal parathyroidectomy in hemodialysis patients. J Am Soc Nephrol 1992; 3: 1008–1017. [DOI] [PubMed] [Google Scholar]
- 21.Packman KS, Demeure MJ. Indications for parathyroidectomy and extent of treatment for patients with secondary hyperparathyroidism. Surg Clin North Am 1995; 75: 465–482. [DOI] [PubMed] [Google Scholar]
- 22.Rothmund M, Wagner PK, Schark C. Subtotal parathyroidectomy versus total parathyroidectomy and autotransplantation in secondary hyperparathyroidism: a randomized trial. World J Surg 1991; 15: 745–750. [DOI] [PubMed] [Google Scholar]
- 23.Tagaki H, Tominaga Y, Uchida K,et al. Subtotal versus total parathyroidectomy with forearm autograft for secondary hyperparathyroidism in chronic renal failure. Ann Surg 1984; 200: 18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Visset J. Parathyroidectomie subtotale pour hyperparathyroidie secondaire. Lyon Chir 1992; 88: 126–128. [Google Scholar]
- 25.Neonakis E, Wheeler MH, Krishnan H,et al. Results of surgical treatment of renal hyperparathyroidism. Arch Surg 1995; 130: 643–648. [DOI] [PubMed] [Google Scholar]