Abstract
Objective
To examine the first decade of experience with minimal access surgery, with particular attention to issues of training surgeons already in practice, and to provide a set of recommendations to improve technical training for surgeons in practice.
Summary Background Data
Concerns about the adequacy of training in new techniques for practicing surgeons began almost immediately after the introduction of laparoscopic cholecystectomy. The concern was restated throughout the following decade with seemingly little progress in addressing it.
Methods
A preliminary search of the medical literature revealed no systematic review of continuing medical education for technical skills. The search was broadened to include educational, medical, and psychological databases in four general areas: surgical training curricula, continuing medical education, learning curve, and general motor skills theory.
Results
The introduction and the evolution of minimal access surgery have helped to focus attention on technical skills training. The experience in the first decade has provided evidence that surgical skills training shares many characteristics with general motor skills training, thus suggesting several ways of improving continuing medical education in technical skills.
Conclusions
The educational effectiveness of the short-course type of continuing medical education currently offered for training in new surgical techniques should be established, or this type of training should be abandoned. At present, short courses offer a means of introducing technical innovation, and so recommendations for improving the educational effectiveness of the short-course format are offered. These recommendations are followed by suggestions for research.
Laparoscopic cholecystectomy was developed in the late 1980s. 1 This new technique represented a substantial change in the way this common surgical procedure was performed. Based on the perceived advantages of this new approach, it rapidly became the standard method for cholecystectomy. 2 Since the introduction of laparoscopic cholcystectomy, there has been an increase in the number of surgical procedures that can be performed using this general approach, and the term minimal access surgery (MAS) has evolved to describe it. 3 This evolution has created an ongoing continuing education need among practicing surgeons for training in these new techniques. This need has been met with short courses developed by surgeons already experienced with the new procedures. 4 These courses have continued to expand to meet this and other technical training needs of surgeons. This type of continuing medical education, developed primarily to teach a new technique, is the focus of this review and is designated continuing medical education for surgical techniques (CMEST).
Concern about the adequacy of short courses for CMEST developed quickly and has persisted throughout the decade. 5–12 For example, in 1991 Dent stated, “Rumors of a steep learning curve, common bile duct injuries, massive hemorrhage, and even deaths following laparoscopic surgery are rife.”5 That same year, Gadacz and Talamini 6 stated, “Hands-on experience is essential and a 2- or 3-day ‘mini’ course is essential but not sufficient.” In 1992 Zucker 7 said, “Weekend courses … are clearly no substitute for hands-on experience.” Two years later Rock and Warshaw 8 stated, “the presumption that new and technically demanding surgical skills can be learned in a ‘weekend course’ makes us vulnerable to the questioning of our profession and of our skill as surgeons.” Gates 9 in 1997 stated, “Generally speaking, a weekend course in endoscopic surgery would not be adequate to provide the required level of knowledge or skill.” As the decade drew to an end, Reznick 10 asked, “How can our profession avoid a repetition of the laparoscopic cholecystectomy fiasco, wherein surgeons were learning a new technique on a live animal model on Sunday and performing the procedure on Monday?”
Studies evaluating the educational impact of these CMEST short courses provide evidence that the concerns were well founded. A survey of practicing surgeons reported that most did not believe they were adequately trained to perform laparoscopic cholecystectomy after a 2-day workshop. 11 Another survey showed that the complication rate was higher in the initial experience among surgeons who performed the new procedures after having taken only one of these courses. 13
This review examines the first decade of experience with MAS, with particular attention to training aspects. The goal was to discover, from this experience, solutions to the general challenge of providing CMEST to surgeons in practice. Although the changes associated with MAS have been profound, gradual technical innovation, both within and beyond MAS, can be expected, 14,15 thus creating a lifelong need for effective CMEST for every surgeon.
METHOD
An initial search of the Medline database was undertaken for the years 1989 to 1999 using the search terms “laparoscopy,” “skills,” “technique,” “surgery,” “minimal access surgery,” and “continuing medical education.” This search yielded no systematic review of the general area of CMEST during this period. Consequently, the review was focused on four general areas: continuing medical education (CME), surgical technical curricula, surgical learning curve, and general psychomotor skills acquisition.
Seven different specific literature databases were searched covering the period 1989 to 1999 and limited to English-language publications. All titles and abstracts were reviewed and appropriate citations were selected for complete review. A manual search of the references of these citations was performed, and relevant papers and textbooks were also selected for review. This included literature in the period before 1989. For the CME literature, the term “continuing medical education” was used to search EBM Reviews, Medline, ERIC, and Education Abstracts. The search was narrowed by selecting review articles published in the past decade. For the literature on surgical technical curricula, the terms “surgery,” “skills,” and “techniques” were used in various combinations to search Medline, EBM Reviews, ERIC, PsycFirst, and Education Abstracts. For the surgical learning curve literature, the terms “learning,” “performance,” and “curve” were used in various combinations to search Medline, Education Abstracts, ERIC, and Newspaper Abstracts. This search was narrowed by selecting only articles that addressed the learning curve associated with surgical procedures. For the motor skills literature, the terms “motor,” “psychomotor,” “skills,” and “acquisition” were used in various combinations to search ERIC, Education Abstracts, and PsycFIRST. Finally, the websites for the Society of American Gastrointestinal Endoscopic Surgeons (SAGES) and the American Council on Continuing Medical Education were searched for standards pertinent to CMEST.
RESULTS
The results of the literature search and analysis of those results will be presented according to the four general areas reviewed: CME, surgical technical curricula, surgical learning curve, and general psychomotor skills acquisition.
Continuing Medical Education
Early in the MAS movement, SAGES developed guidelines for CMEST courses 16 and for granting privileges for MAS procedures. 17 The recommendations stated that in addition to taking a course, a surgeon must have experience as an assistant and then perform the initial procedures on patients under the supervision of a surgeon with MAS privileges. A survey of how surgeons actually obtained training for laparoscopic cholecystecomy showed that only about half of surgeons actually satisfied all the SAGES recommendations. 18 Reasons cited for the failure of surgeons to satisfy all the requirements included a lack of training opportunities, the cost of the training, and the lack of experienced colleagues.
There has been considerable research in improving the effectiveness of general CME courses in changing physician behaviors and patient outcomes. Several factors have been identified that increase the likelihood that change will occur after a physician participates in a CME course. 19,20 Educational sessions that communicate or disseminate information are less effective than interventions that provide the information and facilitate the desired change or reinforce the change. Multifaceted interventions are more effective at producing change than are single interventions. A careful, specific needs assessment improves the effectiveness of the course. Longer programs are more effective than day-long short courses. Performance change is greater when all participants are from the same practice setting. Finally, interactive sessions that provide the opportunity for practice are more effective than didactic sessions.
Most of the research on CME involved evaluating courses designed primarily to impart new knowledge or nontechnical skills. It has been recently recognized in the CME literature that psychomotor skill acquisition is distinct from other types of learning. 21 Consequently, it is unclear which of the above factors should be present in CMEST courses.
In summary, the research on creating effective CME has not included CMEST. Further, many surgeons are not following the existing recommendations for obtaining training in new techniques.
Surgical Technical Curricula
Before the introduction of MAS, the surgical literature addressing technical training dealt primarily with different animate and inanimate models, with little attention to specific aspects of a technical curriculum, 22 except for the short courses developed in Britain for resident technical training. 23
The MAS movement has helped to focus attention on surgical technical training, perhaps because these procedures differed so significantly from the existing techniques. Several studies have examined training methods for teaching the new skills associated with the MAS approach.
Several “drills,” elemental skills that involve more complex surgical skills, have been developed, with a modest correlation between improvement in the performance of these drills and the total task. 24 It has been shown that clinical laparoscopy experience results in enhanced performance on training tasks in a simulated environment, 25 suggesting but not proving that the reverse might be true as well. Substantial evidence has been developed that performance, measured by either a subjective rating or time on task, improves with practice. 24,26,27
A major gap in this literature is the lack of proof of a relationship between performance in these simulated environments and actual surgery. 25,28,29 This gap between performance in a simulated environment, either traditional or computer-based, exists because no work has yet been done demonstrating that performance of a procedure on models relates to performance of the actual procedure on patients. A first step in bridging this gap has been taken with the demonstration that performance of a laparoscopic procedure on an inanimate model translates to performance of the procedure in an animal model. 30
It could be argued that the findings of much of this research do not apply to experienced practicing surgeons, because most studies were done with surgical residents as study subjects. However, it has been shown that “senior surgeons” learn these skills in a fashion similar to residents. 31
The review of technical skills curricula shows that one positive effect of the MAS movement has been to focus attention on training. That practice improves performance suggests that learning a surgical skill shares features with general motor skills learning, 32 and this appears to apply to both experienced surgeons and residents. The approach of teaching a complex surgical skill by dividing it into simpler component tasks, a strategy described in the motor skills literature, 33 has been validated.
Surgical Learning Curve
Another consequence of the MAS movement has been increased attention to the learning curve in the surgical literature. 12,34–47 A learning curve is a graphic representation of the relationship between experience with a procedure and an outcome variable, usually a performance characteristic of clinical interest, such as operative time. Studies have generally shown that with increasing experience, operative time decreases, 34,36,37,39–44,47 the complication rate is lower, 34,35,37,41,42,47 and there are fewer conversions to the standard procedure. 34,41,43,47 Learning curves have four significant implications for CMEST.
First, the general shape of surgical learning curves is similar to the “performance curve” described in the general motor skills literature. 48,49 An established characteristic of performance curves is that improvement occurs more rapidly during the early experience. 33,50 Consequently, the early part of the performance curve is steep, a feature also observed in learning curves associated with surgical procedures 47 (Fig. 1). As experience accumulates, the curve becomes flatter, with less improvement with each additional experience. From an educational perspective, a relatively small increase in the amount of practice provided during a course could substantially improve technical performance.
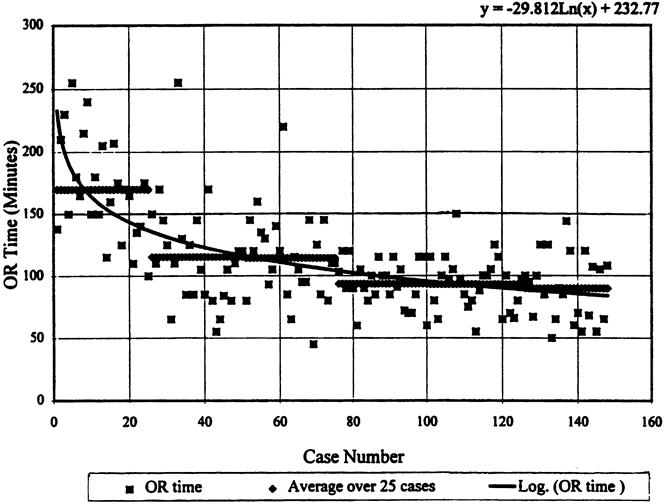
Figure 1. A learning curve showing the relationship between operative time and experience for laparoscopic fundoplication in children. (Used with permission from Meehan JJ, Georgeson KE. The learning curve associated with laparoscopic antireflux surgery in infants and children. J Pediatr Surg 1997; 32:426–429.)
Second, the curves for the declining operative time and complication rate are similar (Figs. 1 and 2). This suggests that increased familiarity with the task increases confidence and therefore increases speed and decreases errors. From the perspective of curriculum design and performance assessment, this relationship is helpful because operative time is easily measured during a course, whereas the complication rate of the actual surgical procedure is not. If the curriculum is designed to optimize the performance characteristic of operative time, then the complication rate should decrease as well, although the extent to which this is true is yet to be precisely known.
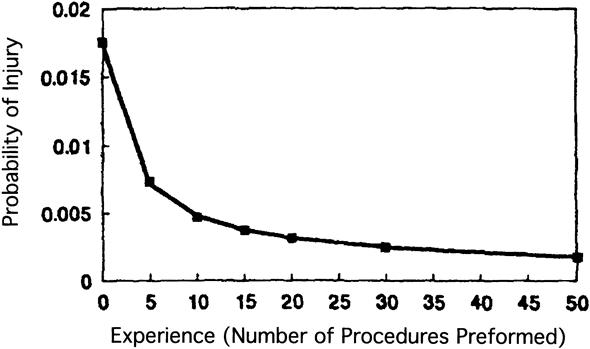
Figure 2. A graph of the calculated probability of bile duct injury during laparoscopic cholecystectomy. (Used with permission from Southern Surgeons Club, Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. Am J Surg 1995; 170:55–59.)
Third, there is evidence in the surgical literature that the shape of the learning curve varies for each individual learner and task, 33,37,40,47 a phenomenon recognized for motor skills learning in the psychology literature. 33,48 A feature of these individual performance curves is that they do not follow the smooth predictable curve generated by a group. 33 The educational implication for CMEST is that a course should take into consideration the performance differences among the participants.
Finally, the fact that surgical learning curves are similar to motor performance curves provides additional evidence that what is known of the psychology of learning motor skills should be applied to teaching surgical skills. This general educational strategy was suggested more than 100 years ago 51 and was endorsed for surgical training in 1987 by Barnes. 52
Motor Skills Theory
Systematic research on motor skills acquisition has been done for more than 100 years, 53 and several theories have been developed to explain how motor skills are learned. 48 The theories are sufficiently divergent to be considered distinct schools. 54 For the purposes of curricular planning, frameworks that describe stages of motor learning are perhaps more useful than these general learning theories. Fitts and Posner 55 described a three-stage model of motor skills acquisition that has received attention in the surgical literature. 56,57 In the first stage, the cognitive phase, the learner gains an understanding of the task, a process assisted by instructor explanations and demonstrations. The second stage is the associative phase, during which the learner practices the task and eliminates error from the performance. The role of the instructor is to provide feedback, identifying errors and providing explanation for corrective actions that the learner may take. Finally, the learner moves into the autonomous stage of learning, where he or she performs the task in a relatively automatic fashion with little or no cognitive input.
To date, most theories and models of motor skills learning have been developed based on studies of extremely simple motor tasks. In this context, even a basic surgical skill, such as tying a knot, would be regarded as a complex motor skill. This is important because some aspects of optimal teaching of simple motor skills do not necessarily apply to the teaching of more complex skills. For example, it has been shown that instructor feedback given after each performance of a simple motor task results in inferior mastery of the skill compared with feedback given at intervals. 58 The opposite has been found in the acquisition of a complex motor task. 59
DISCUSSION
The question of how best to teach practicing surgeons new surgical techniques remains incompletely answered. After a decade of MAS experience, there has been seemingly little progress in developing alternatives to the CMEST short courses, even though the literature shows that these courses are insufficient to provide adequate training in and of themselves. Based on the present review, a set of recommendations is proposed to improve the educational content of workshops or short courses designed to teach technical skills. These include recommendations to the individual surgeon or “consumer” and to those responsible for developing and accrediting the courses. In addition, some suggestions for research are provided.
Recommendations for the Practicing Surgeon
The surgeon consumer of CMEST should select a course designed to move the students “further along the learning curve.”60 In other words, by the end of the course, the surgeon should be at the point on the learning curve where error is minimized and performance is optimal. For the present, the surgeon should select a course that satisfies the SAGES requirements, now interpreted in light of what has been learned in the first decade of MAS experience:
1. The course should provide a set of objectives and a description of the assessment methodology. The current SAGES guidelines include the recommendation that CMEST courses should have objectives that describe the technical task and the method of assessment. 16 These objectives and assessment criteria should include specific performance characteristics: for example, to pass the course, the participant should be able to perform the technique in a given period with a prescribed success rate.
-
2. The faculty should be qualified. The faculty should be qualified to perform and teach the procedure. Evidence of qualification to perform the procedure should be based on performance data, not simply on clinical experience or reputation. Instead, the faculty members must justify their expert status by indicating their own position on the learning curve. This performance data should include information for both the teaching models used in the course and actual patients. Proof of qualification to teach the procedure should be provided by qualitative and quantitative assessments from prior course participants. Evidence that the learner can actually master the technique during the course should be provided. This should include estimates by past participants of their ability to perform the procedure on patients after having taken the course.
In addition to being qualified, faculty members must be present in sufficient quantity to provide individualized feedback throughout the training period. There is little information to suggest an optimal faculty-to-student ratio, although a ratio of 1:4 has been shown to produce a positive training effect. 31 The precise number could be determined by surveys of participants who assess the adequacy of feedback during the training process.
3. The participants should possess the appropriate fundamental knowledge, skills, and clinical experience. Participants should be surveyed before taking the course regarding their current experience and mastery level so that the course content can be adapted to their specific needs. Pretesting at the beginning of the course is recommended by SAGES and would validate the survey results. Comparison of pretest and posttest performance would provide evidence of the educational effectiveness of the course, as has been done with an ultrasound course for surgeons. 61
4. The facility should be adequate. An adequate number of animate and inanimate models should be available for practice. There should be adequate facilities to accommodate the learning needs of all participants, allowing them to practice until they can demonstrate the desired level of performance based on a position on the learning curve.
5. The curriculum should incorporate educational materials that will reduce the time required at the course and will enhance the learning experience. To enhance the cognitive phase of learning, videotapes of the procedure should be sent to course participants before the course. This would allow them to rehearse the procedure mentally before the actual practice period. 62 The same video files could be digitized and made available to participants to download directly from the Internet. Videotape should also be used to record participant performance during practice to allow learner self-critique and review with a faculty member. 12,63 The participant’s videotapes and those of an expert’s performance should be given to participants for review of the course material as they begin to perform the procedure on patients.
Recommendations for Course Developers and Accrediting Agencies
1. The course developers should perform a formal task analysis. This document describing the task should include an analysis of the important aspects of the technique, including equipment needed and environmental constraints, as has been done for microsurgery. 64 An important aspect of the analysis is an estimate of the degree to which the new technique will represent a new motor skill for participants, because this substantially influences the design of the course. This analysis should also involve an inventory of the errors that occur frequently with the technique. The task analysis leads to the development of specific goals and objectives for the course and a curriculum that allows the participants to accomplish the objectives. The description of the curriculum should include the faculty-to-student ratios, practice environment, and assessment methods.
2. The task analysis and curriculum should be approved by the accrediting agencies. The ultimate goal of accrediting agencies is to ensure that the innovation is introduced with maximal safety to patients. These groups should serve as repositories of information about course elements that must be present to produce effective training. Courses should be evaluated based on performance data during the course and in the participant’s practice.
3. Reevaluate the supervised experience requirement. Even though supervised experience has been shown to be important in reducing complication rates, 39,65 many surgeons are either unable or unwilling to arrange this supervision. 18 Hospitals have shown little interest in requiring this experience, and legitimate difficulties exist when a surgeon is in a rural environment and no other surgeons are available, or when a surgeon is the first in an area to perform a procedure. If it is impossible for a surgeon to arrange a supervised experience, then he or she should bring an assistant or partner to the course, because this has been shown to reduce the incidence of complications during the initial experience. 13
Suggested Directions for Research and Study
More research is needed to increase our understanding of the training needs for practicing surgeons. Improving CMEST is an important way to reduce preventable complications. Having surgeons involved in research designed to improve CMEST should provide evidence to the public that the profession is committed to improving the quality of surgical care by reducing errors. 66,67
1. Evaluate the educational effectiveness of CMEST short courses. The short courses that are currently offered do not provide adequate training in new techniques, but they are an important venue for innovations in patient care. Can this format be improved so that it may be preserved? The learning needs of practicing surgeons must be examined and the educational impact of short courses reviewed. The goal of these courses should be to produce surgeons who can perform a procedure on patients with a minimum of error. The first area of research should be to establish predictive validity between performance on models and performance with patients. If the predictive validity is low, then the courses must be either improved or eliminated. Research is needed on the effective use of computer-based instruction. This instructional tool should allow the simulation of pathologic states that is not possible in animal models. This would reduce the need for animals and might enhance the effectiveness of transferring skills from the course to patients.
2. Develop and evaluate alternative training curricula. It some cases, it may not be possible to teach a technique in a day-long short course. Are the longer alternatives that have been suggested 11,68 effective? Are they practical for practicing surgeons?
3. Determine the feasibility of a training network. It has been argued that CME is an obligation of academic medical centers, 69 and a role for such centers has been suggested specifically for CMEST. 4,70 A review of the past decade of experience with MAS reveals that academic medical centers have been slow to react. As technologic innovations continue to occur, the feasibility of establishing a network of training centers should be explored. Creating this network in academic medical centers would create an excellent opportunity to study the evolving learning needs of practicing surgeons. It would also provide an excellent opportunity for practicing surgeons to have an impact on the training of surgical residents and medical students by providing the perspective of surgeons outside academic medical centers.
4. Determine which attributes of effective CME apply to CMEST. The CME literature has identified many course attributes that will affect physician behaviors and improve patient outcomes. Similar work is needed for CMEST. Some of the lessons learned from general CME would seem applicable to CMEST. For example, it has been shown that there is greater performance change when all participants are from the same practice setting. 19 This is thought to be true because the local environment was enhanced when the course participants returned to their practice setting. This would appear to be true for CMEST as well, because the rate of complications was reduced when the physician brought a partner to the course. 13
5. Investigate ways improve the efficiency of CMEST. Taking time away from a practice creates substantial hardships for surgeons. What is known about producing the most efficient and effective teaching and learning of motor skills learning should be applied to CMEST. For example, it is known that by varying the distribution of practice, it is possible to modify the rate of learning. 33,71 Enhancing the efficiency of learning would shorten the course and reduce the time requirements and costs for participants.
In conclusion, this review of the first decade of MAS experience provides several useful lessons that can be applied to improve CMEST. Perhaps the most powerful lesson is that ample evidence has been generated showing that there is much in common between learning a surgical skill and other motor skills acquisition. This provides the opportunity to improve CMEST by applying what is known of motor skills teaching. Investigation in motor skills learning began a century ago in response to telegraphy, the technologic innovation of that day. 53 In the same way, MAS has drawn attention to technical skills instruction and should provide the impetus for research that will improve CMEST and possibly contribute to the field of motor skills acquisition in general.
Footnotes
Correspondence: David A. Rogers, MD, Department of Surgery, Southern Illinois University School of Medicine, P.O. Box 19655, Springfield, IL 62794-9655. E-mail:drogers@siumed.edu
Accepted for publication July 18, 2000.
References
- 1.Litynski GS. Profiles in laparoscopy: Mouret, Dubois, and Perissat: the laparoscopic breakthrough in Europe (1987–1988). JSLS 1999; 3: 163–167. [PMC free article] [PubMed] [Google Scholar]
- 2.Giurgiu DI, Roslyn JL. Calculous biliary disease. In: Greenfield LJ, ed. Surgery: Scientific Principles and Practice, 2d ed. Philadelphia: Lippincott-Raven; 1997: 1033–1056.
- 3.Sackier JM. Evaluation of technical surgical skills. Lessons from minimal access surgery [editorial]. Surg Endosc 1998; 12: 1109–1110. [DOI] [PubMed] [Google Scholar]
- 4.Cuschieri A. Reflections on surgical training [editorial]. Surg Endosc 1993; 7: 73–74. [DOI] [PubMed] [Google Scholar]
- 5.Dent TL. Training, credentialling, and granting of clinical privileges for laparoscopic general surgery. Am J Surg 1991; 161: 399–403. [DOI] [PubMed] [Google Scholar]
- 6.Gadacz TR, Talamini MA. Traditional versus laparoscopic cholecystectomy. Am J Surg 1991; 161: 336–338. [DOI] [PubMed] [Google Scholar]
- 7.Zucker KA. Training issues [editorial]. Surg Laparosc Endosc 1992; 2: 187. [Google Scholar]
- 8.Rock JA, Warshaw JR. The history and future of operative laparoscopy. Am J Obstet Gynecol 1994; 170: 7–11. [DOI] [PubMed] [Google Scholar]
- 9.Gates EA. New surgical procedures: can our patients benefit while we learn? Am J Obstet Gynecol 1997; 176: 1293–1299. [DOI] [PubMed] [Google Scholar]
- 10.Reznick R. Let’s not forget that CME has an “E.” Foc Surg Ed 1999; 17: 1–2. [Google Scholar]
- 11.Morino M, Festa V, Garrone C. Survey on Torino courses. The impact of a two-day practical course on apprenticeship and diffusion of laparoscopic cholecystecomy in Italy. Surg Endosoc 1995; 9: 46–48. [DOI] [PubMed] [Google Scholar]
- 12.Wright D, O’Dwyer PJ. The learning curve for laparoscopic hernia repair. Semin Laparosc Surg 1998; 5: 227–232. [DOI] [PubMed] [Google Scholar]
- 13.See WA, Cooper CS, Fisher RJ. Predictors of laparoscopic complication after formal training in laparoscopic surgery. JAMA 1993; 270: 2689–2692. [PubMed] [Google Scholar]
- 14.Shackford SR, Rogers FB, Osler TM, et al. Focused abdominal sonogram for trauma: the learning curve for nonradiologist clinicians in detecting hemoperitoneum. J Trauma Inf Crit Care 1999; 46: 553–562. [DOI] [PubMed] [Google Scholar]
- 15.Giuliano AE. See one, do twenty-five, teach one: the implementation of sentinel node dissection in breast cancer. Ann Surg Oncol 1999; 6: 520–521. [DOI] [PubMed] [Google Scholar]
- 16.Framework for Post-Residency Surgical Education and Training. A SAGES Guideline. Available at: http://www.sages.org/sg_pub17.html [DOI] [PubMed]
- 17.Guidelines for Granting of Privileges for Laparoscopic and/or Thoracoscopic General Surgery. Available at: http://www.sages.org/sg_pub14.html [PubMed]
- 18.Escarce JJ, Shea JA, Schwartz JS. How practicing surgeons trained for laparoscopic cholecystecomy. Med Care 1997; 35: 291–296. [DOI] [PubMed] [Google Scholar]
- 19.Umble KE, Cervero RM. Impact studies in continuing education for health professionals. A critique of the research synthesis. Eval Health Prof 1996; 19: 148–174. [DOI] [PubMed] [Google Scholar]
- 20.Davis D, O’Brien MA, Freemantle N, et al. Impact of formal continuing medical education. Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999; 282: 867–874. [DOI] [PubMed] [Google Scholar]
- 21.Lewis CE. Continuing medical education: past, present and future. West J Med 1998; 168: 334–340. [PMC free article] [PubMed] [Google Scholar]
- 22.Barnes RW, Lang NP, Whiteside MF. Halstedian technique revisited. Innovations in teaching surgical skills. Ann Surg 1989; 210: 118–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bevan PG. Craft workshops in surgery. Br J Surg 1986; 73: 1–2. [DOI] [PubMed] [Google Scholar]
- 24.Rosser JC, Jr., Rosser LE, Savalgi RS. Skill acquisition and assessment for laparoscopic surgery. Arch Surg 1997; 132: 200–204. [DOI] [PubMed] [Google Scholar]
- 25.Derossis AM, Fried GM, Abrahamowicz M, et al. Development of a model for training and evaluation of laparoscopic skills. Am J Surg 1998; 175: 482–487. [DOI] [PubMed] [Google Scholar]
- 26.Derossis AM, Bothwell J, Sigman HH, et al. The effect of practice on performance in a laparoscopic simulator. Surg Endosc 1998; 12: 1117–1120. [DOI] [PubMed] [Google Scholar]
- 27.Chung JY, Sackier JM. A method of objectively evaluating improvements in laparoscopic skills. Surg Endosc 1998; 12: 1111–1116. [DOI] [PubMed] [Google Scholar]
- 28.Anastakis DJ, Regehr G, Reznick RK, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 1999; 177: 167–170. [DOI] [PubMed] [Google Scholar]
- 29.Reznick RK. Virtual reality surgical simulators: feasible but valid? [editorial; comment]. J Am Coll Surg 1999; 189: 114–127. [DOI] [PubMed] [Google Scholar]
- 30.Fried GM, Derossis AM, Bothwell J, et al. Comparison of laparoscopic performance in vivo with performance measured in a laparoscopic simulator. Surg Endosc 1999; 13: 1077–1081. [DOI] [PubMed] [Google Scholar]
- 31.Rosser JC, Jr., Rosser LE, Savalgi RS. Objective evaluation of a laparoscopic surgical skill program for residents and senior surgeons. Arch Surg 1998; 133: 657–661. [DOI] [PubMed] [Google Scholar]
- 32.Ericsson KA, Charness N. Expert performance. Its structure and acquisition. Am Psychol 1994; 49: 725–747. [Google Scholar]
- 33.Lane NE. Skill Acquisition Rates and Patterns. Issues and Training Implications. New York: Springer-Verlag; 1987.
- 34.Meehan JJ, Georgeson KE. The learning curve associated with laparoscopic antireflux surgery in infants and children. J Pediatr Surg 1997; 32: 426–429. [DOI] [PubMed] [Google Scholar]
- 35.Southern Surgeons Club, Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. Am J Surg 1995; 170:55–59. [DOI] [PubMed]
- 36.Poulin EC, Mamazza J. Laparoscopic splenectomy: lessons from the learning curve. Can J Surg 1998; 41: 28–36. [PMC free article] [PubMed] [Google Scholar]
- 37.Watson DI, Baigrie RJ, Jamieson GG. A learning curve for laparoscopic fundoplication: definable, avoidable or a waste of time? Ann Surg 1996; 2: 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ford WD, Crameri JA, Holland AJ. The learning curve for laparoscopic pyloromyotomy. J Pediatr Surg 1997; 32: 552–554. [DOI] [PubMed] [Google Scholar]
- 39.Liem MS, van Steensel CJ, Boelhouwer RU, et al. The learning curve for totally extraperitoneal laparoscopic hernia repair. Am J Surg 1996; 171: 281–285. [DOI] [PubMed] [Google Scholar]
- 40.Meinke AK, Kossuth T. What is the learning curve for laparoscopic appendectomy? Surg Endosc 1994; 8: 371–375. [DOI] [PubMed] [Google Scholar]
- 41.Cagir B, Rangraj M, Maffuci L, et al. The learning curve for laparoscopic cholecystecomy. J Laparoendosc Surg 1994; 4: 419–427. [DOI] [PubMed] [Google Scholar]
- 42.Hawasli A, Lloyd LR. Laparoscopic cholecystectomy. The learning curve: report of 50 patients. Am Surg 1991; 57: 542–544. [PubMed] [Google Scholar]
- 43.Rege RV, Joehl RJ. A learning curve for laparoscopic splenectomy at an academic institution. J Surg Res 1999; 81: 27–32. [DOI] [PubMed] [Google Scholar]
- 44.Lekawa M, Shaprio SJ, Gordan LA, et al. The laparoscopic learning curve. Surg Lapar Endosc 1995; 5: 455–458. [PubMed] [Google Scholar]
- 45.Wishner JD, Baker JW, Hoffman GC, et al. Laparoscopic-assisted colectomy: the learning curve. Surg Endosc 1995; 9: 1179–1183. [DOI] [PubMed] [Google Scholar]
- 46.Hunter JG, Sackier JM, Berci G. Training in laparoscopic cholecystectomy: quantifying the learning curve. Surg Endosc 1994; 8: 28–31. [DOI] [PubMed] [Google Scholar]
- 47.Soot SJ, Eshraghi N, Farahmand M, et al. Transition from open to laparoscopic fundoplication: the learning curve. Arch Surg 1999; 134: 278–281. [DOI] [PubMed] [Google Scholar]
- 48.Magill RA. Motor Learning Concepts and Applications, 4th ed. Indianapolis: WCB Brown and Benchmark; 1993.
- 49.Schmidt RA. Motor Learning and Performance: From Principles to Practice. Champaign, IL: Human Kinetics Books; 1991.
- 50.Ohlsson S. Learning from performance errors. Psychol Rev 1996; 103: 241–246. [Google Scholar]
- 51.Dewey J. Psychology and social practice. Psychol Rev 1900; 7: 105–124. [DOI] [PubMed] [Google Scholar]
- 52.Barnes RW. Surgical handicraft: teaching and learning surgical skills. Am J Surg 1987; 153: 422–427. [DOI] [PubMed] [Google Scholar]
- 53.Adams JA. Historical review and appraisal of research on the learning, retention, and transfer of human motor skills. Psychol Bull 1987; 101: 41–74. [Google Scholar]
- 54.Dul J, Pieters JM, Dijkstra S. Instructional feedback in motor skill learning. PLET 1987; 24: 71–76. [Google Scholar]
- 55.Fitts AM, Posner MI. Human Performance. Belmont, CA: Brooks-Cole; 1967.
- 56.Kopta JA. An approach to the evaluation of operative skills. Surgery 1971; 70: 297–303. [PubMed] [Google Scholar]
- 57.Kaufman HH, Wiegand RL, Tunick RH. Teaching surgeons to operate: principles of psychomotor skills training. Act Neurochir 1987; 87: 1–7. [DOI] [PubMed] [Google Scholar]
- 58.Weeks DL, Sherwood DE. A comparison of knowledge of results scheduling methods for promoting motor skill acquisition and retention. RQES 1994; 2: 136–142. [DOI] [PubMed] [Google Scholar]
- 59.Wulf G, Shea CH, Matschiner S. Frequent feedback enhances complex motor skill learning. J Mot Beh 1998; 30: 180–192. [DOI] [PubMed] [Google Scholar]
- 60.Royston CM, Lansdown MR, Brough WA. Teaching laparoscopic surgery: the need for guidelines. Br Med J 1994; 308: 1023–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ali J, Rozycki GS, Campbell JP, et al. Trauma ultrasound workshop improves physician detection of peritoneal and pericardial fluid. J Surg Res 1996; 63: 275–279 [DOI] [PubMed] [Google Scholar]
- 62.DesCoteaux J, Leclere H. Learning surgical technical skills. Can J Surg 1995; 38: 33–38. [PubMed] [Google Scholar]
- 63.Kardash K, Tessler MJ. Videotape feedback in teaching laryngoscopy. Can J Anaesth 1997; 44: 54–58. [DOI] [PubMed] [Google Scholar]
- 64.Starkes JL, Payk I, Jennen P, et al. A stitch in time: cognitive issues in microsurgery. In: Starkes JL, Allard F, eds. Cognitive Issues in Motor Expertise. New York: North-Holland; 1993: 225–240.
- 65.Yamashita Y, Kuorhigi T, Kakegawa T. Evaluation of two training programs for laparoscopic cholecystecomy: incidence of major complications. World J Surg 1994; 18: 279–285. [DOI] [PubMed] [Google Scholar]
- 66.Chassin MR, Galvin RW. The urgent need to improve health care quality: Institute of Medicine national roundtable on health care quality. JAMA 1998; 280: 1000–1005. [DOI] [PubMed] [Google Scholar]
- 67.Concerning patient safety and medical errors: Hearings before the Subcommittee on Labor, Health, and Human Services and Education Committee on Appropriations, 106th Congress, First Session (Dec. 13, 1999). Available at: http://www4.nas.edu/ocga/testimon.nsf/ByTopic/9cca3ad200c16e1e852568460075269f?OpenDocument
- 68.McKernan JB, Saye W. Laparoscopic general surgery. J Med Assoc Ga 1990; 79: 157–159. [PubMed] [Google Scholar]
- 69.Davis D, Parboosingh J. “Academic” CME and the social contract. Acad Med 1993; 68: 329–332. [DOI] [PubMed] [Google Scholar]
- 70.Mansberger AR Jr. Personal thoughts on laparoscopic general surgery. J Med Assoc Ga 1990; 79: 148. [PubMed] [Google Scholar]
- 71.Snoddy GS. Learning and stability. J Appl Psychol 1926; 10: 1–36. [Google Scholar]


