Abstract
Objective
To compare the incidence of biliary complications after liver transplantation in patients undergoing choledochocholedochostomy reconstruction with or without T tube in a multicenter, prospective, randomized trial.
Summary Background Data
Several reports have suggested that biliary anastomosis without a T tube is a safe method of biliary reconstruction that could avoid complications related to the use of T tubes. No large prospective randomized trial has so far been published to compare the two techniques.
Methods
One hundred eighty recipients of orthotopic liver transplantation were randomly assigned to choledochocholedochostomy with (n = 90) or without (n = 90) a T tube in six French liver transplantation centers. All types of biliary complications were taken into account.
Results
The overall biliary complication rate was increased in the T-tube group, even though these complications did not lead to an increase in surgical or radiologic therapeutic procedures. The major significant complication was cholangitis in the T-tube group; this did not occur in the other group. The incidence of biliary fistula was 10% in the T-tube group and 2.2% in the group without a T tube. Other biliary complications were similar. The complication rate of cholangiography performed with the T tube was greater than with other types of biliary exploration. The graft and patient survival rates were similar in the two groups.
Conclusion
This study is the first large prospective, randomized trial of biliary complications with or without a T tube. The authors found an increase in the biliary complication rate in the T-tube group, which was linked to minor complications. The T tube did not provide a safer access to the biliary tree compared with the others types of biliary explorations. The authors recommend the performance of choledochocholedochostomy without a T tube in liver transplantation.
Biliary tract reconstruction is the final step of orthotopic liver transplantation (OLT) and can be carried out according to two main techniques. The first one, end-to-end or side-to-side choledochocholedochostomy (CCS), is rapid, simple, and physiologic. The second one, hepaticojejunostomy, is used when the former is not feasible for anatomical reasons or for causes related to the underlying hepatobiliary disease. Usually, CCS is done over a T tube. The use of this stent allows monitoring of bile flow and color and easy performance of cholangiography. Moreover, the presence of a T tube may protect against anastomotic strictures. 1 However, the presence of a T tube may also lead to specific complications, which account for 30% to 50% of the overall biliary complications. 2,3 These complications include bile leakage around the T tube, cholangitis after cholangiography, bile duct obstruction, displacement of the T tube, and biliary peritonitis after T tube removal. The disadvantages associated with the use of a T tube led several authors to perform CCS without a T tube. 4–6 This technique was not associated with an increased level of complications. The aim of the present randomized study was to compare the incidence of biliary complications after CCS performed with or without a T tube in OLT.
METHODS
Between January 1994 and April 1997, 180 OLT recipients were randomly assigned to CCS with a T tube or CCS without a T tube in six French liver transplantation centers. The trial protocol was approved by the committee for patient protection for biomedical research of Paris-Cochin. All patients were informed in detail about the procedure and gave their written consent according to French law. Based on the results of previous studies and personal data, we assumed a global incidence of biliary complications of 30% after CCS with a T tube. All types of complications were taken into account, including life-threatening problems as well as minor incidents. To detect a 50% reduction with a type 1 error rate of 5% and a type 2 error rate of 20%, a sample size of 95 patients per group was calculated.
Inclusion criteria were patients receiving a primary liver transplant, age older than 18 years, and CCS feasible with well-vascularized bile ducts coming easily end to end. Exclusion criteria were age younger than 18 years, retransplantation, transplantation of a reduced-size or split graft, or abnormal bile duct or pancreas head in the recipient.
Protocol
Liver harvesting was performed using standard techniques, and University of Wisconsin solution was used for organ preservation. Bile ducts were washed abundantly during organ harvesting. OLT was performing using either the standard technique, with or without venovenous bypass, or the piggyback technique. The random assignment was done after hepatic artery anastomosis, when CCS appeared clearly feasible. Random assignment was made with the use of a computer-generated randomization schedule with blocks of six randomly assigned numbers. In each block, three patients were assigned to the group of CCS with a T tube and three patients were assigned to the group of CCS without a T tube. CCS was performed end to end with interrupted polydioxanone sutures. Rubber T tubes were used and were introduced through the recipient’s bile duct. The superior part of the horizontal branch stented both the anastomosis and graft bile duct. Routine cholangiography was performed at the end of surgery. During the postoperative period, the T tube was clamped when possible between days 7 and 14, after cholangiography. T-tube removal was scheduled 90 days after OLT. The primary endpoint was the time from randomization to the diagnosis of a biliary complication, irrespective of its type. Survival was defined as the time from randomization to death resulting from any cause.
Statistical Analysis
Data were analyzed on an intent-to-treat basis. Quantitative variables are presented as means with standard deviation or medians. Comparisons of data were performed with the Fisher exact probability test and the Mann-Whitney test, where appropriate. The probability of being free of a biliary complication and probabilities of survival of patient, liver graft, or biliary anastomosis were estimated by the Kaplan-Meier method. Survival rates were compared between the two groups using the log-rank test. The delays between randomization and the occurrence of a biliary complication were compared with the Cox proportional hazards model, with the treatment assignment as the only factor. All significance tests were two-sided.
RESULTS
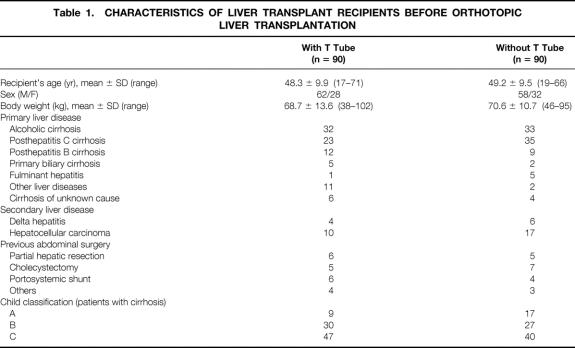
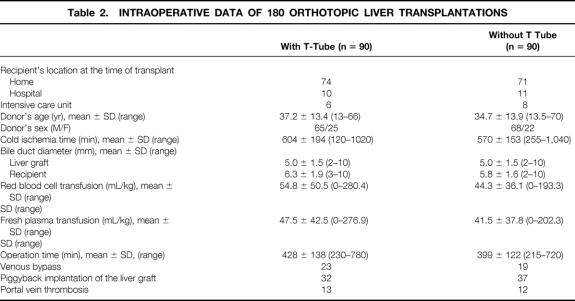
One hundred eighty patients were randomized to undergo CCS with or without a T tube. The number of patients in each center was Rennes (n = 42), Paris (n = 31), Créteil (n = 30), Lyon (n = 27), Strasbourg (n = 26), and Clichy (n = 24). In one patient assigned to the T-tube group, CCS was found to be not feasible and hepaticojejunostomy was preferred; however, the patient was kept in the data analysis. The mean follow-up was 21.5 ± 7.0 months in the T-tube group and 21.3 ± 7.4 months in the group without T tube. Baseline demographic characteristics and disease-related data were similar in the two groups (Table 1). There was no difference in intraoperative data between the groups (Table 2).
Table 1. CHARACTERISTICS OF LIVER TRANSPLANT RECIPIENTS BEFORE ORTHOTOPIC LIVER TRANSPLANTATION
Table 2. INTRAOPERATIVE DATA OF 180 ORTHOTOPIC LIVER TRANSPLANTATIONS
Biliary Complications and Survival of Anastomosis
The overall biliary complication rate was 33.3% in the T-tube group and 15.5% in the group without a T tube (P < .005). In the T-tube group, the estimated hazard ratio was 1.96 (95% confidence interval, 1.22–3.17;P < .005). Biliary event-free survival curves are given in Figure 1, showing a significant difference between the two groups. The types of biliary complications in both groups are detailed in Table 3.
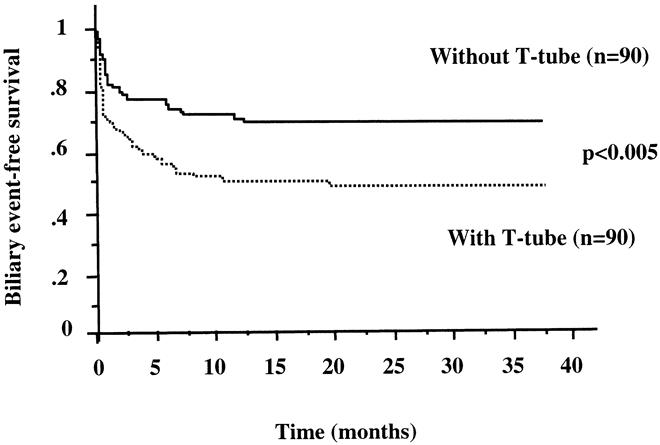
Figure 1. Biliary event-free survival in liver transplant recipients according to the presence or absence of a T tube.
Table 3. BILIARY COMPLICATIONS
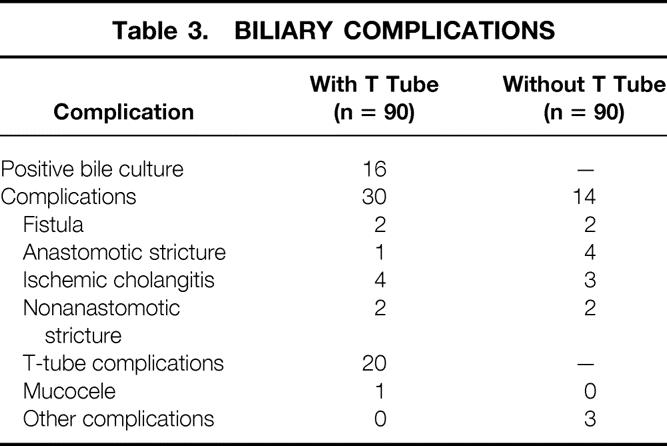
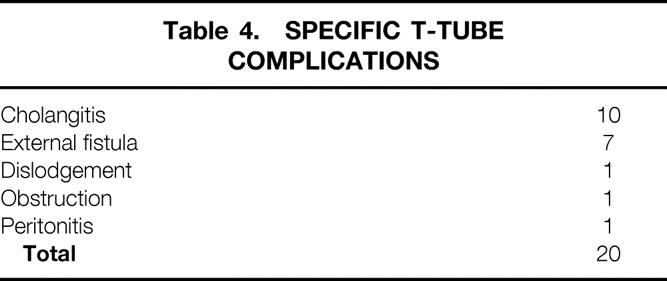
In the T-tube group, 60% of the complications were directly related to the presence of the T tube (Table 4). Cholangitis after cholangiography was the most frequent complication (11.1%) in the T-tube group despite the use of prophylactic antibiotics. The rate of positive bile culture in the T-tube group was 17.7%; in contrast, cholangitis never occurred in the group without a T tube. The second most frequent complication encountered after biliary T-tube anastomosis was bile leakage (10%), which occurred in only 2.2% in the group without a T tube. In the T-tube group, 78% of these fistulas were located at the exit site of the T tube and appeared after removal. Only two intraperitoneal biliary fistulas occurred in each group. The occurrence of early and late strictures did not differ significantly between the two groups (three in the T-tube group, six in the group without a T tube).
Table 4. SPECIFIC T-TUBE COMPLICATIONS
The survival of the biliary anastomosis was also evaluated in the two groups when only major complications requiring invasive therapeutic procedures were considered: no significant difference in biliary anastomosis survival was observed in these conditions (3-year actuarial survival of 62.5% in the T-tube group and 69.8% in the group without a T tube). In the T-tube group, biliary complications generally occurred in the first 2 months after liver transplantation (median delay, day 38); in the group without a T tube, the median delay was 111 days.
Diagnosis and Treatment of Complications
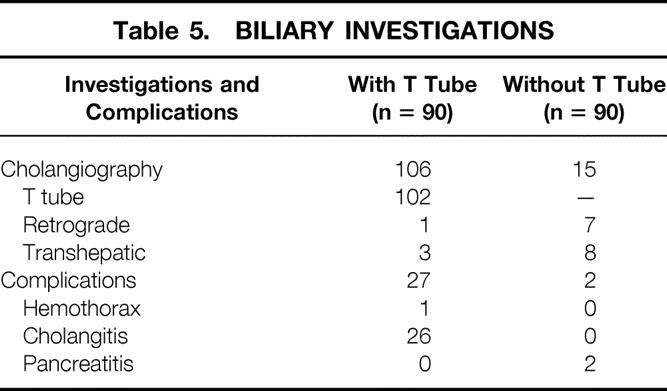
The types of investigations performed and their complications are detailed in Table 5. In the group without a T tube, seven endoscopic retrograde cholangiopancreatographies (ERCPs) and eight percutaneous transhepatic cholangiography (PTCs) were undertaken (16.6%). The overall complication rate was 13%. Pancreatitis was the only underlying cause in this group. In the T-tube group, one ERCP and three PTCs were performed; there was only one complication (hemothorax). Ten of the 90 patients who underwent T-tube cholangiography had cholangitis (11.1%) despite the use of prophylactic antibiotics. Of these patients, half had a positive bile culture before cholangiography. No patient died of biliary tract radiologic exploration in either group. Complications associated with cholangiography through the T tube was more important than ERCP and PTC (P < .005).
Table 5. BILIARY INVESTIGATIONS
Although the biliary complication rate was greater in the T-tube group, there was no increase in the number of patients needing therapeutic procedures. Seven patients required hepaticojejunostomy conversion in the group with a T tube (7.7%), compared with eight in the group without a T tube (8.8%). In the T-tube group, two patients had an internal stent and one had a retrograde dilatation of a biliary stricture. In the group without a T tube, one had an internal stent and three had a dilatation. No patient died of radiologic or endoscopic interventions in the two groups.
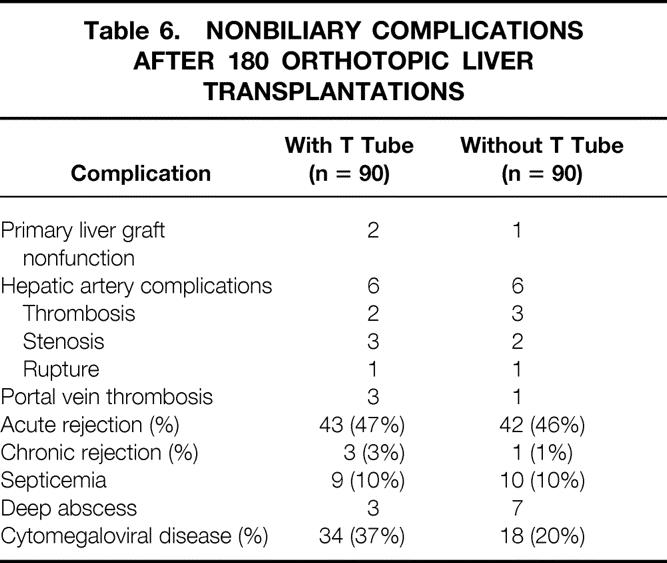
Nonbiliary complications were similar in the two groups (Table 6).
Table 6. NONBILIARY COMPLICATIONS AFTER 180 ORTHOTOPIC LIVER TRANSPLANTATIONS
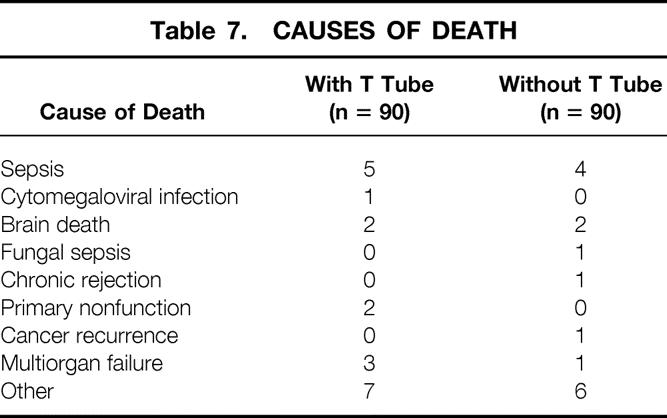
Patient Survival and Graft Loss
The cumulative 3-year patient survival rate was 72.8% in the T-tube group and 80.1% in the group without a T tube; this difference was not significant. One patient died of septic shock after T-tube removal with rupture of a branch of the horizontal part, which remained in the bile duct. The patient underwent immediately reoperation but died in the early postoperative period. The death rate directly related to the use of a T tube was thus 1.1%. The causes of death are detailed in Table 7.
Table 7. CAUSES OF DEATH
The graft survival rate was similar in the two groups (Fig. 2). There were four retransplantations in the T-tube group (4.4%) and three in the group without a T tube (3.3%). In the T-tube group, rejection and virus recurrence were the two causes of retransplantation. In the group without a T tube, primary liver graft nonfunction, arterial thrombosis, and ischemic cholangitis were the main causes of retransplantation.
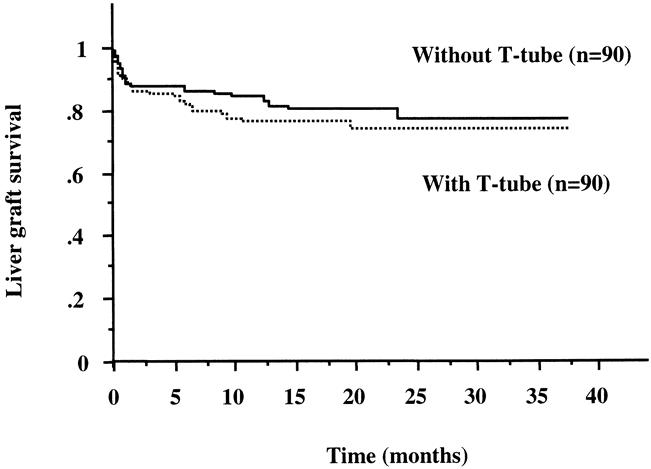
Figure 2. Liver graft survival according to the presence or absence of a T tube.
DISCUSSION
The duct-to-duct anastomosis, stented or not with a T tube, has become the most widely accepted technique of biliary reconstruction. T-tube drainage allows easy radiologic access to the biliary tree and monitoring of the quality of biliary flow. It may decrease the anastomotic stricture rate and lead to biliary decompression. 1 However, the incidence of biliary complications with a T tube is high, ranging from 10% to 50% in large clinical series. 3 Half of these biliary complications seems directly related to the presence of the T tube. 4 Because of the disadvantages associated with the use of a T tube, several authors 4–8 have advocated nonsplinted biliary duct reconstruction.
Our results from a large randomized prospective trial fully support this view. We found a marked increase in the overall rate of biliary complications in the T-tube group versus the nonsplinted group. More than half (60%) of the overall biliary complications were found to be related to the use of the T tube. However, this increased complication rate in the T-tube group involved only minor complications and did not lead to an increase in the number of invasive therapeutic procedures. Moreover, the survival of the biliary anastomosis was similar in both groups, when major complications leading to reintervention were taken into account.
The two main complications associated with biliary reconstruction are anastomotic stricture and internal leakage. In our study, the latter complications were found to be independent of the presence of a T tube. Three retrospective studies 4–6 and one small prospective randomized trial 9 are in line with our findings concerning stricture and leakage rates. Early and late biliary complications were found to be similar irrespective of the biliary reconstruction technique used (stented or not). In contrast to these and our present results, one previous prospective study reported a higher biliary complication rate and an increase in the number of reinterventions when no T tube was used. 10 However, the number of patients in this study was relatively low and inadequate to allow firm conclusions to be drawn regarding the incidence of biliary complications. Overall, CCS without a T tube appears to be a safe and effective technique of biliary reconstruction.
Another important finding of our study is that the use of a T tube is directly related to an increased risk of infection, leakage at the exit site of the T tube, dislodgment, and obstruction. The biliary infection rate in the splinted anastomosis was 11%. In our experience, cholangiography using T tubes was the major cause of biliary infection, but results of a bile culture were not obtained for a controlled comparison. Given that the T tube provides easy access to the biliary tree, cholangiography tends to become a routine procedure, thus causing cholangitis despite the prophylactic use of antibiotics. In support of our findings, a recent study also showed that the infection rate is significantly increased in the T-tube group versus the nonsplinted group (40% vs. 1.7%). 11
Ten percent of the patients who underwent splinted anastomosis developed a fistula. These fistulas did not require reintervention. Our incidence of fistula is lower than that reported by others in two retrospective studies (18.3% and 33%). 12,13 In contrast to our patients, most of the patients of the latter studies underwent surgical treatment. 14 Immunosuppression and the underlying disease are likely responsible for the delay in the formation of a fibrous tract between the biliary duct and the skin after T-tube removal. The demonstrated increase in biliary pressure 15 may be a contributing factor to fistula development.
A potential advantage of CCS with a T tube is the direct access afforded to the biliary tree, which facilitates diagnostic investigations. Nonetheless, in our study, complications from ERCP and PHC were not more important than those associated with T-tube cholangiography. Thus, diagnostic and interventional radiologic access to the biliary tree by percutaneous or endoscopic routes is safe. In addition, the use of a T tube is not of benefit in late biliary complications. In the study by Randall et al, 5 the need for percutaneous investigations and endoscopic retrograde cholangiography was even more common in the T-tube group.
Several studies have shown that endoscopic retrograde access and percutaneous access not only are useful and reliable methods for diagnosis but can also be safely used for dilatation and stenting. 6,16–20 Strictures can be safely managed by nonsurgical methods. Stenting and dilatation are two effective interventional approaches that could offer low-risk alternatives to reoperation. Our patients with biliary strictures treated by endoscopic or radiologic interventions did not experience any complication or death. Overall, the rates of death and graft loss were not modified by the presence of a T tube, if we except one patient who died of sepsis directly related to the use of a T tube. Causes of retransplantation were not related to biliary complications.
In conclusion, this study is the first large prospective randomized trial of biliary complications after CCS with and without a T tube. We found more disadvantages than advantages to the use of a T tube. In fact, T-tube use was associated with an increased incidence of minor complications such as bile infection, cholangitis, and fistula, which nevertheless did not increase the number of invasive therapeutic procedures. Access to the biliary tree with a T tube is no longer a justification for its use, given the existence of safe and effective procedures of biliary exploration (percutaneous or endoscopic). Therefore, we recommend performing CCS without a T tube.
Footnotes
Supported by a grant from the Assistance Publique/Hôpitaux de Paris and the French Ministère de la Santé.
Correspondence: Prof. Olivier Soubrane, MD, Service de Chirurgie, Hôpital Cochin, 27 rue du Faubourg Saint-Jacques, 75679 Paris Cedex 14 France.
E-mail: olivier.soubrane@cch.ap-hop-paris.fr
Accepted for publication July 18, 2000.
References
- 1.Shaked A. Use of T-tube in liver transplantation. Liver Transpl Surg 1997; 3 (5 suppl 1):22–23. [PubMed] [Google Scholar]
- 2.Stratta RJ, Wood RP, Langnas AN, et al. Diagnosis and treatment of biliary tract complications after orthotopic liver transplantation. Surgery 1989; 106: 675–684. [PubMed] [Google Scholar]
- 3.Vallera RA, Cotton PB, Clavien PA. Biliary reconstruction for liver transplantation and management of biliary complications: overview and survey of current practices in the United States. Liver Transpl Surg 1995; 1 (3): 143–152. [DOI] [PubMed] [Google Scholar]
- 4.Rouch DA, Emond JC, Thistlethwaite JR Jr, et al. Choledochocholedochostomy without a T-tube or internal stent in transplantation of the liver. Surg Gynecol Obstet 1990; 170: 239–244. [PubMed] [Google Scholar]
- 5.Randall HB, Wachs ME, Somberg KA, et al. The use of the T tube after orthotopic liver transplantation. Transplantation 1996; 61: 258–261. [DOI] [PubMed] [Google Scholar]
- 6.Rolles K, Dawson K, Novell R, et al. Biliary anastomosis after liver transplantation does not benefit from T-tube splintage. Transplantation 1994; 57: 402–404. [DOI] [PubMed] [Google Scholar]
- 7.Lopez RR, Benner KG, Avancev K, et al. Management of biliary complications after liver transplantation. Am J Surg 1992; 163: 519–524. [DOI] [PubMed] [Google Scholar]
- 8.Roberts JP. T tube or not T tube? Liver Transpl Surg 1997; 3: S20–21. [PubMed] [Google Scholar]
- 9.Vougas V, Rela M, Gane E, et al. A prospective randomised trial of bile duct reconstruction at liver transplantation: T tube or not T tube? Transplant Int 1996; 9: 392–395. [DOI] [PubMed] [Google Scholar]
- 10.Nuno J, Vicente E, Turrion VS, et al. Biliary tract reconstruction after liver transplantation: with or without T tube? Transplant Proc 1997; 29: 564–565. [DOI] [PubMed] [Google Scholar]
- 11.Ben Ari Z, Neville L, Davidson B, et al. Infection rates with or without T-tube splintage of common bile duct anastomosis in liver transplantation. Transplant Int 1998; 11: 123–126. [DOI] [PubMed] [Google Scholar]
- 12.Greif F, Bronsther OL, Van Thiel, et al. The incidence, timing, and management of biliary tract complications after orthotopic liver transplantation. Ann Surg 1994; 219: 40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shuhart MC, Kowdley KV, McVicar JP, et al. Preditors of bile leaks after T-tube removal in orthotopic liver transplant recipients. Liver Transplant Surg 1998; 4: 62–70. [DOI] [PubMed] [Google Scholar]
- 14.Tepetes K, Karavias D, Felekouras E, et al. Bile leakage following T-tube removal in orthotopic liver transplantation. Hepato-Gastroenterology 1999; 46: 425–427. [PubMed] [Google Scholar]
- 15.Thune A, Friman S, Persson H, et al. Raised pressure in the bile ducts after orthotopic liver transplantation. Transplant Int 1994; 7: 243–246. [DOI] [PubMed] [Google Scholar]
- 16.Macfarlane B, Davidson BR, Dooley JS, et al. Endoscopic retrograde cholangiography in the diagnosis and endoscopic management of biliary complications after liver transplantation. Eur J Gastroenterol Hepatol 1996; 8: 1003–1006. [DOI] [PubMed] [Google Scholar]
- 17.Gholson CF, Zibari G, McDonald JC. Endoscopic diagnosis and management of biliary complications following orthotopic liver transplantation. Dig Dis Sci 1996; 41: 1045–1053. [DOI] [PubMed] [Google Scholar]
- 18.Bourgeois N, Deviere J, Yeaton P, et al. Diagnostic and therapeutic endoscopic retrograde cholangiography after liver transplantation. Gastrointest Endosc 1995; 42: 527–534. [DOI] [PubMed] [Google Scholar]
- 19.Sherman S, Jamidar P, Shaked A, et al. Biliary tract complications after orthotopic liver transplantation. Endoscopic approach to diagnosis and therapy. Transplantation 1995; 60: 467–470. [DOI] [PubMed] [Google Scholar]
- 20.Klein AS, Savader S, Burdick JF, et al. Reduction of morbidity and mortality from biliary complications after liver transplantation. Hepatology 1991; 14: 818–823. [DOI] [PubMed] [Google Scholar]