Abstract
Objective
To study mortality after appendectomy.
Summary Background Data
The management of patients with suspected appendicitis remains controversial, with advocates of early surgery as well as of expectant management. Mortality is not known.
Methods
The authors conducted a complete follow-up of deaths within 30 days after all appendectomies in Sweden (population 8.9 million) during the years 1987 to 1996 (n = 117,424) by register linkage. The case fatality rate (CFR) and the standardized mortality ratio (SMR) were analyzed by discharge diagnosis.
Results
The CFR was 2.44 per 1,000 appendectomies. It was strongly related to age (0.31 per 1,000 appendectomies at 0–9 years of age, decreasing to 0.07 at 20–29 years, and reaching 164 among nonagenarians) and diagnosis at surgery (0.8 per 1,000 appendectomies after nonperforated appendicitis, 5.1 after perforated appendicitis, 1.9 after appendectomies for nonsurgical abdominal pain, and 10.0 for those with other diagnoses).
The SMR showed a sevenfold excess rate of deaths after appendectomy compared with the general population. The relation to age was less marked (SMR of 44.4 at 0–9 years, decreasing to 2.4 in patients aged 20–29 years. and reaching 8.1 in nonagenarians). The SMR was doubled after perforation compared with nonperforated appendicitis (6.5 and 3.5, respectively). Nonsurgical abdominal pain and other diagnoses were associated with a high excess rate of deaths (9.1 and 14.9, respectively). The most common causes of deaths were appendicitis, ischemic heart diseases and tumors, followed by gastrointestinal diseases.
Conclusions
The CFR after appendectomy is high in elderly patients. The excess rate of death for patients with nonperforated appendicitis and nonsurgical abdominal pain suggests that the deaths may partly be caused by the surgical trauma. Increased diagnostic efforts rather than urgent appendectomy are therefore warranted among frail patients with an equivocal diagnosis of appendicitis.
Acute appendicitis is one of the most common abdominal emergencies in the industrialized world. Suspected appendicitis remains a diagnostic challenge because of the similarity of symptoms to other gastrointestinal, gynecologic, and nonspecific functional diseases. Recent aids to improve the diagnostic workup, such as ultrasound, computed tomography, and diagnostic scoring systems, have not gained wide acceptance. 1–4
The preferred management of patients with suspected appendicitis has been clinical assessment and a liberal attitude to early surgical exploration, with a subsequently high proportion of surgical procedures where the appendix is unaffected. 5,6 A proportion of negative appendectomies of 20% to 25% has been considered an acceptable level. 7 One reason for this policy has been the increased rates of death and complications after perforation, and the notion that early surgery could prevent perforation. This assumption has not been supported: most perforations probably have occurred by the time the patient arrives at the hospital, and the rate of exploration has not been found to have any influence on the incidence of perforation. 8–11 There are indications that spontaneous resolution occurs more frequently than is commonly thought, and recent studies have shown smaller differences than expected in the long-term complication rate among patients with perforated appendicitis versus those with nonperforated appendicitis. 11,12
The death and complication rates after perforated appendicitis have decreased over the years as a result of improved perioperative routines and postoperative care, including treatment with antibiotics. Parallel to the decrease in the death rate has been a decreasing rate of appendectomies, indicating a more conservative attitude to early surgical exploration. 11,13
The aims of this study are to analyze the case-fatality rate (CFR), the standardized mortality ratio (SMR), and causes of death among patients undergoing appendectomy in Sweden during a 10-year period, and to analyze the association with age, gender, and the underlying cause of the abdominal pain.
METHODS
Setting
Sweden (population 8.9 million) has a national healthcare system based on administratively independent county councils. The private hospital sector is small and provides only elective care. Healthcare is mainly funded by local taxes. Since 1964, the Swedish National Board of Health and Welfare has compiled data on individual hospital discharges in the National Inpatient Register, and since 1987 the register has covered all Swedish hospitals. Besides a national registration number (uniquely identifying every resident of Sweden), each record contains medical data including surgical procedures performed (coded according to the Swedish Classification of Operations and Major Procedures, sixth edition) and diagnoses at discharge (coded according to Swedish version of the International Classification of Diseases, ninth Revision [ICD9] during 1987–1996).
Patients
All patients discharged during the years 1987 through November 1996 with a procedure code of appendectomy, performed as open surgery or by laparoscopy (procedure codes 4510, 4511, and 4517), were identified in the National Inpatient Register. Perforated appendicitis was defined as patients having an ICD9 discharge diagnosis of 540A (acute appendicitis with perforation or rupture) or 540B (acute appendicitis with peritoneal abscess). Nonperforated appendicitis was defined as patients having an ICD9 diagnosis of 540X (acute appendicitis without peritonitis), 541 (appendicitis, not specified), or 542 (appendicitis, otherwise not specified). In this study all diagnoses 289C (mesenterial lymphadenitis) and 789A (abdominal pain) were categorized as nonsurgical abdominal pain (NSAP). All other diagnoses were categorized as “other.”
All postoperative deaths were analyzed by linking information on date of death and underlying cause of death through 1996 from the Swedish Death Register to the National Inpatient Register, using the personal identification number. Date of surgery was not recorded in the National Inpatient Register during this study period. Therefore, the time between surgery and death was calculated as the difference between the date of admission and the date of death, assuming that the patient had undergone surgery immediately after admission. Underlying causes of death were coded by the ICD9 classification. To enable a minimum follow-up of 30 days after admission, only patients undergoing surgery between January 1, 1987, and November 30, 1996, were included.
Data Analysis
Descriptive analyses of the characteristics of all patients undergoing surgery and of the fatal cases to and including 30 days after admission were performed, considering age, gender, discharge diagnoses, underlying causes of death, and time of death after admission. CFR per 1,000 appendectomies was computed by categories of discharge diagnosis and age. The 30-day standardized mortality ratio (SMR) was calculated using age-, calendar year-, and sex-specific expected survival estimates from the Swedish population. Ninety-five percent confidence intervals (CI) were calculated assuming a Poisson-distributed number of events. 14
Multivariate analyses of the SMR patterns as a function of age, diagnosis group, sex, and calendar period were performed by Poisson regression using SAS software. 15 The statistical significance of influential factors and interactions was assessed by likelihood ratio tests.
RESULTS
Basic Data
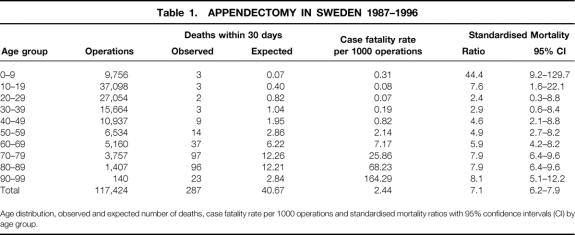
The study cohort consisted of 117,424 patients (Table 1). The median age at surgery was 23 years (quartile range 15–38), and the gender distribution was almost even (male patients 50.7% vs. female patients 49.3%). Four fifths of the patients (80.9%) had a discharge diagnosis of appendicitis, 11.9% had NSAP (nonspecific abdominal pain or lymphadenitis), and the remaining 6.8% had a wide range of other diagnoses. The proportion of appendicitis patients with perforation was 20.2%. Most procedures were conventional appendectomies: only 2.0% of the appendectomies were performed by laparoscopy, increasing from 0.01% in 1986 to 7.6% in 1996. The annual incidence of appendectomies decreased by 17.5% during the study period. The decrease was confined to patients between 20 and 29 years (37%) and 30 to 39 years (23%), and to the patients with nonperforated appendicitis (9%) and negative appendectomy (48%). The incidence of perforated appendicitis remained stable.
Table 1. APPENDECTOMY IN SWEDEN 1987–1996
Age distribution, observed and expected number of deaths, case fatality rate per 1000 operations and standardised mortality ratios with 95% confidence intervals (CI) by age group.
During the study period, 287 of the patients died within 30 days after admission for a CFR of 2.44. For the patients with a final diagnosis of appendicitis, the CFR was 1.63, or 0.2 per 100,000 population and year during the study period. The median age of those who died was 77.0 years (quartile range 69–84). Slightly more than a third of the patients died during the first 7 days (40.0%), and two thirds died within the first 2 weeks (68.3%). Most patients died in the hospital during the same admission as when the surgery was performed (68.4%).
Case Fatality Rate
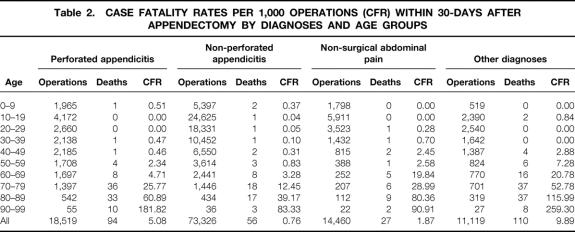
The CFR was strongly influenced by patient age, forming a J-shaped curve (Tables 1 and 2). For those 9 years of age or younger, the CFR was 0.31. It was 0.07 for patients 20 to 29 years of age. From age 40 to 49 years, an almost threefold increase was found for each decade of age, reaching more than 16% in the nonagenarians. Gender had only a marginal influence on CFR (2.2 in female patients vs. 2.7 in male patients).
Table 2. CASE FATALITY RATES PER 1,000 OPERATIONS (CFR) WITHIN 30-DAYS AFTER APPENDECTOMY BY DIAGNOSES AND AGE GROUPS
Patients with nonperforated appendicitis had the lowest CFR (0.76). Perforated appendicitis increased the rate six times to 5.08 (see Table 2). However, the difference between perforated and nonperforated appendicitis was only roughly doubled when analyzed by age interval. Patients with NSAP had a CFR of 1.87; those with other diagnoses had the highest CFR of all, 9.89.
Standardized Mortality Ratio
The SMR showed a sevenfold rate of excess deaths within 30 days after appendectomy compared with the general population (see Table 1). The relation to age was less marked than for CFR. Despite the few deaths in children younger than 10 years of age, the SMR reached 44.4 (95% CI 9.2–129.7) because of the low number of expected deaths. Patients aged 20 to 29 years had the lowest rate of excess deaths (SMR 2.4, 95% CI 0.3–8.8).
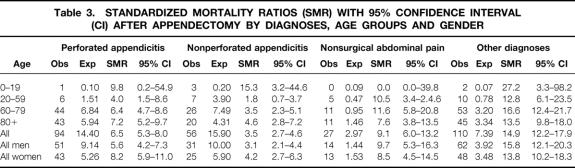
The multivariate analysis showed a significantly higher death rate for patients with perforated appendicitis versus nonperforated appendicitis, with an SMR of 1.73 (95% CI 1.24–2.43) (P = .001). There was a significant U-shaped relation with age (P = .02): SMRs relative to the age group 80+ years as follows (with 95% CI): 60 to 79 years, 0.88 (0.62–1.24); 20 to 59 years, 0.49 (0.27–0.90); and 0 to 19 years, 2.79 (1.00–7.73).
Table 3. STANDARDIZED MORTALITY RATIOS (SMR) WITH 95% CONFIDENCE INTERVAL (CI) AFTER APPENDECTOMY BY DIAGNOSES, AGE GROUPS AND GENDER
For NSAP and other diagnoses, the risk was increased in all age intervals, with an almost 9-fold excess rate of deaths for NSAP and a 15-fold excess rate for other diagnoses. There was a significantly higher SMR for female patients than for male patients, with an SMR of 1.39 (95% CI 1.00–1.92) (P = .05). No difference between the periods 1987 to 1991 and 1992 to 1996 was found.
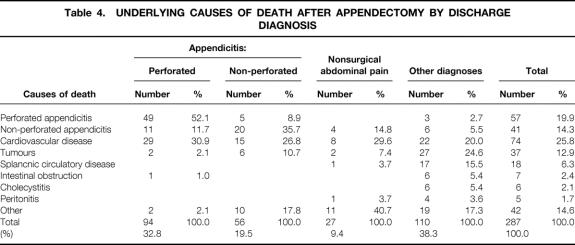
Causes of Death
Cardiovascular disease was the most common cause of death (25.8%), followed by perforated appendicitis (19.9%), nonperforated appendicitis (14.3%), and tumors (12.9%) (Table 4). The patterns of causes of death varied by discharge diagnosis. Appendicitis and peritonitis accounted for 64% of the deaths among patients with perforated appendicitis, 45% of the deaths among the patients with nonperforated appendicitis, 19% of the deaths among the patients with NSAP, and 12% among the patients with other diagnoses. Among the NSAP patients, 70% were assigned a cause of death that was localized outside the abdomen. In these patients, neither the discharge diagnosis nor the cause of death motivated an abdominal exploration.
Table 4. UNDERLYING CAUSES OF DEATH AFTER APPENDECTOMY BY DISCHARGE DIAGNOSIS
DISCUSSION
The CFR and the death rate after appendectomy for appendicitis in this study are among the lowest that have been reported. 16–20 Appendectomy is not, however, a harmless procedure; rather, it is associated with a sevenfold excess 30-day rate of death compared with the general population. The death rate after appendectomy is related to age and to the diagnosis at surgery. The highest CFR was found among elderly patients and the highest SMR among children younger than 10 years of age, showing a high risk in frail patients. Perforation of the appendix was associated with an almost doubled rate of death compared with nonperforated appendicitis, but the difference was smaller among the very young and the very old. This is in accordance with the studies of Addiss et al 19 and Luckmann, 16 but the difference is smaller than reported by others who did not take the effect of age into account. 6,21,22
Death after appendectomy is not caused by appendicitis only but is also related to comorbidity and the trauma of anesthesia and surgery. 20,23 For perforated appendicitis, the excess rate of death is likely to be explained by peritonitis or sepsis. Similarly, the death rate among patients with other diagnoses is also expected, because this group includes patients with other potentially fatal diseases that were diagnosed at surgery.
However, the causes of the excess death rate in the patients with a discharge diagnosis of nonperforated appendicitis and NSAP are not evident. In a few patients, the cause of death indicated a fatal disease that was not noted among the discharge diagnoses and therefore may have been undetected at the time of surgery. In many patients, however, the cause of death was a disease that is normally not fatal, such as nonperforated appendicitis and urinary tract infection. Many died of cardiovascular diseases. Some of these deaths may have been caused by the trauma of anesthesia and surgery in patients with low physiologic reserves as a result of age or comorbidity. 24 The excess death rate after appendectomy for nonperforated appendicitis and NSAP therefore suggests that the surgical trauma itself may in fact be an important cause of death, as proposed in 1971 by Lichtner and Pflanz. 25 An alternative interpretation is that frail patients are more prone to develop nonperforated appendicitis or to be subjected to appendectomy for NSAP. Unfortunately, comorbidity could not be assessed from the available data.
Our study is one of the largest population-based analyses performed on this subject. Unlike other studies, we also included deaths after appendectomy for causes other than appendicitis. The study design, with linkage of the National Inpatient Register to the Swedish Death Register, had the advantage of including all discharges after appendectomy in Sweden during a decade, and enabled a complete follow-up of both dates of death and underlying causes of death. This made it possible to include all deaths that had occurred within 30 days after surgery and also after the patient was discharged from the hospital.
Register studies may give biased results as a result of misclassification. The accuracy of an appendicitis diagnosis in the National Inpatient Register was assessed in one previous local study. 11 The appendicitis diagnosis was falsely positive in 10% and falsely negative in 6% of the patients when the registered diagnoses were compared with the pathologic anatomical diagnoses. These figures are probably representative of the whole register. Misclassification of the date of death is less likely because the reporting from the Swedish Death Register is virtually complete and is of high quality. 26 Misclassification of the causes of death is probably more of a problem because an autopsy has been performed in only some of the patients. However, it seems less likely that misclassification and undiagnosed fatal disease could explain all of the excess deaths after nonperforated appendicitis and NSAP.
Our results have implications for healthcare providers because of the changing panorama of appendectomies in industrialized countries. Longitudinal studies repeatedly have three main findings in common. The first is a decreasing incidence rate of appendectomies, in the range of two to five percentage points per year. The second is an increasing proportion of appendectomies among older patients, and the third is an improved diagnostic accuracy, particularly among women. With fewer patients undergoing surgery and successively older patients coming from an aging population, efforts to monitor outcomes are indeed relevant, but they need to be placed in a proper perspective. Appendectomy is associated with a low absolute number of deaths, only 3 per 1 million population per year. However, appendectomy is still associated with a rather high excess death rate, and our results suggest that some of these deaths may be avoidable.
It may be argued that a certain level of adverse events when operating on patients with suspected appendicitis is a calculated risk to be taken to prevent perforations, thereby reducing an even higher rate of death. However, the natural history of nonperforated appendicitis is not known, but there are indications that spontaneous resolution is common. 11 Others have shown that most perforations have already occurred before the patient arrives at the hospital, with no relation to in-hospital delay. 10,27,28 The strategy to prevent perforations by liberal and early exploration of patients with suspected appendicitis is therefore not supported.
Our results shed additional light on this practice because they suggest that the surgical trauma itself may cause deaths among patients who undergo appendectomy. Avoiding unnecessary surgery by making a correct preoperative diagnosis and minimizing surgical trauma by proper timing of surgery, with preoperative optimization of physiologic reserves, may therefore be more important to reduce the death rate from appendicitis than performing urgent appendectomy in patients with an equivocal diagnosis of appendicitis. Nonsurgical treatment with antibiotics and percutaneous drainage of abscesses may also be considered in selected patients. 29 The historical maxim, “the right to being wrong in the diagnosis of appendicitis is the only sure means to avoid mortality from an essentially benign disease,” therefore no longer seems valid. 30
Footnotes
Roland Andersson was supported by grants from The Health Research Council in the Southeast of Sweden and The Committee for Research and Development, Jönköping County Council, Sweden.
Correspondence: Dr. Roland Andersson, Department of Surgery, Ryhov County Hospital, SE-551 85 Jönköping, Sweden.
E-mail: roland.andersson@ryhov.ltjkpg.se
Accepted for publication November 22, 2000.
References
- 1.Hoffmann J, Rasmussen OO. Aids in the diagnosis of acute appendicitis. Br J Surg 1989; 76: 774–779. [DOI] [PubMed] [Google Scholar]
- 2.Garcia Peña BM, Mandl KD, Fischer AC, et al. Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA 1999; 282: 1041–1046. [DOI] [PubMed] [Google Scholar]
- 3.Rao PM, Rhea JT, Novelline RA, et al. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med 1998; 338: 141–146. [DOI] [PubMed] [Google Scholar]
- 4.Ohmann C, Yang Q, Franke C. Diagnostic scores for acute appendicitis. Abdominal Pain Study Group. Eur J Surg 1995; 161: 273–281. [PubMed] [Google Scholar]
- 5.Andersson RE, Hugander A, Thulin AJ. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg 1992; 158: 37–41. [PubMed] [Google Scholar]
- 6.Velanovich V, Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg 1992; 58: 264–269. [PubMed] [Google Scholar]
- 7.Malt RA. The perforated appendix. N Engl J Med 1986; 315: 1546–1547. [DOI] [PubMed] [Google Scholar]
- 8.Hale DA, Jaques DP, Molloy M, et al. Appendectomy. Improving care through quality improvement. Arch Surg 1997; 132: 153–157. [DOI] [PubMed] [Google Scholar]
- 9.Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults. A prospective study. Ann Surg 1995; 221: 278–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koepsell TD, Inui TS, Farewell VT. Factors affecting perforation in acute appendicitis. Surg Gynecol Obstet 1981; 153: 508–510. [PubMed] [Google Scholar]
- 11.Andersson R, Hugander A, Thulin A, et al. Indications for operation in suspected appendicitis and incidence of perforation. Br Med J 1994; 308: 107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersson R, Lambe M, Bergstrom R. Fertility patterns after appendicectomy: historical cohort study. Br Med J 1999; 318: 963–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blomqvist P, Ljung H, Nyren O, et al. Appendectomy in Sweden 1989–1993 assessed by the Inpatient Register. J Clin Epidemiol 1998; 51: 859–865. [DOI] [PubMed] [Google Scholar]
- 14.Rothman KJ. Introduction to categorical statistics. In: Rothman KJ, Greenland S. Modern epidemiology, 2nd ed. Philadelphia: Lippincott-Raven; 1998: 234.
- 15.SAS Institute Inc. SAS/STAT® Software. Changes and enhancements through release 6.12. Cary, NC: SAS Institute Inc., 1997: 247–348.
- 16.Luckmann R. Incidence and case fatality rates for acute appendicitis in California. A population-based study of the effects of age. Am J Epidemiol 1989; 129: 905–918. [DOI] [PubMed] [Google Scholar]
- 17.Kaufer C, Franz I, Loblich HJ. Appendicitis–Wandel des Krankheitsbildes? Chirurgie 1989; 60: 501–507. [PubMed] [Google Scholar]
- 18.Bisset AF. Appendectomy in Scotland: a 20-year epidemiological comparison. J Public Health Med 1997; 19: 213–218. [DOI] [PubMed] [Google Scholar]
- 19.Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132: 910–925. [DOI] [PubMed] [Google Scholar]
- 20.Wen SW, Naylor CD. Diagnostic accuracy and short-term surgical outcomes in cases of suspected acute appendicitis. Can Med Assoc J 1995; 152: 1617–1626. [PMC free article] [PubMed] [Google Scholar]
- 21.Howie JG. Death from appendicitis and appendicectomy. An epidemiological survey. Lancet 1966; 2: 1334–1337. [DOI] [PubMed] [Google Scholar]
- 22.Peltokallio P, Tykka H. Evolution of the age distribution and mortality of acute appendicitis. Arch Surg 1981; 116: 153–156. [DOI] [PubMed] [Google Scholar]
- 23.McDonald PJ, Royle GT, Taylor I, et al. Mortality in a university surgical unit: what is an avoidable death? J R Soc Med 1991; 84: 213–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ergina PL, Gold SL, Meakins JL. Perioperative care of the elderly patient. World J Surg 1993; 17: 192–198. [DOI] [PubMed] [Google Scholar]
- 25.Lichtner S, Pflanz M. Appendectomy in the Federal Republic of Germany: epidemiology and medical care patterns. Med Care 1971; 9: 311–330. [DOI] [PubMed] [Google Scholar]
- 26.Statistics: Health, Diseases. Causes of death 1996. Stockholm: The National Board of Health and Welfare, Centre for Epidemiology; 1998.
- 27.Hale DA, Jaques DP, Molloy M, et al. Appendectomy. Improving care through quality improvement. Arch Surg 1997; 132: 153–157. [DOI] [PubMed] [Google Scholar]
- 28.Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults. A prospective study. Ann Surg 1995; 221: 278–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamini D, Vargas H, Bongard F, et al. Perforated appendicitis: is it truly a surgical urgency? Am Surg 1998; 64: 970–975. [PubMed] [Google Scholar]
- 30.Jacob ET, Bar-Nathan N, Iuchtman M. Error-rate factor in the management of appendicitis [letter]. Lancet 1975; 2: 1032. [DOI] [PubMed] [Google Scholar]