Abstract
Objective
To evaluate the effect of timing of spine fracture fixation on outcome in multiply injured patients.
Summary Background Data
There is little consensus regarding the optimal timing of spine fracture fixation after blunt trauma. Potential advantages of early fixation include earlier patient mobilization and fewer septic complications; disadvantages include compounded complications from associated injuries and inconvenience of surgical scheduling.
Methods
Patients with spine fractures from blunt trauma admitted to an urban level 1 trauma center during a 42-month period who required surgical spine fracture fixation were identified from the registry. Patients were analyzed according to timing of fixation, level of spine injury, and impact of associated injuries (measured by injury severity score). Early fixation was defined as within 3 days of injury, and late fixation was after 3 days. Outcomes analyzed were intensive care unit and hospital stay, ventilator days, pneumonia, survival, and hospital charges.
Results
Two hundred ninety-one patients had spine fracture fixation, 142 (49%) early and 149 (51%) late. Patients were clinically similar relative to age, admission blood pressure, injury severity score, and chest abbreviated injury scale score. The intensive care unit stay was shorter for patients with early fixation. The incidence of pneumonia was lower for patients with early fixation. Charges were lower for patients with early fixation. Patients were stratified by level of spine injury. There were 163 cervical (83 early, 80 late), 79 thoracic (30 early, 49 late), and 49 lumbar fractures (29 early, 20 late). There were no differences in injury severity between early and late groups for each fracture site. The most striking differences occurred in the thoracic fracture group. Early fixation was associated with a lower incidence of pneumonia, a shorter intensive care unit stay, fewer ventilator days, and lower charges. High-risk patients had lower pneumonia rates and less hospital resource utilization with early fixation.
Conclusions
Early spine fracture fixation is safely performed in multiply injured patients. Early fixation is preferred in patients with thoracic spine fractures because it allows earlier mobilization and reduces the incidence of pneumonia. Although delaying fixation in the less severely injured may be convenient for scheduling, it increases hospital resource utilization and patient complications.
There are several advantages to early mobilization of multiply injured patients. Lower rates of pulmonary complications and venothromboembolic events are the major benefits. Perhaps the best example of this concept is illustrated in the evolution of the management of femur fractures in trauma patients. Historically, standard therapy was balanced skeletal traction. Retrospective studies were then published reporting lower rates of death and complications with aggressive fracture management with internal fixation. 1–3 In a prospective randomized trial, Bone et al 4 compared early surgical stabilization (within 24 hours) with delayed fixation. They showed that the incidences of pulmonary dysfunction, adult respiratory distress syndrome, and pulmonary emboli were all reduced. Ventilator and hospital days were also reduced in the early fixation group. Seibel et al 2 further showed that 10 days of traction in patients with multiple, severe injuries was detrimental. Patients with immediate fracture fixation had a significantly shorter duration of the pulmonary failure state compared with those in prolonged traction. The authors emphasized the importance of mobilization (bed to chair) to reduce pulmonary failure.
Although some have questioned early fixation in high-risk patients (severe associated injuries, including chest and brain injuries), 5,6 others have found that fixation within 72 hours (preferably 24 hours) is beneficial. 7–9 Little work has been done in the important area of spine fracture fixation. We conducted this study to try to answer three questions: Does the timing of spine fracture fixation affect nonneurologic outcomes? Do the location of the spine fracture and the timing of repair affect nonneurologic outcomes? Does the timing of spine fracture fixation affect patients with neurologic deficits?
METHODS
All patients with blunt trauma admitted to the Presley Regional Trauma Center (Memphis, TN) during a 42-month period ending December 1999 with spine fractures that required surgical stabilization were included in the study. These patients were identified from the trauma registry. Patients whose cervical spine fractures were treated only with a halo vest were not included.
All patients were admitted to the trauma service. Spine fracture fixation was performed by either the orthopedic or neurologic surgeons, alternating according to the hospital admission date. The decision to operate was at the discretion of the orthopedic or neurosurgical attending surgeon. General indications for surgical spine fracture fixation included spine fracture with significant neurologic deficit, and an unstable fracture pattern.
General Patient Care
Patients underwent standard resuscitation protocols that included crystalloid (lactated Ringer’s) and blood. Abdominal evaluation for hemodynamically unstable patients included abdominal ultrasound or diagnostic peritoneal lavage if the ultrasound was equivocal. Patients with significant hemoperitoneum underwent emergent celiotomy. Hemodynamically stable patients had computed tomography and celiotomy if necessary. Long bone fractures were repaired within 24 hours unless there were compelling reasons for delay, such as severe brain injury with intracranial hypertension.
Patients with spine fractures were not mobilized (i.e., bed to chair) until fixation was accomplished. These patients were log-rolled in the interim. Indications for mechanical ventilation included severe brain injury, airway protection after maxillofacial trauma, and respiratory failure. Weaning from mechanical ventilatory support was instituted when the problem for which the patient was intubated had resolved. For patients who would likely require prolonged airway protection, tracheostomy was performed, usually within 7 days. All patients had prophylaxis against deep vein thrombosis with subcutaneous heparin (unfractionated or fractionated), calf compression devices, or a combination. Patients with spinal cord injuries had vena cava filters placed.
Definitions and Outcomes
Patients were analyzed according to the timing of spine fracture fixation, the level of spine fracture, and the impact of associated injuries. Total body injury was measured by the Injury Severity Score (ISS; range 0–75). Brain injury was measured by the score on the Glasgow Coma Scale (GCS; range 3–15). Severity of chest injury was measured by the Abbreviated Injury Score (AIS; range 1–5). Functional outcome was measured by the Functional Independence Measure Score (FIM; range 3–12), which uses three components: feeding, locomotion, and expression.
Early spine fracture fixation was defined as surgical stabilization within 3 days of injury. Late spine fracture fixation was defined as surgical stabilization greater than 3 days from injury. A diagnosis of pneumonia required bronchoscopy with bronchoalveolar lavage, with cultures of the lavage effluent yielding at least 105 colony-forming units/mL. Other outcomes analyzed were ventilator days, intensive care unit (ICU) days, hospital length of stay, and hospital charges.
Statistical Analysis
Discrete variables were compared using chi-square analysis or the Fisher exact test. Continuous variables were compared using the unpaired Student t test. Statistical significance was set at P < .05.
RESULTS
Over the 3.5-year study period, there were 11,296 blunt trauma admissions. Of these, 1,756 (16%) had some type of spine fracture, and 291 (17% of spine fractures, 3% of blunt admissions) had surgical fixation of their spine fracture. These patients form the basis of this report. Patients with penetrating spine injuries were not included.
There were 212 male patients (73%) and 79 female patients (27%). Mean age was 34 years, and mean ISS was 24. Mechanism of injury was a motor vehicle crash in 71%, a fall from height in 14%, a motorcycle crash in 7%, a diving accident in 5%, and an assault in 3%. The location of the spine fracture was cervical in 56%, thoracic in 27%, and lumbar in 15%. The overall incidence of spinal cord injury was 50% (145 patients). In these patients, the location of spine fracture was cervical in 50%, thoracic in 31%, and lumbar in 10%. Overall pneumonia incidence was 27%, and overall death rate was 4%.
Patients were assigned to orthopedics or neurosurgery based on the admission date. Orthopedics managed 149 patients (51%) and neurosurgery 142 (49%). Early fixation was accomplished in 52% for orthopedics and 45% for neurosurgery. There were no outcome differences between the patient groups.
Table 1 describes the patient characteristics relative to the timing of surgical spine fracture fixation. Although there are statistical differences between the early and late fixation groups, these differences are of questionable clinical significance. The chest AIS was greater in the late group probably because of the greater number of thoracic spine fractures. Four patients had multiple-level fractures (two cervical and thoracic, two thoracic and lumbar). Three of these had early fixation and one had late fixation. Thus, the early and late fracture fixation groups were well matched for injury severity.
Table 1. PATIENT INJURY CHARACTERISTICS

ISS, Injury Severity Score; SBP, systolic blood pressure; GCS, Glasgow Coma Scale Score; AIS, Abbreviated Injury Score.
Patient outcomes after spine fracture fixation relative to the timing of surgery are shown in Table 2. Despite similar severity of injury, those who underwent late spine fracture fixation had a significantly higher incidence of pneumonia and longer ICU and hospital stays. These translated into substantially higher hospital charges and resource utilization. When the FIM scores were compared, there were no statistical differences between the groups relative to total scores (9.0 vs. 8.4).
Table 2. OUTCOMES RELATIVE TO TIMING OF SPINE FRACTURE FIXATION
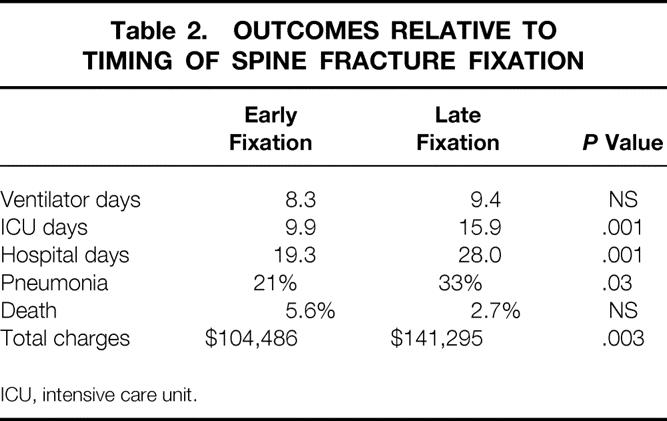
ICU, intensive care unit.
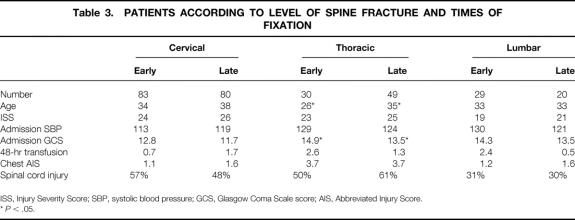
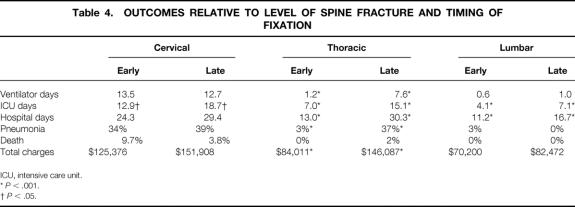
Patients were then analyzed according to the level of spine injury. Table 3 lists the patient characteristics for each fracture level and fixation time. Each fracture level group was fairly well matched relative to injury severity. Those with thoracic fractures who underwent early fixation were younger than those in the late fixation group, but there were otherwise no substantial clinical differences between groups. Despite the similarity between groups, there were significant outcome differences (Table 4), primarily among patients with thoracic spine fractures. Delayed fixation was significantly associated with a prolonged ICU stay regardless of the fracture site and a prolonged hospital stay for patients with thoracic and lumbar fractures. In patients with thoracic fractures, ventilation days and the incidence of pneumonia were both significantly greater with late fixation. Late fixation was also associated with increased hospital charges, and the difference was significant in patients with thoracic fractures. There were no significant differences in FIM scores by fracture level relative to the timing of fixation. Thus, it appears that delayed fixation, when comparing all patients with surgical spine fractures and by individual fracture levels, is detrimental.
Table 3. PATIENTS ACCORDING TO LEVEL OF SPINE FRACTURE AND TIMES OF FIXATION
ISS, Injury Severity Score; SBP, systolic blood pressure; GCS, Glasgow Coma Scale score; AIS, Abbreviated Injury Score.
*P < .05.
Table 4. OUTCOMES RELATIVE TO LEVEL OF SPINE FRACTURE AND TIMING OF FIXATION
ICU, intensive care unit.
*P < .001.
†>P < .05.
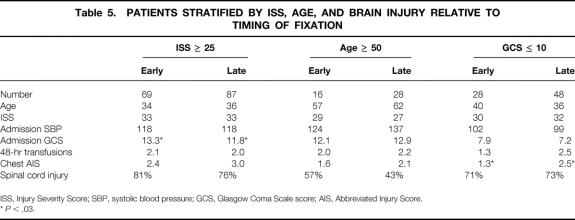
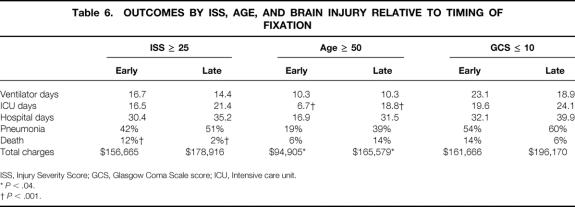
However, other reasons for delayed fixation may exist in patients with blunt trauma, including multiple associated injuries, advanced age, or brain injury. Therefore, patients were stratified according to these factors (Table 5). Within each patient group, there were no substantial clinical differences relative to severity of injury. Table 6 shows the outcomes for these groups according to the timing of fracture fixation. For patients with significant associated injuries (ISS ≥ 25), early spine fracture fixation was associated with shorter ICU and hospital stays, a lower pneumonia rate, and less resource utilization, but a significantly increased death rate. For older patients (50 years or older), early fixation was associated with shorter ICU and hospital stays, lower pneumonia and death rates, and significantly less resource utilization. For patients with significant brain injury (GCS ≤ 10), early fixation was associated with shorter ICU and hospital stays, a slightly lower pneumonia rate, a higher death rate, and less resource utilization. Patients without significant associated injuries (ISS ≤ 25) were also compared in a similar fashion. There were 73 patients who had early fixation and 62 who had late fixation. The groups were well matched with respect to ISS, GCS, chest AIS, and neurologic deficit. The early group was younger (30 vs. 37 years, P < .01). There were statistically significant differences in ventilator days (0.2 early vs. 2.5 late, P < .02), ICU stay (3.6 vs. 8.2 days, P < .001), hospital stay (8.7 vs. 17.9 days, P < .001), and hospital charges ($55,288 vs. $84,252, P < .001). The incidence of pneumonia was lower in the early group (1% vs. 8%), but this difference was not significant.
Table 5. PATIENTS STRATIFIED BY ISS, AGE, AND BRAIN INJURY RELATIVE TO TIMING OF FIXATION
ISS, Injury Severity Score; SBP, systolic blood pressure; GCS, Glasgow Coma Scale score; AIS, Abbreviated Injury Score.
*P < .03.
Table 6. OUTCOMES BY ISS, AGE, AND BRAIN INJURY RELATIVE TO TIMING OF FIXATION
ISS, Injury Severity Score; GCS, Glasgow Coma Scale score; ICU, Intensive care unit.
*P < .04.
†P < .001.
Given the association between the severity of chest injury and the subsequent development of pneumonia, 143 patients with significant pulmonary injury (chest AIS > 2) were analyzed relative to the timing of fixation (60 early, 83 late). Patients were similar according to age, ISS, admission blood pressure, transfusions, and incidence of cord injury. There were significant differences in ICU stay (10.8 days for early vs. 18.4 for late, P < .003), hospital stay (22.5 vs. 32.9 days, P < .02), and hospital charges ($120,815 vs. $164,854, P < .02). The incidence of pneumonia was also significantly higher in patients with late fixation (23% vs. 48%, P < .003). Thus, early fixation was associated with an improved outcome and resource utilization in patients with associated chest injury.
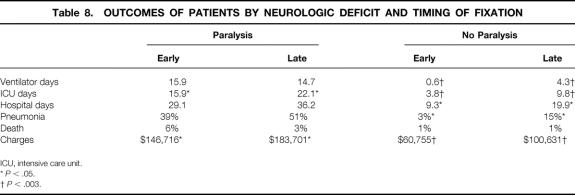
Table 7 compares patients with and without paralysis. Equivalent numbers underwent early and late fixation. Patients with paralysis and early fixation had a higher GCS but were otherwise well matched. Patients without neurologic deficit and delayed fixation were older and had a slightly higher ISS. Table 8 illustrates outcomes in patients relative to spinal cord injury and the timing of fixation. Early fixation resulted in significant resource reductions for patients with neurologic deficits. For those without neurologic deficits, there were significant resource utilization reductions and a lower incidence of pneumonia. Thus, early fixation resulted in a better outcome and less resource utilization regardless of neurologic deficit.
Table 7. PATIENTS STRATIFIED BY NEUROLOGIC DEFICIT AND TIMING OF FIXATION
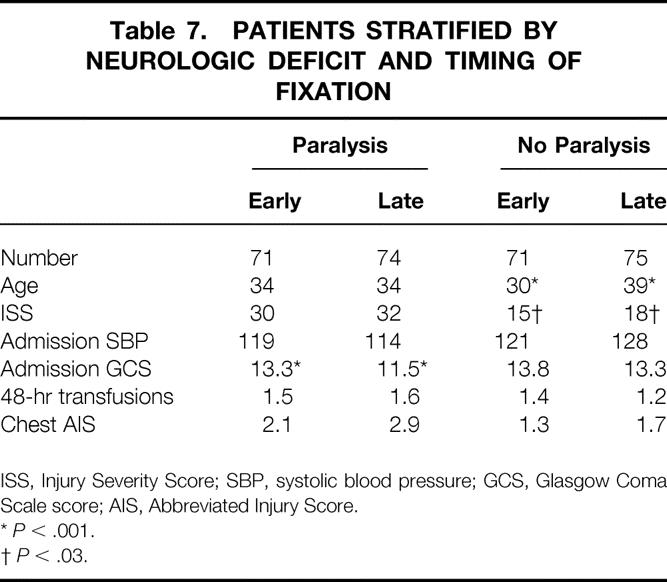
ISS, Injury Severity Score; SBP, systolic blood pressure; GCS, Glasgow Coma Scale score; AIS, Abbreviated Injury Score.
*P < .001.
†P < .03.
Table 8. OUTCOMES OF PATIENTS BY NEUROLOGIC DEFICIT AND TIMING OF FIXATION
ICU, intensive care unit.
*P < .05.
†P < .003.
Thromboembolic complications were evaluated. There were no instances of pulmonary emboli in the study population. In 12 patients (4%) deep vein thrombosis (iliac or femoral) developed. The incidence of deep vein thrombosis was significantly lower in the early group (1% vs. 7%, P < .04).
There were 12 deaths (4%). Eight (6% of early) occurred in the early group and four (3% of late) in the late group (P = NS). The causes of death in the eight patients with early fixation were sepsis and organ failure in five (all of whom had respiratory failure), brain injury in two, and tracheoesophageal fistula in one. All had cervical fractures, and seven had quadriplegia. The causes in the late group were sepsis and organ failure in three (all had respiratory failure) and withdrawal of support in one. Three had cervical fractures (two with quadriplegia) and one had a thoracic fracture with no neurologic injury.
DISCUSSION
The timing of spine fracture fixation is controversial. Several studies have evaluated the neurologic outcome, but there is no consensus on the timing of spine fixation. Wagner and Chehrazi 10 reported that surgical decompression within 48 hours of injury in 44 patients had no effect on neurologic recovery. Tator et al 11 compared surgical and nonsurgical therapy in 208 patients with spinal cord injury and found no difference in neurologic outcome. Marshall et al 12 analyzed 283 patients with spinal cord injuries in a multiinstitutional study and found that although neurologic deterioration was uncommon (5%), no deterioration occurred when surgery was performed after 5 days. A prospective randomized study was conducted by Vaccaro et al 13 comparing early (<72 hours) and late (>5 days) spine fixation. They found no neurologic benefit with early surgery. Others have suggested that early fixation may result in improved neurologic outcome. Levi et al 14 showed, in 103 patients, functional improvement with early (<24 hours) spine fixation. Mirza et al 15 studied 43 patients and stated that early surgery (<72 hours) may improve neurologic recovery in patients with cervical cord injuries. Although long-term neurologic outcome was not addressed in the current study, there were no differences in the FIM scores between those with early and late spine fracture fixation.
Comparative data regarding the timing of spine fracture fixation and nonneurologic outcome have not adequately been addressed in the literature. Mirza et al 15 compared patients with early cervical spine fracture fixation at one institution with delayed fixation from another institution. They found that early fixation was associated with fewer nonneurologic complications. However, given the study design (two different institutions with different management schemes), these outcomes are difficult to interpret. Levi et al 14 compared early and late fixation in 103 patients with cervical cord injuries and ISS higher and lower than 18. They showed improved resource utilization in the early surgery groups, but the groups were relatively small. Schlegel et al 16 had similar findings in a group of 138 patients. The results of other studies have suggested that early fixation does not result in improved nonneurologic outcomes, 10,11,16 and one group showed a higher frequency of thromboembolic complications in the surgical group. 11
The current study emphasized nonneurologic outcome relative to the timing of spine fracture fixation in a large, single-institution series. The groups were well matched for injury severity, level of spine fracture, and incidence of neurologic deficit. Patients with early fixation had a significantly lower incidence of pneumonia and shorter ICU and hospital stays, resulting in lower hospital charges. Thus, when evaluating all patients with spine fractures, there is a distinct advantage to fracture fixation within 3 days of injury relative to nonneurologic outcome. This is likely due to earlier patient mobilization and its advantages to overall patient care, similar to the findings for early long bone fracture fixation. Indeed, fixation at 24 or 48 hours may also be beneficial, but these time frames were not addressed in this study. Further studies may elucidate a better time for fixation.
The most striking outcome and resource utilization differences were seen in patients with thoracic spine fractures. Early fixation enabled more timely mobilization of patients, resulting in a lower incidence of pneumonia and less resource utilization. Patients with cervical and lumbar fractures also had less resource utilization. Early mobilization is extremely important in these patients, most of whom have significant associated pulmonary injuries.
A criticism of this retrospective study is that the early and late fixation groups were statistically different relative to age, GCS, and chest AIS (see Table 1). These confounding variables may skew the analysis because they are all associated with pulmonary complications. 17,18 Thus, high-risk groups were analyzed separately: patients were stratified according to injury severity, age 50 years or older, GCS score 10 or less, and severity of chest injury. There was no advantage to late spine fracture fixation in the high-risk groups of older age and significant brain injury. Patients with chest AIS of more than 2 and early fixation had a significantly lower incidence of pneumonia and less hospital resource utilization. However, there was a significantly higher death rate with early fixation in the most severely injured patients (ISS ≥ 25), although the numbers were small. A possible explanation is that the incidence of cervical cord injury (the highest-risk patient) was greater in the early group (85%) versus the late group (73%). In addition, the ISS was greater in those who died (37 vs. 29), suggesting more severe injury. Further, exclusion of deaths not related to the spine fracture resulted in no significant difference in death rates. It is clear that this select group of severely injured patients warrants careful consideration of risks and benefits before spine fracture fixation. In general, it appears that early fixation in all these high-risk groups is beneficial.
In conclusion, spine fracture fixation within 72 hours of injury is beneficial in trauma patients. Fixation even sooner may also improve outcomes and should be studied. Significant reductions in the incidence of pneumonia were seen with early fixation in patients with thoracic spine fractures, patients with severe associated chest injuries, and patients without neurologic deficit. Significant reductions in hospital resource utilization were seen with early fixation in patients with thoracic spine fractures, severe associated chest injuries, and fewer associated injuries (ISS < 25), and in patients with or without neurologic deficit. Although early fixation may cause problems with surgical scheduling, it does allow early mobilization of patients. Further studies should be performed, ideally in a prospective randomized fashion, to determine the full impact of the timing of spine fracture fixation.
Discussion
DR. GRACE R. ROZYCKI (Atlanta, Georgia): President Aust, Secretary Townsend, members, and guests. Initiatives devoted to streamlining the care of the injured patient are not only important for quality improvement but integral to the financial survival of a department.
In this study, the authors analyzed data on 291 patients who required operative spine fracture fixation relative to the timing of the fracture fixation, level of spine injury, and the impact of associated injuries. The authors chose to focus on select but important parameters, including the length of stay, survival, and hospital charges. And given their special expertise in the assessment of pulmonary complications, Dr. Croce carefully examined the number of ventilator days and the incidence of pneumonia in these patients. Similar to data reported by others, the authors showed that early fixation of spine fractures is beneficial for patients, as evidenced by a decrease in their morbidity, especially that of pulmonary complications. I have several questions for the authors.
Did patients with the presence of cervical neurologic deficits have higher rates of pulmonary complications than expected, compared with those patients who had similar injuries but did not require operative fixation? Did any of the patients have multiple levels of injury, and how did this affect the management? These are a particular challenge to the orthopedic or neurosurgeon who, even if they want to implement early fixation, may have to stage these procedures.
In my experience, patients with spine fractures secondary to a penetrating mechanism frequently have intraabdominal injuries which, by their nature, delay the fracture fixation and include an increase in complication rates. How would you suggest that their fixation be expedited?
Although the management of patients with operative spine fractures requires multidisciplinary efforts, the real importance and message in this paper is that surgeons should lead the way in that management toward superb patient care.
I would like to congratulate the authors on another solid contribution to the literature and express my appreciation to the Association for the privilege of discussing this paper.
DR. WILLIAM C. CIOFFI, JR. (Providence, Rhode Island): Dr. Croce has focused on an important aspect of care of the blunt trauma patient with a spine fracture requiring fixation. In this retrospective review of 291 patients requiring surgery, roughly one half had spinal fixation greater than 72 hours following injury. At first glance, the early and late groups appear equivalent in terms of severity of injury, and the early group appears to have decreased morbidity with cost of care. They conclude that early fixation is beneficial.
From a review of their data, I would conclude that early fixation is at least safe in the appropriately selected patient, especially given the length of these procedures and the positioning required to carry them out. To better understand the data, I have several questions.
Why 3 days, and why was there a delay in the late patients? Despite your thorough univariate analysis, is it possible that these patients were sicker, with more comorbid processes?
Did more late patients have other surgery to include abdominal/extremity orthopedic procedures? Was there a difference in the type of fixation, especially in the cervical group, in terms of open fixation versus use of halos? Was there a difference in the complexity of the spine fracture in the distribution of complete and partial neurologic injury? Did all patients receive steroids in the perioperative period?
Given the retrospective design, is it impossible to be sure that the groups were truly comparable? Indeed, the delayed group was older, with more severe chest injuries.
To help account for these differences, and keep dependent variables at bay, a multivariate analysis would be more appropriate to help control for group differences, and I wonder if you have carried that out.
I enjoyed this paper and I think it is safe to conclude that early spine fixation is safe in the appropriately selected patient, but not necessarily better until we have a more thorough multivariate analysis of the data or a prospective study. Thank you.
DR. MARTIN A. CROCE (Memphis, Tennessee): I’d like to thank Dr. Rozycki and Dr. Cioffi for their comments. First, I’d like to address Dr. Rozycki’s questions.
Indeed, the highest complication rates in the entire study were in patients who had cervical spine fractures with neurologic deficit. We had no comparison with nonoperative patients because we only included in the study those patients who underwent operative spine fracture fixation. Patients who had halo vests were not included in this study population. We did, however, briefly look at those patients who did have halo vests placed. I’m here to tell you that that is not an innocuous procedure. These patients do not typically jump up and run out if they don’t have neurologic deficit, because a halo vest is a restrictive device placed on the chest. And especially in patients with multiple injuries, halo vests are associated with a significant incidence of pneumonia and other pulmonary complications.
The second question dealt with patients who had multiple-level injuries. That occurred in about 2% of the population. Those patients did typically undergo staged procedures. For the purpose of this particular study, they entered into the group which enabled them to be mobilized. Most patients with multiple spine injuries, therefore, went into the late group because, with staging the procedures, they weren’t able to get out of bed until their final spine fracture was fixed, which would put them past the 3-day limit.
The third question dealt with penetrating injuries. We did not evaluate penetrating injuries, although typically those types of injuries are stable fractures and their incidence of operative fixation is not nearly as high as those patients who had blunt spine injuries. We think it is still imperative that they be measured for their brace or whatever sort of device that they’re going to get in a very timely fashion, and I’m not sure that laparoscopy would really preclude that except in the unusual case of open abdomen with subsequent multiple reexplorations.
To address Dr. Cioffi’s question, why 3 days: we chose 3 days for a number of different reasons. First, there is really no consensus in the literature. If one evaluates the limited data for nonneurologic outcomes, early and late is defined as anywhere from 24 hours to 5 days.
Did all patients receive steroids? Yes, they did, and the standard protocol for 24 hours. Relative to the issue of group inequality and, perhaps, those who had cervical spine fractures, again, as I mentioned, people who were treated only with halo vests were not included in the study.
Relative to the overall differences between groups, yes, this is a retrospective study, but I am not here to apologize for the data. Retrospective studies have inherent problems, and I’d like to paraphrase, I guess, Bill Parcells, coach of the Giants, who at the time was asked about his team’s record, and he says, “We are what we are.” Well, to paraphrase that, I’d say the data is what it is, with no definition of “is” required.
Rather than force the data to fit some sort of model with multivariate analysis, we chose to analyze each high-risk group separately. I think in this sort of analysis, it then makes the interpretation a little bit more meaningful. With multiple outcomes that were measured, manipulating a multivariate analysis is certainly possible and one can manipulate it to whatever sort of evaluation you want. We did perform such a multivariate analysis and found that pneumonia and increased resource utilization was associated with injury severity and delayed spine fracture fixation.
Not only is early fixation safe, we think it is really beneficial, with improved outcomes and improved resource utilization. There certainly is no advantage to delayed spine fracture fixation. Much does depend on the individual hospital resources. But if the hospital chooses to care for these particular patients, then it should provide the resources to allow surgeons to perform early spine fracture fixation.
I’d like to thank the Southern for the privilege of presenting this data.
Footnotes
Presented at The Southern Surgical Association, 112th Annual Session December 2000.
Correspondence: Martin A. Croce, MD, Department of Surgery, University of Tennessee, Memphis, 956 Court, E226, Memphis, TN 38163.
E-mail: mcroce@utmem.edu
Accepted for publication December 2000.
References
- 1.Goris RJ, Gimbrere JS, van Niekerk JL, et al. Early osteosynthesis and prophylactic mechanical ventilation in the multitrauma patient. J Trauma 1982; 22: 895–903. [DOI] [PubMed] [Google Scholar]
- 2.Seibel R, LaDuca J, Hassett JM, et al. Blunt multiple trauma (ISS 36), femur traction, and the pulmonary failure-septic state. Ann Surg 1985; 202: 283–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress syndrome in patients with multiple musculoskeletal injuries: effect of early operative stabilization of fractures. J Trauma 1985; 25: 375–384. [DOI] [PubMed] [Google Scholar]
- 4.Bone LB, Johnson KD, Weigelt J, et al. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg [Am] 1989; 71: 336–340. [PubMed] [Google Scholar]
- 5.Reynolds MA, Richardson JD, Spain DA, et al. Is the timing of fracture fixation important for the patient with multiple trauma? Ann Surg 1995; 222: 470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pape HC, Auf’m’Kolk M, Paffrath T, et al. Primary intramedullary femur fixation in multiple trauma patients with associated lung contusion: a cause of posttraumatic ARDS? J Trauma 1993; 34: 540–547. [DOI] [PubMed] [Google Scholar]
- 7.Charash WE, Fabian TC, Croce MA. Delayed surgical fixation of femur fractures is a risk factor of pulmonary failure independent of thoracic trauma. J Trauma 1994; 37: 667–672. [DOI] [PubMed] [Google Scholar]
- 8.Beckman SB, Scholten DJ, Bonnel BW, et al. Long bone fractures in the polytrauma patient. The role of early operative fixation. Am Surg 1989; 55: 356–358. [PubMed] [Google Scholar]
- 9.van Os JP, Roumen RM, Schoots FJ, et al. Is early osteosynthesis safe in multiple trauma patients with severe thoracic trauma and pulmonary contusion? J Trauma 1994; 36: 495–498. [DOI] [PubMed] [Google Scholar]
- 10.Wagner FC Jr, Chehrazi B. Early decompression and neurological outcome in acute cervical spinal cord injuries. J Neurosurg 1982; 56: 699–705. [DOI] [PubMed] [Google Scholar]
- 11.Tator CH, Duncan EG, Edmonds VE, et al. Comparison of surgical and conservative management in 208 patients with acute spinal cord injury. Can J Neurol Sci 1987; 14: 60–69. [DOI] [PubMed] [Google Scholar]
- 12.Marshall LF, Knowlton S, Garfin SR, et al. Deterioration following spinal cord injury. A multicenter study. J Neurosurg 1987; 66: 400–404. [DOI] [PubMed] [Google Scholar]
- 13.Vaccaro AR, Daugherty RJ, Sheehan TP, et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine 1997; 22: 2609–2613. [DOI] [PubMed] [Google Scholar]
- 14.Levi L, Wolf A, Rigamonti D, et al. Anterior decompression in cervical spine trauma: does the timing of surgery affect the outcome? Neurosurgery 1991; 29: 216–222. [PubMed] [Google Scholar]
- 15.Mirza SK, Krengel WF III, Chapman JR, et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop 1999; 359: 104–114. [DOI] [PubMed] [Google Scholar]
- 16.Schlegel J, Bayley J, Yuan H, et al. Timing of surgical decompression and fixation of acute spinal fractures. J Orthop Trauma 1996; 10: 323–330. [DOI] [PubMed] [Google Scholar]
- 17.Wilmot CB, Hall KM. Evaluation of the acute management of tetraplegia: conservative versus surgical treatment. Paraplegia 1986; 24: 148–153. [DOI] [PubMed] [Google Scholar]
- 18.Hoyt DB, Simons RK, Winchell RJ, et al. A risk analysis of pulmonary complications following major trauma. J Trauma 1993; 35: 524–531. [DOI] [PubMed] [Google Scholar]
- 19.Croce MA, Fabian TC, Waddle Smith L, et al. Identification of early predictors for post-traumatic pneumonia. Am Surg 2001; 67: 105–110. [PubMed] [Google Scholar]