Abstract
Objective
To compare a new technique of radical hemorrhoidectomy using an electrothermal device originally devised to seal vessels in abdominal operations, with the conventional open Milligan-Morgan procedure performed with diathermy.
Summary Background Data
Hemorrhoidectomy is one of the most commonly performed anorectal operations. Two well-established methods, the “open” Milligan-Morgan excision and the “closed” Ferguson technique, both carry risks of postoperative bleeding, urinary retention, and late anal stenosis. The convalescence is similarly long and difficult after both operations. The quest for an improved technique of radical excision of hemorrhoids is justified.
Methods
In this case-control study, two groups of patients were alternatively allocated into study and control groups. In the study group (n = 40), an electrothermal system was used. The tissue fusion produced by this device consists of melting of collagen and elastin. This technique essentially achieves a sutureless closed hemorrhoidectomy. The operative time, postoperative complications, and time off work were compared with the group undergoing conventional Milligan-Morgan hemorrhoidectomy (control group, n = 40).
Results
The operative time and time off work were significantly shorter in the study group. There were also fewer postoperative complications in this group.
Conclusions
The “tissue-welding” properties of this device and the shape of the electrode handpiece may be successfully applied to the performance of an operation most appropriately described as a “modified sutureless closed hemorrhoidectomy.” This pilot study shows that this new technique is simple and safe, significantly shortens the operation, and is followed by a significantly easier and shorter recovery.
Hemorrhoidectomy is one of the most commonly performed anorectal operations. However, although it is considered a minor procedure, the postoperative course is protracted and the postoperative complications are not negligible. Two well-established methods of radical surgical ablation of grade 3 and 4 hemorrhoids are popular: the “open” Milligan-Morgan 1 excision and the “closed” Ferguson 2 technique. Although decades of experience confirm the long-term clinical efficacy of these methods, both carry the risk of troublesome complications, as reflected in recent reports. 3–5 Early urinary retention is common, increasing the risk of urinary tract infection. Postoperative bleeding may be severe and sometimes requires reoperation. Occasional late anal stenosis necessitates painful digital dilatations or surgical intervention. The course after both operations is difficult and the convalescence is prolonged.
The quest for an improved technique of radical excision of hemorrhoids led us to a novel application of an electrothermal device originally devised to seal vessels in abdominal surgery. We applied this device to perform an operation that essentially achieves a sutureless closed hemorrhoidectomy. This pilot study compares the outcome of our new technique with conventional open Milligan-Morgan diathermy hemorrhoidectomy.
PATIENTS AND METHODS
Eighty consecutively operated patients were alternatively allocated to either the study group, in which the new technique was used, or the control group, who underwent conventional open Milligan-Morgan hemorrhoidectomy. There were 40 patients in each group. All patients had either advanced grade 3 hemorrhoids (with a significant external component or after failure of rubber band ligations) or grade 4 hemorrhoids. These parameters constitute our usual indications for surgery. All patients were prospectively followed up for 6 months after surgery.
In the study group, the hemorrhoidectomy was performed using an electrothermal system designed to seal vessels by feedback-controlled application of energy and physical pressure, allowing brief cooling in compression (LigaSure, Valleylab, Boulder, CO). The tissue fusion mechanism consists of melting of collagen and elastin. The “seal area” of partially denatured protein has a bursting strength comparable to that of sutures. 6 We found that the “tissue-welding” properties of this device and the clamplike shape of the electrode handpiece may be successfully applied to the performance of an operation most appropriately described as a “sutureless closed hemorrhoidectomy.”
In the control group, a conventional open Milligan- Morgan hemorrhoidectomy was performed with diathermy excision of the hemorrhoidal complexes and chromic cat-gut transfixion of the vascular pedicles, as previously described. 3
All the operations were performed by the same surgeon (J.S.) as day-surgery cases (hospital stay <24 hours). General, caudal, or spinal anesthesia was used, according to the patient’s preference.
Follow-up examinations were conducted 1, 3, and 6 weeks after surgery. Further examinations were carried out 3 and 6 months after the procedure.
The variables compared were operative time, early and late complications, and return to normal activities (return to work in most patients), as reported by the patients on follow-up visits. Data were analyzed using the SPSS statistical software (Chicago, IL). To compare the differences in outcome between the groups, we used the t test.
Surgical Technique
All patients are operated on in the lithotomy position. Hemorrhoidal complexes are exposed using a Chelsea-Eaton operating anoscope (Fig. 1). The internal and external components of each hemorrhoidal complex are grasped and elevated by two Allis clamps. Countertraction is applied on the skin, slightly lateral to the intersphincteric groove, by a third Allis clamp (Fig. 2). The clamplike electrode is positioned beneath the external component (external hemorrhoid or skin tag) and is activated. The feedback mechanism of the device automatically stops the energy delivery when tissue sealing is complete (Fig. 3). The resulting “seal zone” is transected (Fig. 4), and a second application of the electrode continues the sealed tissue line, now comprising the internal hemorrhoid and the inferior hemorrhoidal vascular pedicle. In larger hemorrhoids, a third application may be needed (Fig. 5). The procedure takes minutes to complete and is absolutely bloodless, and a sutureless radical closed hemorrhoidectomy is achieved (Fig. 6).

Figure 1. Exposure of the hemorrhoidal complex using a Chelsea-Eaton operating anoscope.

Figure 2. Preparation of the internal and external components of the hemorrhoidal complex for application of the sealing electrode. Note the lateral countertraction.
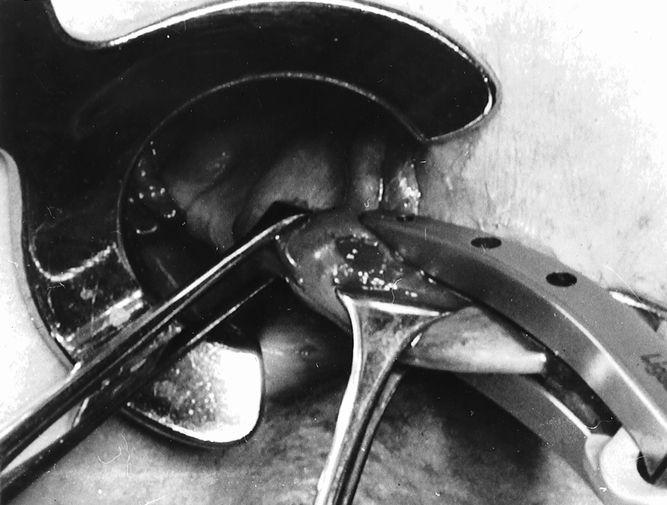
Figure 3. First application of the electrode beneath the external hemorrhoid or skin tag.

Figure 4. The external hemorrhoid is partially detached by cutting through the resulting “seal zone.”
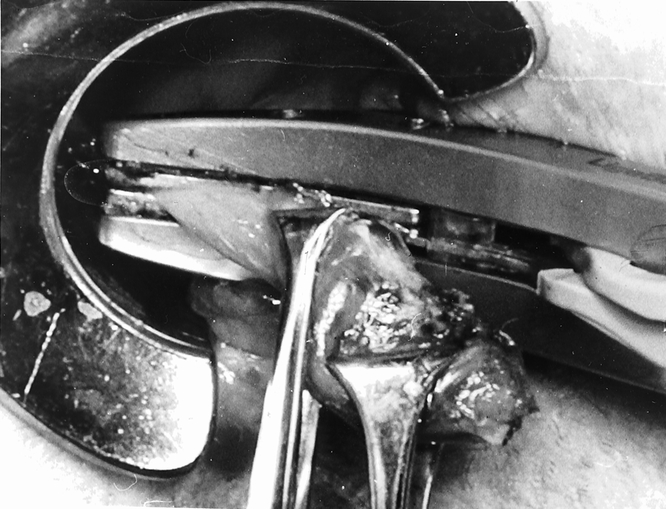
Figure 5. A second application of the electrode on the internal hemorrhoid and the inferior hemorrhoidal vascular pedicle completes the excision of the entire complex.
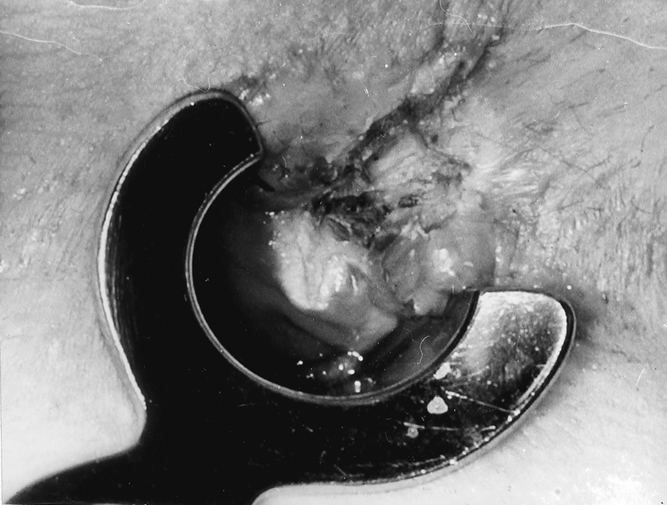
Figure 6. Completed sutureless closed hemorrhoidectomy. The “welded” mucosal line is seen, and the whitish area represents the coagulated inferior hemorrhoidal vascular pedicle.
RESULTS
There were 23 women and 17 men in the study group and 19 women and 21 men in the control group. The mean age was 44.2 years (range 26–72, standard deviation [SD] 10.8) in the study group and 42.0 years (range 27–72, SD 9.9) in the control group. There was no statistical difference in the gender and age mix between the groups (P = .49).
The mean operating time was 11.09 minutes (range 5–15, SD 3.40) in the study group and 38.76 minutes (range 20–60, SD 11.00) in the control group. This difference was statistically significant (P < .001). The operating time in the study group ranged from 5 to 15 minutes. With increasing experience and evolving improvement of technical details, the operating time tended to decrease.
Urinary retention necessitating catheterization was the only early complication in both groups. The incidence was lower in the study group (3/40, 7.5%) than in the control group (5/40, 12.5%), but this difference was not significant.
The return to normal daily activities, as defined and reported by the patient (in most patients time off work was the reference point), was significantly earlier in the study group. The mean convalescence period in the study group was 7.4 days (range 5–14, SD 3.6) versus 18.6 days (range 7–30, SD 5.4) in the control group (P < .001).
The 6-month follow-up did not reveal any late complications in the study group. In this group, most patients had a well-healed and supple anal canal when examined 6 weeks after surgery. In contrast, three patients in the control group (7.5%) were found to have a concentric and stenosing mucosal scar at the level of the dentate line, always detected at the 6-week postoperative examination. In two patients the stenosis responded and resolved after a series of weekly ambulatory digital dilatations, but in one patient surgical dilatation under anesthesia was necessary to relieve the stenosis permanently.
There were no cases of incontinence beyond 3 weeks after both operations. Complete wound healing was achieved in most patients after 6 weeks in the study group and after 3 months in the study group.
DISCUSSION
The accepted indications for surgical ablation are symptomatic hemorrhoids grade 4 or selected grade 3 hemorrhoids that failed a trial of nonsurgical treatment. For symptomatic hemorrhoids grade 1, 2, or 3, different conservative measures are available. The most effective seems to be rubber band ligation. 7
The conventional open and closed hemorrhoidectomy procedures 1,2 and their modifications are time-tested, but both entail similar complications and a protracted postoperative course. 5 This pilot study describes a new technique that proved safe and is significantly more rapid than open hemorrhoidectomy. Postoperative urinary retention occurred with an incidence similar to that found after conventional operations, as reflected in recent studies. 3–5 This complication might also be influenced by the regional anesthesia. However, the troublesome late anal stenosis that occurs in both the open and closed hemorrhoidectomy procedures with a frequency of 4% to 5%3,4 seems to be eliminated by our sutureless technique. In this series no postoperative bleeding occurred in either group, although it is frequently encountered in conventional operations. 4,5 We have recently described our technique aimed to minimize this complication in modified Milligan-Morgan hemorrhoidectomy. 3
There were no cases of incontinence beyond 3 weeks after either operation. The early postoperative partial incontinence that occurs in some patients may be explained by the pain, which hinders the voluntary sphincter contraction and is also compounded by the use of paraffin oil, which we prescribe for 2 weeks after surgery. We now prospectively evaluate the sphincter function and morphology in this procedure by pre- and postoperative manometry, endoanal sonography, and histology of the excised hemorrhoids.
However, the most important benefit of this new technique is the significantly shorter convalescence period. In our control group, the patients were usually incapacitated for 3 weeks, and a similarly long and painful recovery has been confirmed by others after either the conventional open or closed technique. 5 In contrast, our study group patients resumed their daily activities after a week, on average.
Although our follow-up is still short, the long-term results may be extrapolated from the well-proven conventional excisional operations because the surgical principle of radical excision of the hemorrhoidal complexes is identical. However, this pilot study determined the feasibility and safety of this technique and showed improved preliminary patient outcome. Long-term results should be evaluated in larger prospective series.
As a result of the quest for a better technique of hemorrhoidal ablation, two other new methods recently emerged. “Stapled hemorrhoidectomy” is based on an entirely different surgical philosophy, and the long-term results are still awaited. Whether this technique will eliminate the complications of the conventional operations or will create new problems is also a question to be evaluated. Moreover, the mucosectomy performed by the expensive circular stapler is best suited for grade 2 or 3 hemorrhoids without a significant external component, and these clinical situations may usually be dealt with effectively by rubber band ligation. 7 The ultrasonic “harmonic scalpel” was also used for hemorrhoidectomy. We have a limited experience with this technique; we tried it in ten patients. The operating time is much longer than in our technique as described here, mainly because the hemostasis is time-consuming and less effective. Nevertheless, the convalescence and wound healing time were comparable to those found in our technique (significantly shorter than in the conventional Milligan-Morgan operation, although the wounds are similarly wide open). This difference may be due to the absence of sutures.
In summary, our new technique achieves a sutureless closed hemorrhoidectomy that radically ablates both the internal and external components of grade 3 or 4 hemorrhoids and prominent skin tags. This technique is safe and rapid. Compared with conventional open excisional surgery, this method involves fewer complications and significantly shortens the convalescence period. Long-term follow-up in larger series is warranted.
Footnotes
Correspondence: Joel Sayfan, MD, FACS, Department of Surgery, Haemek Medical Center, Afula, Israel.
E-mail: sayfan@netvision.net.il
Accepted for publication February 12, 2001.
References
- 1.Milligan ETC, Morgan CN, Jones LE, Officer R. Surgical anatomy of the anal canal and the operative treatment of hemorrhoids. Lancet 1937; 2: 1119–1124. [Google Scholar]
- 2.Ferguson JA, Heaton JR. Closed hemorrhoidectomy. Dis Colon Rectum 1959; 2: 176–179. [DOI] [PubMed] [Google Scholar]
- 3.Sayfan J. Hemorrhoidectomy: avoiding the pitfalls. Tech Coloproctol 1998; 2: 129–130. [Google Scholar]
- 4.Sagar PM, Wolff BG. The use of the modified Whitehead procedure as an alternative to the closed Ferguson hemorrhoidectomy. Tech Coloproctol 1999; 3: 131–134. [Google Scholar]
- 5.Arbman G, Krook H, Haapaniemi S. Closed vs. open hemorrhoidectomy: is there any difference? Dis Colon Rectum 2000; 43: 31–34. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy JS, Stranahan PL, Taylor KD, Chandler JG. High-burst-strength, feedback-controlled bipolar vessel sealing. Surg Endosc 1998; 12: 876–878. [DOI] [PubMed] [Google Scholar]
- 7.Komborozos VA, Skrekas GJ, Pissiotis CA. Rubber band ligation of symptomatic internal hemorrhoids: results of 500 cases. Dig Surg 2000; 17: 71–76. [DOI] [PubMed] [Google Scholar]


