Abstract
Objective
To analyze reoperation rates for recurrent and primary groin hernia repair documented in the Swedish Hernia Register from 1996 to 1998, and to study variables associated with increased or decreased relative risks for reoperation after recurrent hernia.
Methods
Data were retrieved for all groin hernia repairs prospectively recorded in the Swedish Hernia register from 1996 to 1998. Actuarial analysis adjusted for patients’ death was used for calculating the cumulative incidence of reoperation. Relative risk for reoperation was estimated using the Cox proportional hazards model.
Results
From 1996 to 1998, 17,985 groin hernia operations were recorded in the Swedish Hernia Register, 15% for recurrent hernia and 85% for primary hernia. At 24 months the risk for having had a reoperation was 4.6% after recurrent hernia repair and 1.7% after primary hernia repair. The relative risk for reoperation was significantly lower for laparoscopic methods and for anterior tension-free repair than for other techniques. Postoperative complications and direct hernia were associated with an increased relative risk for reoperation. Day-case surgery and local infiltration anesthesia were used less frequently for recurrent hernia than for primary hernia.
Conclusions
Recurrent groin hernia still constitutes a significant quantitative problem for the surgical community. This study supports the use of mesh by laparoscopy or anterior tension-free repair for recurrent hernia operations.
A cost-effective treatment for groin hernia is important, given that hernia repair is one of the most common procedures in general surgery and is often performed on patients who need compensation for time off work. From the patient’s point of view, prevention of recurrence is more important than speed of recovery 1,2 There is a general acceptance of the use of mesh in the treatment of recurrent groin hernias. However, it is not clear to what extent and with what outcome this policy is adopted in general surgical practice. Surgical audit using prospectively recorded data in a defined population may provide such information.
The Swedish Hernia Register was established in 1992 on a voluntary basis to serve as a tool for describing, analyzing, and improving groin hernia surgery in member units. In a previous report, 3 a favorable outcome of recurrent hernia repair was observed with laparoscopic techniques. A recent analysis of all hernia repairs performed from 1996 to 1998 4 showed that the anterior tension-free repair originally described for primary hernia repair 5 was the only method associated with a reoperation rate lower than the Shouldice repair. The aim of the present report was to study the outcome of recurrent hernia repairs from the same period using reoperation as a proxy indicator of recurrence. 6
METHODS
The Swedish Hernia Register has been described previously. 3,7 Operations for groin hernias are prospectively documented according to a protocol with variables such as mode of admission, time on waiting list, patient characteristics, type of hernia as defined during surgery, methods of repair, anesthesia, nights in hospital, complications within 1 month, and reoperation for recurrence. Follow-up is not mandatory. A 3-year follow-up was, however, undertaken for all patients aged 15 to 80 years at surgery who underwent surgery in 1992 6 and was repeated for patients who underwent surgery in 1995 (unpublished). Swedish citizens are identifiable through Person Numbers, which makes it possible to compare reoperation for recurrence with previous operations documented in the register. It also allows actuarial calculations and risk analyses to be adjusted for death of patients according to the Swedish Death Register. External reviews with on-site visits to hospitals comparing register data with patient files 3 are now performed on an annual basis. In 1996 and 1998 21 and 37 units, respectively, had joined the register. Methods of repair were defined as myoaponeurotic (Shouldice, Bassini, McVay, Marcy, and other open nonmesh repair techniques); laparoscopic (transabdominal preperitoneal or total extraperitoneal techniques); anterior tension-free repair as defined by Lichtenstein et al;5 and other techniques using mesh, whether placed in the preperitoneal posterior space 8,9 or in the anterior space according to a specified technique 10 or as adjunct to a myoaponeurotic repair. Definitions of surgical techniques are available (in Swedish) on the web site of the National Board of Health and Welfare, Sweden (www.sos.se/mars).
Statistical analyses were performed using SPSS (Chicago, IL). The chi-square test was used to determine differences between groups. The cumulative incidence of reoperation was measured through actuarial analysis. Relative risk analyses were estimated with the Cox proportional hazards model, first performing univariate analysis with assumed risk variables and then selecting variables with highest or lowest univariate risks. The proportional hazards assumption was examined as part of the Cox analyses. Interaction terms between risk factors were introduced and examined in the multivariate analysis.
RESULTS
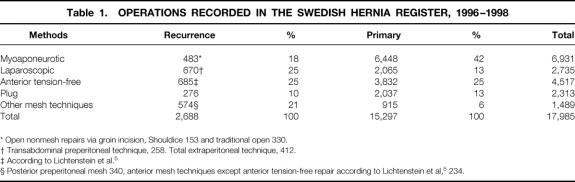
During 1996 to 1998 17,985 hernia operations were registered in the Swedish Hernia Register, 2,688 (15%) for recurrent hernia and 15,297 (85%) for primary hernia. Figure 1 illustrates the cumulative incidence of reoperation after recurrent and primary hernia repair. The reoperation rate was significantly greater after recurrent repair than after primary repair, with a relative risk (RR) of 2.7 (95% confidence interval [CI] 2.1–3.5). At 24 months the cumulative incidence of reoperation was 4.6% (95% CI 2.5–5.8%) for recurrent repair and 1.7% (95% CI 1.4–2.0%) for primary repair. As shown in Table 1, mesh techniques were used for 82% and 58% of operations for recurrent and primary hernia, respectively.
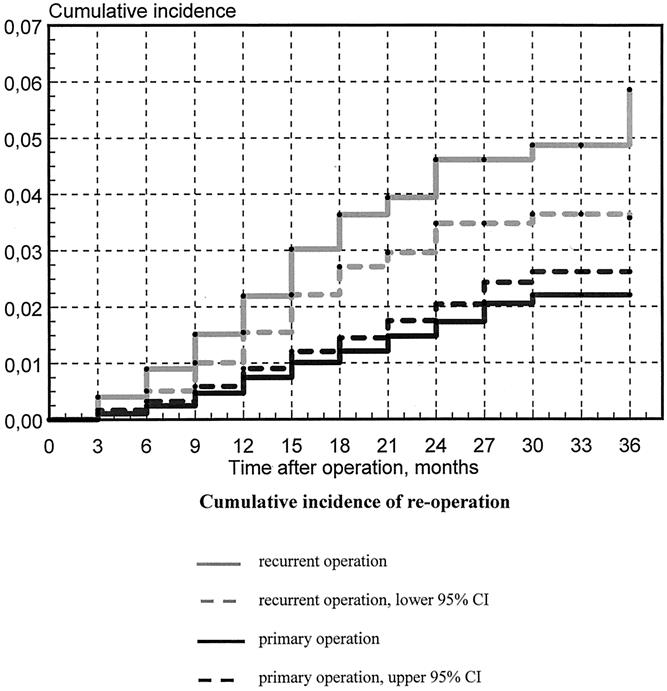
Figure 1. Cumulative incidence of reoperation. Gray solid line, recurrent operation; gray dashed line, recurrent operation, lower 95% confidence interval. Black solid line, primary operation; black dashed line, primary operation, upper 95% confidence interval.
Table 1. OPERATIONS RECORDED IN THE SWEDISH HERNIA REGISTER, 1996–1998
* Open nonmesh repairs via groin incision, Shouldice 153 and traditional open 330.
† Transabdominal preperitoneal technique, 258. Total extraperitoneal technique, 412.
‡ According to Lichtenstein et al. 5
§ Posterior preperitoneal mesh 340, anterior mesh techniques except anterior tension-free repair according to Lichtenstein et al, 5 234.
To facilitate statistical analysis of recurrent hernia repairs, Shouldice operations and traditional open repairs (Bassini, Marcy, McVay, and others) were all classified as myoaponeurotic repairs. Four operations for rerecurrence were observed among 153 Shouldice operations and 17 operations for rerecurrence among 330 traditional open repairs. The log-rank test of corresponding univariate actuarial curves showed a greater RR for reoperation for traditional open repairs compared with the Shouldice technique, but it did not reach statistical significance (RR 2.5 [95% CI 0.9–7.1]). Both posterior mesh repair and anterior mesh repair, with the exception of the Lichtenstein technique, 5 were included in the group “other mesh techniques.” No difference could be observed between these two groups: 12 reoperations were noted after 340 posterior mesh repairs and 9 reoperations after 230 anterior mesh repairs, not classified as the Lichtenstein method.
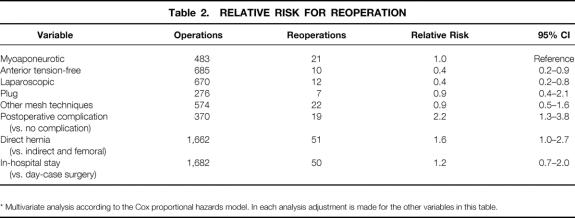
Table 2 shows the outcome of a multivariate analysis of possible risk factors for reoperation after recurrent hernia operation. Using myoaponeurotic repair as a reference, anterior tension-free repair 5 and laparoscopic surgery were associated with a significantly lower RR for reoperation. Direct hernia and postoperative complication carried an increased RR.
Table 2. RELATIVE RISK FOR REOPERATION
* Multivariate analysis according to the Cox proportional hazards model. In each analysis adjustment is made for the other variables in this table.
The use of day-case surgery and local anesthesia was lower in the treatment of recurrent hernia versus primary hernia (37% vs. 57% and 4% vs. 7%, respectively, P < .001 for both comparisons).
DISCUSSION
The present report is based on data from an ongoing register recruiting an increasing number of Swedish surgical units. It gives effectiveness (outcome in routine practice) as distinct from efficacy (results produced by experts under optimal conditions). 11 Further, the information obtained represents a disequilibrium that varies over time depending on surgical methods and the training, interest, and dexterity of surgeons. On a yearly basis each unit is supplied with data of its own achievements as well as aggregated data for all units. This has similarities with other systems designed to improve outcome in different fields of surgery. 12,13 Our results also indicate that participation in the Swedish Hernia Register has a quality-promoting influence. 4,7,14
During the period covered by this study, 15% of all procedures were done for recurrent hernias. This is within the range usually found in an audit of defined populations. 15 However, more favorable results were found in a recent Scottish survey, where 9% of all repairs were done for recurrence. 16 Our data indicate that recurrent hernia still represents a major challenge to general surgeons performing hernia surgery in Sweden.
The end point of the study, reoperation for recurrence, may be considered as a proxy indicator of the recurrence rate. In a recent cohort study 17 based on physical examination of 223 of 230 eligible patients (97%), it was concluded that the reoperation rate 44 months after surgery multiplied by a factor of 1.6 approximated the recurrence rate as defined by patients who need another operation. 18 The reoperation rate had to be multiplied by 2.0 to take into account the wider definition of recurrence, an expansile cough impulse. 19 Using these data, we can extrapolate that 2 years after recurrent and primary hernia operations, 7% and 3% of our patients, respectively, needed a re-do procedure. These figures are lower than previously presented data from the Swedish Hernia Register 20 but are nevertheless of great concern. The high reoperation rate after recurrent hernia repair in the present study makes scrutiny of treatment an essential part of the quality-improvement work of hernia surgery carried out in nonspecialized units.
We found that mesh prosthesis was used in 58% and 82% of primary and recurrent hernia repairs, respectively. The latter figure also indicates that 18% of recurrences were treated by nonmesh techniques, which according to the multivariate analysis gave a higher reoperation rate. Since 1992 the methods of repair used by Swedish surgeons have changed profoundly. 4 Mesh placed through a groin incision was used in a minority of repairs before 1996. However, by 1998 the anterior mesh repair 5 had become the dominant technique, and the use of myoaponeurotic methods (including the Shouldice technique) had declined from its previously high level.
The main finding of the present study is the reduced RR for reoperation for rerecurrence after laparoscopic repair and anterior mesh repair. Because of obvious difficulties in recruiting patients, large randomized trials of recurrent hernia repairs do not exist. Case series have, however, reported, low rerecurrence rates after recurrent hernia repair using laparoscopic methods. 21,22 Excellent results for recurrent hernia using the anterior tension-free repair 5 originally devised for primary hernia have recently been described. 23 The advantage of this technique in treating a recurrence after open myoaponeurotic repair is its relative safety and its familiarity to the general hernia surgeon; its drawback is dissection through scarred tissue, with risk of cord injury. The incidence of this complication can be reduced for indirect hernia by dividing the sac high and leaving the distal end open, thereby avoiding dissection within the cord. 24 In the choice between laparoscopic and anterior tension-free repair, the lower cost and shorter learning curve of the latter should be taken into account. 25,26 Low rerecurrence rates have also been reported after open posterior mesh repair. 27,28 This technique requires knowledge of preperitoneal anatomy as well as the use of general or regional anesthesia. It may be an attractive alternative (for general surgeons not performing laparoscopic hernia surgery) for the unusual recurrence after an anterior tension-free repair.
The finding that postoperative complications and direct hernias are associated with an enhanced risk for reoperation is in agreement with previous observations from the Swedish Hernia Register. 3,4 In this study infiltration local anesthesia was used for a minority of operations and less frequently for recurrent than for primary repairs. Local anesthesia was used for the majority of patients in the anterior tension-free series of Gianetta et al 23 referred to above. A greater use of local anesthesia might increase the cost-effectiveness 29 of Swedish hernia surgery. The lower day-case surgery rate of recurrent versus primary repairs suggests that greater costs are associated with treatment of recurrent hernia. 30
In conclusion, mesh techniques are being used with increasing frequency in hernia surgery in Sweden for both primary and recurrent hernia repairs. Recurrent hernia still represents an important challenge for Swedish hernia surgeons. This register study supports the use of mesh by laparoscopy or anterior tension-free repair for recurrent hernia operations.
Acknowledgments
The authors thank hernia surgeons in participating hospitals for their collaboration. Secretary Gunnel Nordberg and statistician Lennart Gustafsson, PhD, have provided invaluable work for the Swedish Hernia Register.
Footnotes
The Swedish Hernia Register is financially supported by the National Board of Health and Welfare and the Federation of County Councils, Sweden.
Correspondence: Staffan Haapaniemi, MD, Department of Surgery, University Hospital, 581 85 Linköping, Sweden.
E-mail: staffan.haapaniemi@lio.se
Accepted for publication November 15, 2000.
References
- 1.Lawrence K, McWhinnie D, Goodwin A, et al. Randomised controlled trial of laparoscopic versus open repair of inguinal hernia: early results. Br Med J 1995; 311: 981–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gunnarsson U, Heuman R. Recurrence of hernia from the patient perspective [abstract]. Hernia 1999; 3: (suppl 2) S68. [Google Scholar]
- 3.Nilsson E, Haapaniemi S, Gruber G, et al. Methods of repair and risk for reoperation in Swedish hernia surgery 1992–1996. Br J Surg 1998; 85: 1686–1691. [DOI] [PubMed] [Google Scholar]
- 4.Nilsson E, Haapaniemi S. Assessing the quality of hernia repair. In: Fitzgibbons R Jr, Greenburg AG, eds. Hernia. Philadelphia: Lippincott Williams and Wilkins, 2001.
- 5.Lichtenstein IL, Shulman AG, Amid PK, et al. The tension-free hernioplasty. Am J Surg 1989; 157: 188–193. [DOI] [PubMed] [Google Scholar]
- 6.Kald A, Nilsson E, Anderberg B, et al. Reoperation as surrogate endpoint in hernia surgery: A three year follow-up of 1565 herniorrhaphies. Eur J Surg 1998; 164: 45–50. [DOI] [PubMed] [Google Scholar]
- 7.Nilsson E, Haapaniemi S. Hernia registers and specialization. Surg Clin North Am 1998; 78: 1141–1155. [DOI] [PubMed] [Google Scholar]
- 8.Stoppa RE. The preperitoneal approach and prosthetic repair of groin hernias. In: Nyhus LM, Condon RE, eds. Hernia. Philadelphia: JB Lippincott; 1995.
- 9.Wantz GE. Personal experience with the Stoppa technique. In: Nyhus LM, Condon RE, eds. Hernia. Philadelphia: JB Lippincott; 1995.
- 10.Campanelli GP, Cavagnoli R, Gabrielli F, et al. Trabucco’s procedure and local anaesthesia in surgical treatment of inguinal and femoral hernia. Int Surg 1995; 80: 29–34. [PubMed] [Google Scholar]
- 11.Institute of Medicine. Assessing medical technologies. Washington DC: National Academy Press; 1985: 71–71.
- 12.O’Connor GT, Plume SK, Olmstead EM, et al. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. JAMA 1996; 275: 841–846. [PubMed] [Google Scholar]
- 13.Young GJ, Charns MP, Deasi K, et al. Patterns of coordination and clinical outcomes: a study of surgical services. Health Serv Res 1998; 33: 1211–1236. [PMC free article] [PubMed] [Google Scholar]
- 14.Sandblom G, Gruber G, Kald A, et al. Audit and recurrence rates after hernia surgery. Eur J Surg 2000; 166: 154–158. [DOI] [PubMed] [Google Scholar]
- 15.Johanet H, Cossa JP, Marmuse JP, et al. Cure de hernie de l’aine par laparoscopie. Résultats à quatre ans de la voie transprépéritonéale. Ann Chir 1995; 50: 790–794. [PubMed] [Google Scholar]
- 16.O’Dwyer PJ, Duffy K, Taylor S, et al. Scottish audit of groin hernia repair. Hernia 1999; 3 (suppl 2): S88–89. [Google Scholar]
- 17.Haapaniemi S, Nilsson E. Is a questionnaire in combination with selective physical examination enough as follow-up after groin hernia repair? [abstract; in Swedish]. Presented at Surgical Week, Swedish Surgical Society, 1998.
- 18.Marsden AJ. The results of inguinal hernia repairs: a problem of assessment. Lancet 1959; i: 461–462. [DOI] [PubMed] [Google Scholar]
- 19.Shuttleworth KED, Davies WH. Treatment of inguinal herniae. Lancet 1960; i: 126–127. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson E, Haapaniemi S. Quality control and scientific rigour. In: Bendavid R, ed. Hernias of the abdominal wall: principles and management. New York: Springer; 2001.
- 21.Kald A, Anderberg B, Smedh K. Laparoscopic groin hernia repair: results of 200 consecutive herniorrhaphies. Br J Surg 1995; 82: 618–620. [DOI] [PubMed] [Google Scholar]
- 22.Topal B, Hourlay P. Totally preperitoneal endoscopic inguinal hernia repair. Br J Surg 1997; 84: 61–63. [PubMed] [Google Scholar]
- 23.Gianetta E, Cuneo S, Vitale B, et al. Anterior tension-free repair of recurrent inguinal hernia under local anesthesia. Ann Surg 2000; 231: 132–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wantz GE. Complications of inguinal hernia repair. Surg Clin North Am 1984; 64: 287–298. [DOI] [PubMed] [Google Scholar]
- 25.Wellwood J, Sculpher MM, Stoker D, et al. Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. Br Med J 1998; 317: 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johansson B, Hallerbäck B, Glise H, et al. Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair. Ann Surg 1999; 230: 225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoffman HC, Vinton Traverso AL. Preperitoneal prosthetic herniorrhaphy. One surgeon’s successful technique. Arch Surg 1993; 128: 964–970. [DOI] [PubMed] [Google Scholar]
- 28.Janu PG, Sellers KD, Mangiante EC. Recurrent inguinal hernia: preferred operative approach. Am Surg 1998; 6: 569–573. [PubMed] [Google Scholar]
- 29.Callesen T, Bech K, Kehlet H, et al. The feasibility, safety and cost of infiltration anaesthesia for hernia repair. Anaesthesia 1998; 53: 31–35. [DOI] [PubMed] [Google Scholar]
- 30.Millikan KW, Deziel DJ. The management of hernia. Considerations in cost effectiveness. Surg Clin North Am 1996; 76: 105–116. [DOI] [PubMed] [Google Scholar]