Abstract
Objective
To study the effect of Nissen fundoplication on the pattern of gastric emptying and intragastric distribution of symptoms in patients with normal and delayed gastric emptying before surgery, especially in those with delayed emptying before surgery.
Summary Background Data
Gastroesophageal reflux disease is associated with delayed gastric emptying and dyspeptic symptoms in approximately 40% of the patients. After Nissen fundoplication, dyspeptic symptoms are also not uncommon.
Methods
Thirty-six patients (26 men, 10 women, mean age 43.1) were studied before and 3 months after Nissen fundoplication. Gastric emptying (dual-isotope, expressed in lag phase, emptying rate, T50, and intragastric distribution) was not included in the decision for surgery. Reflux-related and dyspeptic symptoms were scored before and at 3, 6, and 12 months after surgery.
Results
Twenty-six patients had normal and 10 had delayed gastric emptying before surgery. Nissen fundoplication on average enhanced gastric emptying for solids in both subgroups by a combination of a decrease in mean lag phase, emptying rate, and T50. The preoperative difference in intragastric distribution between patients with and without delayed gastric emptying was abolished by fundoplication. Patients with normal gastric emptying before surgery showed an increase in early postprandial satiety; in those with delayed emptying, this was not observed. A correlation was found between preoperative T50 for liquid gastric emptying and postoperative nausea at 3 months in patients with normal gastric emptying. In patients with delayed emptying, preoperative correlations between lag phase for liquids and nausea respectively early satiety were significant, as well as for T50 for liquids and vomiting.
Conclusions
Nissen fundoplication equalizes the preoperative difference in intragastric distribution and accelerates gastric emptying without an effect on symptoms in patients with preexisting delayed gastric emptying, but with an increase in early satiety in patients with normal gastric emptying. Delayed gastric emptying is not a contraindication for antireflux surgery.
Gastroesophageal reflux disease (GERD) is associated with delayed gastric emptying for solids and liquids in approximately 40% of the patients. 1–5 Whereas several studies showed that enhancement of delayed gastric emptying by prokinetic drugs improves symptoms of gastroesophageal reflux, 6–9 others found no correlation between reflux and delayed emptying. 3,10–12 Delayed gastric emptying probably plays a causative role in GERD, and delayed gastric emptying has even been considered a contraindication for antireflux surgery. It has been shown that antireflux surgery accelerates gastric emptying, but this does not imply that gastric function has been improved and will have a positive effect on upper gastrointestinal symptoms. 13,14 In the studies presented, patients have not been subdivided in those with and those without delayed emptying before surgery, and such a subdivision has not been related to the surgical outcome. 15–17 Postprandial symptoms of fullness and bloating can mar the otherwise good results of antireflux surgery, and it is conceivable that these gastrointestinal symptoms are induced by alterations in gastric emptying. Thus, the impact of gastric emptying before surgery on outcome has not been thoroughly investigated.
We present a prospective study on the impact of gastric emptying on symptoms and the relation between the pattern of gastric emptying and outcome of antireflux surgery.
METHODS
Subjects
Thirty-six patients (26 men, 10 women, mean age 43.1 years [range 21.7–62.2]) participated in a prospective study. 18 The protocol was approved by the medical ethics committee, and all patients gave written informed consent.
All patients underwent surgery for GERD resistant to medical treatment. Upper gastrointestinal endoscopy confirmed the diagnosis of GERD. Twenty-four-hour pH monitoring and esophageal manometry were routinely performed before and after surgery. A floppy Nissen fundoplication 3 to 3.5 cm in length was performed in all patients. For this purpose, the hiatus and the distal esophagus were dissected free to obtain a 4- to 5-cm segment of distal esophagus in the abdomen. Proximal short gastric vessels were dissected and cut, as were the posterior connections between the spleen, the crural diaphragm, and the esophagogastric junction. Both vagal trunks were identified and included in the wrap. Crural repair was performed in all patients.
Gastrointestinal Symptoms
Reflux-related (heartburn, regurgitation) and upper gastrointestinal symptoms indicative for delayed gastric emptying (early satiety, nausea, vomiting, and belching) were scored from 0 to 5 (no, less than once a month, once a month, once a week, once a day, several times a day) before and at 3, 6, and 12 months after surgery. Scores in patients with normal gastric emptying were compared with those in patients with delayed gastric emptying. Symptoms and emptying rates were calculated and correlated for both groups.
Gastric Emptying Scintigraphy
Gastric emptying studies using a dual-isotope technique were performed after an overnight fast, before and at 3 months after fundoplication. 19 All medication, including proton pump inhibitors, was stopped for at least 72 hours before the study. The solid component of the meal (pancake; 1,240 kJ; 14% protein, 15% fat, 71% carbohydrate) was labeled with 12 MBq 99mTc sulfur colloid and the 150 mL liquid nutrient (dextrose 10%, 250 kJ) was labeled with 4 MBq 111In-DTPA.
Scintigraphic images were acquired in the sitting position with the gamma camera in front of the patient over a 100-minute period after meal ingestion. Data were collected in 1-minute frames and were corrected for movement, Compton scatter, γ-ray attenuation, and radionuclide decay. 19,20 Regions of interest were drawn for the total stomach, the proximal stomach, the distal stomach, and the small intestine to calculate the gastric emptying rate and intragastric transport. 21,22 The time interval between meal ingestion and the first radioactivity in the duodenum (lag phase, minutes), the postlag gastric emptying rate (%/h), and the time for 50% gastric emptying (T50, minutes) were parameters for emptying of solids.
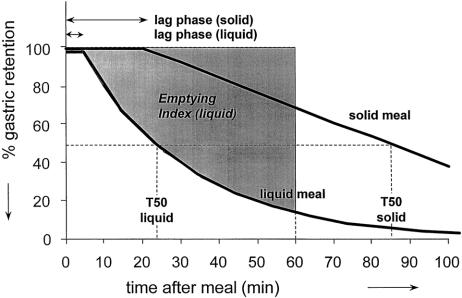
For emptying of liquids, the lag phase, T50, and the emptying index (% * 60 minutes), defined as the area above the curve, measured over 60 minutes after lag phase were the parameters applied (Fig. 1). The emptying index was introduced to overcome difficulties in interpretation of curves not fitting the exponential curve of gastric emptying for liquids. The scintigraphic data were compared with those obtained in 16 healthy volunteers (sex- and age-controlled).
Figure 1. Parameters derived from time-activity curves to describe gastric emptying for a solid and a liquid meal.
For solid gastric emptying (mean [SD]), the lag phase was 25.8 (10.9) and the postlag emptying rate was 33.3 (5.0). For liquid gastric emptying, T50 was 27.7 (15.9) and the emptying index was 0.53 (0.14). Gastric emptying was considered normal if the postlag emptying rate for solids was 25% to 45% per hour. With a postlag emptying rate of less than 25%, gastric emptying was considered to be delayed.
Mean time-activity curves were created for both groups, with separate curves for the proximal and distal stomach to illustrate intragastric distribution in relation to time after ingestion. To investigate the relationship between symptoms and gastric emptying, symptoms and gastric emptying before and 3 months after fundoplication were correlated. In addition, we investigated the relationship between preoperative gastric emptying and postoperative symptoms at 3 months after fundoplication.
Statistical Analysis
Data are expressed as means (SD). The paired-samples t test was used to compare preoperative and postoperative gastric emptying data for both groups. The Wilcoxon signed-rank test was used to compare ordinal symptom score data. The Mann-Whitney test was used to compare gastric emptying and gastrointestinal symptoms between the groups. Correlations between preoperative and postoperative gastrointestinal symptoms and emptying were calculated using the Spearman rank correlation test for each group. Friedman analysis of variance was used to test the effect of time on dyspeptic symptoms at 3, 6, and 12 months in each group. Significance level was set at P < .05.
RESULTS
One patient experienced severe postoperative dysphagia lasting more than 3 months, necessitating further treatment with successful outcome. There were three postoperative complications: pneumothorax in two (one had pneumonia) and wound infection in one. Recurrent GERD with symptoms and pathologic esophageal acid exposure was not observed at 3 months.
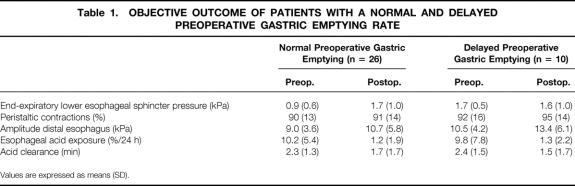
Twelve months after surgery, two patients with preoperative normal gastric emptying had recurrent GERD requiring reoperation. The results of preoperative and postoperative esophageal manometry and 24-hour pH studies are described in Table 1, showing no difference in objective outcome between patients with a decreased and normal preoperative gastric emptying rate. There were no postoperative deaths.
Table 1. OBJECTIVE OUTCOME OF PATIENTS WITH A NORMAL AND DELAYED PREOPERATIVE GASTRIC EMPTYING RATE
Values are expressed as means (SD).
Symptoms
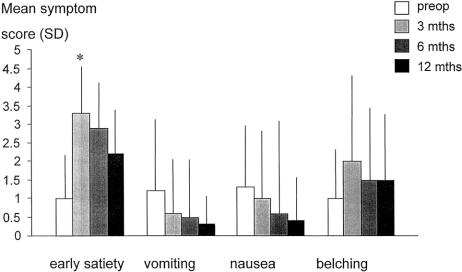
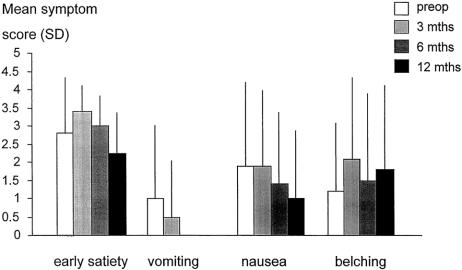
Before surgery, patients with delayed preoperative gastric emptying showed significantly more early satiety (2.8 [1.60] vs. 1.0 [1.2], P < .01) than patients with normal gastric emptying (Figs. 2 and 3).
Figure 2. Mean (SD) gastrointestinal symptoms scores (0–5) in 26 patients with normal preoperative gastric emptying (solid meal), before and at 3, 6, and 12 months after Nissen fundoplication. Early satiety increased significantly 3 months after surgery (*P < .01).
Figure 3. Mean (SD) gastrointestinal symptoms scores (0–5) in 10 patients with delayed preoperative gastric emptying (solid meal), before and at 3, 6, and 12 months after Nissen fundoplication.
Heartburn and regurgitation were significantly reduced for all patients at 3, 6, and 12 months after fundoplication (P < .01 for all patients).
Analysis of Gastric Emptying
Solids
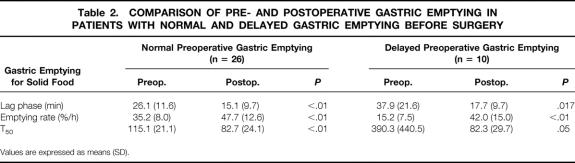
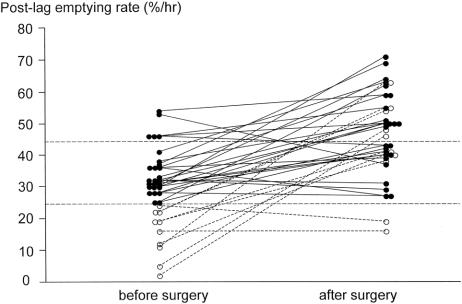
Gastric emptying was delayed in 10 patients before surgery. After fundoplication, return to normal was observed in three and acceleration was observed in five; in the remaining two, gastric emptying was not affected. Nissen fundoplication on average accelerated gastric emptying both in patients with normal and delayed gastric emptying before surgery (Table 2, Fig. 4). There was a significant decrease in lag phase for both subgroups (P < .01) and an increase in emptying rate and T50 after surgery (P < .01).
Table 2. COMPARISON OF PRE- AND POSTOPERATIVE GASTRIC EMPTYING IN PATIENTS WITH NORMAL AND DELAYED GASTRIC EMPTYING BEFORE SURGERY
Values are expressed as means (SD).
Figure 4. Gastric emptying for a solid meal (postlag emptying rate) in 26 patients with normal and 10 patients with delayed gastric emptying (%/h) before and after Nissen fundoplication. Normal range lies between dotted lines.
Before surgery, no difference in lag phase was found between the groups, but patients with delayed gastric emptying before surgery had a significantly lower activity in the antrum at 30 and 50 but not at 80 minutes after ingestion.
Intragastric Distribution
Before surgery, 10 minutes after ingestion of a solid meal, 79% of the ingested radioactivity was found in the proximal stomach and 21% in the distal stomach, for patients with delayed gastric emptying before surgery. This was significantly different from the preoperative distribution in patients with normal gastric emptying (64% in proximal stomach vs. 36% in the distal stomach, P = .03). After surgery, intragastric distribution at 10 minutes was similar in both groups (51% in the proximal stomach and 49% in the distal stomach). The effects of surgery on the whole stomach, the gastric fundus, and the antrum in both groups of patients are presented in Figure 5.
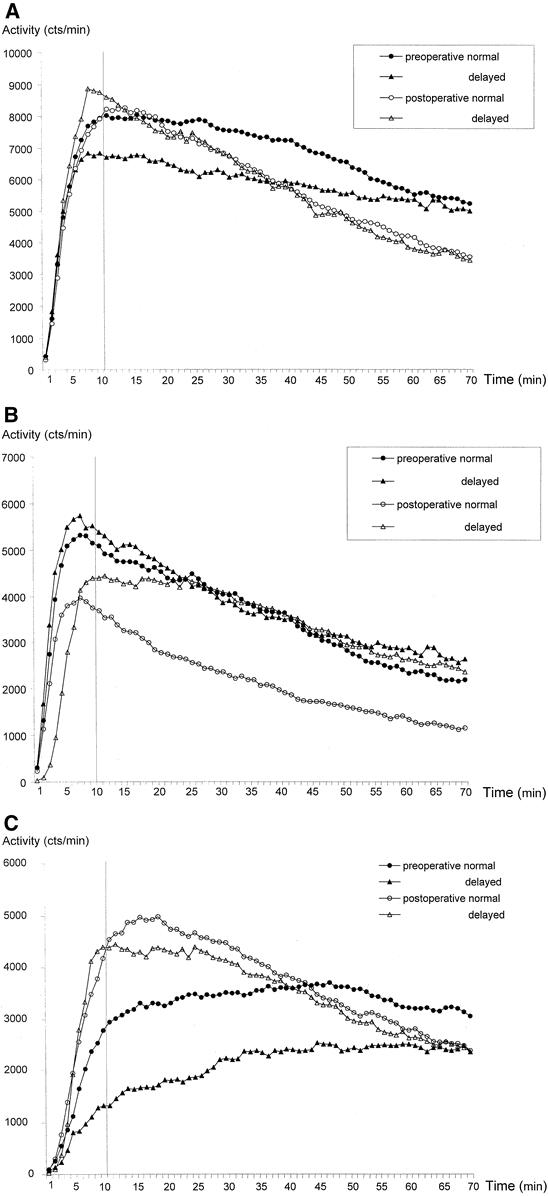
Figure 5. The effect of Nissen fundoplication on the whole stomach (A), the gastric fundus (B), and the antrum (C).
Liquids
Before surgery, only three patients had delayed gastric emptying for liquids, which was observed in combination with delayed gastric emptying for solids in two, so no subdivision was made for delayed and normal liquid emptying. After surgery, all values were within the normal range. Nissen fundoplication shortened the lag phase (4.8 [3.3] to 2.6 [2.1], P < .01) and the emptying index (0.49 [0.1] vs. 0.57 [0.09], P < .01) but without affecting the T50 (25.1 [17.3] vs. 18.9 [10.3]. P = .12).
Relation between Upper Gastrointestinal Symptoms and Gastric Emptying
Patients with normal preoperative gastric emptying showed an increase in early postprandial satiety (P < .001) at 3 months (see Fig. 2). The severity of early satiety, vomiting, and nausea showed a trend to return to normal over time; belching did not (see Figs. 2 and 3). Early satiety showed a significant decrease from 3 to 12 months in both groups (P < .01). In patients with delayed gastric emptying, preoperative correlations between lag phase for liquids on the one hand and nausea and early satiety on the other were significant (r = 0.72, P = .02 respectively r = 0.84, P = .03), as well as for T50 for liquids and vomiting (r = 0.74, P = .014). After surgery, gastric emptying for solids correlated with nausea (r = 0.66, P = .04).
Patients with normal gastric emptying showed a significant correlation between preoperative T50 for liquids and nausea at 3 months (r = 0.54, P = .04), and after Nissen fundoplication gastric emptying for solids was correlated with vomiting (r = 0.41, P = .04).
DISCUSSION
This study is the first to show that fundoplication has an impact on intragastric distribution as a potential explanation for postoperative upper gastrointestinal symptoms, and that delayed gastric emptying before surgery does not adversely affect the outcome of surgery. Our results also show that enhancement of gastric emptying has no beneficial effect on symptoms of delayed emptying and is responsible for the induction or increase of symptoms such as nausea, early satiety, and belching in those with normal gastric emptying before surgery. Our results confirm the observation of others that fundoplication accelerates gastric emptying and can induce upper gastrointestinal symptoms. 13
Nissen fundoplication accelerated gastric emptying for both solids and liquids in most of our patients. These results are consistent with other studies confirming enhancement of gastric emptying by Nissen fundoplication, 23–25 whereas partial fundoplication 26 or Angelchik prosthesis 27 had either no or only a limited effect on emptying rates. Altered reservoir function of the fundus after fundoplication with increased gastric tone as the result of a decreased capacity 23 or a redistribution of gastric contents from fundus to antrum caused by the change in gastric anatomy are the mechanisms proposed for enhancement of gastric emptying.
Hinder et al 16 studied 25 patients with delayed gastric emptying before fundoplication and observed upper gastrointestinal symptoms in 7 after surgery. Five of them had either delayed or accelerated gastric emptying. They concluded that abnormal gastric emptying, delay or acceleration, after Nissen was the cause of upper gastrointestinal symptoms. Lundell et al 17 found that delayed gastric emptying (for solids) before surgery was correlated with postoperative dysphagia, postprandial distention, early satiety, and gas bloating. They also concluded that abnormalities in gastric motor function might play a role in bloating symptoms.
It has so far not been elucidated how these alterations are brought about, how they relate to the changes in gastric emptying, and how they affect symptoms. Three aspects of gastric function must be taken into consideration: adaptive relaxation, compliance, and (visceral) perception. After ingestion of solid and liquid nutrients, the interaction of these mechanisms determines the pattern of gastric emptying and the symptomatic response.
The enhancement of gastric emptying in both groups can partly be explained by the combination of the alterations in anatomy (full mobilization of the fundus, division of all short gastric vessels, and a 360-degree wrap of 3–3.5 cm in length) 28 and the decrease in adaptive relaxation of the stomach after fundoplication. 25,29 These studies using the barostat have shown a significant decrease in adaptive relaxation after Nissen fundoplication without an effect on compliance. Apparently, therefore, the viscoelastic properties of muscle and fibrous tissue are not affected by antireflux surgery. In that study, however, no subdivision between normal and delayed gastric emptying before surgery was made. Partial local denervation as a result of the dissection of the whole fundus can add to the decrease in adaptive relaxation. The suggestion is supported by the observation that proximal gastric vagotomy had an additional effect on already accelerated gastric emptying, as shown by Jamieson. 30 Partial fundoplication with, obviously, less impact on fundal anatomy had less effect on gastric emptying. 26
The combination of alterations in anatomy with a decrease in adaptive relaxation is also likely to play a role in the accelerated transport of solids after fundoplication. The antrum plays a major role in controlling gastric emptying for solids, as shown in humans by Camilleri et al, who found a positive correlation between gastric emptying and antral motility. 31 These observations are in line with our results, showing enhancement of intragastric transport after fundoplication, apparently with promotion of antral peristalsis, and acceleration of gastric emptying for solids.
Alterations in gastric emptying have been considered a risk factor for the outcome of fundoplication. 15,16 This has prompted others 32 to perform pyloroplasty or pyloromyotomy in patients with delayed emptying on preoperative workup. Having observed that T50 is in the same range after surgery irrespective of the preoperative emptying, it seems that pyloroplasty is superfluous and may be even harmful because of the risk of inducing duodenogastric reflux and gastritis. Postfundoplication symptoms can overshadow the positive effect on GERD symptoms; therefore, preoperative selection and exclusion of patients with delayed gastric emptying might result in better outcome. We showed that Nissen fundoplication indeed accelerates intragastric distribution, which might be an explanation for the postoperative increase in bloating. In contrast to the common belief, this had no effect on the symptom scores, except for postprandial satiety. Interpretation of symptoms based on motor function is difficult because of the interindividual differences in visceral perception and response to distention of the fundus, corpus, and antrum. 33–35
How can the difference in symptomatic response between the two groups be understood when they had the same operation, the same anatomic changes, and roughly the same enhancement in gastric emptying?
Like patients after antireflux surgery, patients with functional dyspepsia also have decreased adaptive relaxation, but they may also have altered visceral perception, which may be responsible for their symptoms. 36,37 This is also shown in patients with diabetes mellitus. 38
No such pattern has been shown in this group of patients with GERD. It even seems that patients with delayed gastric emptying in this study tended to have a decrease in visceral perception. They did not react with an increase in dyspeptic symptoms after surgery, whereas patients with normal gastric emptying translated the acceleration of emptying into early satiety, albeit transient.
In summary, Nissen fundoplication leads to enhancement of gastric emptying by a combination of a decrease in fundal reservoir with a decrease in adaptive relaxation. This leads to accelerated intragastric transport with an increase in antral motility and enhanced emptying. As a result of potential differences in visceral perception, these alterations are perceived as early satiety in patients with normal gastric emptying before surgery and not so much by patients with delayed emptying before surgery.
Because delayed gastric emptying before antireflux surgery does not lead to an increase in upper gastrointestinal symptoms and has no adverse effect on the outcome of surgery, both in terms of symptoms and objective reflux control, we propose that delayed gastric emptying does not represent a contraindication for antireflux surgery. Therefore, there is no need for gastric emptying studies to be performed routinely before antireflux surgery.
Acknowledgment
The authors thank Mrs. Alice van Dongen, research staff member of the Department of Nuclear Medicine, for her assistance.
Footnotes
Correspondence: Hein G. Gooszen, PhD, Professor of Surgery, University Medical Center Utrecht, P.O. Box 85500, 3508 GA Utrecht, The Netherlands.
E-mail: h.gooszen@chir.azu.nl
Accepted for publication January 28, 2001.
References
- 1.Little AG. Gastro-oesophageal reflux and oesophageal motility diseases. Who should perform antireflux surgery? Ann Chir Gynaecol 1995; 84: 103–105. [PubMed] [Google Scholar]
- 2.McCallum RW, Berkowitz DM, Lerner E. Gastric emptying in patients with gastroesophageal reflux. Gastroenterology 1981; 80: 285–291. [PubMed] [Google Scholar]
- 3.Schwizer W, Hinder RA, DeMeester TR. Does delayed gastric emptying contribute to gastroesophageal reflux disease? Am J Surg 1989; 157: 74–81. [DOI] [PubMed] [Google Scholar]
- 4.Little AG, DeMeester TR, Kirchner PT, et al. Pathogenesis of esophagitis in patients with gastroesophageal reflux. Surgery 1980; 88: 101–107. [PubMed] [Google Scholar]
- 5.Maddern GJ, Chatterton BE, Collins PJ, et al. Solid and liquid gastric emptying in patients with gastro-oesophageal reflux. Br J Surg 1985; 72: 344–347. [DOI] [PubMed] [Google Scholar]
- 6.McCallum RW, Fink SM, Lerner E, et al. Effects of metoclopramide and bethanechol on delayed gastric emptying present in gastroesophageal reflux patients. Gastroenterology 1983; 84: 1573–1577. [PubMed] [Google Scholar]
- 7.McCallum RW. Gastric emptying in gastroesophageal reflux and the therapeutic role of prokinetic agents. Gastroenterol Clin North Am 1990; 19: 551–564. [PubMed] [Google Scholar]
- 8.Maddern GJ, Jamieson GG, Myers JC, et al. Effect of cisapride on delayed gastric emptying in gastro-oesophageal reflux disease. Gut 1991; 32: 470–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fink SM, Lange RC, McCallum RW. Effect of metoclopramide on normal and delayed gastric emptying in gastroesophageal reflux patients. Dig Dis Sci 1983; 28: 1057–1061. [DOI] [PubMed] [Google Scholar]
- 10.Shay SS, Eggli D, McDonald C, et al. Gastric emptying of solid food in patients with gastroesophageal reflux. Gastroenterology 1987; 92: 459–465. [DOI] [PubMed] [Google Scholar]
- 11.Keshavarzian A, Bushnell DL, Sontag S, et al. Gastric emptying in patients with severe reflux esophagitis. Am J Gastroenterol 1991; 86: 738–742. [PubMed] [Google Scholar]
- 12.Benini L, Sembenini C, Castellani G, et al. Gastric emptying and dyspeptic symptoms in patients with gastroesophageal reflux. Am J Gastroenterol 1996; 91: 1351–1354. [PubMed] [Google Scholar]
- 13.Negre JB. Post-fundoplication symptoms; do they restrict the success of Nissen fundoplication? Ann Surg 1983; 198: 698–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rantanen TK, Salo JA, Salminen JT, et al. Functional outcome after laparoscopic or open Nissen fundoplication: a follow-up study. Arch Surg 1999; 134: 240–244. [DOI] [PubMed] [Google Scholar]
- 15.Maddern GJ, Jamieson GG, Chatterton BE, et al. Is there an association between failed antireflux procedures and delayed gastric emptying? Ann Surg 1985; 202: 162–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinder RA, Stein HJ, Bremner CG, et al. Relationship of a satisfactory outcome to normalization of delayed gastric emptying after Nissen fundoplication. Ann Surg 1989; 210: 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lundell LR, Myers JC, Jamieson GG. Delayed gastric emptying and its relationship to symptoms of “gas bloat” after antireflux surgery. Eur J Surg 1994; 160: 161–166. [PubMed] [Google Scholar]
- 18.Bais JE, Bartelsman JFWM, Bonjer HJ, et al. Laparoscopic or conventional Nissen fundoplication for gastro-oesophageal reflux disease. Lancet 2000; 355: 170–174. [DOI] [PubMed] [Google Scholar]
- 19.Collins PJ, Horowitz M, Cook DJ, et al. Gastric emptying in normal subjects: a reproducible technique using a single scintillation camera and computer system. Gut 1983; 24: 1117–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akkermans LM, van Isselt J. Gastric motility and emptying studies with radionuclides in research and clinical settings. Dig Dis Sci 1994; 39: S95–96. [DOI] [PubMed] [Google Scholar]
- 21.Ropert A, des VS, Bizais Y, et al. Simultaneous assessment of liquid emptying and proximal gastric tone in humans. Gastroenterology 1993; 105: 667–664. [DOI] [PubMed] [Google Scholar]
- 22.Troncon LE, Rosa Oliveira RB, Iazigi N, et al. Abnormal intragastric distribution of a liquid nutrient meal in patients with diabetes mellitus. Dig Dis Sci 1998; 43: 1421–1429. [DOI] [PubMed] [Google Scholar]
- 23.Maddern GJ, Jamieson GG. Fundoplication enhances gastric emptying. Ann Surg 1985; 201: 296–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Viljakka M, Saali K, Koskinen M, et al. Antireflux surgery enhances gastric emptying. Arch Surg 1999; 134: 18–21. [DOI] [PubMed] [Google Scholar]
- 25.Vu MK, Straathof JW, Schaar PJ, et al. Motor and sensory function of the proximal stomach in reflux disease and after laparoscopic Nissen fundoplication. Am J Gastroenterol 1999; 94: 1481–1489. [DOI] [PubMed] [Google Scholar]
- 26.Velasco N, Hill LD, Gannan RM, et al. Gastric emptying and gastroesophageal reflux. Effects of surgery and correlation with esophageal motor function. Am J Surg 1982; 144: 58–62. [DOI] [PubMed] [Google Scholar]
- 27.Maddern GJ, Myers JC, McIntosh N, et al. The effect of the Angelchik prosthesis on esophageal and gastric function. Arch Surg 1991; 126: 1418–1422. [DOI] [PubMed] [Google Scholar]
- 28.Samsom M, Brinkmann H, Lighvani SS, et al. Gastric accommodation measured noninvasively in post-fundoplication and non-ulcer dyspepsia patients. Gastroenterology 2000, 113: A2044. [Google Scholar]
- 29.Wijnhoven BP, Salet GA, Roelofs JM, et al. Function of the proximal stomach after Nissen fundoplication. Br J Surg 1998; 85: 267–271. [DOI] [PubMed] [Google Scholar]
- 30.Jamieson GG, Maddern GJ, Myers JC. Gastric emptying after fundoplication with and without proximal gastric vagotomy. Arch Surg 1991; 126: 1414–1417. [DOI] [PubMed] [Google Scholar]
- 31.Camilleri M, Malagelada JR, Brown ML, et al. Relation between antral motility and gastric emptying of solids and liquids in humans. Am J Physiol 1985; 249: G580–585. [DOI] [PubMed] [Google Scholar]
- 32.Patti MG, Arcerito M, Pellegrini CA, et al. Minimally invasive surgery for gastroesophageal reflux disease. Am J Surg 1995; 170: 614–617. [DOI] [PubMed] [Google Scholar]
- 33.Troncon LE, Bennett RJ, Ahluwalia NK, et al. Abnormal intragastric distribution of food during gastric emptying in functional dyspepsia patients. Gut 1994; 35: 327–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moragas G, Azpiroz F, Pavia J, et al. Relations among intragastric pressure, postcibal perception, and gastric emptying. Am J Physiol 1993; 264: G1112–1117. [DOI] [PubMed] [Google Scholar]
- 35.Azpiroz F, Malagelada JR. Perception and reflex relaxation of the stomach in respons to gut distention. Gastroenterology 1990; 98: 1193–1198. [DOI] [PubMed] [Google Scholar]
- 36.Salet GA, Samsom M, Roelofs JM, et al. Responses to gastric distension in functional dyspepsia. Gut 1998; 42: 823–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tack J, Piessevaux H, Coulie B, et al. Role of impaired gastric accomodation to a meal in functional dyspepsia. Gastroenterology 1998; 115: 1346–1352. [DOI] [PubMed] [Google Scholar]
- 38.Samsom M, Roelofs JM, Akkermans LM, et al. Proximal gastric motor activity in response to a liquid meal in type I diabetes mellitus with autonomic neuropathy. Dig Dis Sci 1998; 43: 491–496. [DOI] [PubMed] [Google Scholar]