Abstract
Objective
To establish selection criteria for reoperation in patients with peritoneal dissemination from appendiceal malignancy.
Summary Background Data
The outcome of patients with mucinous appendiceal neoplasms with peritoneal surface dissemination has changed as a result of a better understanding of the clinical and pathologic features of this disease. This knowledge, combined with aggressive strategies for the use of perioperative intraperitoneal chemotherapy and peritonectomy procedures, has resulted in long-term disease-free survival in many of these patients. However, some of the patients develop progressive disease, and a question regarding additional surgery is appropriate. A critical analysis of the results of second-look surgery should assist in the management of patients with recurrent peritoneal surface dissemination of an appendiceal neoplasm.
Methods
Three hundred twenty-one patients with epithelial peritoneal surface malignancy of appendiceal origin underwent surgery during a 12-year period. Ninety-eight of these patients (30.5%) underwent a second-look procedure. A database of selected clinical features regarding these 98 patients was gathered from the clinical records. A critical statistical analysis of these clinical features and their prognostic impact was performed using survival as an endpoint. All patients were managed by a treatment regimen that used cytoreductive surgery and intraperitoneal chemotherapy.
Results
The overall 5-year survival rate of these 98 patients was 73.6%. This compared favorably with a 68% survival rate of 223 patients who did not undergo reoperation. Survival based on the number of cytoreductive surgeries and the free interval between them showed no significant difference. Patients who had second-look surgery with bowel obstruction as a symptom and those in whom the amount of tumor was increased or minimally decreased at the first and second cytoreductions had a significantly inferior 5-year survival rate. A complete second cytoreduction was associated with an improved 5-year survival rate.
Conclusions
Follow-up of patients treated for peritoneal dissemination from neoplasms of appendiceal origin is indicated. Selected patients in whom recurrence develops are candidates for repeat cytoreductive surgery plus intraperitoneal chemotherapy with curative intent.
Peritoneal surface dissemination of pseudomyxoma peritonei and of adenocarcinomas of appendiceal origin has a perforated appendiceal tumor as the primary site of disease. 1 Mucinous ascites and mucus-producing epithelial cells from the appendiceal tumor accumulate and progress, with a characteristic distribution throughout the abdomen and pelvis. Copious mucinous ascites and tumors distend the peritoneal cavity over time and eventually bring intestinal function to a halt. In the past, treatment involved repeated debulking procedures over several years. The goal of this surgery was to relieve the abdominal distention by evacuating all free mucus, irrigating vigorously, and wiping the peritoneal surfaces as clean as possible. All solid tumor except that contained within the greater omentum remained. 2
With repeated debulking procedures, the natural history of appendiceal malignancy is characterized by progression of both mucinous tumor and intestinal adhesions until there are no further surgical options. All patients die of gradual progressive intestinal obstruction and terminal starvation. Gough et al 3 at the Mayo Clinic followed up 56 patients treated by reoperation over a 26-year period. In the absence of special treatments, disease-free survival was approximately 2.5 years, and only a few patients were disease-free after 5 years. One of us 4 showed a median survival of 2 years in patients who had incomplete cytoreduction.
Better understanding of the clinical and pathologic features of the disease, combined with aggressive use of peritonectomy procedures and intraperitoneal chemotherapy, has changed the outcome for these patients. Treatment of a large number of patients resulted in a standardized plan of management. 4,5 The goal of treatment has been changed from palliative to curative intent. However, about one third of patients who underwent cytoreduction with perioperative intraperitoneal chemotherapy developed progressive disease and could be considered candidates for additional treatment.
The purpose of this study was to critically evaluate all patients who had peritoneal surface spread of an appendiceal neoplasm and a second-look surgery. Our goal was to establish selection criteria for reoperation. This was done by performing a statistical analysis of clinical factors that influenced outcome, with survival as an endpoint. These data should facilitate better clinical management.
PATIENTS AND METHODS
Patients
From February 1985 to September 1997, 321 patients with the diagnosis of an epithelial peritoneal surface malignancy of appendiceal origin were treated using a standardized management plan with cytoreductive surgery and perioperative intraperitoneal chemotherapy. 5 This group of patients represents the complete surgical experience with this disease during this period; no patients were eliminated from the data analysis. No patients were lost to follow-up. Ninety-eight of these patients (30.5%) underwent at least one second-look surgery with repeat cytoreductive surgery plus perioperative intraperitoneal chemotherapy if indicated. A statistical analysis of these 98 patients constitutes the basis of our study.
Precytoreduction Data
The preoperative workup was aimed at quantitative evaluation of the biologic aggressiveness, distribution, and extent of abdominopelvic disease. Clinical examination included a detailed history and physical examination. Laboratory examination included a tumor marker panel with carcinoembryonic antigen, CA 19-9, CA-125, CA 15.3, and CA 72.4. Upper gastrointestinal series or barium enemas were performed as needed but were rarely indicated. After bowel preparation, a computed tomography (CT) scan was obtained of the chest, abdomen, and pelvis with maximum oral, intravenous, and intrarectal contrast. 6,7 Surgical reports, pathology reports, and pathology slides from prior surgical procedures were reviewed in all patients before the first cytoreduction at our institution.
Management by Cytoreduction Plus Intraperitoneal Chemotherapy
Three hundred twenty-one patients with an epithelial peritoneal surface malignancy of appendiceal origin underwent cytoreductive surgery. The goal of surgery was to remove all clinical evidence of disease if possible. The cytoreductive surgery consisted of an exploratory laparotomy with lysis of all intraabdominal adhesions and determination of the peritoneal cancer index (PCI). 8 Using extensive electrosurgery, one to six peritonectomy procedures and appropriate gastrointestinal resections were performed to remove all visible tumor. 9,10 All patients received perioperative intraperitoneal chemotherapy with mitomycin C and 5-fluorouracil. In the initial 94 patients, the mitomycin C was given as early postoperative intraperitoneal chemotherapy on postoperative day 1 at a dose of 12.5 mg/m2 for men and 10 mg/m2 for women. 11 After January 1995, the same dose of mitomycin C was given in the operating room with 41° to 42°C heat and manual distribution of the chemotherapy solution. 5 The 5-fluorouracil has always been given at 650 mg/m2 as early postoperative intraperitoneal chemotherapy on postoperative days 2 to 6 or 1 to 5. 5 The initial 94 patients who received early postoperative intraperitoneal mitomycin C also received three cycles of combined intravenous mitomycin C and intraperitoneal 5-fluorouracil. A completeness of cytoreduction (CC) score was determined at the completion of surgery.
Data Analysis
The clinical features selected for analysis with survival as an endpoint were age; sex; tumor marker elevation before and after the first cytoreduction; CT of the chest, abdomen, and pelvis before and after the first cytoreduction; PCI at the first cytoreduction and at second-look surgery; CC score at the first and at the second cytoreduction; histopathologic type of tumor (adenomucinosis, hybrid morphology, mucinous carcinoma); time interval between first and second surgery (<1 year, 1–2 years, 2–3 years, >3 years); indication for second-look surgery (planned, abnormal CT scan in follow-up, intestinal obstruction, increasing tumor marker, other); number of cytoreductive surgeries (one, two, three, four); and percentage change in PCI (no change or an increase, decrease 1–50%, decrease 51–99%, decrease 100%). The significance of each of these clinical features was analyzed. A Kaplan-Meier survival curve was fitted to the data and tested using a log-rank test for difference between the curves. The response variable was survival (in months) for the clinical features that were compared. The probability values were calculated for each analysis. The follow-up was 100%, and no patients were censored from the data analysis.
Standard follow-up protocol after the first cytoreductive surgery consisted of assays of the appropriate tumor marker selected from the panel by a preoperative determination every 3 months and a CT scan of the chest, abdomen, and pelvis with maximum oral, intravenous, and intrarectal contrast every 6 months.
Quantitative Prognostic Indicators for Peritoneal Surface Malignancy
The PCI was a combined score of the distribution of tumor implants and their mass. 8 The score was determined after a thorough exploration of the abdomen and pelvis. The abdominopelvic area was divided into nine regions and the small bowel into four regions. Each of these regions was scored for implant size on a scale of 0 to 3 (0, no visible tumor implants; 1, implants <0.50 cm in greatest diameter; 2, implants 0.50–5.0 cm; 3, implants >5.0 cm or a confluence of implants). The PCI was the sum of scores from all 13 abdominopelvic regions (0–39).
The CC score was an assessment of the largest tumor mass left behind after the removal of tumor. 12 In contrast to the PCI, the abdomen and pelvis were scored as a single unit after the surgery was completed (0, no visible evidence of tumor, but microscopic residual disease assumed; 1, tumor implants <0.25 cm in greatest dimension; 2, tumor implants 0.25–2.5 cm in greatest dimension; 3, tumor nodules >2.5 cm in greatest dimension or a confluence of nodules). Patients with a CC score of 0 and 1 were designated as having had complete cytoreduction.
Histologic Type of Mucinous Tumor
The histologic type of mucinous tumor was scored as 1 to 3.3. 13 A score of 1 indicated adenomucinosis: scant epithelial cells existed as single cells or as a single layer surrounding a glandular structure, fibrous matrix was minimal, and epithelial cells appeared bland without atypia or mitoses. A score of 2 indicated a hybrid morphology of adenomucinosis and mucinous adenocarcinoma; the large majority of the tumor mass was typical of adenomucinosis, but areas of cellular atypia, a confluence of glandular structures, and a well-organized fibrous stroma were apparent. A score of 3 indicated mucinous adenocarcinoma; signet ring morphology was apparent and cellular atypia was more evident throughout the specimen.
Lymph node status was determined within ileocolic and right colic nodes both at the time of initial appendiceal malignancy treatment and at the time of definitive cytoreduction. The presence versus absence of appendiceal malignancy in lymph nodes was analyzed for its impact on survival.
Interval Between First Cytoreduction and Second-Look Procedure
This interval was defined as the time elapsed between the first and second cytoreductive procedures. Patients were classified into those who had the second-look surgery within 1 year, those who had the second-look surgery between 1 and 2 years, those who had it between 2 and 3 years, and those who had it after 3 years.
Indication for Second-Look Surgery
Patients were classified into one of the following groups based on the indication for their second-look surgery. In group 1, a second-look procedure was planned at the time of the first cytoreduction. Usually these patients had a temporary ostomy that needed to be reversed. The second-look surgery in this group of patients occurred 6 months after the first cytoreduction. Group 2 consisted of patients who had an abnormal CT scan on follow-up but were asymptomatic. Group 3 comprised patients who underwent reoperation because of signs and symptoms of intestinal obstruction regardless of normal or abnormal tumor markers or CT scans. Group 4 comprised patients who underwent reoperation because they had a rising tumor marker but had no significant findings on CT or physical examination and were clinically asymptomatic. Group 5 consisted of all the other patients who underwent reoperation but could not be categorized in any of the above groups. Indications for reoperation in this group included, but were not limited to, tumor in the abdominal wall, severe bile reflux, and incisional hernia. The time selected for surgical intervention of groups 2 through 5 was the time at which the clinical information suggested recurrent malignancy.
Number of Cytoreductive Surgeries
Of the original 321 patients with peritoneal dissemination of a perforated appendiceal tumor, 98 underwent a second-look surgery. Sixteen of these 98 patients underwent a third surgery and 3 of them had a fourth surgery. The timing of all third and fourth surgeries was determined by the clinical status of the patient, with no predetermined interventions.
Percentage Change in Peritoneal Cancer Index
As previously described, the PCI is a quantitative assessment of the amount of disease present in the abdominopelvic regions and on small bowel visually determined at the time of abdominal exploration. Patients were evaluated by comparing the PCI at the time of their first cytoreductive surgery with the score at the time of their second-look surgery. Based on the percentage change, the patients were categorized into one of four groups: group 1, the score was the same or had increased; group 2, the score had decreased by 1% to 50%; group 3, the score had decreased by 51% to 99%; group 4, no tumor was found at the second-look surgery (decrease of 100%).
Statistical Evaluation
The comparison of patients’ clinical characteristics was conducted using chi-square or the Fisher exact chi-square test for categorical variables; the Student t test or analysis of variance was used for continuous variables. For patient survival analysis, Kaplan-Meier survival curves were plotted and tested by log-rank test.
RESULTS
Of the 321 patients treated for peritoneal surface spread of an appendiceal malignancy, 98 (30.5%) required second-look surgery. The overall 5-year survival rate of these 98 patients was 73.6%. This compared favorably with a 5-year survival rate of 68% for patients who did not undergo a reoperation. The time to disease progression and the overall survival are shown in Figure 1.
Figure 1. Kaplan-Meier distribution showing disease-free survival (interval between first cytoreduction and second-look surgery) and overall survival from time of second-look surgery.
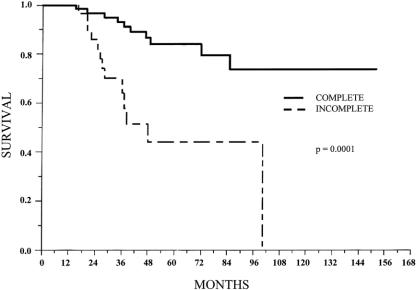
In the patients who underwent second-look surgery, the CC score was not a significant prognosticator at the first cytoreduction (P = .1626), but it was a robust prognosticator at the second-look surgery. Sixty-seven patients who had a complete second cytoreduction had a 5-year survival rate of 84%; when the second cytoreduction was incomplete, the 5-year survival rate dropped to 44% (Fig. 2). The comparison was significant (P = .0001 (Table 1).
Figure 2. Survival distribution by completeness of cytoreduction at second-look procedure.
Table 1. CLINICAL FEATURES AT THE SECOND-LOOK SURGERY AND THEIR PROGNOSTIC IMPACT
Survival computed from the time of the first cytoreduction.
Table 1 shows an evaluation of the patients based on the interval between the first cytoreduction and second-look surgery. There was a 5-year survival rate of 82% for patients who had their second surgery within 1 year of the first. Survival decreased to 67% with a 2-year interval and dropped even more with a 3-year interval (27%). Patients who required a second-look surgery after 3 years from the first cytoreduction had an increase in survival to 63%. The interval between the first cytoreduction and second-look surgery did not have a significant impact on survival (P = .248).
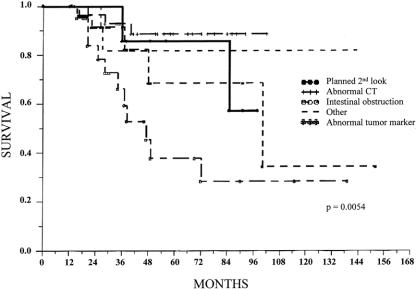
There was no significant difference in survival if the second cytoreductive surgery was either a planned one for a closure of an ostomy or the operation was dictated because the patient had an increasing tumor marker or an abnormal CT scan (Fig. 3). All these patients were asymptomatic. However, if the indication for the second-look surgery was intestinal obstruction, the 5-year survival rate decreased significantly (P = .0054; see Table 1).
Figure 3. Survival distribution by indication for second-look surgery.
The number of cytoreductions in these patients varied from two to six. Seventy-nine patients had a second cytoreduction, 16 had a third cytoreduction, and 3 had a fourth or greater cytoreduction. The effect of the number of cytoreductions on the 5-year survival rate showed borderline significance (P = .069). There was a trend toward improved outcome if patients were selected for multiple cytoreductions.
Patients were analyzed comparing the PCI at the first cytoreductive surgery with the PCI at the second-look surgery. The impact of change in the PCI is shown in Table 2. Survival was significantly reduced if the PCI at the second surgery was the same or greater than at the first. Also, survival was diminished if the PCI was only modestly reduced from the first cytoreduction. If the PCI had decreased 50% or more at the second-look surgery, the survival rate improved. These differences were significant (P < .0001;Fig. 4).
Table 2. IMPACT OF CHANGE IN PERITONEAL CANCER INDEX (PCI)
* Data are given as mean ± SD.
Figure 4. Survival distribution by change in peritoneal cancer index. Survival time was determined from time of second-look surgery.
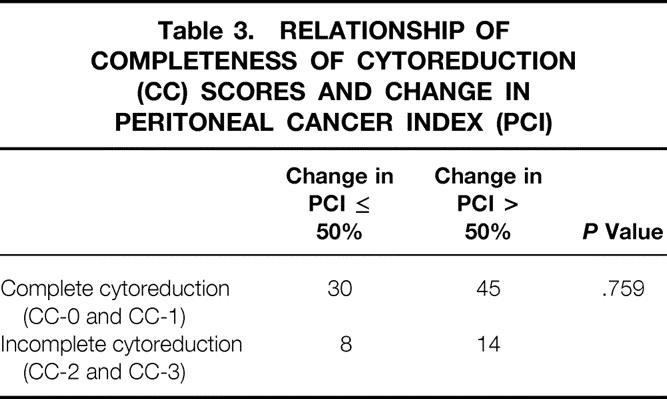
A statistical relationship was sought between the CC score at the first cytoreduction and the change in the PCI. To perform this analysis, the groups of patients with complete cytoreduction and incomplete cytoreduction were compared with the groups of patients with a 50% or less decrease in the PCI and those whose PCI decrease exceeded 50%. Table 3 shows no significant relationship of these parameters (P = .759).
Table 3. RELATIONSHIP OF COMPLETENESS OF CYTOREDUCTION (CC) SCORES AND CHANGE IN PERITONEAL CANCER INDEX (PCI)
Other statistical evaluations, including age, sex, PCI at the first and the second cytoreduction, histopathologic type of the tumor, and positive versus negative lymph nodes, had no significant impact on survival after second-look surgery.
DISCUSSION
Second-look surgery has fallen into disfavor for most malignancies because the therapeutic options available to patients with persistent or progressive disease have been determined to have little or no long-term benefit in terms of survival or quality of life. The results in patients with peritoneal surface spread of appendiceal malignancy suggest that second-look surgery with aggressive cytoreduction plus intraperitoneal chemotherapy may be of benefit. The survival rate at 5 years of 74% obtained with second-look surgery in this group of patients is far superior to that reported in the literature with colon cancer or ovarian cancer. 13–15
There may be some important features of the natural history of appendiceal mucinous tumors with peritoneal dissemination that help explain these favorable results. These malignancies rarely cause treatment failure outside the abdomen or pelvis as a result of metastases. Repeated efforts to eradicate locally persistent disease can be expected to be more successful in the absence of distant metastases.
Secondly, these mucinous tumors, even with grade 3 morphology, tend to have pushing rather than invasive margins. In this situation, the laser mode electrosurgery and intraperitoneal chemotherapy can eradicate microscopic residual disease and secure local control. With persistent disease, however, all of these patients will eventually die of disease. 1,3,4
Thirdly, these minimally invasive malignancies relatively spare small bowel; tumor distributes at dependent anatomic sites and sites of peritoneal fluid resorption. Because oral nutrition is dependent on small bowel function, extensive resection and peritonectomy of other structures can occur with first, second, third, and even fourth reoperation with an acceptable quality of life. Small bowel sparing by mucinous tumor allows successful repeat cytoreduction with preservation of oral nutrition.
Finally, peritoneal surface malignancies are unique in the possibility to treat all tumor with an intraperitoneal route of chemotherapy. The dose intensity of regional chemotherapy uniformly distributed allows eradication of disease rather than a partial response.
It is clear from these data that second-look surgery is of benefit to patients with appendiceal malignancy but that selection factors are important in recommending that patients undergo a second-look procedure. Of 14 clinical features analyzed, 3 suggest an impact on survival and should be considered.
Tumor involvement of the small bowel was extremely important in determining the long-term result with a second-look cytoreduction and perioperative intraperitoneal chemotherapy. If the indication for second-look surgery was intestinal obstruction caused by tumor, the outcome for second-look surgery was guarded (28% 5-year survival). This was significantly different than observed for the other indications for second-look surgery. A large portion of the stomach or colon can be resected with return of nutritional function compatible with an acceptable quality of life. Unfortunately, for small bowel no effective cytoreductive procedures have been developed; aggressive resection is associated with profound nutritional problems. Consequently, preoperative intestinal obstruction, signifying in most patients small bowel invasion by malignancy, was associated with a guarded long-term prognosis despite second-look cytoreduction.
The sites of disease treated at the first cytoreduction must remain free of disease or show minimal progression. The PCI at the second-look procedure must show a decrease of 51% or more compared with the PCI at the first cytoreduction. A durable response to prior therapy suggested a favorable outcome with similar additional treatments.
The completeness of cytoreduction at the time of second-look surgery had a profound effect on outcome. If, on exploration of the abdomen at second-look surgery, it was determined that a complete removal of malignancy was impossible, an aggressive approach to this disease should be abandoned and a palliative intervention pursued. Long-term survival was seen with complete cytoreduction but not with incomplete tumor resection.
A contrast was shown between second-look surgery for peritoneal dissemination of appendiceal malignancy and second-look surgery for colon cancer by Gomez et al. 16 In their data, if the initial cytoreduction was incomplete, subsequent attempts to achieve a complete cytoreduction were not successful. However, in the present analysis of appendiceal malignancy (a more indolent and less aggressive disease), the completeness of the first cytoreduction had little effect on outcome. It was the completeness of cytoreduction at the second-look procedure that determined prognosis in a significant manner.
The change in PCI between the first and the second cytoreduction had a significant impact on prognosis in this report and in a prior report by Berthet et al. 17 They reported that a small increase in the number of anatomic sites involved by sarcoma between a first operation and a definitive cytoreduction was associated with a good prognosis. In 11 patients, they reported an 80% 5-year survival rate. However, if the increase in abdominopelvic regions was four or more, 0 of 32 patients survived 5 years. This was significant (P = .0007). These data from appendiceal malignancy show similar significant differences in the percentage change recorded in the PCI (P = .0001). From a tumor biology perspective, it may be that a decrease in the volume of tumor recorded by comparison of the PCI at the first cytoreduction and second-look surgery indicates one of two situations. If there is little or no disease progression, this indicates that the treatments were effective; alternatively, it may indicate an indolent disease process. If a similar volume of mucinous tumor was recorded at the first cytoreduction and the second-look procedure, this indicates that the treatments were not effective and the tumor has grown back. It is likely that there was an aggressive disease process.
These data seem to confirm the efficacy of a treatment strategy often used in this group of patients who have a low likelihood of developing distant metastatic disease. Frequently, the extent of mucinous tumor was so great at the time of first cytoreduction that complete removal was considered unwise; the magnitude of a surgical procedure resulting in complete tumor resection was judged to carry a prohibitive risk of complications and death. Consequently, an incomplete cytoreduction was performed. However, the peritonectomy procedures that were performed were designed to clear a certain portion of the anatomy completely. The anatomic sites left with gross residual tumor were minimally dissected. If at the second-look procedure the previously peritonectomized regions remained free of disease, then a complete removal of the mucinous tumor was planned. Cytoreductive surgery commensurate with the patient’s physical condition was pursued. This staged approach to a massive cytoreduction to minimize the risk of death and complications seems to be supported by these data.
Footnotes
Correspondence: Paul H. Sugarbaker, MD, FACS, FRCS, The Washington Cancer Institute, 110 Irving St., NW, Washington DC 20010.
E-mail: paul.sugarbaker@medstar.net
Accepted for publication March 2, 2001.
References
- 1.Sugarbaker PH, Ronnett BM, Archer A, et al. Pseudomyxoma peritonei syndrome. Adv Surg 1997; 30: 233–280. [PubMed] [Google Scholar]
- 2.Sugarbaker PH. Observations concerning cancer spread within the peritoneal cavity and concepts supporting an ordered pathophysiology. In: Sugarbaker PH, ed. Peritoneal carcinomatosis: principles of management. Boston: Kluwer; 1996: 79–100. [DOI] [PubMed]
- 3.Gough DB, Donohue JH, Schutt AJ, et al. Pseudomyxoma peritonei: long-term patient survival with an aggressive regional approach. Ann Surg 1994; 219: 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sugarbaker PH. Results of treatment of 385 patients with peritoneal surface spread of appendiceal malignancy. Ann Surg Oncol 1999; 6: 727–731. [DOI] [PubMed] [Google Scholar]
- 5.Sugarbaker PH. Management of peritoneal surface malignancy using intraperitoneal chemotherapy and cytoreductive surgery. A manual for physicians and nurses, 3d ed. Grand Rapids: Ludann Co; 1998.
- 6.Jacquet P, Jelinek JS, Sugarbaker PH. Abdominal computed tomographic scan in the selection of patients with mucinous peritoneal carcinomatosis for cytoreductive surgery. J Am Coll Surg 1995; 181: 530–538. [PubMed] [Google Scholar]
- 7.Archer AG, Sugarbaker PH, Jelinek JS. Radiology of peritoneal carcinomatosis. In: Sugarbaker PH, ed. Peritoneal carcinomatosis: principles of management. Boston: Kluwer; 1996: 289–309.
- 8.Esquivel J, Sugarbaker PH. Elective surgery in recurrent colon cancer with peritoneal seeding: when to and when not to. Cancer Ther 1998; 1: 321–325. [Google Scholar]
- 9.Sugarbaker PH. Peritonectomy procedures. Ann Surg 1995; 221: 29–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sugarbaker PH. Laser-mode electrosurgery. In: Sugarbaker PH, ed. Peritoneal carcinomatosis: principles of management. Boston: Kluwer; 1996: 375–385. [DOI] [PubMed]
- 11.Sugarbaker PH, Chang D, Koslowe P. Peritoneal carcinomatosis from appendiceal cancer: a paradigm for treatment of abdomino-pelvic dissemination of gastrointestinal malignancy. Acta Chir Austriaca 1996; 28: 4–8. [Google Scholar]
- 12.Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. In: Sugarbaker PH, ed. Peritoneal carcinomatosis: principles of management. Boston: Kluwer; 1996: 359–374. [DOI] [PubMed]
- 13.Ronnett BM, Zahn CM, Kurman RJ, et al. Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis: a clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to “pseudomyxoma peritonei.” Am J Surg Pathol 1995; 19: 1390–1408. [DOI] [PubMed] [Google Scholar]
- 14.Cohen AM, Minsky BD, Schilsky RL. Cancer of the colon. In: DeVita VT, Hellman S, Rosenberg SA, eds. Cancer: principles & practice of oncology, 5th ed, vol 1. Philadelphia: Lippincott-Raven; 1997: 1177–1178.
- 15.Hacker NF, Berek JS. Cytoreductive surgery for ovarian cancer. In: Alberts DS, Surwit EA, eds. Ovarian cancer. Boston: Martinus Nijhoff; 1985: 53–67.
- 16.Gomez-Portilla A, Sugarbaker PH, Chang D. Second-look surgery after cytoreductive and intraperitoneal chemotherapy for peritoneal carcinomatosis from colorectal cancer: analysis of prognostic features. World J Surg 1999; 23: 23–29. [DOI] [PubMed] [Google Scholar]
- 17.Berthet B, Sugarbaker TA, Chang D, et al. Quantitative methodologies for selection of patients with recurrent abdominopelvic sarcoma for treatment. Eur J Cancer 1999; 35: 413–419. [DOI] [PubMed] [Google Scholar]