Abstract
Objective
To evaluate the need for a preoperative tumor biopsy of liver lesions suspicious for hepatocellular carcinoma (HCC).
Summary Background Data
With advances in liver imaging, the results of recent studies have suggested a very high accuracy of preoperative evaluation of liver masses suspicious of HCC, making preoperative tumor biopsy unnecessary.
Methods
A retrospective analysis was conducted of all liver resections for HCC at the Toronto General and Mt. Sinai Hospitals, Toronto, between October 1994 and December 1998.
Results
Sixty patients underwent 65 liver resections without a preoperative liver biopsy. The median age was 61 years. Sixty percent of the patients had cirrhosis and 38.5% had noncirrhotic chronic hepatitis. HCC was confirmed histologically in the surgical specimen in 63 of the 65 cases (96.9%). Both patients without HCC had a significant risk factor for HCC (chronic hepatitis C and alcohol in one and chronic hepatitis B and previous resection for HCC in the other). The lesions were 2 cm and 2.7 cm in diameter, and the alpha-fetoprotein level was low (<5 and 22 ng/mL, respectively). In such patients, with tumor 3 cm or smaller and an alpha-fetoprotein level less than 100 ng/mL (10 patients), the false-positive rate for the preoperative diagnosis was 2/10 (20%).
Conclusions
Preoperative diagnosis of HCC was highly accurate in lesions larger than 3 cm. Tumor biopsy is unnecessary in these patients. However, in a subgroup of patients with lesions less than 3 cm, particularly those with alpha-fetoprotein levels less than 100 ng/mL, there is a higher false-positive diagnostic rate, and tumor biopsy should be considered.
Hepatic resection of hepatocellular carcinoma (HCC) is a major operation in high-risk patients (mostly cirrhotic or with chronic hepatitis), with a postoperative death rate of 5% in most recent large series. 1–3 The advances in magnetic resonance imaging and spiral computed tomography (CT) scanning have significantly improved the radiologic diagnostic accuracy of HCC. 4,5 A preoperative liver tumor biopsy has become unnecessary in many cases. Recently, a prospective study from Japan reported a very high accuracy of preoperative evaluation of liver mass without the use of a liver biopsy. 6 Further, the results of four recent reports indicate that core needle biopsy of HCC may carry a 2% to 5% risk of seeding tumor cells along the needle track. 7–10 The hepatobiliary service at the Toronto General and Mount Sinai hospitals has for several years had a policy of not performing biopsy of liver lesions suspicious for HCC before surgery. In this report we evaluate the diagnostic accuracy of this policy.
PATIENTS AND METHODS
We undertook a retrospective analysis of 82 patients who underwent 87 liver resections for HCC in the Toronto General and Mt. Sinai hospitals, Toronto, between October 1994 and December 1998. Data were collected from a prospectively developed database of a weekly multidisciplinary tumor board and a search of hospital medical records (ICD-9 code 155.0, liver neoplasm, primary). Files were reviewed to determine whether a biopsy had been performed before surgery. The histologic and surgical reports were reviewed to confirm HCC. Clinically relevant parameters were also extracted. We limited the study to a single question: whether the preoperative clinical/radiologic diagnosis of the dominant lesion in each patient was correct compared with the pathology report.
Twenty-two patients were excluded. Eighteen patients had a tumor biopsy before surgery. Two patients presented with ruptured HCC and underwent emergency surgery. There was insufficient data for two patients. All the patients who were excluded had HCC in the surgical specimen. Among the 18 patients who were excluded because of a presurgical biopsy, 9 had been referred with a tumor biopsy and 9 had had a biopsy done as part of the diagnostic workup. The reason for biopsy in the latest nine was related to practice variability among investigating physicians.
Only patients with positive test results were included (preoperative clinical/radiologic diagnosis of HCC). Thus, only the positive predictive value and the false-positive rate of the preoperative diagnosis were calculated.
RESULTS
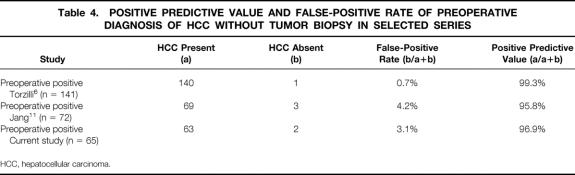
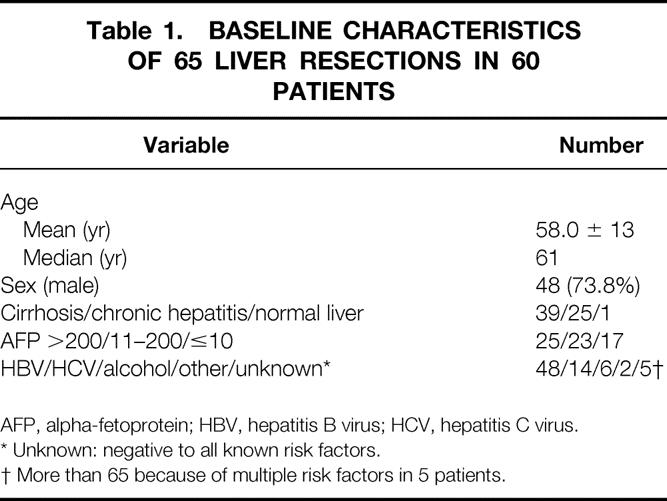
Sixty patients underwent 65 hepatic resections between October 1994 and December 1998 without having a preoperative liver biopsy. Their demographics and baseline characteristics are described in Table 1. Mean age was 58 years. Only 39 of the 65 (60.0%) had cirrhosis, and all but two of the cirrhotic patients were Child-Pugh class A. Twenty-six patients (35%) had alpha-fetoprotein (AFP) levels of more than 200 ng/mL. Five patients had no known risk factor for HCC; one had a presumed colon cancer metastasis but was found to have HCC. Most of the tumors were unifocal (52/65 [80%]), and most were less then 5 cm in diameter (37/65 [56.9%]). In three patients diffuse disease was diagnosed during surgery (Table 2).
Table 1. BASELINE CHARACTERISTICS OF 65 LIVER RESECTIONS IN 60 PATIENTS
AFP, alpha-fetoprotein; HBV, hepatitis B virus; HCV, hepatitis C virus.
* Unknown: negative to all known risk factors.
† More than 65 because of multiple risk factors in 5 patients.
Table 2. TUMOR CHARACTERISTICS IN 65 HEPATIC RESECTIONS OF HCC WITHOUT PREOPERATIVE LIVER BIOPSY
* 3 patients, diffuse disease diagnosed during surgery.
Pathology examination confirmed HCC in 63 resected specimens (96.9%) and was negative for HCC in 2 patients only. Thus, the false-positive rate for the clinical/radiologic evaluation was 2 of 65 (3.1%).
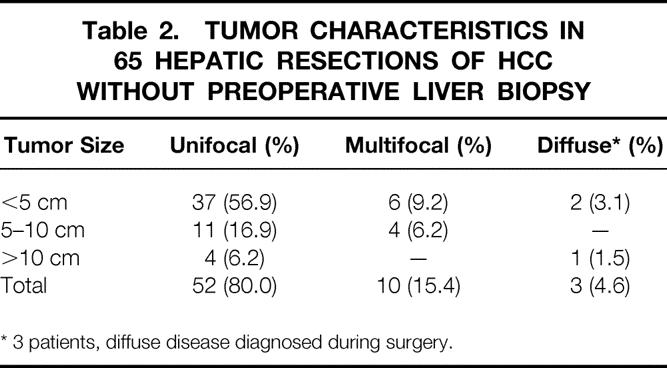
Both patients with false-positive diagnoses had risk factors for HCC. One had a history of chronic hepatitis C and excess alcohol consumption. Ultrasound and triphasic CT scan showed a 2.7-cm enhancing lesion consistent with HCC. The AFP was normal (<5 ng/mL). Intraoperative ultrasound also suggested HCC. The surgical specimen showed a simple hemangioma. The second patient had chronic hepatitis B and had a previous resection for HCC. Two years after the initial resection, a new 2.0-cm arterialized lesion was seen on a triphasic CT scan. The AFP was 22 ng/mL. The lesion was not visible by ultrasound or by Lipiodol angiography. Intraoperative ultrasound showed a plaque area with inhomogeneity but could not identify a mass. The surgical specimen showed only chronic hepatitis with fibrosis and incomplete cirrhosis but no HCC. The two false-positive cases diagnosed in our study were in patients with small lesions (≤3 cm) and low AFP levels (<5 and 22 ng/mL). There were 18 patients with HCC lesions measuring 3 cm or less. The AFP was less than 100 ng/mL in 10 of these patients (Table 3). Thus, in patients with tumor 3 cm or smaller and AFP levels between 0 and 100 ng/mL, the false-positive rate of the preoperative diagnosis was 2 of 10 (20%). Forty-seven patients (72%) had tumors larger than 3 cm, although 26 of them (55.3%) had AFP levels less than 100 ng/mL; all of them were correctly diagnosed.
Table 3. TUMOR SIZE, AFP LEVELS, AND FALSE-POSITIVE CLINICAL DIAGNOSIS OF HCC
AFP, alpha-fetoprotein; FP, false-positive; HCC, hepatocellular carcinoma.
DISCUSSION
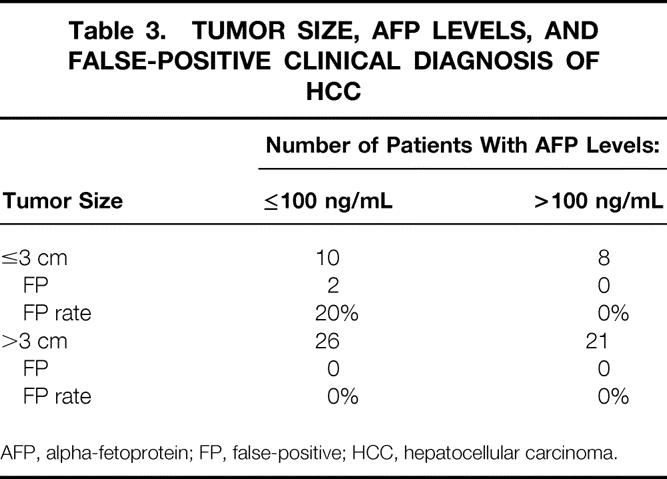
The evaluation of a liver mass has changed since the introduction of magnetic resonance imaging and helical CT, both of which enhance the diagnostic accuracy for these lesions. 4,5 Our study shows that 63 of the 65 preoperative diagnoses of HCC were correct (96.9%), and a preoperative liver biopsy was unnecessary in these cases. Similar clinical/radiologic accuracy of diagnosis of HCC has been described recently in Japan. 6 In that study, a sensitivity of 100% and specificity of 98.9% was achieved. We could not calculate the sensitivity and specificity because we captured only patients with positive test results. However, our study shows that the clinical/radiologic diagnosis had a positive predictive value of 96.9% (63/65) and a false-positive rate of 3.1%. A similar false-positive rate of the radiologic diagnosis before HCC resection (4%) was recently described in a prospective study from Korea. 11 The results of these studies (summarized in Table 4) support a policy of not performing a biopsy before resection of a liver mass suspicious for HCC.
Table 4. POSITIVE PREDICTIVE VALUE AND FALSE-POSITIVE RATE OF PREOPERATIVE DIAGNOSIS OF HCC WITHOUT TUMOR BIOPSY IN SELECTED SERIES
HCC, hepatocellular carcinoma.
These results are not applicable for small tumors (<2–3 cm). The two false-positives diagnosed in our study were in patients with small lesions (2.7 and 2.0 cm) and low AFP levels. There were 10 such patients in the study. Their false-positive diagnosis rate was 2 of 10 (20.0%). The high false-positive rate in small HCCs (<3 cm) is related to the limitation of the radiologic findings in small lesions within a cirrhotic liver. A recent study that examined 32 small (<2 cm) hepatic nodules detected by ultrasound showed that more than half were not HCC, and that current imaging techniques, including CT and magnetic resonance imaging, are insensitive in characterizing these hepatic nodules. 12 Another study of small, well-differentiated HCCs detected by ultrasound and not seen in CT arterial portography indicated once more that in this type of tumor, it is very difficult to differentiate between malignant and benign nodules. 13
In advanced cirrhosis, as has been shown in pretransplant patients, the positive predictive value of the radiologic diagnosis decreases to less than 70%, with a false-positive rate of more than 30%. 14,15 Further, the diagnostic yield of spiral CT was recently examined in 354 pretransplant cirrhotic patients and compared with the pathology reports in the explanted livers. 16 Sixty-one hypervascular lesions were detected in the pretransplant livers. Two thirds of the lesions were regenerative nodules (43/61). The authors concluded, “in small tumors (<3 cm) it was impossible to differentiate between regenerative nodules and HCC using the current spiral CT scanning.”
The false-positive clinical/radiologic diagnosis of HCC in our study was 3.1%. This is equal to or lower than the combined rate of seeding and bleeding from tumor biopsy. Four reports 7–10 have recently shown that core-needle biopsy (18–19 gauge) may carry a 2% to 5% risk of tumor seeding and a 1% risk of bleeding. 7 The high tumor-seeding rate has not been previously observed in large retrospective series of fine-needle biopsies of the liver. 17,18 Fine-needle biopsies that use a 20- to 21-gauge needle may have lower rates of tumor seeding than the 18-gauge core-needle biopsy. It is possible that examination of tumor tissue may in future be useful for histopathology staging or DNA studies of the tumor. If so, the issue of tumor biopsy will have to be reviewed.
In summary, the preoperative clinical/radiologic diagnosis of HCC is highly accurate in lesions larger than 3 cm. Preoperative liver biopsy is not necessary in these patients. However, in small lesions (≤3 cm), particularly in patients with an AFP level less than 100 ng/mL, the false-positive rate was high (20%). In such patients, close observation or a tumor biopsy should be considered before liver resection.
Footnotes
Correspondence: Morris Sherman, MD, Toronto General Hospital EN9-223, 200 Elizabeth St., Toronto, ONT, M5G2C4 Canada.
E-mail: morrissherman@globalserve.net
Accepted for publication January 11, 2001.
References
- 1.Fong Y, Sun RL, Jarnagin W, et al. An analysis of 412 cases of hepatocellular carcinoma at a western center. Ann Surg 1999; 229;6:790–800. [DOI] [PMC free article] [PubMed]
- 2.Foster J, Valdecasas-Garcia JC, Grande L, et al. Hepatocellular carcinoma and Cirrhosis Results of surgical treatment in a European series. Ann Surg 1996; 223: 297–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philosophe B, Greig P, Hemming A, et al. Surgical management of hepatocellular carcinoma: resection or transplantation? J Gastrointest Surg 1997; 2: 21–27. [DOI] [PubMed] [Google Scholar]
- 4.Van Leeuwen MS, Noordzi J, Feldberg MAN, et al. Focal liver lesions: Characterization with triphasic CT. Radiology 1996; 160: 625–629. [DOI] [PubMed] [Google Scholar]
- 5.Nino-Murcia M, Olcott EW, Brooke JR, et al. Focal liver lesions: pattern-based classification scheme for enhancement at arterial phase CT. Radiology 2000; 215: 746–751. [DOI] [PubMed] [Google Scholar]
- 6.Torzilli G, Minagawa M, Takayama T, et al. Accurate preoperative evaluation of liver mass lesions without fine needle biopsy. Hepatology 1999; 30: 889–893. [DOI] [PubMed] [Google Scholar]
- 7.Huang GT, Sheu CJ, Yang PM. Ultrasound-guided cutting biopsy for the diagnosis of hepatocellular carcinoma: study based on 420 patients. J Hepatol 1996; 25: 334–348. [DOI] [PubMed] [Google Scholar]
- 8.Chapoutot C, Perney P, Faber D, et al. Essaimages tumorax sur letrajet de ponctions echo-guided de carcinomes hepatocellulaires. Etude de 150 malades. Gastroenterol Clin Biol 1999; 23: 552–556. [PubMed] [Google Scholar]
- 9.Takamori R, Wong LL, Dang C, Wong L. Needle tract implantation of hepatocellular carcinoma: is needle biopsy of the liver always necessary? Liver Transplant 2000; 6: 62–72. [DOI] [PubMed] [Google Scholar]
- 10.Kim SH, Lim HK, Lee WJ, et al. Needle-tract implantation in hepatocellular carcinoma: frequency and CT findings after biopsy with a 19.5-gauge automated biopsy gun. Abdomen Imaging 2000; 25: 246–250. [DOI] [PubMed] [Google Scholar]
- 11.Jang HJ, Lim JH, Lee SJ, et al. Hepatocellular carcinoma: are combined CT during arterial portography and CT hepatic arteriography in addition to triple-phase helical CT all necessary for preoperative evaluation? Radiology 2000; 215: 373–380. [DOI] [PubMed] [Google Scholar]
- 12.Kanematsu M, Hoshi H, Yamada T. Small hepatic nodules in cirrhosis: ultrasonographic, CT, and MR imaging finding. Abdom Imaging 1999; 24;1:47–55. [DOI] [PubMed]
- 13.Tanaka Y, Sasati Y, Katayama K, et al. Probability of hepatocellular carcinoma of small hepatocellular nodules undetectable by computed tomography during arterial portography. Hepatology 2000; 31: 890–898. [DOI] [PubMed] [Google Scholar]
- 14.Chalasani N, Horlander JC, Said A, et al. Screening for hepatocellular carcinoma in patients with advanced cirrhosis. Am J Gastroenterol 1999; 94; 2988–2993. [DOI] [PubMed] [Google Scholar]
- 15.Gambarin-Gelwan M, Wolf DC, Shapiro R, et al. Sensitivity of commonly available screening tests in detecting hepatocellular carcinoma in cirrhotic patients undergoing liver transplantation. Am J Gastroenterol 2000; 96: 1535–1538. [DOI] [PubMed] [Google Scholar]
- 16.Freenly PC, Kaakaji K, Grossholz ME, et al. The significance of hypervascular hepatic nodules detected during four-phase helical CT in patients with cirrhosis: correlation of CT and explanted liver pathology. Radiology 1999; 213: 335. [Google Scholar]
- 17.Buscarini L, Fornini F, Bolondi L, et al. Ultrasound-guided fine-needle biopsy of focal liver lesions: techniques, diagnostic accuracy and complications. A retrospective study on 2091 biopsies. J Hepatol 1990; 11: 344–348. [DOI] [PubMed] [Google Scholar]
- 18.Smith EH. Complication of percutaneous abdominal fine-needle biopsy. Radiology 1991; 17: 253–258. [DOI] [PubMed] [Google Scholar]