Abstract
Objective
To evaluate the safety of a policy of selective nonoperative management (SNOM) in patients with abdominal gunshot wounds.
Summary Background Data
Selective nonoperative management is practiced extensively in stab wounds and blunt abdominal trauma, but routine laparotomy is still the standard of care in abdominal gunshot wounds.
Methods
The authors reviewed the medical records of 1,856 patients with abdominal gunshot wounds (1,405 anterior, 451 posterior) admitted during an 8-year period in a busy academic level 1 trauma center and managed by SNOM. According to this policy, patients who did not have peritonitis, were hemodynamically stable, and had a reliable clinical examination were observed.
Results
Initially, 792 (42%) patients (34% of patients with anterior and 68% with posterior abdominal gunshot wounds) were selected for nonoperative management. During observation 80 (4%) patients developed symptoms and required a delayed laparotomy, which revealed organ injuries requiring repair in 57. Five (0.3%) patients suffered complications potentially related to the delay in laparotomy, which were managed successfully. Seven hundred twelve (38%) patients were successfully managed without an operation. The rate of unnecessary laparotomy was 14% among operated patients (or 9% among all patients). If patients were managed by routine laparotomy, the unnecessary laparotomy rate would have been 47% (39% for anterior and 74% for posterior abdominal gunshot wounds). Compared with patients with unnecessary laparotomy, patients managed without surgery had significantly shorter hospital stays and lower hospital charges. By maintaining a policy of SNOM instead of routine laparotomy, a total of 3,560 hospital days and $9,555,752 in hospital charges were saved over the period of the study.
Conclusion
Selective nonoperative management is a safe method for managing patients with abdominal gunshot wounds in a level 1 trauma center with an in-house trauma team. It reduces significantly the rate of unnecessary laparotomy and hospital charges.
During the past two decades selective nonoperative management (SNOM) has been used with increasing frequency for abdominal trauma. Many injuries previously managed exclusively by surgery are now being observed closely in the absence of peritonitis or hemodynamic instability. SNOM is considered the standard of care for blunt injuries and stab wounds and has decreased the rate of unnecessary laparotomy, shortened the length of hospital stay, and produced significant cost savings. 1,2 However, abdominal gunshot wounds have been excluded from this advancement. Identically to the way abdominal blunt injuries and stabbings were managed 20 years ago, abdominal gunshot wounds are still managed by routine laparotomy in most trauma centers around the world. 3,4 The reasons cited for this are three: first, the incidence of significant intraabdominal injuries after abdominal gunshot wounds is more than 90%; second, an unnecessary laparotomy is a harmless procedure; and third, clinical examination is unreliable.
The high-volume level 1 trauma center at the Los Angeles County and University of Southern California Medical Center admits many patients with abdominal gunshot wounds every year. Because we believe that all three of the above arguments in favor of routine laparotomy are invalid, we manage our patients by SNOM. 5,6 In this study, we describe our experience with abdominal gunshot wounds during the past 8 years with the intent of offering a convincing argument about the advantages of SNOM over routine laparotomy. Our hypothesis is that SNOM is safe and cost-effective, prevents unnecessary negative laparotomies, and decreases the hospital length of stay and therefore should become the standard of care for the management of abdominal gunshot wounds.
METHODS
All patients who were admitted at our trauma center with an anterior or posterior abdominal gunshot wound between January 1993 and December 2000 were included and had their medical records reviewed. Anterior abdominal gunshot wounds were defined as gunshot wounds confined between the two midaxillary lines laterally, a line connecting the two nipples superiorly and a line over the pubic symphysis inferiorly. Posterior abdominal gunshot wounds were defined as gunshot wounds confined between the two midaxillary lines laterally, a line connecting the tips of the scapulae superiorly and a line over the gluteal folds inferiorly. In the presence of anterior and posterior gunshot wound sites, the patients were classified as having an anterior gunshot wound. Patients of all ages were included. Patients with obviously superficial gunshot wounds (i.e., an entry next to an exit site) were excluded. Patients who had an emergency room thoracotomy and died shortly after admission were reported but excluded from the statistical analysis. A laparotomy was defined as therapeutic when intraabdominal injuries requiring repair were found. A laparotomy was defined as unnecessary when no intraabdominal injuries were found or the injuries found did not require intervention (e.g., a small nonbleeding liver laceration or a nonexpanding retroperitoneal hematoma located away from major structures). A delayed laparotomy (i.e., a laparotomy on a patient initially selected for observation) indicated failure of SNOM. Failure was caused by the appearance of new abdominal tenderness, progression of mild around-the-wound tenderness to deeper and more generalized abdominal pain, and an unexplained drop in the hematocrit or blood pressure. Increases in the white blood cell count and temperature were also considered in the context of the general clinical picture.
Our trauma center is run by seven dedicated trauma surgeons who provide in-house around-the-clock coverage, participate in all operations and major resuscitations, and supervise the care of all patients from admission to discharge. Patients with abdominal gunshot wounds are managed by the trauma team, including surgical and emergency room residents, nurses, and ancillary personnel under the direction of the on-call attending trauma surgeon. Our policy of SNOM indicates that all patients with abdominal gunshot wounds are managed based on individual signs and symptoms and no evaluable patient is taken to the operating room for laparotomy based on the mere presence of a gunshot wound. Clinical examination is the primary tool to select patients; those who are hemodynamically unstable or have diffuse abdominal tenderness are taken emergently for surgery. Also, patients with unreliable clinical examination because of associated head injury, spinal cord injury, or severe intoxication, or because they need to be sedated or intubated, are explored. All other patients are managed by observation and, if needed, further radiographic evaluation. Patients selected for nonoperative management are admitted in a highly monitored observation area for at least 12 to 24 hours before being sent to a floor bed or discharged. In this area, clinical examinations are performed frequently, preferably by the same resident. Attending surgeons are actively involved in the care delivered to patients selected for observation.
Additional radiographic tests are ordered on an individual basis. The most commonly ordered test is an abdominal computed tomography (CT) scan. Although ordered sporadically in the early phase of the study, it has become our routine practice after 1998 for all patients selected for nonoperative management. The intent is to define the bullet trajectory and its proximity to important structures. The results of the abdominal CT serve to add information to the findings of the clinical examination. Although CT is not the principal determinant of the need for surgery, it increases or lowers the threshold for it.
Data were collected from the medical records and the trauma registry, which is maintained by seven dedicated trauma nurses, and included patient demographics, physiologic condition on arrival, severity of injury (Injury Severity Score [ISS]), laparotomy findings, procedures done, complication and death rates, and length of hospital stay. Particular attention was paid to patients who were initially managed without surgery and subsequently taken to the operating room. We compared patients who were taken emergently for laparotomy with patients managed without surgery. We also compared patients who were managed without surgery with success against those who failed to respond to nonoperative management. Finally, we compared the patients who failed to respond to nonoperative management and had a positive laparotomy with those who failed to respond to nonoperative management but had an unnecessary laparotomy. Hospital stay and charges were calculated only among survivors. Comparisons were made by the chi-square and Fisher exact tests for categorical variables and t test for continuous variables. Continuous variables were dichotomized across clinically significant cutoff points: age was dichotomized to older or younger than 55 years, systolic blood pressure to more or less than 100 mm Hg, heart rate to more or less than 100 beats per minute, and ISS to more or less than 16. All the variables that achieved P < .2 were subsequently entered into stepwise logistic regression to identify independent risk factors for failure of nonoperative management. If such risk factors were identified, we could avoid selecting such patients for nonoperative management. A second stepwise logistic regression aimed at identifying independent predictors of a negative laparotomy among patients who failed to respond to nonoperative management. If such predictors were identified, we could avoid a laparotomy in selected patients who show signs of failing nonoperative management. A level of significance at P < .05 was maintained for all comparisons.
RESULTS
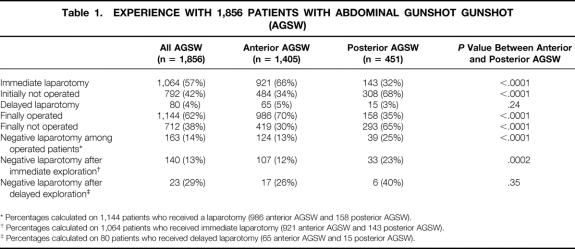
Of 1,975 patients initially included in this trial, 119 who underwent an emergency room thoracotomy and died shortly after admission were excluded from further analysis. Our sample size consisted of 1,856 patients, 1,405 (76%) with anterior abdominal gunshot wounds and 451 (24%) with posterior abdominal gunshot wounds. Seven hundred ninety-two patients (42%) were initially managed without surgery, but 80 (4%) were eventually taken to the operating room. Finally, 712 (38%) patients were discharged from the hospital without surgery. Patients with posterior abdominal gunshot wounds had a higher rate of nonoperative management but a similar rate of delayed laparotomy due to failure of nonoperative management compared with patients with anterior abdominal gunshot wounds (Table 1). The rate of unnecessary laparotomy among the 1,144 operated patients was 14% (or 8% among all patients). During the 8 years of the study, the percentage of patients selected for nonoperative management remained steady: 202 of 459 (44%) in 1993, 145 of 335 (43%) in 1994, 128 of 326 (39%) in 1995, 102 of 218 (47%) in 1996, 65 of 162 (40%) in 1997, 51 of 132 (38%) in 1998, 60 of 121 (50%) in 1999, and 39 of 103 in (38%) in 2000 (P = .32). One hundred eighty-four patients (10%) died, but only 27 deaths occurred after 48 hours of admission. There was one patient in the group managed without surgery who died of reasons unrelated to SNOM (severely cirrhotic patient with additional injuries to the lung who died of pneumonia and liver failure). The patients who were managed without surgery stayed in the hospital for a median of 3 days (4 days in the presence of extraabdominal injuries and 2 days in the absence of extraabdominal injuries).
Table 1. EXPERIENCE WITH 1,856 PATIENTS WITH ABDOMINAL GUNSHOT GUNSHOT (AGSW)
* Percentages calculated on 1,144 patients who received a laparotomy (986 anterior AGSW and 158 posterior AGSW).
† Percentages calculated on 1,064 patients who received immediate laparotomy (921 anterior AGSW and 143 posterior AGSW).
‡ Percentages calculated on 80 patients who received delayed laparotomy (65 anterior AGSW and 15 posterior AGSW).
Immediate Laparotomies
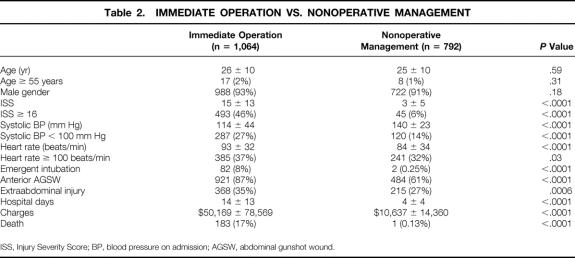
When compared with patients initially selected for nonoperative management, patients immediately taken to the operating room were more severely injured, had a lower systolic blood pressure and a higher heart rate, required more frequently emergent intubation, and were more likely to have extraabdominal injuries and an anterior abdominal gunshot wound (Table 2). They also had longer hospital stays, higher hospital charges, and a higher death rate.
Table 2. IMMEDIATE OPERATION VS. NONOPERATIVE MANAGEMENT
ISS, Injury Severity Score; BP, blood pressure on admission; AGSW, abdominal gunshot wound.
Delayed Laparotomies
Of the 792 patients initially selected for nonoperative management, 80 (10%) progressed to develop signs or symptoms prompting a laparotomy. In 23 of these 80 patients (29%), the delayed laparotomy was unnecessary. Therefore, only 57 patients (0.3% of the entire population) initially managed without surgery eventually had injuries requiring operative repair. The injured organs included the retroperitoneal colon or rectum in 23 patients, small bowel in 15, liver in 10, spleen in 9, kidney in 9, posterior stomach in 7, bladder in 5, ureter in 3, gallbladder in 1, and duodenum in 1. The annual rates of delayed laparotomy were not different during the study period. There was a higher likelihood of failure of nonoperative management among patients with anterior abdominal gunshot wounds (13%) versus patients with posterior abdominal gunshot wounds (5%, P < .0001). No significant differences in gender (91% vs. 95% male, P = .24), admission systolic blood pressure (140 ± 22 vs. 137 ± 24 mm Hg, P = .19), heart rate (94 ± 19 vs. 89 ± 20 beats per minute, P = .07), age (25 ± 10 vs. 27 ± 9 years, P = .07), and the incidence of extraabdominal injuries (26% vs. 34%, P = .16) were found between patients who had successful or failed nonoperative management. Patients with failed nonoperative management had a higher ISS (9 ± 9 vs. 3 ± 5, P < .0001), longer hospital stays (10 ± 6 vs. 4 ± 3 days, P < .0001) and higher charges ($27,461 ± 29,043 vs. $8,731 ± 9,966, P < .0001) compared with patients with successful nonoperative management, but shorter hospital stays (P < .0001) and lower charges (P < .0001) than patients who were operated on immediately.
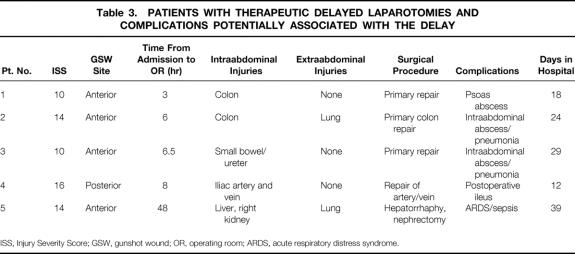
No patient with a delayed laparotomy died, but 5 of these 80 patients (6%) developed complications potentially caused by the delay (Table 3). Four of them had abdominal abscesses, which were managed by CT-guided drainage with success. The last patient had a right upper quadrant gunshot wound and had a CT scan on admission that revealed a significant injury to the right lobe of the liver and upper pole of the right kidney. Although he manifested persistent tachycardia and a dropping hematocrit and required multiple blood transfusions, he was observed for 48 hours in violation of our protocol. At operation he underwent a right nephrectomy and hepatorrhaphy. After surgery, he developed sepsis and the acute respiratory distress syndrome and required a prolonged hospital stay. Excluding this patient, the longest interval between admission and a therapeutic delayed laparotomy was 23 hours on an 18-year-old male patient who was found to have a retroperitoneal colon injury and recovered uneventfully after repair. The average interval for all 80 patients with delayed laparotomies was 6 ± 4 hours from admission. The multivariate analysis failed to identify any independent risk factors for the failure of nonoperative management.
Table 3. PATIENTS WITH THERAPEUTIC DELAYED LAPAROTOMIES AND COMPLICATIONS POTENTIALLY ASSOCIATED WITH THE DELAY
ISS, Injury Severity Score; GSW, gunshot wound; OR, operating room; ARDS, acute respiratory distress syndrome.
Unnecessary Laparotomies
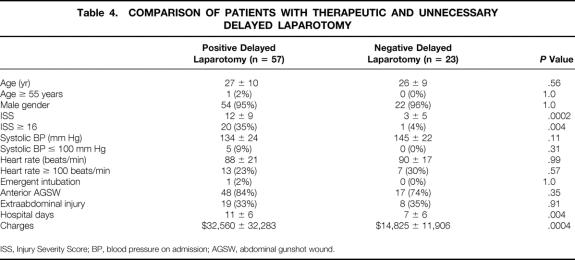
There were 163 unnecessary laparotomies among 1,144 operated patients (14%). The incidence of unnecessary laparotomy in the entire population was 9%; it was higher among patients who were operated on immediately than among patients who underwent a delayed laparotomy (13% [140/1,064] vs. 29% [23/80], P = .007). The annual rates of unnecessary laparotomy were not different during the study period. When we compared the patients who had a therapeutic delayed laparotomy with the patients who had an unnecessary delayed laparotomy, no differences were found in gender, ISS, or physiologic condition on arrival (Table 4). Delayed laparotomy was unnecessary in 6 of 15 (40%) patients with posterior abdominal gunshot wounds and 17 of 65 (26%) patients with anterior abdominal gunshot wounds, but this difference did not achieve statistical significance (P = .35). Patients with therapeutic delayed operations had longer hospital stays and higher charges than patients with unnecessary delayed operations. The multivariate analysis failed to identify any independent risk factor for unnecessary laparotomy among patients with delayed laparotomies. Patients with unnecessary laparotomy stayed in the hospital for a median of 7 days (9 days in the presence and 6 days in the absence of extraabdominal injuries).
Table 4. COMPARISON OF PATIENTS WITH THERAPEUTIC AND UNNECESSARY DELAYED LAPAROTOMY
ISS, Injury Severity Score; BP, blood pressure on admission; AGSW, abdominal gunshot wound.
Cost-Effectiveness
The difference in hospital days and charges was estimated between our current policy of SNOM and a hypothetical policy of routine laparotomy. If we had managed our patients by routine laparotomy, we would have operated on the 712 patients who were eventually discharged without an abdominal exploration. These patients would have had an unnecessary laparotomy. The hypothetical rate of unnecessary laparotomy would be 38%. By our current policy of SNOM, these 712 patients remained on average 4 ± 4 days in the hospital and were charged $8,792 ± 10,091, for a total of 2,848 hospital days and $6,259,904 in hospital charges. If they were managed by routine laparotomy, they would have stayed in the hospital the same number of days that the patients with an unnecessary laparotomy did (9 ± 7 days) and would have been charged similarly ($22,213 ± 24,780), for a total of 6,408 hospital days and $15,815,656 in hospital charges. Therefore, SNOM resulted in 3,560 fewer hospital days and $9,555,752 less in hospital charges compared with routine laparotomy. In 80 patients with delayed operations, the delay in operation did not increase the hospital stay or charges when compared with patients who underwent an immediate laparotomy. Therefore, their management by routine laparotomy would have not resulted in differences in hospital days and charges compared with their current management by SNOM.
DISCUSSION
The management of blunt and penetrating abdominal trauma has evolved dramatically during the past 20 years. In the midst of major changes related to improvements in resuscitation and surgical techniques, antibiotic management, and monitoring equipment, SNOM emerges probably as the single most significant advancement. The ability to manage patients safely and reliably without operating on them when an operation is not needed seems not only scientifically correct but also ethically justified. However, the management of abdominal gunshot wounds has been glaringly excluded from the evolution of SNOM.
The advocates of maintaining routine laparotomy as the standard of care for most abdominal gunshot wounds claim that abdominal gunshot wounds are very likely to cause intraabdominal organ injuries, 3,7 unnecessary laparotomies are not likely to cause significant complications, 8,9 and clinical examination is unreliable to select patients for operation or nonoperative management. 3,7,10 The first argument is based on an alleged incidence of intraabdominal organ injury, after an abdominal gunshot wound, of 90% or greater. Although this may be true for military missiles, abdominal gunshot wounds from civilian violence are associated with a lower incidence of clinically significant intraabdominal organ injuries, ranging in many studies from 30% to 74%. 5,6,11–15 The second argument is similarly flawed. Unnecessary laparotomies for trauma are associated with a significant complication rate, ranging from 22% to 41%, 15–17 and a significantly prolonged hospital stay. 18 It is difficult to imagine that emergent surgery in the middle of the night by tired and usually junior surgeons and anesthesiologists on unprepared patients with full stomachs will not be associated with a significant complication rate, even in the absence of intraabdominal organ injuries. Finally, the third argument about the unreliability of physical examination has been already proven wrong in other types of trauma, such as stab wounds and blunt trauma. 1,2 There is little ground to support that clinical examination is reliable for stabbings but unreliable for abdominal gunshot wounds. In addition, the continuous improvement of imaging techniques increasingly allows their use in the diagnosis of intraabdominal organ injuries as valuable adjuncts to clinical examination. Helical CT, traditionally thought to have limited usefulness in penetrating trauma, is now shown to determine with reasonable accuracy bullet trajectories and their proximity to vital structures. 19
The concept of SNOM in abdominal gunshot wounds is not new in the United States. For more than 20 years, studies have shown that managing abdominal gunshot wounds selectively is safe. The idea of “selective conservatism,” introduced by Shaftan 20 in the 1960s, was validated in larger samples of patients by the same group 21 and by Nance et al 22 in later studies. Around the same time, reports from the high-volume trauma center of the Baragwanath Hospital in South Africa by Demetriades et al 13,23 were showing convincingly that selected patients with abdominal gunshot wounds can be managed safely without surgery. A series of prospective studies from our group at the Los Angeles County and University of Southern California Medical Center confirmed that SNOM could be practiced with minimal complications and a low rate of unnecessary laparotomy in patients with gunshot injuries to the abdomen, 5 back, 6 buttocks, 24 or pelvis. 25 We also reported on successful nonoperative management of gunshot wounds of specific organs, such as the liver 26 and kidney. 27 Other investigators around the country reported favorably on SNOM. 28,29
Despite such evidence, routine laparotomy is still considered the standard of care in most trauma centers. A 1996 editorial by Nance and Nance 30 prompted surgeons to reconsider the financial and societal burden created by a policy of performing unnecessary laparotomies in patients with abdominal gunshot wounds.
The current study describes our experience with a long-standing policy of SNOM for abdominal gunshot wounds. In contrast to our previous prospective studies, this study offers a more realistic view of the SNOM policy in a large sample of patients who were not managed under the strict protocol of a prospective study. Therefore, we believe that these results reflect more accurately the outcomes that can be expected if such a policy were to be applied in other centers. It is remarkable that 38% of patients were eventually discharged without an abdominal exploration. Against the existing dogma, we showed that approximately one third of patients with anterior abdominal gunshot wounds and two thirds of patients with posterior abdominal gunshot wounds do not have significant intraabdominal injuries. The incidence of unnecessary laparotomy was 14% (or 9% if the rate is calculated over the entire study population), significantly lower than the rates reported in the literature. 12,16,31 Although this rate is higher than the 10% and 4% unnecessary laparotomy rates we found during our previous prospective studies on anterior 5 and posterior 6 abdominal gunshot wounds, respectively, we believe that 14% is a more realistic goal to achieve in most trauma centers at this point. When surgeons believe that they do not violate the standard of care by observing patients with abdominal gunshot wounds, it is likely that operations for equivocal symptoms will be done less liberally and the rate of unnecessary laparotomy will decrease. The surgeon’s anxiety about managing an abdominal gunshot wound without surgery under the current medicolegal implications of SNOM for abdominal gunshot wounds was evident even in our series. There was a significantly higher unnecessary laparotomy rate among patients who were explored initially versus those who were initially observed and explored later (13% vs. 29%). This indicates that even the members of a trauma team with extensive experience in SNOM kept a low threshold for operating on patients who were initially managed without surgery but later developed suspicious symptoms.
In trying to reduce the rate of unnecessary laparotomies, we tried to identify differences in characteristics between patients with therapeutic and unnecessary laparotomy, which might help avoid negative abdominal explorations in the future. However, there were no such differences in terms of gender, extraabdominal injuries, location of gunshot wound site, or physiologic presentation on admission. These results confirm that the best method to decide who needs or does not need an operation is to rely on the information provided by hemodynamic monitoring and careful physical examination.
Obviously, the greatest concern related to a policy of SNOM is the complications produced by delays in operating on patients who, despite the absence of signs and symptoms, have an intraabdominal injury requiring repair. Again, in contrast to the standard dogma, this occurs infrequently: according to our results, in 0.6% of patients initially selected for nonoperative management (5/792) or 0.3% of the entire series (5/1,856). More importantly, these patients can be safely managed by undergoing the operation at the time symptoms appear. Among 80 patients with delayed laparotomy, 5 developed complications potentially related to the delay in operation. In four of them an abscess, which was formed by the area of primary repair of a colonic injury, was drained under CT guidance successfully. The one patient who suffered significant complications and had a prolonged hospital stay due to a 48-hour delay in operating on a bleeding gunshot injury to the liver and right kidney was not really a failure of our nonoperative policy but rather a failure of the treating physician to follow the guidelines of this policy (i.e., operate on a patient with a decreasing hematocrit instead of transfusing him). This patient aside, we believe that there is no significant risk in delaying an operation until relevant symptoms declare the need for it. We did no colostomies for colon injuries, nor did we leave any abdomen open due to the delay. These injuries should not be referred as “missed,” because they have little relevance to injuries that were not treated despite the presence of symptoms as a result of a frivolous physical examination or inadequate clinical follow-up. The average delay to operation for patients initially managed without surgery was 6 hours. Except for the patient mentioned above, no patient had a therapeutic delayed operation later than 24 hours from admission. For this reason, we believe that for the vast majority of patients, 24 hours of observation is adequate.
Patients who were managed without surgery were naturally less injured and more stable than patients taken to operation. These patients spent less than one third of the time in the hospital and were charged less than one fifth of the charges of operated patients. From a financial standpoint the most important comparison was between the patients who were managed without surgery and a hypothetical population consisting of the same patients, if they had been managed by routine laparotomy. These patients would have had an unnecessary exploration and then would have stayed in the hospital as long as our patients with unnecessary laparotomy did. According to these calculations, SNOM decreased the hospital stay by a total of 3,560 days and the hospital charges by $9,555,752 during a period of 8 years. This translates in $1,194,469 less in hospital charges per year.
The method of SNOM may not be applicable to all medical centers. The encouraging results reported here are produced in a high-volume academic urban level 1 trauma center with 24-hour in-house coverage by trauma surgeons experienced with SNOM. Careful observation and close monitoring are integral parts of SNOM in abdominal gunshot wound patients. In the absence of experience with this technique or the lack of qualified physicians to monitor patients selected for nonoperative management closely, abdominal exploration might be a safer alternative. However, with increasing experience, SNOM may be adopted progressively by more surgeons, as has occurred with stab wounds.
This study is retrospective. Most of the patients included were not managed under the stringent protocol of a prospective study. Although the retrospective design has all the known limitations, it serves to offer a realistic impression of the results that should be anticipated by different centers that may follow a policy of SNOM. Although the study covers a long period, the core group of surgeons managing these patients remained the same and the policy remained unchanged. Therefore, the care provided remained consistent throughout these 8 years.
An additional point to argue about this study relates to the incidence of superficial abdominal gunshot wounds. Although we tried to exclude patients with obviously superficial abdominal gunshot wounds during our review of the trauma registry and medical records, it is possible that a few such patients were still included as a result of the retrospective nature of the study and the lack of precise description of bullet trajectories. Patients with superficial abdominal gunshot wounds are likely to be managed without surgery even in centers that practice routine laparotomy. The inclusion of such patients may have artificially increased the percentage of patients reported as eligible for nonoperative management after nonsuperficial abdominal gunshot wounds. However, if this occurred, the increase is expected to be very small. It is also more significant to report that SNOM is an overall safe policy than argue about the exact percentage of patients who can be managed without surgery.
Our study shows that in a large sample of patients with abdominal gunshot wounds, a policy of SNOM produces excellent results and significantly reduces hospital stay and charges. Approximately one third of patients with anterior abdominal gunshot wounds and two thirds with posterior abdominal gunshot wounds can be safely managed without surgery. Under this policy, the expected rate of unnecessary laparotomy is 14% and the incidence of patients who will need a delayed laparotomy because of development of suspicious symptoms is 4%. Academic trauma centers with adequate coverage should use these data to consider a change in the current standard of care for patients with abdominal gunshot wounds and terminate the dichotomy of using SNOM for stab wounds and blunt trauma but not gunshot wounds. “It is time we told the emperor about his clothes.”30
DISCUSSION
Dr. David B. Hoyt (San Diego, California): I would like to congratulate Dr. Velmahos on his excellent presentation and another fine study from UC.
In 1510, Ambrose Pare’ published arguably the first example of nonoperative management. Nonoperative management of gunshot wounds is in fact not new. However, it has not been widely adapted. The reasons for this are not really clear.
I think this study demonstrates that with appropriate selection, careful observation, and in experienced hands, about one-third will avoid operation. The authors are really saying wait till you have peritonitis or hypertension, and that this is safe practice. This really is the question. Is this safe practice? Dr. Velmahos, I have several questions for you.
What is your exact protocol? Are patients in a specific unit? Who watches them? And what are the responsibilities of that individual during the time that they are making this decision? What are your failure criteria? Are there specific criteria or just physician judgment? What select x-rays do you use and who gets what, when?
The average time to operation in this series was six hours. But when do the patients actually evident their failure? Aren’t you really just operating at a slightly delayed time frame following admission in many of these patients?
Have you changed the operative care as a result of delay? In other words, done a colostomy instead of primary repair? Or have you done more frequent open abdomens as a result of this? Finally, should centers with infrequent gunshot wound experience follow selective nonoperative management?
I enjoyed your paper. This will undoubtedly evolve us toward selective nonoperative management as introduced by Dr. Shaftan and Dr. Nance over 30 years ago in this country.
Presenter Dr. George C. Velmahos (Los Angeles, California): Thank you, Dr. Hoyt. Responding to your first question, we are keeping patients who are selected for non-operative management in a closely monitored area where staff is available on a 24-hourly basis. We do not send these patients in different wards scattered across the hospital. The patients are examined continuously by the in-house trauma team, including an attending. We insist on having the same person examining the patients in order to understand changes in clinical findings. Usually, our senior residents are pretty good with it.
The most important element of the decision to take a patient, initially selected for non-operative management, to the operating room is increasing abdominal tenderness. The selected patients are invariably hemodynamically stable, so we rarely had hypotension as a reason to operate on one of these patients.
With regard to additional diagnostic tests, it is the abdominal CT that we increasingly use these days. It helps us define the bullet trajectory and confirm the absence of significant organ injury.
When do these patients fail? They usually fail within the first few hours. If there is an intra-abdominal injury, it manifests in most instances within 4-8 hours after admission. This is why we believe that in the absence of any symptoms, in-house follow-up of more than 24 hours is unnecessary.
Did we change our surgical management for any of the patients who received a delayed operation? The answer is clearly no. In this group, there was no patient with colon injury who received a colostomy. They all had primary colon repair.
Finally, the very important question as to whether small centers with less experience in this type of injuries should adopt selective non-operative management. I think that at this point, the answer is probably negative. Experience and 24-hour commitment by in-house staff are the right ingredients of success. However, I predict that as the policy spreads, more and more surgeons will become more comfortable with this method, exactly as it happened with abdominal stab wounds. So, hopefully in the future, even smaller centers will build the necessary experience and resources to avoid unnecessary operations.
Dr. Francis C. Nance (Short Hills, New Jersey): Dr. Velmahos and his colleagues have exposed the myths about abdominal gunshot wounds that have been around since the 19th century — maybe because we have seen too many John Wayne movies.
Of those, I have always felt that the myth that the clinical examination of the patient was unreliable was hardest to understand, and I have said previously. Thirty years ago, following Jerry Shaftan’s pioneering insight, I said that to this Association, to the considerable disapprobation of many of the members of this organization.
Since then, selective management of stab wounds has achieved general but not universal acceptance. It seems to me that the time has come for those surgeons who continue to advocate routine or mandatory laparotomy for gunshot wounds be asked to provide hard data to support their conclusions.
This outstanding paper is only one of many recent papers that are providing clinical evidence that utilization of a surgeon’s mind and his diagnostic skills is superior to a rote protocol-driven approach to abdominal gunshot wounds.
I do have one question. You still have a significant incidence of non-therapeutic laparotomies. Have you identified any specific clinical findings which if understood and heeded might further reduce the incidence of unnecessary operations?
Dr. George C. Velmahos: Thank you, Dr. Nance. I would like to recognize your lead in advancing this idea. With regard to your question about the 9% negative laparotomies, I would consider this as an almost irreducible percentage at this point. We looked at multiple variables in patients with therapeutic and patients with unnecessary laparotomy. None of these variables was statistically or even clinically different between the two groups. So, there was nothing that could help us select out the patients likely to have an unnecessary laparotomy. Taking into account the learning curve that needs to be built and the involvement of residents in a teaching program, we believe that a 9-10% unnecessary laparotomy rate is a reasonable target to aim for.
Dr. Gerald W. Shaftan (East Meadow, New York): The fifth meeting of The American Surgical Association was held in Washington on April 24-28, 1885, 116 years ago. Thirty-five members were signed in attendance and there was spirited discussion of this same topic. This is the first paper of a panel on the subject from the Proceedings of that meeting; the other papers were by William W. Keen also from Philadelphia and Robert A. Kinloch of Charleston. The discussion of the three papers was opened with the statement that “The subject is one of great interest, probably the most interesting surgical subject that could be brought before us at the present time.” One third of the members at the meeting — I hope it won’t be true today — participated in the discussion; Tobias G. Richardson of Charity in New Orleans noted that out of 33 cases of gunshot wounds of the abdomen, 13 recovered without operation. The single laparotomy was among the 20 deaths.
Dr. Velmahos and his colleagues from L. A. County have provided with us indisputable proof that well trained and diligent Surgeons can, with reasonable accuracy, select for celiotomy those patients who require repair of injured structures. More importantly the decision to treat in an expectant manner has minimal morbidity and no death attributable to the failure to operate expeditiously. Our approach always has been that abdominal trauma, blunt or penetrating, stab, gunshot, shotgun or any other projectile, is a potential celiotomy which requires clinical indication for operation rather than basing operative indication on etiology.
Over the years the county type hospitals in areas of civilian warfare have reported on their adoption of a selective conservative approach to all types of penetrating injury; in many instances out of practicality in their inability to operate on everybody. Nevertheless the classic mantra remains that gunshot wounds, by definition, demands celiotomy. The authors have stated in their manuscript that selective nonoperative management of lower torso gunshot wounds “may not be applicable to all medical centers.” I disagree. Perhaps the solo practitioner in a small hospital might well adopt the practice of “look and see” rather than “wait and see” because his ability to monitor the rare patient with such injuries is limited but we certainly can expect that the large hospitals in suburban areas with a high volume of blunt trauma now adopt the same standard of resuscitation, evaluation and care for gunshot injuries that they use for the blunt trauma patient. Unfortunately I know from sad experience that many Surgeons, even my own Residents from Kings County Hospital, in practice, will prefer dogma rather than the application of trained surgical judgment.
I thank the Association for the privilege of discussing this excellent paper and congratulate the authors for the courage to carry out this “heretical” study.
Dr. George C. Velmahos: Thank you, Dr. Shaftan, for your kind comments and pioneering work in the field of non-operative management of penetrating abdominal injuries.
Dr. Anthony A. Meyer (Chapel Hill, North Carolina): I rise to congratulate the authors. I would bring up a couple of questions that were raised by the authors — the three deaths and unreliable exam. I think that the reliability exam improves with experience. But I think most people would agree that in fact even in the most reliable hands it is by no means a guaranteed way to identify patients with visceral injuries.
In regard to the consequences of, as you put, unnecessary laparotomy, we didn’t see any data on what the consequences were of yours. And you quoted 22 to 41%. The Cook County data cited as a reason not to operate on patients came from, I think, a group of patients that were possibly managed in a less optimal way.
One comment. Seventeen years ago, I presented a paper at this very location to another organization on selective nonoperative management of blunt liver injury. Seven percent of the liver injuries is what I described as being managed nonoperatively, 7%. Now many more are managed nonoperatively. But unfortunately, some of those are managed nonoperatively to the detriment of the patient.
And my concern is that when you say, and I agree that somebody who knows how to watch these patients can follow them closely, but you say “can,” that gets interpreted by other people as that is an equal opportunity, you can or not operate on patients with gunshot wounds to the abdomen. And I would suggest that in some years to come we will hear about the incidence of late complications.
Two questions: How many patients had trans-peritoneal penetration by the missiles without organ injury? Secondly, how come you have a nine-day average stay for your laparotomy patients? That seems to be excessive, especially those without colostomy or other types of major injury.
Dr. George C. Velmahos: Thank you, Dr. Meyer. Unfortunately I missed some of your comments because the microphone was not working but I will try to answer those that I was able to hear.
Some of the patients we operated on after a period of non-operative management were found to have retroperitoneal bullet trajectories or even intraperitoneal but without major organ injury. Unfortunately, these patients forced us to operate on them because they had progressively increasing abdominal tenderness. I believe that the unnecessary laparotomy rate among these patients is appropriate and similar to or lower than other literature reports.
One may think that unnecessary laparotomies should have a lower morbidity rate and shorter hospital stay than what is reported in our study. When Dr. Feliciano looked at this issue prospectively, he found a much higher morbidity rate than anybody would suspect for patients with unnecessary laparotomy. Additionally, we need to remember that most of our patients with unnecessary laparotomy had extra-abdominal injuries, such as hemothorax, or extremity fractures, which delayed the discharge.
I would like to thank all the discussants and the Association for the privilege of the floor.
Footnotes
Presented at the 121st Annual Meeting of the American Surgical Association, April 26–28, 2001, the Broadmoor Hotel. Colorado Springs, Colorado.
Correspondence: George C. Velmahos, MD, PhD, LAC+USC Medical Center, 1200 N. State St., Rm. 9900, Los Angeles, CA 90033.
E-mail: velmahos@usc.edu
Accepted for publication April 26, 2001.
References
- 1.Demetriades D, Rabinowitz B. Indications for operation in abdominal stab wounds. A prospective study of 651 patients. Ann Surg 1987; 205: 129–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pachter HL, Guth AA, Hosfstetter SR, et al. Changing patterns in the management of splenic trauma: the impact of nonoperative management. Ann Surg 1998; 227: 708–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore EE, Moore JB, van Duzer-Moore S, et al. Mandatory exploration for gunshot wounds penetrating the abdomen. Am J Surg 1980; 140: 847–851. [DOI] [PubMed] [Google Scholar]
- 4.Saadia R, Degiannis E. Non-operative treatment of abdominal gunshot injuries. Br J Surg 2000; 87: 393–397. [DOI] [PubMed] [Google Scholar]
- 5.Demetriades D, Velmahos GC, Cornwell E III, et al. Selective nonoperative management of gunshot wounds of the anterior abdomen. Arch Surg 1997; 132: 178–183. [DOI] [PubMed] [Google Scholar]
- 6.Velmahos GC, Demetriades D, Foianini E, et al. A selective approach to the management on gunshot wounds to the back. Am J Surg 1997; 174: 342–346. [DOI] [PubMed] [Google Scholar]
- 7.Lowe RJ, Salietta JD, Read DR, et al. Should laparotomy be mandatory or selective in gunshot wounds of the abdomen? J Trauma 1977; 17: 903–907. [DOI] [PubMed] [Google Scholar]
- 8.Weigelt JA, Kingman RG. Complications of negative laparotomy for trauma. Am J Surg 1988; 156: 544–546. [DOI] [PubMed] [Google Scholar]
- 9.Shah R, Max MH, Flint LM Jr. Negative laparotomy: Mortality and morbidity among 100 patients. Am Surg 1978; 26: 150–154. [PubMed] [Google Scholar]
- 10.Thal ER, May RA, Beesinger D. Peritoneal lavage: its unreliability in gunshot wounds of the lower chest and abdomen. Arch Surg 1980; 115: 430–433. [DOI] [PubMed] [Google Scholar]
- 11.Muckart DT, Abdool AT, King B. Selective conservative management of abdominal gunshot wounds: a prospective study. Br J Surg 1990; 77: 652–655. [DOI] [PubMed] [Google Scholar]
- 12.Vanderzee J, Christenberry P, Jurkovich GJ. Penetrating trauma to the back and flank. A reassessment of mandatory celiotomy. Am Surg 1987; 53: 220–222. [PubMed] [Google Scholar]
- 13.Demetriades D, Charalambides D, Lakhoo M, et al. Gunshot wounds of the abdomen: role of selective management. Br J Surg 1991; 78: 220–222. [DOI] [PubMed] [Google Scholar]
- 14.Ivatury RR, Simon RJ, Stahl WM. Selective celiotomy for missile wounds of the abdomen based on laparoscopy. Surg Endosc 1994; 8: 366–369. [DOI] [PubMed] [Google Scholar]
- 15.Sosa JL, Arrilaga A, Puente I, et al. Laparoscopy in 121 consecutive patients with abdominal gunshot wounds. J Trauma 1995; 39: 501–504. [DOI] [PubMed] [Google Scholar]
- 16.Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective review of morbidity. J Trauma 1995; 38: 350–356. [DOI] [PubMed] [Google Scholar]
- 17.Ross SE, Dragon GM, O’Malley KF, et al. Morbidity of negative coeliotomy in trauma. Injury 1995; 26: 393–394. [DOI] [PubMed] [Google Scholar]
- 18.Renz BM, Feliciano DV. The length of hospital stay after an unnecessary laparotomy for trauma: a prospective study. J Trauma 1996; 40: 187–190. [DOI] [PubMed] [Google Scholar]
- 19.Hanpeter DE, Demetriades D, Asensio JA, et al. Helical CT scan in the evaluation of mediastinal gunshot wounds. J Trauma 2000; 49: 689–695. [DOI] [PubMed] [Google Scholar]
- 20.Shaftan GW. Selective conservatism in penetrating abdominal trauma. J Trauma 1969; 9: 1026–1028. [DOI] [PubMed] [Google Scholar]
- 21.McAlvanah MJ, Shaftan GW. Selective conservatism in penetrating abdominal wounds: a continuous reappraisal. J Trauma 1978; 18: 206–212. [DOI] [PubMed] [Google Scholar]
- 22.Nance FC, Martin HW, Johnson LW, et al. Surgical judgment in the management of penetrating wounds of the abdomen: Experience with 2,212 patients. Ann Surg 1974; 179: 639–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demetriades D, Rabinowitz B, Sofianos C, et al. The management of penetrating injuries of the back. A prospective study of 230 patients. Ann Surg 1988; 207: 72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velmahos GC, Demetriades D, Cornwell EE III, et al. Gunshot wounds to the buttocks: predicting the need for operation. Dis Colon Rectum 1997; 40: 307–311. [DOI] [PubMed] [Google Scholar]
- 25.Velmahos GC, Demetriades D, Cornwell EE III. Transpelvic gunshot wounds: Routine laparotomy or selective management? World J Surg 1998; 22: 1034–1038. [DOI] [PubMed] [Google Scholar]
- 26.Demetriades D, Gomez H, Chahwan S, et al. Gunshot injuries to the liver: The role of selective nonoperative management. J Am Coll Surg 1999; 188: 290–295. [DOI] [PubMed] [Google Scholar]
- 27.Velmahos GC, Demetriades D, Cornwell EE III, et al. Selective management of renal gunshot wounds. Br J Surg 1998; 85: 1121–1124. [DOI] [PubMed] [Google Scholar]
- 28.Chmielewski GW, Nicholas JM, Dulchavsky SA, et al. Nonoperative management of gunshot wounds of the abdomen. Am Surg 1995; 61: 665–668. [PubMed] [Google Scholar]
- 29.Renz BM, Feliciano DV. Gunshot wounds to the right thoracoabdomen: a prospective study of nonoperative management. J Trauma 1994; 37: 737–744. [DOI] [PubMed] [Google Scholar]
- 30.Nance ML, Nance FC. It is time we told the emperor about his clothes. J Trauma 1996; 40: 185–186. [DOI] [PubMed] [Google Scholar]
- 31.Fabian TC, Croce MA, Stewart RM, et al. A prospective analysis of diagnostic laparoscopy in trauma. Ann Surg 1993; 217: 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]