Abstract
Objective
To evaluate and compare the short- and long-term outcomes in female and male patients after carotid endarterectomy (CEA).
Summary Background Data
Randomized carotid trials have clearly shown the benefits of CEA in specific symptomatic and asymptomatic patients. However, the short- and long-term benefits in women appear to be less clear, and the role of CEA among women with carotid disease remains uncertain.
Methods
During a 21-year period, 1,204 CEAs were performed, 464 (39%) in women and 739 (61%) in men. Complete follow-up was available in 70% of patients.
Results
Women were less likely to have evidence of coronary artery disease, were more likely to be hypertensive, and had a significantly greater incidence of diabetes. The mean age at CEA was 68.5 ± 9.5 years for women and 68.0 ± 8.5 years for men. There were no significant differences in the use of shunts, patching, tacking sutures, or severity of carotid stenoses between men and women. Surgical death rates were nearly identical for asymptomatic and symptomatic patients. Perioperative stroke rates were similar for asymptomatic and symptomatic patients. Life-table stroke-free rates at 1, 5, and 8 years were similar for asymptomatic women and men and symptomatic women and men. Long-term survival rates at 1, 5, and 8 years were higher for asymptomatic women compared with men and for symptomatic women compared with men. As a result, stroke-free survival rates at these follow-up intervals were greater for asymptomatic women compared with men, and for symptomatic women compared to men.
Conclusions
The results from this study challenge the conclusions from the Asymptomatic Carotid Endarterectomy Study and the North American Symptomatic Carotid Endarterectomy Trial regarding the benefits of CEA in women. Female gender did not adversely affect early or late survival, stroke-free, or stroke-free death rates after CEA. The authors conclude that CEA can be performed safely in women with asymptomatic and symptomatic carotid artery disease, and physicians should expect comparable benefits and outcomes in women and men undergoing CEA.
Randomized carotid trials have clearly shown the importance of carotid endarterectomy (CEA) in reducing the risk of stroke for specific symptomatic and asymptomatic patients. 1–5 Public acknowledgment of the results from these trials has led to an apparent change in the practice patterns of surgeons performing this procedure, resulting in a dramatic increase in the number of CEAs being performed in the United States. 6,7 Unfortunately, the randomized trials have not remained free from criticism. Male patients represented the majority of the trial populations, making it difficult to evaluate the outcome of surgery for certain patient subgroups, such as women and minorities. As a result, the short- and long-term benefits of CEA in women appear to be less clear, and the role of CEA surgery among women with carotid disease remains uncertain. 5,8
A review of the more recent literature has provided conflicting information regarding the effect of female gender on the outcome after CEA. Several multicenter reviews, reviews of state-based hospital discharge databases, collective reviews, and large single-center studies have suggested that female gender may be a predictor of complications after CEA and have questioned the value of surgery in women. 6,9–13 Meanwhile, other reports have shown no evidence of gender-based differences in terms of outcome after CEA. 14,15 Various single-institution reviews have specifically addressed the stroke and death rates between women and men after CEA. 16–20 The authors of these reviews concluded that CEA can be performed safely in women, with success rates similar to those observed in men.
The present report highlights our experience with CEA during a 21-year period. The purpose of this review was to evaluate and compare the short- and long-term outcomes in women and men after CEA. By doing so, we sought to provide answers to the following questions: Can CEA be performed safely in women with symptomatic and asymptomatic carotid artery disease? Are the early results in women after CEA comparable to the results in men? Is female gender a risk factor for nonneurologic complications after CEA? Does female gender adversely affect late stroke and death rates after CEA compared with the rates in men? Are the results from our study comparable to the early and late results reported in the Asymptomatic Carotid Atherosclerosis Study (ACAS) and the North American Symptomatic Carotid Endarterectomy Trial (NASCET)? Should the indications for CEA in women remain the same as for men?
MATERIALS AND METHODS
Patients
The computerized cerebrovascular surgery registry at Southern Illinois University School of Medicine identified 1,113 patients who had undergone 1,249 CEAs from March 1976 to October 1997. Data acquisition was retrospective before July 1, 1987, and prospective after that time. Patients were excluded from our review if they underwent simultaneous carotid–subclavian artery bypass or myocardial revascularization, if they underwent primary CEA but were found to have no recorded data, and if they underwent secondary or tertiary CEA.
Surgical Technique
All procedures were performed by vascular surgery fellows or senior general surgery residents under the direct supervision of full-time faculty in the Division of Peripheral Vascular Surgery. Nearly all patients underwent endarterectomy with normocarbic, normotensive general anesthesia. Selective shunting was used when carotid stump pressures were less than 50 mm Hg or when the patient had suffered a prior stroke. Patch angioplasty was performed selectively by some of the authors based on an objective examination of internal carotid artery diameter using caliper measurements (<4 mm in external diameter); others patched routinely. Electroencephalographic monitoring was not used. Completion arteriograms were not obtained, but patency was confirmed by routine continuous-wave Doppler evaluation, performed during surgery after restoration of flow.
Postoperative Data
Our standard practice is to have patients return for clinical evaluation and duplex examination at 6 weeks, 6 months, 12 months, and then yearly after CEA. Information was obtained from clinic charts, hospital records, referring physicians, telephone conversations with the patients, and autopsy or death records of surrounding county offices.
Statistical Analysis
Clinical endpoints were stroke and death. Stroke was defined as any localized neurologic deficit persisting for more than 24 hours, regardless of mechanism and involving the cerebral hemisphere ipsilateral to the endarterectomy. Because of the extended period of time the study encompasses, no attempt was made to distinguish between disabling or nondisabling stroke. Because we were concerned with the effect of the procedure on the neurologic outcome of the hemisphere ipsilateral to the CEA, all data (unless otherwise specified) were analyzed relative to individual arteries rather than patients. The data, therefore, are artery-specific rather than patient-specific.
Comparative data between patient groups were assessed with chi-square analysis, the Fisher exact test, or the Student t test. Cumulative life tables were constructed to assess long-term death, stroke-free, and stroke-free survival rates. Log-rank analysis was used to compare life-table data. Statistical significance was assumed at P < .05.
RESULTS
Demographic data and risk factors were available for 1,068 patients undergoing 1,204 CEAs. We performed 465 CEAs (39%) in 413 women and 739 CEAs (61%) in 655 men. Comparisons between the two groups are shown in Table 1. Mean follow-up was 48.6 ± 39.7 months (range 1–213) for women and 50.9 ± 45.2 months (range 1–242) for men.
Table 1. DEMOGRAPHICS AND RISK FACTORS
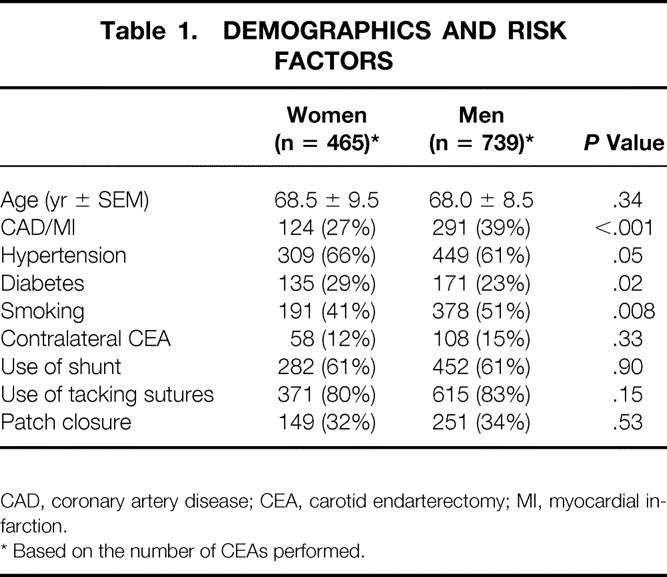
CAD, coronary artery disease; CEA, carotid endarterectomy; MI, myocardial infarction.
* Based on the number of CEAs performed.
Indications for Surgery
The indications for CEA and disease severity are listed in Table 2. The percentage of women and men who presented with clinical symptoms was similar with regard to whether they underwent CEA for permanent (19% vs. 21%) or transient (47% vs. 45%) hemispheric events. There were no significant differences between women and men who presented with or without symptoms with regard to the severity of internal carotid artery disease. Nearly all women and men (99% vs. 98%) undergoing CEA for asymptomatic carotid artery disease satisfied the disease severity inclusion criteria recommended by the ACAS (60–99% diameter-reducing stenosis). Likewise, a similar percentage of women and men (92% vs. 95%) undergoing CEA for symptomatic carotid artery disease satisfied the disease severity inclusion criteria recommended by the NASCET (50–99% diameter-reducing stenosis).
Table 2. PREOPERATIVE INDICATIONS AND DISEASE SEVERITY
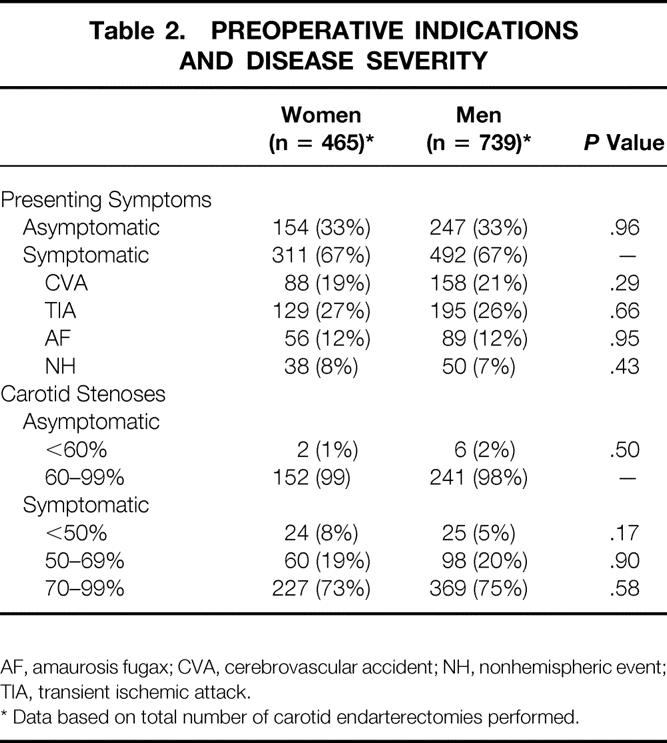
AF, amaurosis fugax; CVA, cerebrovascular accident; NH, nonhemispheric event; TIA, transient ischemic attack.
* Data based on total number of carotid endarterectomies performed.
Early Death Rates
Death data are shown in Table 3. Perioperative death rates were nearly identical for women and men in both the asymptomatic and symptomatic patient subgroups. Overall, seven early deaths occurred within 30 days after CEA. Cardiac-related complications were the cause of death in four (one woman and three men) of the seven early deaths. Two symptomatic men suffered early stroke-related deaths and one man died of septic complications secondary to diabetes mellitus. No early stroke-related deaths occurred in women, and no early deaths occurred in the subgroup of asymptomatic women.
Table 3. EARLY COMPLICATIONS*
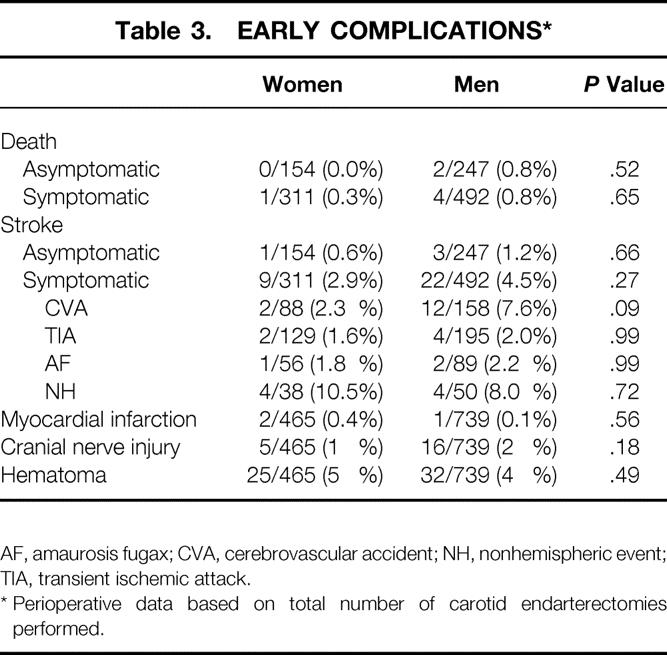
AF, amaurosis fugax; CVA, cerebrovascular accident; NH, nonhemispheric event; TIA, transient ischemic attack.
* Perioperative data based on total number of carotid endarterectomies performed.
Early Stroke Rates
Stroke data are shown in Table 3. Overall, 35 strokes occurred within 30 days of CEA, all but two (one woman and one man) referable to the hemisphere ipsilateral to the endarterectomy. Perioperative stroke rates for women were lower compared with men in both the asymptomatic and symptomatic patient subgroups. In the symptomatic patient subgroup, there was a trend toward a decreased perioperative stroke rate in women who presented with a preoperative stroke (2.3%) compared with men (7.6%) (P = .09).
Other Early Complications
Myocardial infarction occurred rarely after CEA, and cranial nerve injuries and cervical hematomas developed infrequently in both women and men. Overall, there were no significant differences in complication rates between the sexes, and the incidence of myocardial infarction, cranial nerve injury, and hematoma was nearly identical between women and men.
Late Stroke Rates
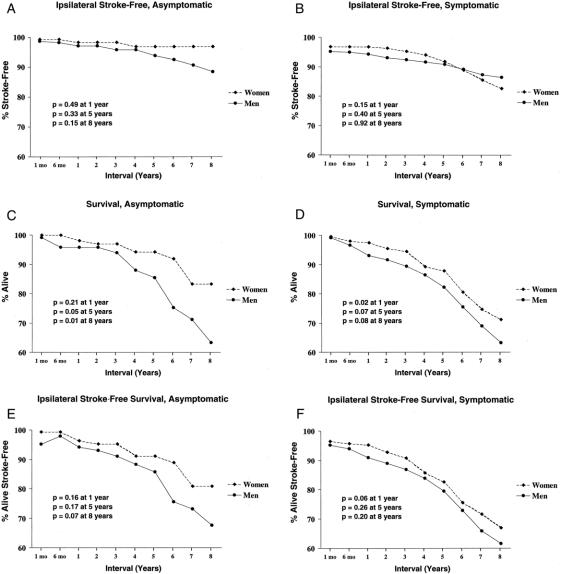
Overall, 48 late ipsilateral strokes had occurred during the first 8 years of follow-up (18 women, 30 men). Life-table analysis of ipsilateral stroke-free rates for women and men are shown in Figures 1 A and 1B. Stroke-free rates for asymptomatic women were higher at every interval of follow-up compared with asymptomatic men, and their stroke-free rates began to diverge after 4 years. These differences never did achieve statistical significance (P > .15). Similarly, comparison of stroke-free rates in symptomatic women versus symptomatic men revealed no significant differences between the sexes (P > .15). However, the stroke-free rates for symptomatic women, although higher than for symptomatic men during the early years of follow-up, decreased below that of symptomatic men shortly after the 5-year follow-up interval.
Figure 1. Life-table survival curves for the treatment groups. Log-rank comparisons are shown at 1-, 5-, and 8-year follow-up intervals. Life-table ipsilateral stroke-free rates for (A) asymptomatic women and men and (B) symptomatic women and men. Life-table survival rates for (C) asymptomatic women and men and (D) symptomatic women and men. Life-table ipsilateral stroke-free survival rates for (E) asymptomatic women and men and (F) symptomatic women and men.
Late Death Rates
Comparison of the causes of late deaths between women and men are shown in Table 4. Overall, the majority of late deaths for both women and men were caused by either cardiovascular disease or malignancy. The incidence of late death was significantly lower in women (10.5%; 49/465) than in men (17.9%; 132/739) (P < .001). This difference was directly attributed to the significantly lower incidence of late cardiac-related deaths suffered by women compared with men (34.6% vs. 54.5%, P = .03). Late stroke-related deaths occurred infrequently in women (8.2%) and men (6.1%). No significant difference was noted between the sexes (P = 0.74).
Table 4. CAUSES OF LATE DEATH
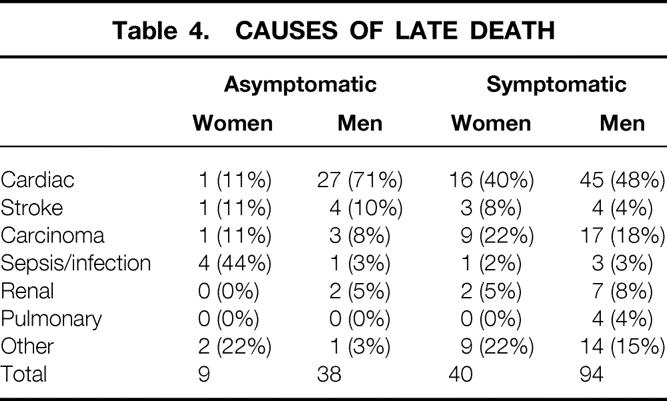
Comparison of survival rates as calculated by life-table analysis between women and men are shown in Figures 1 C and 1D. At every interval of follow-up, asymptomatic women had improved long-term survival compared with asymptomatic men. This survival advantage became statistically significant by the 5-year follow-up interval. Similarly, a greater survival rate was noted in symptomatic women compared with symptomatic men at every year of follow-up after CEA. However, a significant survival advantage for symptomatic women occurred only up to the third year of follow-up (P = .03), after which further analysis revealed no significant differences in the survival rates between the sexes (P > .07).
Life-table analysis of long-term ipsilateral stroke-free survival rates in women and men are shown in Figures 1 E and 1F. A greater stroke-free survival advantage was observed in asymptomatic women compared with asymptomatic men at every interval of follow-up. The stroke-free survival rates between the sexes were significantly different only at the 6-year follow-up interval (P = .05). Likewise, symptomatic women enjoyed higher stroke-free survival rates compared with symptomatic men at every follow-up interval. However, the differences between the sexes were not significantly different at any interval.
DISCUSSION
Several previous series have reported on the perioperative results in women after CEA. 16–22 One series reported unacceptable perioperative death and stroke-morbidity rates in women of 3.4% and 6.9%, respectively. 22 These poor results appeared to be related to an excessive number of complications observed in black women undergoing CEA, a subgroup of patients not well represented in the randomized trials. 1,5 Perioperative death and stroke-morbidity rates in other series ranged from 0.0% to 0.6% and 0.0% to 2.4%, respectively. Few of the investigators reported their results based on asymptomatic and symptomatic patient subgroups, so comparisons of outcomes between each of the series have been problematic. Most series have found no significant difference in the early death and stroke-morbidity rates between women and men after CEA. Hertzer et al 12 reviewed in-hospital stroke and death rates of 2,228 patients undergoing CEA and found a significantly higher perioperative stroke rate in women undergoing isolated CEA compared with men (2.8% vs. 1.3%, P = .05). Using a multivariate model, they concluded that the composite stroke and death rate was significantly influenced by female gender (P = .05). The perioperative death and stroke-morbidity rates in women reported from these earlier series are comparable to the overall combined perioperative death (0.0–0.3%) and stroke-morbidity (0.6–2.9%) rates of women reported in our study.
Two studies reported on long-term outcomes after CEA. 16,17 Schneider et al 16 reported that women enjoyed better 5-year survival rates than men (95% vs. 85%, P = .48) and 30-month stroke-free rates similar to those of men (96% vs. 97%, P = .55). The authors concluded that they were equally likely to recommend CEA to women as to men. More recently, Ballotta et al 17 reported that no late strokes occurred in their female patients, and cumulative life-table survival rates at 7 years were comparable in women and men (82.3% vs. 79.6%, P = .80). Again, similar to the earlier study, the authors concluded that early and late outcomes were comparable in women and men. In our series, survival and stroke-free rates at 7 years for asymptomatic and symptomatic women were 83.3% and 74.7% and 96.9% and 90.7%, respectively.
Although the ACAS reported the surgical results in the sexes separately, this was not the primary endpoint for the study. 5,23 Nonetheless, it remains the standard by which surgeons and their results are currently judged and compared, deficiencies notwithstanding.
The incidence of perioperative stroke or death in the ACAS was nearly twice as high in the surgical arm of the study for women (3.6%) than for men (1.7%), but this difference was not statistically significant (P = .12). 5 However, when evaluating the relationship between perioperative stroke alone and the effect of gender, no significant differences were noted. 23 The findings in our study differ from those reported in the ACAS. The combined perioperative stroke and death rate of 0.6% for women in our study was much lower compared with that of men in our study (2.0%) and with the perioperative stroke and death rates observed for women and men in the ACAS. In addition, the perioperative ipsilateral stroke rates in our study were similar for women (0.6%) and men (1.2%) and were slightly lower than the overall ipsilateral perioperative stroke rate of 1.5% reported in the ACAS.
The ACAS showed that success in long-term stroke reduction after CEA is ultimately dependent on low perioperative stroke and death rates. 5,23 Carotid endarterectomy was more effective in reducing the 5-year ipsilateral stroke rate in men than in women (4.1% vs. 7.3%). The 5-year relative stroke risk reduction was 66% for men and just 17% for women, but this difference was not significant (P = .10). When patients with perioperative events are removed from long-term analysis, the 5-year relative risk reduction improved threefold to 56% for women and increased to 79% for men. Conversely, an increase in the complication rate by two percentage points would have reduced long-term benefits by more than 30%. 7 Although the early and late outcomes in women and men in the ACAS were not reported as being significantly different, the conclusions put forth by the investigators indicated that men were adequately protected from stroke by CEA but women were not.
Based on the results from our study, and contrary to the conclusions from ACAS, we believe that women can enjoy long-term stroke reduction similar to that observed in men after CEA. We support the concept, as do other investigators, 12,16–20 that the perioperative complication rate reported in women in the ACAS is excessive and may not represent the current state of the art regarding carotid surgery. In the ACAS, the 5-year event rate in the medical arm was lower for women than men (8.7% vs. 12.1%), but the difference was not significant (P = .17). The lower perioperative complication rate in men, although not significantly different than the rate in women (P = .12), would appear to be the single critical correctable factor that allowed men to achieve a greater 5-year freedom from events after CEA than women. The ipsilateral stroke-free rate at 5-year follow-up for women in our study was 96.9%, which is greater than that reported for women (92.7%) and men (95.9%) in the ACAS, and greater than the rate observed for men in our study (92.9%) (P = .19). Our data reinforce the idea that if perioperative complication rates in women after CEA are maintained at or decreased below the perioperative complication rates reported for men in ACAS, comparable long-term stroke reduction can be achieved for women. Everything considered, if the perioperative complication rates had been better for women, the message from ACAS regarding the benefits of CEA in women might have been received differently by both the medical community and the public at large.
Of the multitude of reports published regarding the results from the NASCET, only two have provided data documenting the outcome in women. 8,21 In these reports, gender was not found to be associated with either an increased or decreased risk of perioperative stroke or death. The results from our study support these findings because we observed no significant difference in the perioperative stroke or death rates between symptomatic women and men (2.9% vs. 4.5% and 0.3% vs. 0.8%, respectively). Further, the overall combined perioperative stroke, death, and combined stroke and death rates from our study appear better than those reported in the NASCET (3.8% vs. 5.4%, 0.6% vs. 1.1%, and 3.9% vs. 6.5%). Unfortunately, we could not directly compare our gender-specific results because similar data were not provided by the NASCET.
With respect to the long-term durability of CEA in asymptomatic and symptomatic patients, surgery provided similar benefits for women and men in our study. The ipsilateral stroke-free rate at 8 years was slightly lower for women than for men (82.6% vs. 86.4%), but the difference was not statistically significant (P = .92). Similar long-term stroke-free benefits for women and men with 50% to 99% diameter-reducing stenoses undergoing CEA were reported from the NASCET. The ipsilateral stroke-free rates at 8 years were 81.9% for women and 82.3% for men. Unfortunately, our study comprised a high percentage of symptomatic women with severe carotid disease (70–99% diameter-reducing stenosis), and our 5-year stroke-free results may not be strictly comparable to the 5-year stroke-free rates of women in the NASCET, the majority (75%) of whom were noted to have moderate carotid disease (50–69% diameter-reducing stenosis).
In our study, the incidence of patch angioplasty closure of the carotid artery was similar between women and men (see Table 1). Overall, there was no significant difference in the perioperative stroke rates in patients who received patch angioplasty compared with patients who underwent primary closure of the arteriotomy (2.3% vs. 3.2%, P = .44) (Table 5). However, when the results were separated by gender, we discovered an unanticipated benefit in stroke reduction in women who received patch angioplasty compared with men. No perioperative strokes occurred in women who received patch angioplasty. This finding was significantly different compared with the stroke rate in men who received patch angioplasty (0.0% vs. 3.6%, P = .03). Further, women who received patch angioplasty had a significantly lower perioperative stroke rate than did women who underwent primary closure. Patch angioplasty did not produce the same neurologic benefits in men. Perioperative stroke rates were similar in men who received patch angioplasty or underwent primary closure of the carotid artery.
Table 5. PERIOPERATIVE STROKE RATES
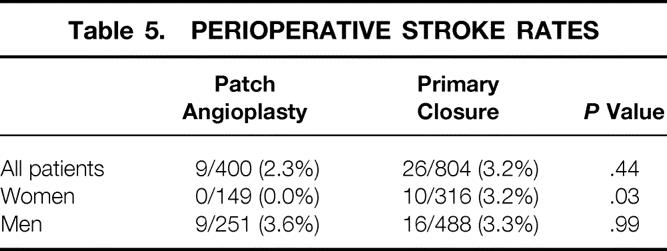
Recent studies specifically comparing the outcomes of women versus men after CEA have provided some data concerning the potential value of patch angioplasty in reducing the risk of perioperative stroke in these patient subgroups; the randomized trials have provided none at all. In the series reported by Akbari et al, 19 in contrast to the data reported from our study, a significantly greater percentage of women received patch angioplasty than men (59% vs. 50%, P = .002). However, the increased incidence of patch angioplasty observed in women did not translate into a lower perioperative stroke rate compared with men receiving patch angioplasty (1.3% vs. 1.5%, P = .99). Further, comparisons with women who underwent primary closure identified a similar lack of benefit (1.3% vs. 0.9%, P = .68).
Serial observations by Hertzer et al 12,24 regarding the effects of patch angioplasty on the perioperative stroke rates have shown that vein patch angioplasty enhances the early outcome of CEA. A more recent update of their data indicates that although vein patch angioplasty does indeed reduce the risk of perioperative stroke in both women and men, it does to a greater extent in men. Vein patch angioplasty decreased stroke rates from 1.1% to 0.4% in men and from 3.3% to 1.7% in women (P = .02) (Hertzer NR, personal communication, April 26, 2001). These findings are somewhat at odds with the results from our study: we found no advantage of patch angioplasty in reducing the risk of perioperative stroke in men. This basic difference in the outcomes between the two studies may revolve around the fact that greater than 90% of the patients in the series from Hertzer et al 12 underwent patch angioplasty, whereas only 33% of our patients received patch angioplasty. The large differences in the sizes of the patient groups in the study by Hertzer et al 12 may have inadvertently skewed the statistical analysis in favor of patching. However, many of our data were accumulated retrospectively, and different criteria (objective vs. subjective) were used by each of the authors to determine whether to use patch angioplasty. Accordingly, any direct comparison of the corresponding perioperative death and stroke death rates between women and men, and comparisons against other studies describing the benefits of patching, should be interpreted with circumspection.
The primary drawback of this study is that although our data have been accumulated prospectively since 1987, our observations and conclusions are based on a retrospective analysis of the data. This imperfect method of data analysis has resulted in gaps in our knowledge base regarding long-term follow-up in about 30% of our patients. Also, we could not obtain additional risk factor data, thereby precluding us from performing a multivariate analysis to assess the effect of confounding variables on the outcomes in women and men. In addition, although we have previously published information detailing the relationship between recurrent carotid stenosis and postoperative neurologic events, 25,26 no data were provided in this study regarding the effect of gender on the development of recurrent carotid stenosis and the occurrence of late neurologic events. We are resolving these deficits, and until we do so, we would urge caution in the rigid transference of our findings to one’s own clinical practice.
Nonetheless, this series represents an in-depth evaluation of the short- and long-term risks and benefits of CEA in women versus men. Our results provide answers to our earlier questions. First, we have shown that in experienced hands, CEA can be performed safely in carefully selected women with asymptomatic and symptomatic carotid artery disease. Second, the perioperative death and stroke rates achieved in women in this study are comparable and in most cases superior to the rates observed in asymptomatic and symptomatic men undergoing CEA. Third, we have shown that female gender does not adversely affect early or late survival, stroke-free, or stroke-free survival after CEA. Fourth, the long-term benefits in survival and stroke reduction for women after CEA are superior to the benefits achieved in men in this study and are comparable to the results reported for women in the ACAS and the NASCET. Fifth, patch angioplasty produced an early benefit in women by significantly reducing their risk of perioperative stroke compared with men.
CONCLUSIONS
Results and concerns from the ACAS and NASCET regarding the lack of perceived benefit of CEA for asymptomatic and symptomatic women do not correlate with the findings from our study. In the final analysis, the indications for CEA in women with asymptomatic and symptomatic carotid artery disease should not differ from those applied to men. Further, physicians should expect comparable outcomes and benefits in women and men undergoing CEA.
Acknowledgments
The authors thank Mary Garfield, BS, MT(ASCP), for her assistance in data storage and compilation, and our former partner, Lynne D. Barkmeier, MD, for her contribution in providing a portion of this patient population for review.
Discussion
Dr. Norman R. Hertzer (Cleveland, Ohio): I have always admired the reports concerning carotid endarterectomy from Southern Illinois University, and I appreciate the invitation to review this manuscript and participate in its discussion.
The NASCET never showed any distinctions between men and women with respect to perioperative risk. The impression that surgical treatment was less effective in symptomatic women is predicted on the fact that strokes occurred less frequently in women than in men who were randomized to nonoperative management. This also was the case in the ACAS, but asymptomatic women did seem to have a slightly higher risk for postoperative stroke and/or death – 3.6% versus 1.7% in men – that approached, but did not quite attain statistical significance. (The P-value for this comparison was 0.12.)
None of us at the Cleveland Clinic has ever recognized an obvious difference in the early risk of carotid endarterectomy between men and women. If we look closely enough at our data, however, such a difference does appear to exist and will be reported at the Eastern Vascular Society meeting next week.
From 1989 through the year 2000, we performed operations for asymptomatic carotid stenosis in 1,312 men and 686 women, or more than twice the number of patients in the ACAS. The combined stroke and mortality rate was 0.8% in men and 2.5% in women, with a convincing P-value of 0.004. Vein patching was associated with low stroke rates of 0.4% in 852 men and 1.7% in 471 women, but these results still were significantly different at a P-value of 0.02. The stroke rates in conjunction with synthetic patches and a few primary closures were 1.1% in men and 3.3% in women, and the P-value for this comparison just barely failed to gain significance at 0.06.
In summary, while our results in women are a little better than those in the ACAS, they still indicate that women probably do have more perioperative complications than men. Dr. Mattos found in his own large series that gender did not influence the early risk of carotid endarterectomy despite the fact that only 32% of the women in this series received patch angioplasty. This is interesting because there is a considerable amount of information elsewhere to suggest that women have something to gain from patching on the basis of the relatively small size of their internal carotid arteries. So, Dr. Mattos, my question is whether patching had any effect in your outcomes in women, or, for that matter in men?
This report contains a lot of reliable data and it should be a valuable contribution to the literature on carotid endarterectomy.
Presenter. Dr. Mark A. Mattos (Springfield, Illinois): Dr. Hertzer, thank you very much for your kind comments. I did not show any data regarding the results following patch angioplasty on slides today because of allotted time constraints but data regarding outcomes and patching in women and men is detailed in the manuscript. We observed that there was a significant benefit in women who underwent patch angioplasty. In fact, none of the women in our study who underwent patch repair suffered a perioperative stroke. In contrast, the perioperative stroke rate in men who underwent patch angioplasty was 3.6%. For women who underwent primary repair the stroke rate was 3.2%. There was no difference in the perioperative stroke rates between men who underwent primary repair vs. patch angioplasty.
Dr. Bruce A. Perler (Baltimore, Maryland): At the 1957 annual meeting of the American Surgical Association, Galbraith and Lyons presented a series of six patients who underwent bypass grafts for symptomatic carotid exclusive disease. We have come a long way since that time.
Today, carotid endarterectomy is the most frequently performed peripheral vascular procedure in this country – and for good reason. As demonstrated in the NASCET and ACAS trials, carotid endarterectomy prevents strokes and saves lives. Yet subgroup analysis, as Dr. Mattos pointed out, has raised an important question: Is the benefit of carotid endarterectomy gender specific? In both trials, the long-term benefit was greater in men and in ACAS women experienced double the perioperative stroke and mortality rate. This issue is particularly relevant at a time when some are advocating carotid stenting as a less invasive and potentially less risky treatment for carotid disease.
Dr. Mattos and his colleagues have demonstrated that in the hands of experienced vascular surgeons, carotid endarterectomy is a very safe and gender-neutral operation. In this 21-year experience including 1,204 cases, the perioperative stroke and mortality rate was 3.6%, and early and long-term outcome was slightly better in women.
One potential limitation of this study is the retrospective nature of the data analysis. Approximately 25% of the patients were lost to follow-up during the first postoperative year. Nevertheless, the major end-points of perioperative death and stroke are very objective, so the results that we just heard are truly outstanding. I have several questions.
As you pointed out in the manuscript and in response to the last question, carotid patching clearly reduced the incidence of stroke in women. Do you now routinely patch all female patients, and have you identified any other factors that favorably, or unfavorably, impacted on outcome?
Secondly, half of the surgical morbidity in the ACAS was in fact angiographically-related strokes. How many of your patients underwent preoperative arteriograms, and have you included angiographic complications in the assessment of morbidity?
Third, your long-term freedom-from-stroke data was actually superior to what was reported in NASCET and ACAS. How confident are you that this very favorable outcome was not influenced at least in part by the retrospective nature of the study?
Finally, your group has been a major leader in endovascular techniques. In view of that expertise and the results you have just presented, could you speculate on the appropriate role of carotid stenting in the management of uncomplicated carotid disease in the future?
Dr. Mark A. Mattos: Dr. Perler, I appreciate your insight and kind words. I will try to answer your questions in order. My practice has been to perform selective patch angioplasty for women and men when the external diameter of the internal carotid artery as measured by calipers was less than 4mm. However, based on the results from this study I will most likely proceed with routine patch angioplasty for all women who undergo carotid endarterectomy, regardless of the diameter of the internal carotid artery. We have not been able to identify other factors that have impacted on outcome, either favorable or unfavorably.
In regards to stroke-related complications following diagnostic carotid angiography, I do not any information regarding the time period from 1976 to 1991 since the radiologists performed the angiograms during this time period. However, from 1992 to the present our group have been performing diagnostic angiograms ourselves. During this period we have had a single stroke-related complication resulting in a stroke rate of well less than 1%.
In terms of our long-term freedom from stroke I believe that our data is real despite a lack of follow-up in approximately 30% of patients. I certainly believe that if you can minimize the perioperative complications a long-term benefit can be realized for both women and men.
You asked if we should performing carotid stenting in asymptomatic patients? I do not believe that at the present time we can justify performing carotid stenting for primary carotid stenosis. The natural history of patients with asymptomatic 60–99% carotid stenosis is relatively benign and the stenting data at present with current technology as it exists today just doesn’t measure up. Additionally, there is a cost issue that we as a society needs to consider. The use of stents in treating asymptomatic patients may be result in an excessive cost-benefit ratio that society is not going to be willing to pay for.
Dr. Michael E. Debakey (Houston, Texas): I have enjoyed this presentation and wanted to express my congratulations to the authors for their excellent study and admirable results. As you may know, I have been interested in carotid endarterectomy since I performed my first case in 1953.
Since that time, I have performed this procedure on more than 3,000 patients, whose follow-up is 95% complete. As you will observe from this slide, showing Kaplan-Meier survival probability for males and females, I can confirm the authors’ conclusions. Indeed, it would appear from my series that females have a significantly better survival expectancy than males over a follow-up of more than 35 years.
In addition, there was no significant difference in age between males (63.2 years, standard deviation 8.4 years) and females (62.8 years, standard deviation 9.2 years). Likewise, there was no significant difference in the incidence of diabetes between the sexes, with males having an incidence of 17.3% and females an incidence of 16.1% (p=0.463). The incidence of prior cardiac disease in my series was significantly different between the sexes, with males having an incidence of 45.7% and females an incidence of 38.1%, in agreement with the presentation here. Also, in my series, hypertension was more likely to occur in women (62.2%) than men (48.8%), with a chi-square of 39.05 and a p-value less than 0.0001.
The final question I would like to ask is: would you comment on your observations by sex in patients who had bilateral lesions requiring endarterectomy.
Dr. Mark A. Mattos: Thank you Dr. Debakey for your kind remarks. I am honored and awed by your nearly 40-year personal experience and excellent results in performing carotid endarterectomy. To answer your question, we noted that 139 patients underwent bilateral carotid endarterectomy in our series. We did not observe a significant difference in the combined perioperative stroke rate for this subset of patients as compared to those women and men who received unilateral carotid endarterectomy. Additionally, there was no difference in the perioperative stroke rate between women and men who underwent bilateral carotid endarterectomy.
Footnotes
Presented at the 121st Annual Meeting of the American Surgical Association, April 26–28, 2001, the Broadmoor Hotel, Colorado Springs, Colorado
Correspondence: Mark A. Mattos, MD, Associate Professor of Surgery, Director of Endovascular Surgery, University of Washington School of Medicine, 1959 N.E. Pacific Street, Box 356410, Seattle, WA 98195-6165.
E-mail: mmattos@u.washington.edu
Accepted for publication April 26, 2001.
References
- 1.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991; 325: 445–453. [DOI] [PubMed] [Google Scholar]
- 2.Mayberg MR, Wilson SE, Yatsu F, et al. Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. JAMA 1991; 266: 3289–3292. [PubMed] [Google Scholar]
- 3.The European Carotid Surgery Trials’ Collaborative Group. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70–99%) or with mild (0–29%) carotid stenosis. Lancet 1991; 337: 1235–1243. [PubMed] [Google Scholar]
- 4.Hobson RW II, Weiss DG, Fields WS, et al. Efficacy of carotid endarterectomy for asymptomatic carotid stenosis. N Engl J Med 1993; 328: 221–227. [DOI] [PubMed] [Google Scholar]
- 5.Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA 1995; 273: 1421–1428. [PubMed] [Google Scholar]
- 6.Huber TS, Wheeler KG, Cuddeback JK, et al. Effect of the asymptomatic carotid atherosclerosis study on carotid endarterectomy in Florida. Stroke 1998; 29: 1099–1105. [DOI] [PubMed] [Google Scholar]
- 7.Chassin MR. Appropriate use of carotid endarterectomy. N Engl J Med 1998; 339: 1468–1471. [DOI] [PubMed] [Google Scholar]
- 8.Barnett HJM, Taylor D, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. N Engl J Med 1999; 339: 1415–1425. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein LB, Samsa GP, Matchar DB, Oddone EZ. Multicenter review of perioperative risk factors for endarterectomy for asymptomatic carotid artery stenosis. Stroke 1998; 29: 750–753. [DOI] [PubMed] [Google Scholar]
- 10.Rothwell PM, Slattery J, Warlow CP. Clinical and angiographic predictors of stroke and death from carotid endarterectomy: systematic review. Br Med J 1997; 315: 1571–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Golledge J, Cuming R, Beattie DK, et al. Influence of patient-related variables on the outcome of carotid endarterectomy. J Vasc Surg 1996; 24: 120–126. [DOI] [PubMed] [Google Scholar]
- 12.Hertzer NR, O’Hara PJ, Mascha EJ, et al. Early outcome assessment for 2228 consecutive carotid endarterectomy procedures: the Cleveland Clinic experience from 1989 to 1995. J Vasc Surg 1997; 26: 1–10. [DOI] [PubMed] [Google Scholar]
- 13.Frawley JE, Hicks RG, Woodforth IJ. Risk factors for perioperative stroke complicating carotid endarterectomy: selective analysis of a prospective audit of 1000 consecutive operations. Aust NZ J Surg 2000; 70: 52–56. [DOI] [PubMed] [Google Scholar]
- 14.McCory DC, Goldstein LB, Samsa GP, et al. Predicting complications of carotid endarterectomy. Stroke 1993; 24: 1285–1291. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein LB, Hasselblad V, Matchar DB, McCory DC. Comparison and meta-analysis of randomized trials of endarterectomy for symptomatic carotid artery stenosis. Neurology 1995; 45: 1965–1970. [DOI] [PubMed] [Google Scholar]
- 16.Schneider JR, Droste JS, Golan JF. Carotid endarterectomy in women versus men: patient characteristics and outcomes. J Vasc Surg 1997; 25: 890–898. [DOI] [PubMed] [Google Scholar]
- 17.Ballotta E, Renon L, Da Giau G, et al. Carotid endarterectomy in women: early and long-term results. Surgery 2000; 127: 264–271. [DOI] [PubMed] [Google Scholar]
- 18.Sternbach Y, Perler BA. The influence of female gender on the outcome of carotid endarterectomy: a challenge to the ACAS findings. Surgery 2000; 127: 272–275. [DOI] [PubMed] [Google Scholar]
- 19.Akbari CM, Pulling MC, Pomposelli FB, et al. Gender and carotid endarterectomy: does it matter? J Vasc Surg 2000; 31: 1103–1109. [DOI] [PubMed] [Google Scholar]
- 20.Rockman CB, Castillo J, Adelman MA, et al. Carotid endarterectomy in female patients: are the concerns of the Asymptomatic Carotid Atherosclerosis Study valid? J Vasc Surg 2001; 33: 236–241. [DOI] [PubMed] [Google Scholar]
- 21.Ferguson GG, Eliasziw M, Barr HW, et al, for the NASCET Collaborators. The North American Symptomatic Carotid Endarterectomy Trial. Surgical results in 1415 patients. Stroke 1999; 30:1751–1758. [DOI] [PubMed]
- 22.Rigdon EE. Racial and gender differences in outcome after carotid endarterectomy. Am Surg 1998; 64: 527–532. [PubMed] [Google Scholar]
- 23.Young B, Moore WS, Robertson JT, et al, for the ACAS Investigators. An analysis of perioperative surgical mortality and morbidity in the Asymptomatic Carotid Atherosclerosis Study. Stroke 1996; 27: 2216–2224. [DOI] [PubMed] [Google Scholar]
- 24.Hertzer NR, Beven EG, O’Hara PJ, Krajewski LP. A prospective study of vein patch angioplasty during carotid endarterectomy: three-year results for 801 patients and 917 operations. Ann Surg 1987; 206: 628–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mattos MA, van Bemmelen PS, Barkmeier LD, et al. Routine surveillance after carotid endarterectomy: does it affect clinical management? J Vasc Surg 1993; 17: 819–831. [PubMed] [Google Scholar]
- 26.Mattos MA, Hodgson KJ, Ramsey DE, Sumner DS. Clinical outcome of patients developing transient ischemic attacks following carotid endarterectomy. Vasc Surg 2000; 34: 471–474. [Google Scholar]