Abstract
Objective
To analyze the impact of a conservative strategy of management in patients with necrotizing pancreatitis, reserving intervention for patients with documented infection or the late complications of organized necrosis.
Summary Background Data
The role of surgery in patients with sterile pancreatic necrosis remains controversial. Although a conservative approach is being increasingly used, few studies have evaluated this strategy when applied to the entire spectrum of patients with necrotizing pancreatitis.
Methods
The authors reviewed 1,110 consecutive patients with acute pancreatitis managed at Brigham and Women’s Hospital between January 1, 1995, and January 1, 2000, focusing on those with pancreatic necrosis documented by contrast-enhanced computed tomography. Fine-needle aspiration, the presence of extraintestinal gas on computed tomography, or both were used to identify infection.
Results
There were 99 (9%) patients with necrotizing pancreatitis treated, with an overall death rate of 14%. In three patients with underlying medical problems, the decision was made initially not to intervene. Of the other 62 patients without documented infection, all but 3 were managed conservatively; this group’s death rate was 11%. Of these seven deaths, all were related to multiorgan failure. Five patients in this group eventually required surgery for organized necrosis, with no deaths. Of the 34 patients with infected necrosis, 31 underwent surgery and 3 underwent percutaneous drainage. Only four (12%) of these patients died, all of multiorgan failure. Of the total 11 patients who died, few if any would have been candidates for earlier surgical intervention.
Conclusions
These results suggest that conservative strategies can be applied successfully to manage most patients with necrotizing pancreatitis, although some will eventually require surgery for symptomatic organized necrosis. Few if any patients seem likely to benefit from a more aggressive strategy.
The management of necrotizing pancreatitis (NP) has undergone considerable evolution. Although the role of surgical therapy in this condition has remained controversial, recent advances in our understanding and care of these patients have considerably focused this debate. Today, with improvements in the care of the critically ill, many patients with severe acute pancreatitis survive the early systemic inflammatory response and enter a second phase of illness dominated by sepsis and the consequences of organ failure. 1,2 Patients with significant pancreatic necrosis, at highest risk for such complications, can now be identified with contrast-enhanced computed tomography (CT) 3 and the presence or absence of infection can be established using fine-needle aspiration (FNA). 4 Although the need for intervention in patients with pancreatic infection is undisputed, the success of this technology in distinguishing between infected and sterile necrosis has raised the issue of whether infection should be the only indication for surgery in the initial management of NP. 5,6 Opponents of this strategy have continued to suggest that there are some patients with the most severe disease, based on the extent of necrosis or organ failure, who might benefit from debridement regardless of the status of infection. 7,8
Arguments for and against the conservative approach have been based largely on the results of select and nonrandomized series from surgical referral centers. 5–10 Despite the lack of convincing data, it was our impression that we had increasingly adopted a conservative strategy at our institution, reserving intervention for patients with documented infection or the small group of patients who recover from the acute inflammatory process but suffer from symptoms related to organized necrosis. Acknowledging our bias in favor of conservative therapy, we have remained sympathetic to the concept that there may be a subset of patients with severe sterile necrosis who would benefit from surgery regardless of the status of infection; however, it was our impression that this group is relatively small. In this context, we reviewed our institutional experience, including the entire spectrum of patients with NP, focusing on the success of conservative therapy.
METHODS
Patient Identification
We reviewed the hospital charts and computerized medical records of all patients with acute pancreatitis consecutively admitted to Brigham and Women’s Hospital from January 1, 1995, through January 1, 2000. The search was confined to patients with the International Classification of Disease-9 (ICD-9) code for acute pancreatitis (code 577.0) using a computer-assisted hospitalization analysis for the study of efficacy (CHASE) management system. Review then focused on patients with pancreatic necrosis documented on dynamic contrast-enhanced CT. All scans were rereviewed by a single radiologist, unaware of the clinical course, for confirmation. The protocol was approved by the Brigham and Women’s Hospital Committee for the Protection of Human Subjects.
Study Design
The hospital records of the patients with confirmed pancreatic necrosis were reviewed for demographic data as well as the following: the cause of the pancreatitis; the site of diagnosis (transfer, emergency room, inpatient); APACHE II scores at admission (the score for transfer patients was calculated based on data retrieved from the referring hospital); the maximal extent of necrosis, measured by contrast-enhanced CT, expressed as a percentage of the whole pancreas and classified into less than 30%, 30% to 50%, and more than 50% during the hospital stay; the presence of organ failure, defined by shock (systolic blood pressure <90 mm Hg), pulmonary insufficiency (Pao2 <60 mm Hg), renal failure (creatinine level > 2 mg/dL after rehydration), or gastrointestinal bleeding (>500 mL/24 hours); the presence or absence of infection, defined as a positive gram stain and/or culture on FNA and/or the presence of extraintestinal air on CT; the use of antibiotics; the type of intervention and its timing; surgical complications; death (cause and timing in relation to date of admission); length of stay in relation to date of admission and intervention; and the need for readmission.
In addition, management was analyzed to determine the success of a conservative strategy. This strategy was defined as intervention, either by surgery or percutaneous drainage, for only two indications: the presence of infection, as defined previously, or symptomatic organized necrosis. Symptomatic organized necrosis was further defined as pain and/or inability to tolerate oral feeding persisting at least 3 weeks after the onset of illness. Finally, in the patients who died, we attempted to identify those who might have benefited from a more aggressive approach to intervention.
Statistics
Comparison of continuous variables between two groups was performed using the Wilcoxon matched pairs test. Results of continuous data are expressed as mean (range). Categorical data were compared using the chi-square and Fisher exact test when appropriate. A two-tailed P < .05 was considered statistically significant.
RESULTS
Patient Characteristics
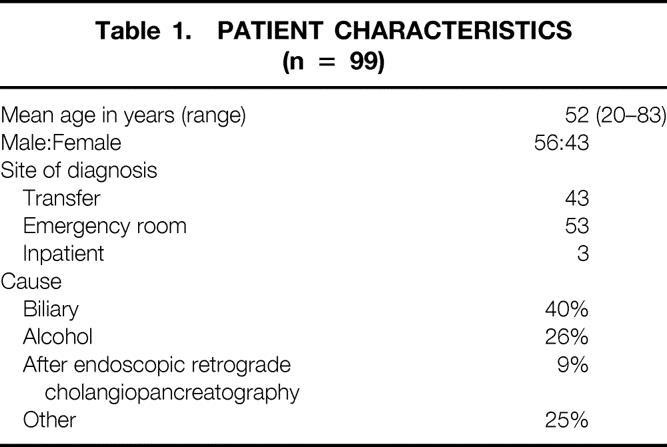
The patient characteristics are summarized in Table 1. There were a total of 99 patients with evidence of pancreatic necrosis on contrast-enhanced CT, representing 9% of the 1,110 patients admitted to the hospital for acute pancreatitis during the 5-year period. Although Brigham and Women’s Hospital serves as a tertiary referral center, fewer than half of these patients were initially admitted at another hospital before transfer to our institution. For 74 patients, this was their first episode of pancreatitis; the remainder had suffered one or more episodes of pancreatitis before this admission for necrosis. In most patients, the cause was biliary or alcohol-induced, although nine patients developed necrosis after endoscopic retrograde cholangiopancreatography. There were three elderly patients with multiple chronic medical conditions in whom the decision was made not to proceed with any further therapy (“do not resuscitate” [DNR]); these patients were excluded from the subsequent analysis.
Table 1. PATIENT CHARACTERISTICS (n = 99)
Disease Severity
The mean APACHE II score at admission to either Brigham and Women’s Hospital or the referring institution hospital was 7 (range 0–22). Review of CT scans to determine the extent of necrosis revealed that there were 39 patients with less than 30%, 30 patients with 30% to 50%, and 27 patients with more than 50%. Forty-four patients developed organ failure during their hospital stay. Of these, 19 had single organ failure and the remaining 25 had multiorgan failure. Hypotension was present in 9 patients, pulmonary insufficiency in 36 patients, renal insufficiency in 25 patients, and gastrointestinal bleeding in 2 patients.
Infection
Based on the results of CT and FNA in patients with suspected infection, there were 62 patients with sterile necrosis and 34 with infection. In four patients, the diagnosis was established by the presence of extraintestinal gas on CT; the remainder were identified by FNA. There were 55 patients who had a total of 83 FNAs. Of these, 37 patients had one FNA, 10 had two FNAs, and 8 had three or more FNAs. Of the 30 patients with FNA showing infection, the first aspirate was positive in 17 (57%); 7 (23%) required two and 6 (20%) required three or more FNAs to establish the diagnosis. The results of cultures and the pattern of microorganisms were for the most part similar to those in other series. 6,8 Staphylococcal species accounted for 33% of isolates, followed by Escherichia coli (22%) and Klebsiella (13%). Candida was isolated in only 3%. There were only two patients in whom the results of FNA and intraoperative cultures did not correlate. One was a patient with a negative FNA who underwent exploration because of progressive acidosis; intraoperative cultures grew Candida. The other patient’s FNA revealed coagulase-negative Staphylococcus but grew E. coli and Bacteroides from intraoperative cultures.
Management and Outcomes
Table 2 summarizes the overall management and outcome in the 99 patients. Of the 96 patients considered potential candidates for surgery for NP, 34 underwent either surgery (n = 31) or percutaneous drainage (n = 3). The rest (63 patients) were managed conservatively, and five (8%) of these eventually required surgery for symptomatic organized necrosis. Forty-two (78%) received prophylactic antibiotics; most were treated with the combination of ampicillin, gentamicin, and metronidazole, although a significant number received imipenem or ceftazidime. The overall death rate was 14%, but only 11% if the 3 DNR patients are excluded. In the 36 patients who underwent surgery either for NP or organized necrosis, there were 5 (13%) deaths; in the group managed without surgery, 6 of the 60 (10%) patients died. None of the 4 patients who died early (within 14 days) were managed surgically; 5 of the 10 patients who died late had undergone surgery. The mean length of stay for the survivors was 35 days (range 2–221). Only 20 (23%) required readmission.
Table 2. SUMMARY OF MANAGEMENT AND OUTCOME
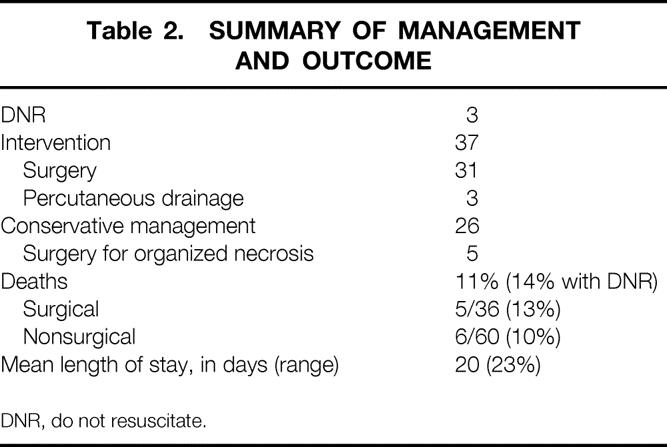
DNR, do not resuscitate.
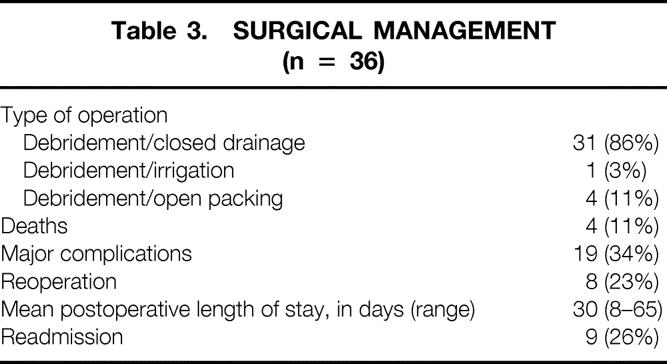
Surgical Therapy
The results of surgical intervention in 36 patients are shown in Table 3. Most patients (31 patients, 86%) underwent debridement and closure over drains. The mean interval from presentation to surgery was 27 days (range 0–156). Only one received postoperative irrigation, and four required open packing and planned reexploration. Nineteen (34%) of these patients developed major complications. Most common were persistent pancreatic or enteric fistulas (9% each) and endocrine or exocrine insufficiency (15%). One patient developed a deep venous thrombosis. Eight (23%) required reexploration; in four it was planned, and in the remainder it was required because of inadequate initial debridement.
Table 3. SURGICAL MANAGEMENT (n = 36)
Conservative Therapy
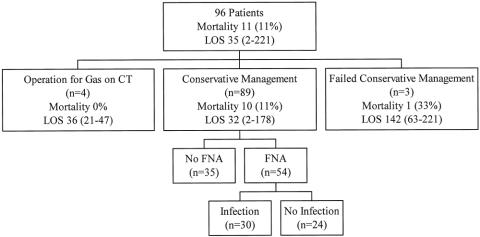
Figure 1 summarizes the management of the 96 patients for whom conservative therapy was a possibility, excluding the 3 who were initially made DNR. Four patients were found to have gas on CT, and all underwent surgery, with no deaths; none of these patients underwent FNA. Of the remaining 92 patients who were potential candidates for conservative management, 3 failed to meet the criteria for such therapy and underwent surgery in the absence of documented infection. Of the remaining 89, 35 were managed without aspiration and 54 underwent FNA. These FNAs were positive in 30 patients and negative in 24. Table 4 summarizes the success of conservative therapy in each of three groups: no FNA, FNA infection, and FNA sterile.
Figure 1. Management strategy in 96 patients with necrotizing pancreatitis. Length of stay (LOS) in days is represented as mean (range). CT, computed tomography; FNA, fine-needle aspiration.
Table 4. MANAGEMENT BASED ON FNA STATUS
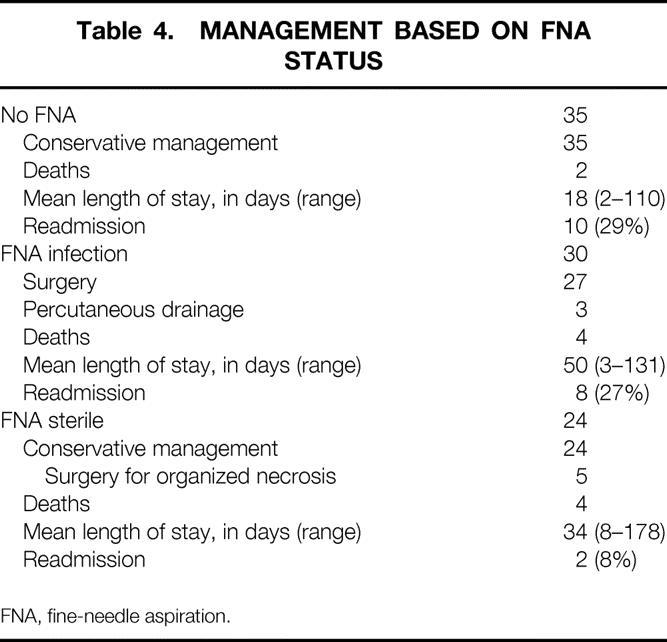
FNA, fine-needle aspiration.
Of the three patients who were exceptions to the conservative strategy, one was a woman in the first trimester of pregnancy who had reluctantly undergone a CT showing pancreatic necrosis. She subsequently developed increasing fever and leukocytosis and elected to proceed with surgery rather than undergo another radiographic study with pancreatic aspiration. The second patient, transferred from another institution, underwent exploration for an acute abdomen with suspected colonic necrosis shortly after admission and died after a prolonged postoperative course. The third exception was a patient with respiratory insufficiency who suddenly developed marked metabolic acidosis and underwent exploration based on concern that she had an intraabdominal catastrophe. Laparotomy failed to reveal anything other than pancreatitis. She underwent debridement and eventually recovered.
Thirty-five patients did not undergo FNA; they had a mean APACHE II score of 7 (range 0–22), and organ failure occurred in 12 (34%). There were two deaths in this group. One was a 49-year-old alcoholic who presented to the emergency room in cardiac arrest. Although he was resuscitated and underwent a CT showing pancreatic necrosis, he failed to recover neurologically and developed aspiration pneumonia. The second death was a patient transferred to our institution 2 days after presentation elsewhere with severe multiorgan failure including respiratory insufficiency, renal failure, and evidence of disseminated intravascular coagulation and rhabdomyolysis. He died within 72 hours. Neither of these two conservatively managed patients seems likely to have benefited from debridement. The remaining 33 patients in the no-FNA group were successfully managed with a mean hospital stay of 18 days and a readmission rate of 29%. None of these patients were thought to have enough evidence of infection to warrant FNA. Readmissions were for recurrent abdominal pain (six patients), fever (four patients), diarrhea (two patients), and nausea (two patients). None of these patients subsequently required operation.
The group of 30 patients with FNAs showing infection had a mean APACHE II score of 8 (range 1–17), and organ failure occurred in 17 (57%). They were managed by either surgery or percutaneous drainage. Each of the three patients successfully treated by percutaneous drainage had been found to have an infected fluid collection in the context of less than 30% necrosis and subsequently recovered uneventfully. In the 27 who underwent debridement, there were 4 deaths. One was a complicated postoperative patient who developed pancreatic necrosis in the setting of multiorgan failure after radical nephrectomy with removal of a caval-atrial tumor thrombus. In this patient, the timing of debridement was influenced more by the patient’s postoperative status than any strategy of management. Another patient suffered a cardiac arrest related to mucus plugging of his endotracheal tube the evening after debridement; although his general condition improved, he never recovered neurologically. There were two in this group who might have benefited from earlier intervention. One was a woman who developed severe adult respiratory distress syndrome within 24 hours of admission and required maximal ventilatory support. At approximately 2 weeks, she improved enough to tolerate transport to CT, where pancreatic aspiration showed infection. She underwent debridement but died shortly after leaving the operating room. The other patient underwent debridement 7 days after presentation and initially did well. However, 1 week after surgery, she developed pneumonia complicated by progressive pulmonary insufficiency.
The group of 24 patients with sterile FNAs had a mean APACHE II score of 7 (range 0–14), and organ failure occurred in 11 (46%). Four of these patients died. One was a woman who had previously undergone bone marrow transplant, had chronic graft-versus-host disease, and was dialysis-dependent. Despite a negative FNA, she became increasingly ill and care was withdrawn. Another developed multiorgan failure after emergent coronary artery bypass grafting. His NP did not develop until several weeks after surgery, when his chances for survival were already compromised. There were two patients in this group who might have been candidates for debridement based on the severity of their illness. One was a 74-year-old patient with diabetes and peripheral vascular disease who died at 2 weeks after presentation with multiorgan failure. The other was transferred from an outside hospital 1 week after presentation with multiorgan failure on hemodialysis. He died 5 days after admission with a negative FNA.
Surgery for Organized Necrosis
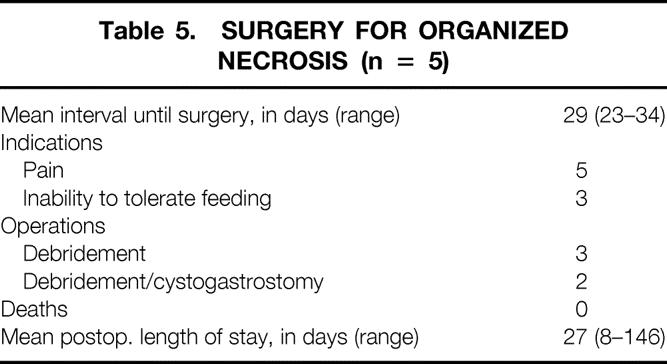
Table 5 summarizes the indications and outcome in five patients who underwent surgery for organized necrosis. Surgery was performed a mean of 29 (range 23–34) days after presentation, and each of these patients had previously undergone at least one negative FNA. Indications were primarily persistent pain and inability to tolerate oral feeding. All patients underwent debridement; in two, the inflammatory process was sufficiently mature that cystogastrostomy was added to the debridement. All these patients recovered after the procedures and were discharged a mean of 27 (range 8–146) days after surgery. There may have been other patients who underwent surgery for organized necrosis during this interval; however, none had a CT showing necrosis at our institution.
Table 5. SURGERY FOR ORGANIZED NECROSIS (n = 5)
DISCUSSION
This retrospective review is unique in several respects. It represents one of the largest single-institution series of patients in the literature managed with a conservative bias. In contrast to most recent analyses, which have focused on the results in select patients referred to surgical centers, this study evaluates the entire spectrum of patients referred to our institution with this disease. Finally, it is the only American series in which conservative approaches were applied so consistently in management.
It was not entirely clear that the patients identified in our institutional review would be comparable to those studied by the more select referral services in the literature. It seems likely that such studies might be biased by patterns of referral. For example, surgical centers might receive only the patients with the most severe disease who could not be managed elsewhere. Alternatively, patients with underlying chronic medical problems might not be considered candidates for surgical management, or patients with the most severe disease might be too unstable for transfer. In fact, a comparison of at least some of our patient characteristics and indices of severity with those of several recent series 2,5–9 suggests that at we are in fact studying patients with very similar pancreatic disease. Because few of these studies, including our own, stratify based on underlying medical conditions, this parameter is impossible to compare. Our analysis, reflected in the previous discussion of patient deaths, would suggest that, if anything, this institutional review included several chronically debilitated patients who might not have been considered for referral to a surgical service. However, there was a significant group (35 patients) whose signs and symptoms of potential infection were not thought to be severe enough to warrant FNA. Although the initial APACHE II scores and the incidence of organ failure in this group were not all that different from those in the group who had sterile FNAs, these patients generally improved from the time of presentation. Although FNA has usually been advocated only in patients suspected of having infection, we were surprised that this group was so large. However, even in the recent prospective evaluation of conservative management from the Bern group, 6 using strict criteria of suspected infection for FNA, 42 of 86 patients with NP were managed conservatively without aspiration. In our series, these patients recovered relatively rapidly and were seldom readmitted. This group, which represents a significant percentage of all patients with NP, has been largely ignored in many retrospective series addressing the benefits of surgery in sterile pancreatic necrosis. Although its recognition should not in any way diminish the need for continuing vigilance regarding infection, its existence represents another argument in favor of conservative strategies.
Despite recent studies suggesting that prophylactic antibiotics may reduce the incidence of infection in NP, 11 we did not identify any consistent approach to this at our institution, although 78% of patients did receive some form of prophylaxis. Although many have favored quinolones such as imipenem because of their broad spectrum and excellent penetration into the pancreas, 12 triple-antibiotic therapy was most commonly used in our series. This probably reflects our concerns about the relatively high incidence of fungal superinfection in recent studies using imipenem; for example, in the Bern series, where all patients received imipenem and cilastatin, 6 29% of infections involved Candida albicans. It seems conceivable that a more consistent approach to prophylaxis might have reduced our overall incidence of infected necrosis; however, if anything, such an effect would have strengthened the argument for conservative management.
Even in the context of our reservations about differences in patient selection, the outcomes from our study compare favorably with those in the literature. In the 96 patients who were considered candidates for further therapy, the death rate was only 11% and was not significantly different (13%) in the 36 patients treated surgically. In the group treated without surgery, 10% died. Historically, the literature would suggest a death rate for NP in the range of 20% to 40%, 1 although surgical series from the past decade have improved significantly on these results. 2,5–9,13,14 In fact, two recent studies, one including only surgical patients 8 and the other from Bern studying conservative management in a prospective trial, 6 reported death rates of 6.2% and 10%, respectively. It seems unlikely, given the relatively small numbers of total deaths in any of these series, that these differences are significant.
Although techniques of debridement and postoperative management (closed drainage, irrigation, open packing) have been the subject of considerable debate in the literature, 8–10,13,14 most have concluded that each method has a role in specific patients. We have found that most patients can be treated by debridement and simple closed drainage, although a few require open packing. It may be that the conservative strategy, by delaying surgical intervention beyond the period of ongoing necrosis, favored such an approach; the time from presentation to surgery was 27 days (range 0–156). Several nonrandomized series have shown significantly better outcomes in patients undergoing late versus early debridement, 8,15 and most surgeons would agree that surgery is considerably facilitated by the demarcation of nonviable tissue that occurs as necrosis become organized.
The results of our analysis of surgical death and complication rates do not suggest major differences from other series; in fact, the 23% rate of reoperation is comparable to that reported by others. 8,10,16 Although surgical expertise certainly makes some difference in this disease, it is our impression that patient selection, the timing of surgery, and the quality of perioperative care play just as great a role. We might anticipate higher death and complication rates for surgical patients in a conservatively managed series compared with studies in which patients are more frequently treated by surgery; the better-risk, less-ill patients would be expected to increase the denominator at the more aggressive institutions. These considerations probably have some impact on comparisons between series and make the issue of debridement versus conservative therapy for sterile necrosis even more difficult to evaluate.
The tenor of discussions regarding this controversy seems to have relaxed considerably with time. In 1991, when Bradley and Allen 5 published their original series reporting 11 patients with sterile necrosis treated successfully without surgery, the concept was greeted with resistance. For example, Rattner et al 17 shortly thereafter reported a series suggesting that early debridement is beneficial irrespective of the status of infection. As experience with FNA and conservative therapy accumulated, 18 clinicians became increasingly comfortable with the concept of conservative management in the stable patient, although surgical intervention was still contemplated in the absence of documented infection in critically ill patients or in the face of deterioration. 19 Efforts were made to establish criteria other than infection that might identify patients who would benefit from debridement. Computed tomography evidence of necrosis of more than 50% of the pancreas has received the most attention 7 but has not been shown to be sufficiently specific to use as a basis for decision making. 20 Although series advocating a more aggressive approach continue to be reported, 8,9 it is our impression that most centers have adopted an increasingly conservative posture. However, there have been relatively few large studies analyzing the results of such an approach. The recent study from the Bern group 6 represents the major exception to this generalization. Studying 86 patients with NP prospectively using a strict conservative protocol, they reported a death rate of 10%, with just a single patient undergoing surgery in the absence of documented infection.
Although the Bern study is convincing, the conclusions from such a prospective series from a referral service are not always readily generalizable to the usual practice setting. At Brigham and Women’s Hospital, we have had a specific interest in conservative techniques of management and previously reported our results in patients undergoing CT-guided FNA. 20 However, we had not analyzed the effects of this bias on management and outcomes across our entire institutional experience with this disease. To this end, we conducted this retrospective review and can draw several new conclusions.
First, these results suggest that even in the absence of a strict prospective protocol, conservative strategies can be applied successfully in most patients with NP with reasonable outcomes. However, there were exceptions to this approach. Although the operation in the pregnant patient without documented infection might be debated, an acute abdomen and severe acidosis are clearly indications for surgery that should supersede any general management strategy. Undoubtedly, other exceptions will be identified, and we believe that flexibility is mandatory in the clinical application of this approach.
Second, analyzing the patients who died, it is difficult to identify patients who might benefit from a more aggressive strategy. Although we believe that a randomized trial may be the only way to resolve this controversy completely, 21 the small number of patients in this category, at least if death is used as the major parameter, may preclude any definitive conclusions even if such a study were designed in a multicenter fashion. Although other measures such as complication rates, length of hospital stay, readmission rates, and quality of life indices may be altered by surgical intervention, few would argue that operations for these indications should be performed early in the course of NP.
Finally, in this context, we would suggest that such delayed operations should be considered a success, not a failure, of the conservative strategy. The conservative approach does produce a group of patients with sterile necrosis who suffer from what Warshaw 22 has described as “persistent unwellness.” They have continuing pain, malaise, or inability to tolerate a diet. These patients have what we have defined as organized necrosis, which we would suggest is a different pathologic process than acute necrosis, accompanied by maturation and demarcation of the inflammatory process. In our experience, these patients were confined to the group who had previously undergone a negative FNA and, in fact, accounted for a significant percentage (21%) of that group. We believe that surgery in these patients is considerably facilitated by the maturation process, and we found that they consistently did well after surgery. The most appropriate timing for surgery in this group is not defined by our study, and there may have been patients who would have benefited from earlier surgery in this group. Fernandez-del Castillo et al 8 have suggested that there is no added benefit from delaying more than 4 weeks, approximately the same interval applied in our five patients who underwent surgery for organized necrosis (range 23–34 days). We believe that the indications and timing for surgery in this group deserve further study.
Discussion
Dr. Andrew L. Warshaw (Boston, Massachusetts): Dr. Ashley, I congratulate you and your group at the Brigham & Women’s Hospital in your management of a very difficult group of patients. Your colleague Dr. Banks has been a pioneer in this area especially as one of the original investigators of fine needle aspiration for detecting infection.
It is now widely accepted that non-interventional management will suffice in most instances of necrotizing pancreatitis. So there is no argument with your basic thesis. The mortality for acute necrotizing pancreatitis is now universally below 15% and as low as 6% in specialized centers. Yours was right in this group with 14%. But I would challenge you in the same vein that you have challenged yourself that this isn’t good enough. We are still searching for improved strategies, whether pharmacologic or interventional, that will refine the indications for operation and improve the outcomes.
It is agreed that infection is an absolute indication for debridement and drainage. But sepsis may closely mimic the SIRS which can occur in sterile conditions; so FNA may become critical to defining the circumstances.
I suggest, however, that your analysis needs to be revised on an intention-to-treat basis, rather than the findings of the FNA, because only 57% of the ultimately proven infection was proven on the first FNA pass. In 23% of your cases it took two tries, and in 20% it took three or more FNAs to prove or detect infection. Does that mean that there were so many false negative FNAs? Or that infection develops over time and only present by the time of the third or fourth FNA? What are the strategic implications for treating necrotizing pancreatitis if the proof of infection is so uncertain or mutable?
35% of your patients had no FNA ever done, presumably because of a clinical judgment that they didn’t need one. This group of patients was clearly less sick in general because they had an 18-day average length of stay compared with 34 days for patients who were chosen for FNA. But two of these patients who did not get an FNA died with infection. What are your criteria for FNA, for repeat aspiration, and at what intervals?
It is widely promulgated that the extent of necrosis is a principal risk factor for complications, including and perhaps especially infection. One-third of your patients had minor necrosis, less than 30%, one-third had 30 to 50% of necrosis, and one-third greater than 50%. Different from many other reports, you found no correlation between extent of necrosis and infection, Apache score, organ failure, need for operative intervention, or ultimately death. This needs to be emphasized and explained.
Organ failure was nonetheless the principal pathway to death, whether in infected or sterile necrosis. 44 out of your 96 patients developed organ failure, 25 of them multi-organ failure, including patients with sterile necrosis, 4 out of 24 of those patients, or 16% of your series, had apparently sterile necrosis by FNA findings but died.
How can we better anticipate organ failure, perhaps at its incipience, when patients without the extraordinary comorbidities of your patients may be more salvageable?
What about other indices of high risk or doom such as obesity? Is there hope for a serum test, an index cytokine, trypsinogen activation peptide, circulating active trypsin, PLA-2, or some other marker which might give us a handle on early intervention? Dr. Banks has noted that a hematocrit over 46 is a major predictor for necrosis. Does that also correlate with ultimate organ failure?
Finally, I am concerned about your new term ‘organized necrosis.’ Most necrosis becomes organized over time, certainly in the weeks to months that healing requires. But the majority of these patients, as you would certainly agree, are not greatly symptomatic. You have used pain and inability to eat at three weeks as your reasons to operate for organized necrosis. It is therefore symptoms, not the radiographic findings of necrosis that determine the need for operation. We have preferred the concept of ‘persistent unwellness’ to describe the set of circumstances which justify surgical debridement of sterile necrosis. Your series includes a patient operated on at 164 days. We have one who was eventually debrided at 300 days. How much is too much observation time for an unwell but not acutely ill patient?
Presenter Dr. Stanley W. Ashley (Boston, Massachusetts): Thank you for your comments, Dr. Warshaw. I do want to acknowledge first that we, and virtually everyone else that cares for patients with this disease, are enviable of the results that you and your colleagues have reported from the Massachusetts General Hospital. I believe that your most recent series of surgically treated patients had a mortality of 6%, whether they were infected or not. Clearly, our mortality for the surgically treated patients was higher but I would suggest that our numbers are comparable to those in virtually every other surgical series. I can only speculate that some of this difference might be because we only operated on the most ill patients whereas, with your more liberal indications for operation, there may have been a less sick group that increased the denominator. I think that one of the problems with evaluating the literature on this subject is that it is very difficult to compare series. In our review, we did include the entire spectrum of patients treated with necrotizing pancreatitis over this time interval and some of these patients were never referred for surgical consideration. This is in contrast to many series in the literature.
With respect to your question about the initially negative FNAs that became positive, I don’t think we really know whether those patients were infected to begin with and we just missed it or they became infected over time. In the studies that have tried to evaluate the accuracy of FNA, the data suggest that its accuracy is greater than 95% but this is for a single aspirate. I would suggest that, whether or not it is positive the first time, it remains the best marker for infection and the need for operation that we have. One might even argue that an initially negative FNA, even if it eventually becomes positive, is of benefit by extending the interval to operation, permitting more organization of the necrosis.
With regard to our indications for FNA, this was a retrospective review and no strict criteria were applied. In the 35 that were not aspirated, although many of them were very ill at the time of admission, all improved with time and it was not felt that they needed FNA. In general terms, we have used persistent fever, leukocytosis, worsening organ failure or systemic inflammatory response syndrome as the criteria for FNA. The Bern group has described very specific numbers for temperature and white count. We would usually obtain the first FNA within 3 to 4 days of admission.
In response to your question regarding other markers that might be used as an indication for intervention, neither extent of necrosis nor infection correlated with mortality. I think that you had the same results with regard to infection in your series – with intervention in the infected patients, the excess mortality is eliminated. Extent of necrosis has been used by others but, in our series, there were about equal numbers in the groups with less than 30, 30-50, and greater than 50% necrosis with no correlation with the development of infection or ultimately with mortality. The Apache II scores, calculated at admission not their maximum which was difficult to determine because so many of these patients were transferred from other hospitals, and organ failure both correlate with mortality but I don’t believe that either index is predictive enough to use as an indication for operation. With respect to biochemical markers, I do not think that we have anything that can be used to predict which patients might eventually need operation.
In conclusion, we would suggest that there really is a very small group of patients in whom the issue of early operation without documented infection even arises. Peter Banks at our institution, I think, would now say that, in the absence of documented infection, he would not refer anyone for operation. I guess that, as a surgeon frustrated by not being able to fix a problem, I could pick a scenario where I would have a hard time not intervening – for example, a young, otherwise healthy patient who is probably going to die tonight. I might offer the family the option of taking that patient to the operating room with the proviso that I probably was only going to speed that patient’s demise. The main message of our paper is that the need to make such a decision almost never arises.
Dr. Michael G. Sarr (Rochester, Minnesota): I think we need to acknowledge that there is an up-front bias in your study for conservative management, and the real question remains: Would anyone with sterile necrosis have benefited by operative debridement early on – that is, to decrease the duration of hospitalization, the late readmission, the quality of life, et cetera. This question really is not answered by your study. So I have three short questions.
First, readmissions in the conservatively managed treatment group are undefined. Would these patients have benefited by early debridement?
Second, why were most patients in this current era treated with triple antibiotics and not with imipenem? The use of imipenem might very well have decreased the incidence of an infected necrosis and made you look even better.
Third, several groups have suggested that an increasing Apache II score in spite of conservative management selects out a higher risk group. You have reported to us only the Apache II scores at the time of admission. Do you have any data on changes in the Apache II score during the course of conservative therapy?
Dr. Stanley W. Ashley: Thank you, Dr. Sarr. With regard to the readmissions, I think there were a total of 20. Eight were in the group that underwent operation or percutaneous drainage as an early maneuver. Two were patients that had undergone surgery for organized necrosis. All of the remaining 10 were in the group that did not undergo FNA. We discharged those patients at a mean of 18 days after admission, which was probably, at least in some of these patients, too early. All these patients recovered and got over the cause for readmission.
With regard to the antibiotics, about 80% of these patients got some form of prophylactic antibiotic. The greatest number received triple antibiotic coverage followed by imipenem and ceftazidime. It has been our concern that imipenem may selective produce colonization with Candida, and we have in many patients therefore stayed away from that agent. We have also tried to avoid prophylactic antibiotics for more than two weeks to prevent superinfection.
The mean Apache II at admission – we calculated this based on the Brigham & Women’s Hospital data and admission data from transferring institutions – was 7. For the Brigham patients, this increased with time but we couldn’t really get an accurate number for that for the transfers. Organ failure correlates better with outcome, although as I suggested we do not feel that this can be used as a basis for operation.
DR. JOHN M. HOWARD (Toledo, Ohio): I personally do not accept pancreatic necrosis as being defined by perfusion studies as seen on the CT scan. In our hands, follow up with ERCP a year later on these patients, we characteristically have found a normal pancreatic duct. I interpreted this to reflect a normal pancreas, as anatomically defined.
Based on a personal study of 76 patients treated by repetitive open operations, often with necrotic tissue being weighed, my mortality rate was 2.5%. It is important under those circumstances that the same surgeon carry out each repetitive operation. This results in ethical problems when the patient is ill over a period of weeks.
I would like to ask you, do you think this necrotizing process is a pancreatic enzyme-digestive process or do you think it is an ischemic process? The latter may be important, as it would suggest a window of therapeutic opportunity in which we might prevent the necrosis. That would be a major contribution.
Dr. Stanley W. Ashley: Thank you, Dr. Howard. Your contributions in this area have been enormous. I do think there is a component of this disease that is ischemic – microvascular stasis and hypoperfusion related to inflammatory mediators. Whether we will ever be able to devise a way to intervene early enough to prevent such problems is open to speculation.
Footnotes
Presented at the 121st Annual Meeting of the American Surgical Association, April 26–28, 2001, the Broadmoor Hotel, Colorado Springs, Colorado.
Correspondence: Stanley W. Ashley, MD, Department of Surgery, Brigham and Women’s Hospital, 75 Francis St., Boston, MA 02115.
E-mail: sashley@partners.org
Accepted for publication April 26, 2001.
References
- 1.Banks PA. Acute pancreatitis: medical and surgical management. Am J Gastroenterol 1994; 89 (suppl): S78–S85. [PubMed] [Google Scholar]
- 2.Isenmann R, Rau B, Beger HG. Bacterial infection and extent of necrosis are determinants of organ failure in patients with acute necrotizing pancreatitis. Br J Surg 1999; 86: 1020–1024. [DOI] [PubMed] [Google Scholar]
- 3.London NJM, Neoptolemos JP, Lavelle J, et al. Serial computed tomography scanning in acute pancreatitis: a prospective study. Gut 1989; 30: 397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerzof SG, Banks PA, Robbins AH, et al. Early diagnosis of pancreatic infection by computed tomography-guided aspiration. Gastroenterology 1987; 93: 1315–1320. [DOI] [PubMed] [Google Scholar]
- 5.Bradley EL, Allen K. A prospective longitudinal study of observation versus surgical intervention in the management of necrotizing pancreatitis. Am J Surg 1991; 161: 19–25. [DOI] [PubMed] [Google Scholar]
- 6.Buchler MW, Gloor B, Muller CA, et al. Acute necrotizing pancreatitis: Treatment strategy according to the status of infection. Ann Surg 2000; 232: 619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rau B, Pralle U, Uhl W, et al. Management of sterile necrosis in instances of severe acute pancreatitis. J Am Coll Surg 1995; 181: 279–288. [PubMed] [Google Scholar]
- 8.Fernandez-del Castillo C, Rattner DW, Makary MA, et al. Debridement and closed packing for the treatment of necrotizing pancreatitis. Ann Surg 1998; 228: 676–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Branum G, Galloway J, Hirchowitz W, et al. Pancreatic necrosis: results of necrosectomy, packing, and ultimate closure over drains. Ann Surg 1998; 227: 870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beger HG. Surgical management of necrotizing pancreatitis. Surg Clin North Am 1989; 69: 529–549. [DOI] [PubMed] [Google Scholar]
- 11.Pederzoli P, Bassi C, Vesentini S, et al. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surg Gynecol Obstet 1993; 176: 480–483. [PubMed] [Google Scholar]
- 12.Buchler M, Malfertheiner P, Freiss H, et al. Human pancreatic tissue concentration of bactericidal antibiotics. Gastroenterology 1992; 103: 1513–1517. [DOI] [PubMed] [Google Scholar]
- 13.Sarr MG, Nagorney DM, Mucha P Jr, et al. Acute necrotizing pancreatitis: management by planned, staged pancreatic necrosectomy/debridement and delayed primary wound closure over drains. Br J Surg 1991; 78: 576–581. [DOI] [PubMed] [Google Scholar]
- 14.Beger HG. Operative management of necrotizing pancreatitis: necrosectomy and continuous closed postoperative lavage of the lesser sac. Hepato-Gastroenterology 1991; 38: 129–133. [PubMed] [Google Scholar]
- 15.Mier J, Luque-de Leon E, Castillo A, et al. Early versus late necrosectomy in severe necrotizing pancreatitis. Am J Surg 1997; 173: 71–75. [DOI] [PubMed] [Google Scholar]
- 16.Pederzoli P, Bassi C, Vesentini S, et al. Necrosectomy by lavage in the surgical treatment of severe necrotizing pancreatitis. Acta Chir Scand 1990; 156: 775–780. [PubMed] [Google Scholar]
- 17.Rattner DW, Legermate DA, Lee MJ, et al. Early surgical debridement of symptomatic pancreatic necrosis is beneficial irrespective of infection. Am J Surg 1992; 163: 105–109. [DOI] [PubMed] [Google Scholar]
- 18.Banks PA, Gerzof SG, Langevin RE, et al. CT-guided aspiration of suspected pancreatic infection. Bacteriology and clinical outcome. Int J Pancreatol 1995; 18: 265–270. [DOI] [PubMed] [Google Scholar]
- 19.McFadden DW, Reber HA. Indications for surgery in severe acute pancreatitis. Int J Pancreatol 1994; 15: 83–90. [DOI] [PubMed] [Google Scholar]
- 20.Tenner S, Sica G, Hughes, M, et al. Relationship of necrosis to organ failure in severe acute pancreatitis. Gastroenterology 1997; 113: 899–903. [DOI] [PubMed] [Google Scholar]
- 21.Ashley SW. Editorial. Operation for sterile pancreatic necrosis: an evolving strategy. J Am Coll Surg 1995; 181: 363–364. [PubMed] [Google Scholar]
- 22.Warshaw AL. Editorial. Pancreatic necrosis: to debride or not to debride, that is the question. Ann Surg 2000; 232: 627–629. [DOI] [PMC free article] [PubMed] [Google Scholar]