Abstract
Objective
To test the hypothesis that early and low doses of erythromycin reduce the incidence of early delayed gastric emptying (DGE) and induce phase 3 of the migratory motor complex in the stomach after Billroth I pylorus-preserving pancreaticoduodenectomy (PPPD).
Summary Background Data
Delayed gastric emptying is a leading cause of complications after PPPD, occurring in up to 50% of patients. High doses of erythromycin (200 mg) accelerate gastric emptying after pancreaticoduodenectomy and reduce the incidence of DGE, although they induce strong contractions that do not migrate to the duodenum.
Methods
Thirty-one patients were randomly assigned to either the erythromycin or control groups. The patients received erythromycin lactobionate (1 mg/kg) every 8 hours, or H2-receptor antagonists and gastrokinetic drugs from days 1 to 14 after surgery. On postoperative day 30, gastroduodenal motility was recorded in 14 patients.
Results
Preoperative, intraoperative, and postoperative factors were comparable in the erythromycin and control groups. The erythromycin group had a shorter duration of nasogastric drainage, earlier resumption of eating, and a 75% reduction in the incidence of DGE. Erythromycin was an independent influence on nasogastric tube removal, and preservation of the right gastric vessels was a significant covariate. Low doses of erythromycin induced phase 3 of the migratory motor complex and phase 3-like activity, with the same characteristics as spontaneous phase 3, in 86% of patients: two had quiescent stomachs and the others had spontaneous phase 3 or phase 3-like activity.
Conclusions
Low doses of erythromycin reduced the incidence of DGE by 75% and induced phase 3 of the migratory motor complex after Billroth I PPPD. Low doses of erythromycin are preferable to high doses in the unfed period after PPPD.
Pylorus-preserving pancreaticoduodenectomy (PPPD) has become accepted as a safe, appropriate operation in selected patients with malignant and benign disease of the pancreas and periampullary region. 1 Delayed gastric emptying (DGE) is a leading cause of complications after PPPD, occurring in up to 50% of patients. 2,3 The pathogenesis of DGE is thought to be gastric atony in response to resection of the duodenal pacemaker 4 or reduction in circulating motilin levels. 5 Erythromycin and related 14-member macrolide compounds act as motilin agonists by binding to motilin receptors and initiating phase 3 activity of the interdigestive migratory motor complex (MMC). 6,7 A prospective, randomized, placebo-controlled, double-blind study showed that erythromycin significantly accelerates gastric emptying after pancreaticoduodenectomy and reduces the incidence of DGE. 8 In this study, patients were given high doses (200 mg) of erythromycin every 6 hours from days 3 to 10 after surgery. Studies in unfed normal patients have shown that high doses of erythromycin (200–300 mg) induce strong, prolonged bursts of antral contraction, which are not propagated to the small bowel. 9 Low doses of erythromycin (40 mg) induce a premature phase 3, commencing in the stomach and migrating through the small intestine; this has the same characteristics as spontaneously occurring phase 3. 9 This suggests that low doses of erythromycin are preferable to high doses once eating recommences after surgery. The effect of low doses of erythromycin on patients after pancreaticoduodenectomy is unknown. This study tested the hypothesis that early and low doses of erythromycin reduce the incidence of early DGE and induce phase 3 in the stomach after PPPD.
PATIENTS AND METHODS
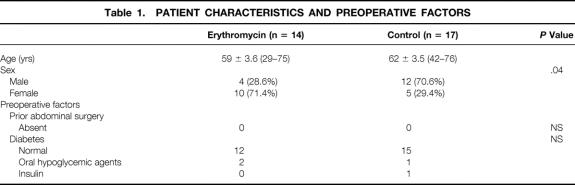
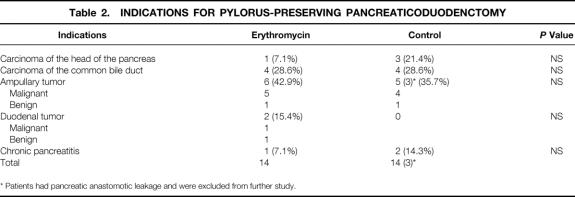
From April 1997 to March 2000, 31 patients underwent PPPD with a Billroth I-like reconstruction and were randomly assigned to either the erythromycin or the control group. The patients ranged in age from 29 to 76 years; the mean age was 59 ± 3.6 years in the erythromycin group and 62 ± 3.5 years (range 42–76) in the control group. Fifteen patients were women (55%) and 16 were men (45%). There were more women and fewer men in the erythromycin group compared with the control group. Preoperative factors associated with gastric emptying problems were comparable between the two groups (Table 1). Indications for PPPD were periampullary tumor (n = 14), bile duct carcinoma (n = 8), pancreatic duct carcinoma (n = 4), duodenal tumor (n = 2), and chronic pancreatitis (n = 3). Disease was malignant in 28 patients and benign in 3. No significant differences were observed between the two groups (Table 2). Three patients in the control group were excluded from further analysis because they developed pancreatic anastomotic leakage, which is one of the pathogenic factors of DGE. 10 Appropriate written informed consent was obtained from each patient.
Table 1. PATIENT CHARACTERISTICS AND PREOPERATIVE FACTORS
Table 2. INDICATIONS FOR PYLORUS-PRESERVING PANCREATICODUODENCTOMY
* Patients had pancreatic anastomotic leakage and were excluded from further study.
Surgical Procedures
Extended dissection of the regional, hepatoduodenal, and paraaortic lymph nodes and surrounding connective and nerve tissues was performed for patients with malignant tumor; in the standard dissection, dissection of the paraaortic lymph nodes and surrounding connective and nerve tissues was omitted. The right gastric vessels were skeletonized and conserved, which resulted in dissection of the vagal pyloric branch. Pylorus-preserving pancreaticoduodenectomy was performed as pancreas head resection with pylorus-preserving duodenectomy. We made a Billroth I-type reconstruction, which has a normal anatomic arrangement. This entailed duodenoduodenostomy or duodenojejunostomy followed by pancreaticojejunostomy and biliary anastomosis. 11 Stent tubes were placed in both the biliary and pancreatic anastomoses and brought out through a hepaticojejunostomy, the liver, and skin. A tube gastrostomy was not created in any patient.
Erythromycin
In the erythromycin group, intravenous administration of erythromycin lactobionate (1 mg/kg) in 50 mL of 0.9% saline, given over 15 minutes through a central venous route every 8 hours, started on postoperative day 1 and continued to postoperative day 14. H2-receptor antagonists and metoclopramide hydrochloride as a gastrokinetic drug were avoided in the erythromycin group but were used in the control group.
Data Collection
Cephamycins or cepharosporins were used prophylactically for 3 consecutive days before and after surgery. Intravenous hyperalimentation was administered after surgery until the patients could eat satisfactorily. The nasogastric tube was removed when the daily drainage volume was less than 200 mL on 2 consecutive days. An oral diet was resumed 2 or 3 days after nasogastric tube removal. Delayed gastric emptying was defined according to the criteria of Yeo et al 8 as a nasogastric tube left in place for 10 or more days, emesis after nasogastric tube removal, reinsertion of nasogastric tube, postoperative use of prokinetic agents after postoperative day 10, or failure to progress with diet.
Manometric Recording
After a 16-hour fast, a catheter containing three microtransducers was transnasally introduced into the stomach and connected to a Microdigitrapper portable data-logger (Synectics Medical, Stockholm, Sweden). The use of H2-receptor antagonists and gastrokinetic drugs was avoided for 1 day before recording. Erythromycin lactobionate (1 mg/kg) in 50 mL of 0.9% saline was intravenously infused over 15 minutes at 10 pm. Motility was analyzed using a computer with manual aid, and the frequency, duration, amplitude, and motor index of phase 3 were evaluated.
Statistical Analysis
Data are presented as the mean ± standard error of the mean. Statistical analysis was performed using the program StatView J-5.0 (Abacus Concepts, Inc, Berkeley, CA). The chi-square, Fisher exact, and Mann-Whitney tests were used for clinical data. A parametric Student t test was used for paired gastric motility data. The Kaplan-Meier method was used to estimate nasogastric tube removal day, and the Breslow-Gehan and log-rank tests were used to determine statistical significance. A Cox proportional hazard model was used to assess the risk ratio under simultaneous contributions from several covariates. P < .05 was considered statistically significant.
RESULTS
Patient Characteristics
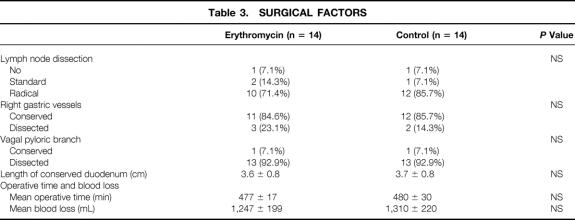
The right gastric artery was skeletonized and preserved in 85% of patients. The vagal pyloric branch was conserved in one patient in each group. Intraoperative factors were comparable in the erythromycin and control groups (Table 3). Three patients in the control group developed pancreatic anastomotic leakage and their nasogastric tube drainage was postoperative day 13, 13, and 36. There were no other complications in either group, including bilioenteric anastomotic leakage, wound infection, cholangitis, or upper gastrointestinal bleeding. There were no postoperative deaths in the hospital or within 30 days of discharge.
Table 3. SURGICAL FACTORS
Clinical Gastric Emptying
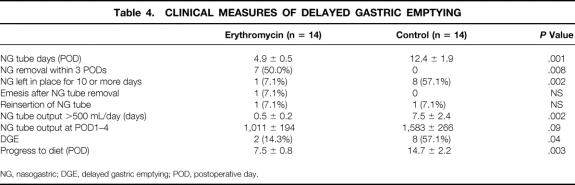
Patients receiving erythromycin had a shorter duration of nasogastric tube drainage (postoperative day 4.9 ± 0.5 vs. 12.4 ± 1.9), and in 50% of the patients the nasogastric tube was removed by postoperative day 3 (Table 4). In contrast, the nasogastric tube was left in place for 10 or more days in more patients in the control group (one vs. eight). Patients receiving erythromycin resumed eating earlier (postoperative day 7.5 ± 0.8 vs. 14.7 ± 2.2). The number of days with high-volume (>500 mL) nasogastric tube drainage was significantly less in the erythromycin group, although total drainage over 4 postoperative days was not significant (1,011 ± 194 vs. 1,583 ± 266 mL). The number of patients who had a nasogastric tube reinserted and had emesis after nasogastric tube removal was similar in both groups. The incidence of DGE was 14.3% in the erythromycin group and 57.1% in the control group (P = .04), indicating a 75% reduction in the incidence of DGE with erythromycin administration.
Table 4. CLINICAL MEASURES OF DELAYED GASTRIC EMPTYING
NG, nasogastric; DGE, delayed gastric emptying; POD, postoperative day.
Nasogastric Tube Removal and its Prognostic Factors
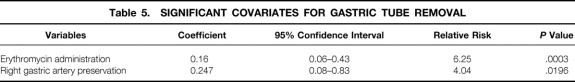
Univariate analysis revealed significantly earlier nasogastric tube removal with erythromycin administration (Breslow-Gehan test, P = .002; log-rank test, P = .004) (Fig. 1). Tube removal in 50% of patients was significantly earlier in the erythromycin group than in the control group (4.0 ± 0.8 vs. 12.0 ± 4.7 days). Multivariate analysis using a Cox proportional hazard model showed that administration of erythromycin exerted an independent influence (P = .011) on tube removal. Length of the preserved duodenum (P = .44), preservation of the right gastric artery (P = .16), preservation of the vagal pyloric branch (P = .16), the presence of diabetes (P = .64), and age (P = .72) were not significant covariates. However, a stepwise multiple regression analysis using a Cox proportional hazard model indicated that erythromycin administration and preservation of the right gastric artery were significant covariates (relative risk, 6.3-fold [P < .001] and 4-fold [P = .019], respectively) (Table 5). Groups of patients with different combinations of erythromycin and preservation of the right gastric artery showed relevant differences in tube removal. Patients who did not receive erythromycin and who underwent right gastric artery dissection had the longest period before tube removal (P < .001) (Fig. 2)
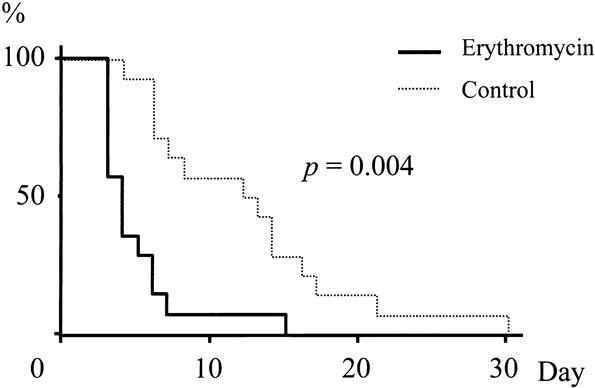
Figure 1. Nasogastric tube removal probability according to the Kaplan-Meier method. Univariate analysis revealed a significantly earlier nasogastric tube removal day for erythromycin administration (Breslow-Gehan test, P = .002; log-rank test, P = .004). Nasogastric tube removal for 50% of patients was significantly earlier in the erythromycin group than in the control group (4.0 ± 0.8 vs. 12.0 ± 4.7 days).
Table 5. SIGNIFICANT COVARIATES FOR GASTRIC TUBE REMOVAL
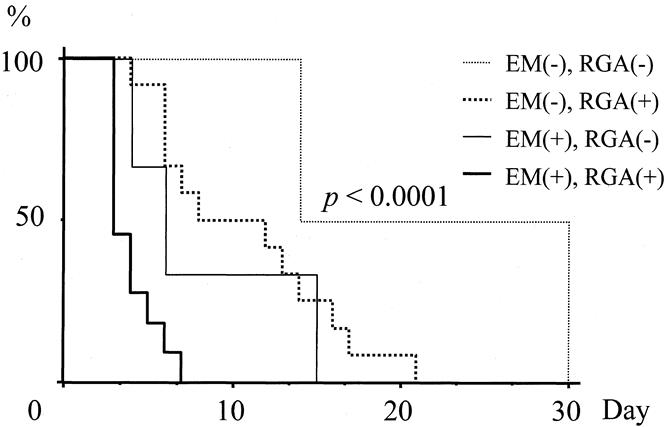
Figure 2. Nasogastric tube removal probability in various subgroups with different combinations. Patients who did not receive erythromycin (EM (-)) and underwent right gastric artery dissection (RGA (-)) had the greatest number of days until nasogastric tube removal (P < .001). EM (+), erythromycin administration; RGA (+), preservation of right gastric artery.
Gastric Motility Index
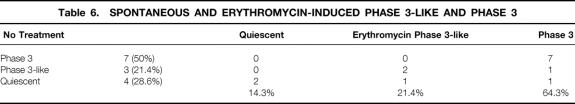
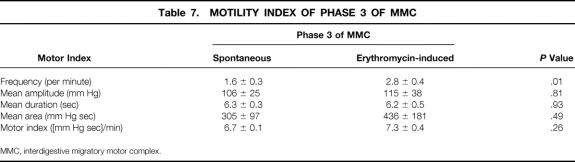
Gastrointestinal motility was recorded in 14 patients (erythromycin group, 13; control group, 1) on day 30 after surgery. Gastric motility was completely quiescent in 4 of the 14 (28.6%). Spontaneous phase 3-like contractions, which did not migrate to the duodenum, were observed in three patients (21.4%), and spontaneous phase 3 activity of the MMC was seen in seven patients (50%). Erythromycin induced phase 3-like contractions and phase 3 of the MMC in one of the four patients with a quiescent stomach and phase 3 in one and phase 3-like activity in two of the three patients with spontaneous phase 3-like contractions. Further, erythromycin induced phase 3 in all patients with spontaneous phase 3 contractions (Table 6). Low-dose erythromycin induced phase 3 of the MMC in 64.3% of patients and phase 3-like contractions in 21.4%. The injection of erythromycin significantly increased the frequency (2.8 ± 0.4/min) of phase 3 compared with the patients with spontaneous contractions (1.6 ± 0.3/min). In contrast, the mean amplitude (106 ± 25 vs. 115 ± 38 mm Hg), mean duration (6.3 ± 0.3 vs. 6.2 ± 0.5 seconds), mean area (305 ± 97 vs. 436 ± 181 mm Hg sec), and gastric motility index (6.7 ± 0.1 vs. 7.3 ± 0.4 [mm Hg sec]/min) were similar in the spontaneous and erythromycin-induced phase 3 (Table 7).
Table 6. SPONTANEOUS AND ERYTHROMYCIN-INDUCED PHASE 3-LIKE AND PHASE 3
Table 7. MOTILITY INDEX OF PHASE 3 OF MMC
MMC, interdigestive migratory motor complex.
Adverse Effects
Abdominal pain and cramping were seen in one patient in the erythromycin group. However, nausea and vomiting, angialgia, and diarrhea, the major adverse effects of erythromycin, were not seen.
DISCUSSION
The pathogenesis of DGE after pancreaticoduodenectomy or PPPD is thought to involve factors such as peritonitis from anastomotic leaks, 10 ischemia of the antropyloric muscles, 12 gastric atony in response to resection of the duodenal pacemaker, 4 and reduction in circulating motilin levels. 5 Univariate analysis of DGE after PPPD showed that establishment of a gastrostomy, the length of the preserved duodenum, gastric juice output, duration of gastric tube placement, and administration of cisapride were significant covariates. 2 Therefore, to simplify the pathogenesis of DGE and the influence of erythromycin on DGE after Billroth 1 PPPD, pancreatic anastomotic leakage was excluded from the analysis and no gastrostomy was created. In this series, patients receiving erythromycin had a shorter duration of nasogastric drainage, earlier resumption of eating, and a 75% reduction in the incidence of DGE (14.3 vs. 57.1). This reduction in the incidence of DGE was much better than the 53% reduction that Yeo et al 8 reported. The difference may be due to differences in dosage and the date on which erythromycin was commenced. They used a higher dose of erythromycin (200 mg) on days 3 to 10 after surgery; we gave low doses (1 mg/kg) from days 1 to 14 after surgery. Higher doses of erythromycin (200–300 mg) induce strong contractions, which are not propagated, whereas a lower dose of erythromycin (40 mg) induces a premature phase 3 that migrates through the small intestine. 9
Erythromycin hastened the nasogastric tube removal day on univariate analysis and was an independent influence on nasogastric tube removal in the multivariate analysis using a Cox proportional hazard model. In addition, in a stepwise multiple regression analysis using a Cox proportional hazard model, erythromycin and preservation of the right gastric artery were significant covariates. The relative risk was 6.3-fold for erythromycin and 4-fold for preservation of the right gastric artery. Groups of patients with different combinations of erythromycin and preservation of the right gastric artery had relevant differences in nasogastric tube removal. Tube removal was delayed the longest in patients who did not receive erythromycin and who underwent right gastric artery dissection (P < .001). Right gastric artery removal was a predictive factor for the effectiveness of erythromycin. Chronic mesenteric ischemia causes reversible gastroparesis and gastric dysrhythmias. 12 Ischemia of the antropyloric muscles resulting from right gastric artery dissection may result in gastric dysrhythmias and influence the effects of erythromycin. In this study, the mean length of the preserved duodenum was 3.6 cm, and it did not influence DGE or erythromycin. Preservation of the vagal pyloric branch had no major affect on DGE in this series, as in a previous report. 13
Abnormal motility in the antrum, called tachygastria and dysrhythmia, plays a part in the pathogenesis of DGE after PPPD. Electrogastrography showed tachygastria 2 weeks to 1 month after Billroth I PPPD, 14 and monometric studies showed a few irregular contractions with no cyclic pattern on postoperative day 18. 15 In this series, gastric motility was still quiescent in 4 of the 14 patients (29%), but no patients showed abnormal motility on postoperative day 30. The other 71% of patients already had phase 3-like or phase 3 activity of the MMC in the stomach. Matsunaga et al 15 reported that the return of phase 3 activity in the gastric MMC was not observed within 3 weeks after PPPD; the earliest recovery was noticed on postoperative day 32 and the latest on day 54. In our study, phase 3 of the MMC appeared earlier than their mean first appearance of 41 ± 2 days. This is probably explained by differences in the methodology used to study motility. We did not create a gastrostomy and placed the catheter transnasally. In contrast, they established a gastrostomy and used that route to insert the manometric catheter into the stomach. The gastrostomy might be a cause of DGE and the delay of the first appearance of phase 3.
Low-dose erythromycin (40 mg) induces a premature phase 3 that commences in the stomach and migrates through the small intestine with the same characteristics as a spontaneously occurring phase 3 in a normal unfed stomach. 9 Low-dose erythromycin (1 mg/kg) induced phase 3 in two patients who had a quiescent stomach and phase 3 activity of the MMC in other patients with spontaneous phase 3 after Billroth I PPPD, as well as in unfed normal patients. The phase 3 induced by low-dose erythromycin was similar to the spontaneous phase 3 in amplitude, duration, area, and gastric motility index. These characteristics were no different from those of the spontaneous contractions of phase 3 and erythromycin-induced phase 3 in healthy subjects. 16 However, the erythromycin-induced phase 3 had a higher frequency than the spontaneous phase 3 after Billroth I PPPD. Low-dose erythromycin induced phase 3 of the MMC in 64.3% of patients and phase 3-like activity in 21.4%. The erythromycin-induced phase 3 activity of the MMC may act as a “housekeeper”17 and drastically reduce the incidence of DGE after PPPD. High doses of erythromycin may induce strong, prolonged bursts of antral contraction that do not migrate after Billroth I PPPD as in unfed normal patients.
It is well known that in dogs and humans, the initiation of interdigestive phase 3 contractions in the stomach and duodenum is closely related to elevation of the plasma motilin concentration. 18,19 Erythromycin acts as a motilin agonist by binding to motilin receptors, which are largely confined to the antrum and upper duodenum, 20 and initiates phase 3 activity of the gastric MMC. 6,7 Ischemia of the antropyloric muscles and the length of the preserved duodenum are associated with the functional volume of motilin receptors. These factors would be covariates with the effects of erythromycin on the stomach after Billroth I PPPD. We did not measure the serum motilin level and could not confirm any association between its level, the initiation of phase 3 of the MMC, preservation of the right gastric artery, and the length of the preserved duodenum after Billroth I PPPD. Preservation of the right gastric artery alone, however, was determined as a covariate in a multivariate analysis using a Cox proportional hazard model.
Our injection dosage was much smaller than that of Yeo et al, 8 and the rate of adverse effects was much lower than in their study. Abdominal pain and cramping were seen in just one patient in the erythromycin group. Nausea and vomiting, angialgia, and diarrhea, the major adverse effects of erythromycin, were not seen. Our study determined that a low dose of erythromycin was preferable to a high dose after the unfed period after patients undergoing Billroth I PPPD.
Footnotes
Correspondence: Susumu Ohwada, MD, Second Department of Surgery, Gunma University Faculty of Medicine, 3-39-15 Showa-Machi, Maebashi 371-8511, Japan.
E-mail: sohwada@med.gunma-u.ac.jp
Accepted for publication October 24, 2000.
References
- 1.Yeo CJ, Cameron JL, Sohn TA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg 1997; 226: 248–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamaguchi K, Tanaka M, Chijiiwa K, et al. Early and late complications of pylorus-preserving pancreatoduodenectomy in Japan 1998. J Hepatobiliary Pancreat Surg 1999; 6: 303–311. [DOI] [PubMed] [Google Scholar]
- 3.Hishinuma S, Ogata Y, Matsui J, et al. Complications after pylorus-preserving pancreatoduodenectomy with gastrointestinal reconstruction by the Imanaga method. J Am Coll Surg 1998; 186: 10–16. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka M, Sarr MG. Total duodenectomy: effect on canine gastrointestinal motility. J Surg Res 1987; 42: 483–493. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka M, Sarr MG. Role of the duodenum in the control of canine gastrointestinal motility. Gastroenterology 1988; 94: 622–629. [DOI] [PubMed] [Google Scholar]
- 6.Kondo Y, Torii K, Itoh Z, et al. Erythromycin and its derivatives with motilin-like biological activities inhibit the specific binding of 125I-motilin to duodenal muscle. Biochem Biophys Res Commun 1988; 150: 877–882. [DOI] [PubMed] [Google Scholar]
- 7.Itoh Z, Nakaya M, Suzuki T, et al. Erythromycin mimics exogenous motilin in gastrointestinal contractile activity in the dog. Am J Physiol 1984; 247: G688–694. [DOI] [PubMed] [Google Scholar]
- 8.Yeo CJ, Barry MK, Sauter PK, et al. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective randomized, placebo-controlled trial. Ann Surg 1993; 218: 229–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tack J, Janssens J, Vantrappen G, et al. Effect of erythromycin on gastric motility in controls and in diabetic gastroparesis. Gastroenterology 1992; 103: 72–79. [DOI] [PubMed] [Google Scholar]
- 10.Hocking MP, Harrison WD, Sninsky CA. Gastric dysrhythmias following pylorus-preserving pancreaticoduodenectomy. Possible mechanism for early delayed gastric emptying. Dig Dis Sci 1990; 35: 1226–1230. [DOI] [PubMed] [Google Scholar]
- 11.Ohwada S, Iwazaki S, Nakamura S, et al. Pancreaticojejunostomy-securing technique: duct-to-mucosa anastomosis by continuous running suture and parachuting using monofilament absorbable thread. J Am Coll Surg 1997; 185: 190–194. [DOI] [PubMed] [Google Scholar]
- 12.Liberski SM, Koch KL, Atnip RG, et al. Ischemic gastroparesis: resolution after revascularization. Gastroenterology 1990; 99: 252–257. [DOI] [PubMed] [Google Scholar]
- 13.Sumida K, Nimura Y, Yasui A, et al. Influence of vagal pyloric branches on gastric acid secretion and gastrointestinal motility in patients following a pylorus-preserving pancreatoduodenectomy. Hepato-gastroenterology 1999; 46: 336–342. [PubMed] [Google Scholar]
- 14.Takeda T, Yoshida J, Tanaka M, et al. Delayed gastric emptying after Billroth 1 pylorus-preserving pancreatoduodenectomy. Ann Surg 1999; 229: 223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsunaga H, Tanaka M, Naritomi G, et al. Effect of leucine 13-motilin (KW5139) on early gastric stasis after pylorus-preserving pancreatoduodenectomy. Ann Surg 1998; 227: 507–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tomomasa T, Kuroume T, Arai H, et al. Erythromycin induces migrating motor complex in human gastrointestinal tract. Dig Dis Sci 1986; 31: 157–161. [DOI] [PubMed] [Google Scholar]
- 17.Suzurszewski JH. A migrating electric complex of the canine small intestine. Am J Physiol 1969; 217: 1757–1763. [DOI] [PubMed] [Google Scholar]
- 18.Itoh Z, Honda R, Hiwatashi K, et al. Motilin-induced mechanical activity in the canine alimentary tract. Scand J Gastroenterol (Suppl) 1976; 39: 93–110. [PubMed] [Google Scholar]
- 19.Peeters TL, Vantrappen G, Janssens J. Fasting plasma motilin levels are related to the interdigestive motility complex. Gastroenterology 1980; 79: 716–719. [PubMed] [Google Scholar]
- 20.Peeters TL, Bormans V, Vantrappen G. Comparison of motilin binding to crude homogenates of human and canine gastrointestinal smooth muscle tissue. Regul Pept 1988; 23: 171–182. [DOI] [PubMed] [Google Scholar]