I would like to express my deep appreciation for the support and confidence of the European Surgical Association for allowing me to serve as your president. Besides being a great honor, this has been one of the most interesting experiences in my life from both the human and professional standpoint.
It is indeed a big pleasure for me to be here today and to share with you some reflections over my academic life. As many of you know, being 70 years old means that you have seen several changes in your profession during the second half of the 20th century. Incredibly, by the time you retire the scenario is still evolving so quickly!
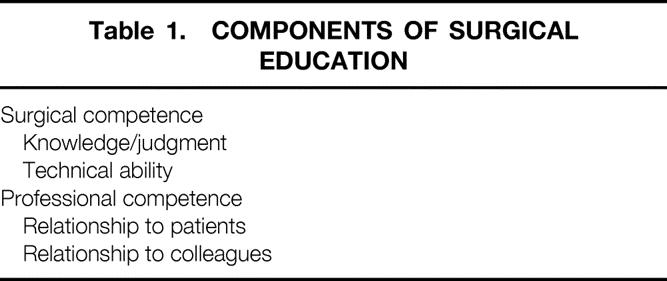
Surgical education, the topic I am going to address, includes a couple of very important aspects. The first is surgical competence, which means knowledge, common sense, and technical ability. The second is professional competence, which means ability to deal with patients and colleagues. Both of these components are necessary for achieving leadership in our discipline (Table 1).
Table 1. COMPONENTS OF SURGICAL EDUCATION
Surgical education is by definition a life-long process, which starts with a solid training period and should be followed by high-quality, continuing medical education. Today, such a process is critical to deliver optimal healthcare in our highly competitive and conflictual society. Surgical competence has become a critical social issue in this era of increasing patient–physician litigation. There is an increasing demand to assess competence in order to ensure safety. Risk factors of surgical procedures may be reduced by adequate training and continuous reinforcement of technical skills. On the other hand, the definition of competence is still elusive, and it is difficult to quantify precisely its essential components.
The subject of surgical education has already been discussed within our Society back in 1995, when a working session on training took place in Paris. Van Schilfgaarde was the chairman of that session. He reported on the changing patterns of graduate surgical education in the Netherlands, emphasizing the need to adapt surgical programs to changes in demands in surgical practice and healthcare delivery systems. 1 Outside Europe, an important panel on surgical education was organized by the International Federation of Surgical Colleges in Vienna in 1999. Lloyd Nyhus put together the experience of four countries (Australia, Japan, South Africa, United States) in an effort to merge different experiences and find a common platform for debate. The result was that surgeons pay more and more attention to certification and recertification issues of trainees, being aware that surgical training does not end with the awarding of the diploma; improvements in many facets of surgical education have been made worldwide, but many gaps remain. 2
The problem is still open even in countries that have a long-lasting tradition in surgical education. For example, it has been recognized that although the surgical residency system in the United States represents a very good model of education, there are other aspects of competence that are difficult to evaluate. In addition to cognitive knowledge, clinical thinking, and surgical judgment, there are other intangible qualities that are difficult to evaluate by the methods currently available. 3
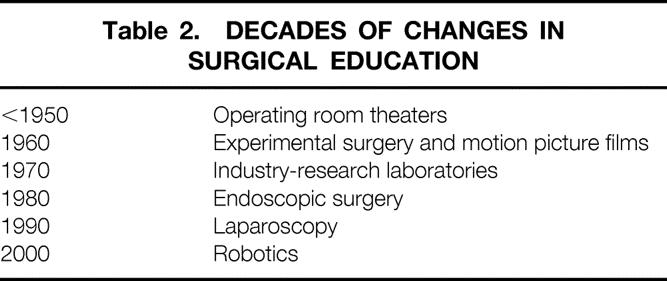
There have been many changes in the methodology of surgical teaching during the past decades (Table 2). Before 1950, the operating room theaters represented the only place dedicated to teaching. Subsequently, during the 1960s, experimental surgery and motion picture films played a major role in surgical education. One of the pioneers in visual education was Dr. Rudolph Matas from New Orleans, who gave his presidential address at the Southern Surgical and Gynecological Association in 1912. To illustrate his thesis, Dr. Matas showed films of operative procedures produced by Dr. Doyen from Paris. The Ciné Clinic program was introduced in 1950 as part of the Clinical Congress of the American College of Surgeons. 4 The first research laboratories supported by the industry appeared during the 1970s and paralleled the development of mechanical sutures. A big step forward in the 1980s was the introduction of videoendoscopic surgery first, followed in the 1990s by laparoscopy and minimal access surgery. And now, at the beginning of the third millennium, we are fully immersed in the robotic era. The predictions made by Dr. Matas have become reality: “The picture machine will ultimately revolutionize the present methods of general education and training.. . . We see the time rapidly approaching when the surgical specialist or teacher of surgery may keep a cinematographic record of his own operations and thus establish the basis of a mutually cooperative and interchangeable cinematographic surgical clinic in which all interested workers can participate.”
Table 2. DECADES OF CHANGES IN SURGICAL EDUCATION
Technical ability is indeed a very important dimension in surgical education. It is still unclear whether technical dexterity depends mostly on congenital ability or training exposure of the individual person. So, the question arises: what is the best way to transform an immature resident into a master surgeon? Indeed, some sophisticated studies from Dundee have found a relationship between congenital ability and the score on psychomotor tests, indicating that such tests may help to select individuals who are technically superior. 5 In fact, there is no question that surgery is, in some respects, a technical exercise at which some people are more adept than others. Perhaps a structured skill program can benefit the teacher in the selection process and the resident in improving his or her technical ability. This kind of philosophy is slowly spreading throughout Europe and getting some consensus. Alfred Cuschieri, one of the pioneers in this field, just a few months ago collected the results of a very interesting survey on surgical competence. The result was that changes are needed, and some can be implemented with relative ease. Moreover, it was felt that improved trainee selection and more objective assessment of performance and progress during training represent the bases for future quality assurance in surgical practice.
While preparing this presidential address, I felt that it was important to have some feedback from all of you in order to answer the following questions: What can we do to strengthen the values of our profession? Does the European Surgical Association have a mission in surgical education? A multiple-item questionnaire was mailed to all members in September 2000. There was a 62% response rate from colleagues of 13 countries. Overall, 94% of the responding members are academic surgeons with a strong interest in surgical education, to which they devote 5% to 50% of their working time (median 15%). The three skills that most members feel should be encouraged during the training period are preoperative assessment, postoperative care, and relation with patients. Most members believe that the optimal learning curve to perform major open or laparoscopic procedures should include between 20 and 40 cases. While most members believe that video-assisted surgery should not be an independent surgical specialty, more than half of them believe that training with minimal access surgery should start from the beginning of the residency program. However, only 14% of the members use objective methods to assess the manual dexterity of the trainees in their institutions. Methods include recording postoperative complications, videotape records, basic skill courses, and sophisticated computer robotics in one center.
Regarding the surgical competence of trainees, 84% of the members think that this should be assessed every year; about two thirds of them feel that a 1-year period of full-time research should be incorporated in a training program. Regarding reassessment of competence, 63% of members would reassess certified surgeons every 5 years, and 95% believe that some operations should be performed only in high-volume centers. It is the opinion of most members that esophageal, pancreatic, and liver operations should be restricted to high-volume centers in order to improve outcome.
The questionnaires showed that most members rely on scientific guidelines in clinical practice, and about 70% feel that the European Surgical Association should organize consensus conferences. The first three preferred topics are colorectal liver metastases, surgery for pancreatic tumors, and research in surgical training. Annals of Surgery is the favorite refereed journal and source of information (70% of the responding members), followed by British Journal of Surgery, Surgery, and World Journal of Surgery. Interestingly, about 30% of the members would open up journals peer review, which means that authors should be allowed to know who are the reviewers.
For clinical decision-making, 82% of members rely on personal experience, original articles, and guidelines from scientific societies. Interestingly, 63% of the members use quality-of-life instruments to better assess surgical outcome, and this indeed reflects the high scientific standard of academic European surgeons. There is a wide consensus on the evidence-based approach in surgery. However, most members feel that randomized clinical trials are not applicable to many surgical procedures; therefore, there is a need to focus on the value of nonrandomized studies of good quality. About 70% of members believe that the European Surgical Association should constitute ad hoc working groups on quality assurance and ethical issues.
A critical look at the results of this survey indicates that European surgeons are ready to meet the new challenges of the third millennium. They are very interested in educational issues, but still there is the need to improve assessment of competence and to implement objective means of evaluation. The way we teach medicine today has considerably changed compared to the last century. It is still true, as Flexner stated in 1910, 6 that learning medicine is a process that requires three steps: being told how to do it, watching a teacher doing it, and then practicing, at first with close supervision and later under general oversight. However, it is the way we practice that should change. Teaching basic surgical skills in the operating room is not efficient anymore and carries high costs. The bench models are the most promising approach, but they are still far from perfection. Bridges and Diamond 7 have calculated the financial impact of teaching residents in the operating room in the United States (Table 3). These costs are impressive if you consider the reduced amount of resources available for healthcare throughout the world! Thus, surgical skills are still learned at considerable expense, including complications, longer operating room times, longer hospital stay, and less-than-optimal long-term results. Looking at the future, the perspective is even worse. Who will pay for graduate education in the future? So, it is evident that there is a need for an articulated training curriculum, for the development of resource facilities, for animal or cadaver laboratories, and for the implementation of virtual surgery.
Table 3. FINANCIAL IMPACT OF TEACHING SURGICAL RESIDENTS IN THE OPERATING ROOM
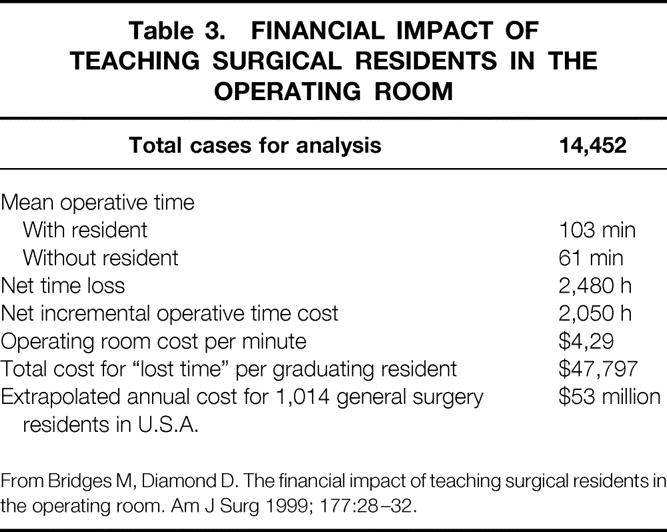
From Bridges M, Diamond D. The financial impact of teaching surgical residents in the operating room. Am J Surg 1999; 177:28–32.
Back in the 1980s, when I was Professor and Chairman of the Department of Surgery at the University of Padua, we started working on case simulation with a personal computer to help students develop clinical skills. This experience was stimulating for the students and the teachers as well. Today, things have evolved a lot and we are getting very close to simulation of technical abilities. At the University of Toronto there is a lot of ongoing research on objective assessment of technical skills. The 5-point rating scale of the OSATS (Objective Structured Assessment Technical Skill), which can assess a number of parameters such as respect for tissue, instrument handling, flow of operation, and so forth, is an interesting educational tool. If validated on a larger scale, it could serve as an objective indicator of technical skills and contribute to the evaluation of our residents. 8
It is probably too early to predict the future of virtual reality. However, just think about aircraft pilots: are they not instructed and assessed this way? Why should not this happen for the surgeons as well? The future of learning and assessing surgical skills will probably be founded in simulation and virtual reality. 9,10 In addition to a solid basic training, education includes a life-long process of continuous professional development, as clearly outlined by the Royal College of Surgeons. In Europe, the Royal College has been the first organization to promote a superb training program that includes the most advanced technological resources. Of course, the Internet and the satellite technology will play an increasingly important role in the future as tools for continuing medical education.
It is time now for another crucial question: who are the potential providers of surgical education in Europe? The answer could be the European Council (through the advisory committee on medical training), the UEMS (through the European Board of Surgery), the universities, the leading scientific societies, and, last but not least, the private groups. But, unfortunately, no distinct responsibilities exist at present. Toni Lerut, who served as our past president, clearly stated in his presidential address last year that professional networking between surgeons may improve quality and outcome. 11 I agree with him that the academic surgeons need to regain leadership in the field of education, and that the European Surgical Association should be involved in the process of training and continuing development. The European Surgical Association is a leading scientific group that should have the power to make effective proposals in this matter!
In conclusion, information technology is rapidly changing the pattern of education throughout the world, and we must quickly adapt to this explosive change. As scientists, clinicians, and academic surgeons, we must be more and more aware of our mission in training, continuing education, and maintenance of high ethical standards. The European Surgical Association may contribute to our mission and to the spreading of educational issues.
Acknowledgments
The author thanks Luigi Bonavina, Associate Professor of Surgery at the University of Milano, for his skillful and enthusiastic assistance in writing this paper. The author also thanks Professor Henry Bismuth, Alfred Puschieri, and Jacques Marescaox for their advice and support.
Footnotes
Correspondence: Alberto Peracchia, Department of Surgical Sciences, University of Milano, Via F. Sforza 35, I-20122 Milano, Italy.
E-mail: alberto.peracchia@unimi.it
Accepted for publication April 2001.
References
- 1.Zwierstra R, Scherpbier A, Van Schilfgaarde R. Changing patterns in graduate surgical education in the Netherlands. World J Surg 1994; 18: 717–723. [DOI] [PubMed] [Google Scholar]
- 2.Nyhus L, Idezuki Y, Sheldon D, et al. Creation, evaluation, and continuing assurance of excellence of the certified surgical specialist. World J Surg 2000; 24: 1519–1525. [DOI] [PubMed] [Google Scholar]
- 3.Scott D, Valentine J, Bergen P, et al. Evaluating surgical competency with the American Board of Surgery in-training examination, skill testing, and intraoperative assessment. Surgery 2000; 128: 613–622. [DOI] [PubMed] [Google Scholar]
- 4.Stephenson G. American College of Surgeons at 75. Chicago: American College of Surgeons; 1994.
- 5.Macmillan A, Cuschieri A. Assessment of innate ability and skills for endoscopic manipulations by the advanced Dundee endoscopic psychomotor tester: predictive and concurrent validity. Am J Surg 1999; 177: 274–277. [DOI] [PubMed] [Google Scholar]
- 6.Flexner A. Medical Education in the United States and Canada. Boston: Merrymount Press; 1910.
- 7.Bridges M, Diamond D. The financial impact of teaching surgical residents in the operating room. Am J Surg 1999; 177: 28–32. [DOI] [PubMed] [Google Scholar]
- 8.Reznick R, Regehr G, Reznick R, et al. Testing technical skill via an innovative “bench station” examination. Am J Surg 1996; 173: 226–230. [DOI] [PubMed] [Google Scholar]
- 9.Meier A, Rawn C, Krummel T. Virtual reality: surgical application-challenge for the new millennium. J Am Coll Surg 2001; 192: 372–384. [DOI] [PubMed] [Google Scholar]
- 10.Trunkey D, Botney R. Assessing competency: a tale of two professions. J Am Coll Surg 2001; 192: 385–395. [DOI] [PubMed] [Google Scholar]
- 11.Lerut T. The surgeon as a prognostic factor. Ann Surg 2000; 6: 729–732. [DOI] [PMC free article] [PubMed] [Google Scholar]


