Abstract
Objective
To conduct a retrospective study of 15 patients with persistent (n = 4) and recurrent (n = 11) hyperparathyroidism.
Summary Background Data
Secondary hyperparathyroidism may persist or recur because of hyperfunction of the parathyroid remnant or transplanted parathyroid tissue. It is a great challenge to localize the parathyroid tissue either in the neck or at the arm before surgery.
Methods
From June 1994 to June 2000, 15 patients with recurrent and persistent secondary hyperparathyroidism were selected for surgery for the removal of parathyroid tissue. The indications for surgery included bone pain, hypercalcemia, general weakness, and skin itching. Their ages ranged from 23 to 66 years. The average period of persistent hyperparathyroidism after total parathyroidectomy with autotransplantation was 3.8 months; that of recurrent hyperparathyroidism was 53 months. Serum levels of calcium, phosphorus, parathyroid hormone (iPTH), and alkaline phosphatase were measured before surgery and 1 week after surgery. Before surgery, the parathyroid gradient in the blood draining the graft-bearing arm versus the contralateral arm was measured. A 99mTc-sestamibi (MIBI) scan was performed including the neck and the arm area, and a computed tomography (CT) scan of the neck was performed to confirm the localization. The neck and mediastinal exploration was done directly at the side of localization under general anesthesia to remove the parathyroid tissue that had been located with the MIBI scan or CT scan. An arm exploration was done under local anesthesia to remove all parathyroid tissues detected in the MIBI scan or palpable masses during surgery. If all glands were removed, 0.5 × 0.5 × 0.5 cm of tissue (60–100 mg) was maintained in situ or the same amount of tissue was reimplanted.
Results
The average ratio of iPTH in the graft-bearing arm to the contralateral arm in the 5 patients with parathyroid tissue in the neck was 1.17 ± 0.16, and that in the 10 patients with parathyroid at the arm was 14.15 ± 16.62. A significant difference was found between the two groups. MIBI scans showed parathyroid tissues in the neck in four of five patients and in seven of eight patients at the arm. Computed tomography showed the parathyroid tissues in the neck and mediastinum in five of five patients (100%). Five glands were removed from these five patients, three in the neck, one in the mediastinum, and one in the carotid sheath. In total, 20 glands and 2 half-glands were removed from 10 patients; among these, 14 glands were shown in the MIBI scan. All patients had improvements of symptoms and signs after surgery. Serum levels of calcium, phosphorus, and iPTH decreased rapidly after surgery, but alkaline phosphatase did not.
Conclusions
With the results obtained from the ratio of iPTH of the graft-bearing arm to the contralateral arm, clinical palpation of the arm, MIBI scan, CT scan, careful surgical exploration, and adequate resection, recurrent and persistent secondary hyperparathyroidism can be successfully treated with surgery in the neck or at the arm.
Persistent and recurrent hyperparathyroidism after total parathyroidectomy with autotransplantation is a challenge to surgeons as well as physicians of nuclear medicine. Persistent disease occurs when there is inadequate initial surgery as a result of missed fifth parathyroid gland or an inadequate subtotal resection of parathyroid tissue. Recurrence after initially successful surgery usually occurs because of hypertrophy of the cervical parathyroid tissue or the parathyroid grafts.
Before a study of autotransplantation of parathyroid tissue to the forearm muscle or the subcutaneous tissue in 1996, 1,2 we had routinely removed all parathyroid glands no matter whether three, four, or five glands were found during surgery for secondary hyperparathyroidism and implanted 60 mg fresh parathyroid tissue into three dry pockets in the forearm (muscle layer or subcutaneous tissue). After that study, we implanted the parathyroid tissue in the subcutaneous tissue in all patients. We now report our experience with surgery for persistent or recurrent hyperparathyroidism after total parathyroidectomy with autotransplantation.
METHODS
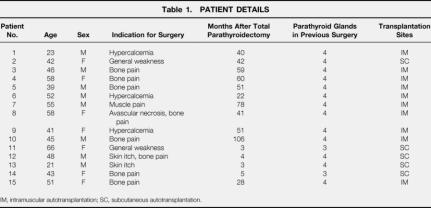
From June 1994 to June 2000, 185 patients underwent surgery for symptomatic secondary hyperparathyroidism with total parathyroidectomy and autotransplantation. Among them, 110 patients had autotransplantation to the subcutaneous tissue and 75 patients to the muscle layer. After surgery, serum levels of calcium, phosphorus, and alkaline phosphatase were checked monthly and levels of parathyroid hormone (iPTH) were checked every 6 months. If those levels increased gradually (iPTH > 650 ng/L) and patients had symptoms such as bone pain, skin itching, general weakness, and so forth, the nephrologist would refer them to this team for further work-up. A total of 15 patients who were selected for surgery because of persistent or recurrent hyperparathyroidism were enrolled into this study. Their ages ranged from 23 to 66 years (median 45). Seven of them were women. They all received regular dialysis three times a week, and the mean period after total parathyroidectomy with autotransplantation was 3.8 months (range 3–5) for persistent disease and 53 months (range 22–106) for recurrent disease. Previous operations showed four glands in 13 patients and three glands in 2 patients. The indications for surgery were bone pain in eight patients, hypercalcemia (>11 mg/dL) in three, general weakness in two, and skin itching in two (Table 1). Previous autotransplantation was performed in the subcutaneous tissue in 5 patients and in the muscle layer in 10 patients.
Table 1. PATIENT DETAILS
IM, intramuscular autotransplantation; SC, subcutaneous autotransplantation.
Persistence of secondary hyperparathyroidism can be defined as the persistence or recurrence of the typical symptoms, laboratory parameters, and radiologic signs within 6 months after surgery. 3 A later occurrence of symptoms and signs of secondary hyperparathyroidism should be classified as recurrence.
Before surgery, serum levels of calcium, phosphorus, iPTH, and alkaline phosphatase were measured routinely. Serum iPTH levels were measured by iPTH radioimmunoassay and prediluted with zero standard reagent C (iPTH 100T Kit-catalog No.40-2107, Nichols Institute Diagnostics, San Juan Capistrano, CA) to 10× and 100× routinely in these patients.
The iPTH gradient of the graft-bearing arm versus the contralateral arm was then measured and recorded. Serum samples were obtained from the antecubital veins of the transplanted arm and the dorsal palm veins of the contralateral arm (with arteriovenous fistula). A positive gradient was defined as a twofold step-up in the grafted arm. 4 99mTc-sestamibi (MIBI) scan was performed in 13 patients but not in the other 2. After 25 mCi 99mTc-sestamibi was injected intravenously, three sets of images were obtained: the initial set at 10 to 15 minutes and delayed sets at 2 and 4 hours after injection of the pharmaceutical. The initial set of images corresponded to the thyroid phase and the delayed sets to the parathyroid phase, 5–7 either in the neck or at the graft-bearing arm.
Computed tomography (CT) of the neck and upper chest using thin cuts (3 mm) with intravenous contrast was performed in five patients who had a negative iPTH gradient of the graft-bearing arm versus the contralateral arm or a positive MIBI scan in the neck. Neck surgery was performed under general anesthesia at the side of localization after the MIBI scan and the positive CT scan to remove the parathyroid tissue. Exploration of the arm with the grafted parathyroid tissue was performed under local anesthesia if the iPTH gradient was positive and the parathyroid tissue was detected in the MIBI scan. All the parathyroid tissue apparent in the MIBI scan or clinically palpable during surgery was completely removed, and about a half-piece (0.5 × 0.5 × 0.5 cm in largest dimension; 60–100 mg) of the tissue was left remaining, or the same size was autotransplanted.
One week after surgery, calcium, phosphorus, alkaline phosphatase, and iPTH were measured in the contralateral arm. Symptoms and signs were recorded in the follow-up period.
Statistical significance was assessed by the Student t test for paired and unpaired samples and by the Mann-Whitney test for nonparametric samples. Statistical tests were performed using SPSS (SPSS Inc., Cary, NC, 1994). P < .05 was considered significant.
RESULTS
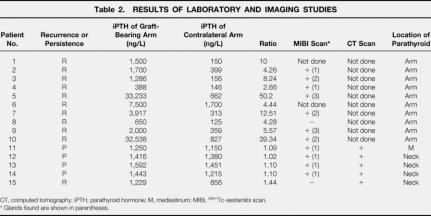
Four patients had persistent disease and 11 had recurrent disease (Table 2). The five patients with persistent and recurrent hyperparathyroidism in the neck had an iPTH ratio (graft-bearing arm to contralateral arm) of 1.02 to 1.44 (1.17 ± 0.16, mean ± SD). The 10 patients with recurrent hyperparathyroidism in the arm had an iPTH ratio of 2.66 to 50.2 (14.15 ± 16.62). Using the Mann-Whitney test, significant differences were noted between the two groups (P = 0.001).
Table 2. RESULTS OF LABORATORY AND IMAGING STUDIES
CT, computed tomography; iPTH, parathyroid hormone; M, mediastinum; MIBI, 99mTc-sestamibi scan.
* Glands found are shown in parentheses.
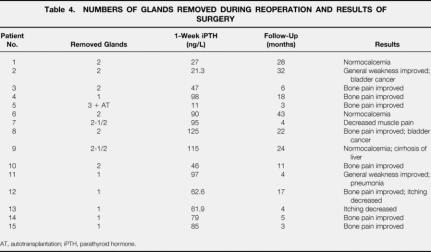
The MIBI scan showed four of five parathyroid glands in the neck. The sizes of the glands in surgery were 1.5 × 1.1 × 1.1 cm, 2 × 1.7 × 1.4 cm, 3 × 1.6 × 1.2 cm, and 1.5 × 0.8 × 0.7 cm; the one that did not show up on the MIBI scan was smaller (0.9 × 0.8 × 0.6 cm). The CT scan of the neck showed all five parathyroid glands: three at the neck, one at the carotid sheath, and one at the mediastinum. Surgery identified those five glands, which weighed about 1.88 g, 2.10 g, 3.02 g, 0.48 g, and 0.25 g (Table 3).
Table 3. DETAILS OF FIVE PARATHYROID GLANDS
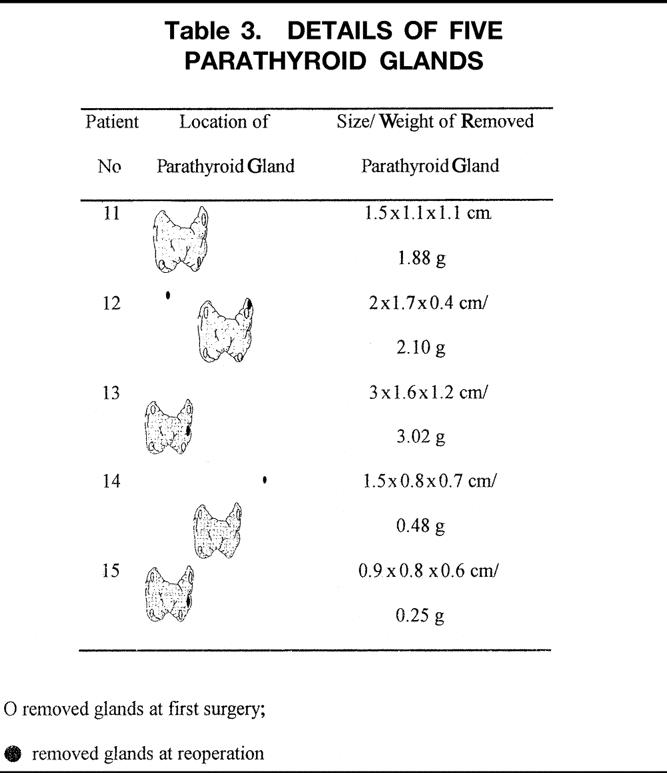
The MIBI scan gave positive results of 14 glands at the forearm in seven of eight patients. These glands measured 3 × 2 × 3 cm to 0.6 × 0.6 × 0.6. Only two glands (one of eight patients) not detected by the MIBI scan were palpable during surgery, and they measured 0.5 × 0.5 × 0.4 cm and 0.6 × 0.5 × 0.5 cm. Patient 1 had two parathyroid glands (0.7 × 0.7 × 0.6 cm and 0.6 × 0.6 × 0.4 cm) and patient 6 also had two glands (0.8 × 0.6 × 0.5 cm and 0.7 × 0.6 × 0.4 cm); these clinically and intraoperatively palpable masses were removed without a preoperative MIBI scan. The iPTH ratio was 10 in patient 1 and 4.44 in patient 6 (see Table 2). In total, 20 glands and 2 half-glands were removed from these 10 patients. Among them, only patient 5 had autotransplantation of parathyroid tissue (Table 4). Before surgery, serum levels of calcium, phosphorus, iPTH, and alkaline phosphatase were 10.4 ± 0.7 mg/dL, 5.1 ± 1.8 mg/dL, 728 ± 541 pg/mL, and 196 ± 157 U/L, respectively. One week after surgery, the corresponding levels were 8.4 ± 1.7 mg/dL, 3.5 ± 1.4 mg/dL, 72 ± 35 pg/mL, and 205 ± 183 U/L. A significant reduction was noted in calcium (P < .001), phosphorus (P = .005), and iPTH (P < .001); no reduction was noted in alkaline phosphatase (P = .741).
Table 4. NUMBERS OF GLANDS REMOVED DURING REOPERATION AND RESULTS OF SURGERY
AT, autotransplantation; iPTH, parathyroid hormone.
In the follow-up period of 3 to 43 months, all patients’ symptoms improved. Patient 11 had pneumonia and adult respiratory distress syndrome after parathyroid surgery. She was admitted as an inpatient for more than 2 months before discharge. An improvement in general weakness was noted in patient 2, and a decrease of bone pain was noted in patient 8. Both of these patients had bladder cancer in the follow-up period. Patient 9 had cirrhosis of the liver with a normal calcium level (see Table 4).
DISCUSSION
Like many surgeons, we consider total parathyroidectomy with immediate reimplantation of parathyroid tissue in the forearm to be the surgical treatment of choice for secondary hyperparathyroidism, because in case of recurrence, reoperation in the forearm is easier than in the neck. 7–9 Our procedure of implanting 60 mg into three pockets in the forearm subcutaneous tissue made reoperation even easier. We decided to remove parathyroid tissues detected by the MIBI scan or palpable during surgery. We kept about 0.5 × 0.5 × 0.5 (60–100 mg) in situ or for reimplantation immediately.
Persistent secondary hyperparathyroidism after total para-thyroidectomy with autotransplantation was never graft-dependent but was related to missed tissues in the neck or mediastinum. Usually, persistent secondary hyperparathyroidism was caused by failure to locate all four hyperplastic glands, as in patient 11 (mediastinum) and patient 14 (carotid sheath near the bifurcation). Another reason for initial failure was overlooking supernumerary glands, which can be expected in 13% of patients with secondary hyperparathyroidism. 10 Three patients in our study (patients 12, 13, and 15) had a fifth gland on the left side of the neck that we missed at the first operation. Hyperfunction of the autografted tissue in the forearm was the most common reason for a second surgery. All graft-dependent recurrences occurred after autotransplantation of fresh tissue and led to symptomatic disease and reoperation after a minimum of 22 months in this study. In patients with persistence or recurrence of secondary hyperparathyroidism after total parathyroidectomy with autotransplantation, it was difficult to localize the source of hormone excess, to determine whether it was in the neck or at the forearm. In our study, we found that the iPTH ratio of the graft-bearing arm to the contralateral arm, MIBI scan, CT scan, and clinical palpation before or during surgery were helpful. The parathyroid hormone determination in the blood draining the graft-bearing arm versus the contralateral arm was most helpful: the ratio was less than 2.0 if the parathyroid tissue was in the neck and more than 2.0 if it was in the arm. A previous report found that the parathyroid hormone determination in the blood draining the graft-bearing arm versus the contralateral arm was not successful. 11 One possible reason for the failure is the high level of parathyroid hormone in the systemic blood, which can disguise a hormone gradient. The determinations in patients with normal graft function show better results in the presence of generally lower systemic levels than were found in patients with recurrent or persistent secondary hyperparathyroidism. 12,13 However, in this study of symptomatic recurrent or persistent hyperparathyroidism, this ratio seemed to work very well in differentiating the location of parathyroid tissues in the neck or at the arm. Accurate measurements of iPTH levels after predilution to 10× and 100× made the data more dependable and the localization more correct. We did not use intraoperative parathyroid hormone measurements, 14 but this might be very useful for the complete removal of parathyroid tissue, whether in primary surgery or in persistent and recurrent disease.
The MIBI scan was initially used for myocardial perfusion imaging but has gained widespread use in parathyroid imaging during the past several years. The large number of mitochondria present in cells of parathyroid adenomas may be responsible for the abundant uptake and slow release of MIBI for these cells. 6 Before reoperation, MIBI scanning has been reported to show a range of successful localization rates: Majors et al 15 reported a 100% preoperative localization rate in 9 patients, Weber et al 16 reported a 88% localization rate in 16 patients, Rodriquez et al 17 reported a 60% localization rate, and Peeler et al 7 reported that 69% were localized before surgery. In this study, 11 of 13 (84.6%) were localized before surgery. Two of three glands found in the normal position were located before surgery by the MIBI scan. Two glands, one in the carotid sheath and another in the mediastinum, were also located. Using the MIBI scan, we missed only one in the neck, which was relatively small (0.9 × 0.8 × 0.6 cm) and one in the arm with two glands, which showed a low iPTH (650 ng/L). The size and function of parathyroid tissues may affect the localization rate of the MIBI scan.
The accuracy of CT depends on tumor size. Published gland localization rates for CT scanning have been 46% to 76%. 6,7,18,19 Computed tomography is best at visualizing glands in ectopic locations, including undescended and retrosternal glands. In a previous study, the glands were found in the ectopic location in 9 of 13 (69%) positive scans, 7 whereas two of five were found in the current study. Overall, five of five (100%) glands were found using CT scan. This high preoperative rate was due to the fact that the iPTH ratio and the MIBI scan had been obtained before the CT scan was ordered, and both gave information about the localization of parathyroid tissue and helped the radiologist to interpret the CT scan.
The surgical alternative avoids the need for medication, and if the autografted tissues function, it allows normal calcium and phosphate metabolism and demineralization of bone. Because permanent postoperative hypoparathyroidism can occur after total parathyroidectomy or after reoperation for recurrent or persistent hyperparathyroidism, cryopreservation should be performed after all these operations, even if most patients will not need the cryopreserved tissue later. After surgery, transient hypocalcemia was found in eight patients, but 3 months later all could be maintained with low dose of calcium carbonate and vitamin D3. Hypocalcemia seemed to cause little trouble, and none of the patients in this study needed reimplantation of the cryopreserved tissue.
Symptomatic patients with persistent or recurrent secondary hyperparathyroid should have iPTH levels obtained both at the graft-bearing arm and the contralateral arm; this should be followed by a MIBI scan. Localization of the parathyroid tissue in the neck or mediastinum should be accompanied by an anatomic imaging technique, either CT scan or magnetic resonance image. Surgery is performed at the localization site. If parathyroid tissue is found in the forearm and is compatible with the ratio of iPTH levels of more than 2, surgery to remove parathyroid tissues detected in the MIBI scan or palpable during surgical exploration should be carried out. A 100% success rate in our series compares favorably with other reported reoperative parathyroid studies in the literature, which in general have success rates in the range of 70% to 96%. 4,20–22
In patients with persistent and recurrent secondary hyperparathyroidism, we generally call for independent localization by at least two positive studies before surgery, 7,19,23,24 as other surgeons have suggested (Fig. 1). Those studies should include the iPTH gradient, MIBI scan, CT scan, and clinical palpation at the arm. Computed tomography and other localization procedures are necessary if the parathyroid tissue is found in the neck or mediastinum.
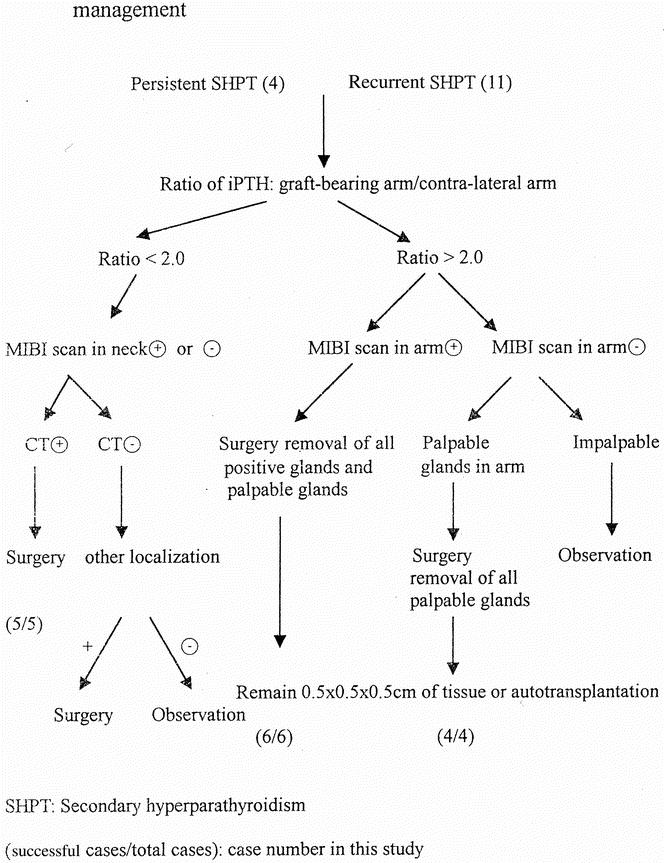
Figure 1. Algorithm for the preoperative localization and surgical management of patients with persistent or recurrent secondary hyperparathyroidism (SHPT).
Footnotes
Correspondence: Fong-Fu Chou, MD, 123, Ta-Pei Road, Niao-Sung Hsiang, Kaohsiung Hsien, Taiwan
E-mail: choulu@ms4.hinet.net
Accepted for publication April 5, 2001.
References
- 1.Wells SA Jr, Leight GS, Ross AJ. Primary hyperparthyroidism. Curr Probl Surg 1980; 17: 398–463. [PubMed] [Google Scholar]
- 2.Chou FF, Chan HM, Huang TJ, et al. Autotransplantation of parathyroid glands into subcutaneous forearm tissue for renal hyperparathyroidism. Surgery 1998; 124: 1–5. [PubMed] [Google Scholar]
- 3.Brennan MF, Doppman JL, Marx SJ, et al. Reoperative parathyroid surgery for persistent hyperparathyroidism. Surgery 1978; 83: 669–676. [PubMed] [Google Scholar]
- 4.Rotstein L, Irish J, Gullane P, et al. Reoperative parathyroidectomy in the era of localization technology. Head Neck 1998; 20: 535–539. [DOI] [PubMed] [Google Scholar]
- 5.Martin D, Rosen I, Ichise M. Evaluation of single isotope technetium 99M-sestamibi in localization efficiency for hyperparathyroidism. Am J Surg 1996; 172: 663–666. [DOI] [PubMed] [Google Scholar]
- 6.Falke THM, Sandler MP, Schipper J. Parathyroid glands. In: Sandler MP, Coleman RE, et al, eds. Diagnostic nuclear medicine, 3d ed. Baltimore: Williams & Wilkins; 1994: 991–1012.
- 7.Peeler BB, Mortin WH, Sandler MP, et al. Sestamibi parathyroid scanning and preoperative studies for patients with recurrent/persistent hyperparathyroidism or significant comorbid conditions: development of an optional localization strategy. Am Surgeon 1997; 63: 37–46. [PubMed] [Google Scholar]
- 8.Skinner KA, Zuckerbraun L. Recurrent secondary hyperparathyroidism. An argument for total parathyroidectomy. Arch Surg 1996; 131: 724–727. [DOI] [PubMed] [Google Scholar]
- 9.Rothmund M, Wagner PK, Schark C. Subtotal parathyroidectomy versus total parathyroidectomy and antotransplantation in secondary hyperparathyroidism: a randomized trial. World J Surg 1991; 15: 745–750. [DOI] [PubMed] [Google Scholar]
- 10.Akerstrom G, Malmaeus J, Berstrom R. Surgical anatomy of human parathyroid glands. Surgery 1984; 95: 14–21. [PubMed] [Google Scholar]
- 11.Rothmund M, Wagner PK. Reoperations for persistent and recurrent secondary hyperparathyroidism. Ann Surg 1988; 207: 310–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rothmund M, Wagner PK. Total parathyroidectomy and autotransplantation of parathyroid tissue for renal hyperparathyrodism. A one- to six-year follow-up. Ann Surg 1983; 197: 7–16. [PMC free article] [PubMed] [Google Scholar]
- 13.Rothmund M, Wagner PK. Assessment of parathyroid graft function after autotransplantation of fresh and cryopneserved tissue. World J Surg 1984; 8: 527–533. [DOI] [PubMed] [Google Scholar]
- 14.Tonelli F, Spini S, Tommasi M, et al. Intraoperative parathyroid hormone measurement in patients with multiple endocrine neoplasia type I syndrome and hyperparathyroidism. World J Surg 2000; 24: 556–563. [DOI] [PubMed] [Google Scholar]
- 15.Majors JD, Burke GJ, Mansberger AR, et al. Technetium Tc-99m sestamibi scan for localization abnormal parathyroid glands after previous neck operation: preliminary experience in reoperative cases. South Med J 1995; 88: 327–330. [DOI] [PubMed] [Google Scholar]
- 16.Weber CJ, Vansant J, Alazraki N, et al. Value of technetium-99m sestamibi iodine-123 imaging in reoperative parathyroid surgery. Surgery 1993; 114: 1011–1018. [PubMed] [Google Scholar]
- 17.Rodriquez JM, Tezelman S, Siperstein AE, et al. Localization procedures in patients with persistent or recurrent hyperparathyroidism. Arch Surg 1994; 129: 870–875. [DOI] [PubMed] [Google Scholar]
- 18.McIntyre RC, Kumpe DA, Liechty RD. Reexploration and angiographic ablation for hyperparathyroidism. Arch Surg 1994; 129: 499–503. [DOI] [PubMed] [Google Scholar]
- 19.Levin KE, Gooding GAW, Okerlund M, et al. Localizing studies in patients with persistent or recurrent hyperparathyrodism. Surgery 1987; 102: 917–925. [PubMed] [Google Scholar]
- 20.Grant CS, van Heerden JA, Charbonneau JW, et al. Clinical management of persistent and recurrent primary hyperparathyroidism. World J Surg 1986; 10: 555–565. [DOI] [PubMed] [Google Scholar]
- 21.Silver CE, Veley FJ. Parathyroid reexploration. Am J Surg 1992; 164: 606–609. [DOI] [PubMed] [Google Scholar]
- 22.Cattan P, Halimi B, Aidan K, et al. Reoperation for secondary aremia hyperparathyroidism: Are technical difficulties influenced by initial surgical procedure? Surgery 2000; 127; 562–565. [DOI] [PubMed] [Google Scholar]
- 23.Miller DL. Preoperative localization and interventional treatment of parathyroid tumors: When and how? World J Surg 1991; 15; 706–715. [DOI] [PubMed] [Google Scholar]
- 24.Carter WB, Carter DL, Cohn HE. Cause and current management of reoperative hyperparathyroidism. Am Surg 1993; 59: 120–124. [PubMed] [Google Scholar]