Abstract
Objective
To assess the effectiveness of bioresorbable Seprafilm membrane in preventing abdominal adhesions in a prospective clinical randomized multicenter trial.
Summary Background Data
Adhesions occur frequently after abdominal operations and are a common cause of bowel obstruction, chronic abdominal pain, and infertility. To reduce the formation of adhesions, a mechanical barrier composed of hyaluronic acid and carboxymethylcellulose was developed, preventing adherence of tissues after abdominal surgery.
Methods
Between April 1996 and September 1998, all patients requiring a Hartmann procedure for sigmoid diverticulitis or obstructed rectosigmoid were randomized to either intraperitoneal placement of the antiadhesions membrane under the midline during laparotomy and in the pelvis, or as a control. Direct visual evaluation of the incidence and severity of adhesions was performed laparoscopically at second-stage surgery for restoration of the continuity of the colon.
Results
A total of 71 patients were randomized; of these, 42 could be evaluated. The incidence of adhesions did not differ significantly between the two groups, but the severity of adhesions was significantly reduced in the Seprafilm group both for the midline incision and for the pelvic area. Complications occurred in similar numbers in both groups.
Conclusions
Seprafilm antiadhesions membrane appears effective in reducing the severity of postoperative adhesions after major abdominal surgery, although the incidence of adhesions was not diminished. The authors recommend using Seprafilm when relaparotomy or second-look intervention is planned. Long-term studies are needed to assess the cost-effectiveness and value of Seprafilm in preventing bowel obstruction, chronic abdominal pain, and infertility.
Adhesions after abdominal surgery are abnormal attachments between tissues or organs. The formation of adhesions may result from mechanical peritoneal damage, intraabdominal ischemia, and the presence of foreign materials in the abdominal cavity such as glove powder, microorganisms, gauze lint, sutures, and prosthetic mesh. 1–3 Adhesions occur in 68% to 100% of patients undergoing one or more laparotomies. 1,3,4
Although intraabdominal adhesions are asymptomatic in most patients, adhesions can cause intestinal obstruction, chronic abdominal pain, infertility, and an increased rate of complications during subsequent operations. 5 Adhesions are the most common cause of intestinal obstructions in the Western world. 4 Another clinical problem, possibly caused by adhesions, is chronic abdominal pain. 6,7 Infertility is a known sequela of intraabdominal adhesions. 8,9 The increased complication rate can be caused by a longer duration of surgery, postoperative bleeding, and a higher risk of bowel perforations. 5,10 The incidence of these complications increases with the number of previous laparotomies or laparoscopies. 11
Substantial costs are associated with adhesion-related clinical problems. 12,13 In 1988, hospital admissions for adhesiolysis were responsible for an estimated $1.180 million in expenditures in the United States. 14,15
Prevention of the formation of adhesions during surgery entails reducing surgical trauma and avoiding contamination of the abdominal cavity with foreign materials. Other means have been sought to reduce postoperative adhesions. Theoretically, a mechanical barrier between adjacent tissues could provide a way of reducing adhesion formation by preventing tissues and organs from adhering to each other. Regeneration of damaged peritoneum is completed within 7 days after surgical trauma. 16 To avoid the persistent presence of foreign material within the abdominal cavity and still attain the intended effect, a temporary barrier not resolving within 7 days is preferable. HAL-F Bioresorbable Membrane (Seprafilm; Genzyme Corp., Cambridge, MA) was developed to serve as a mechanical barrier between surgically damaged tissues. Resorption of this biodegradable membrane starts after 7 days. In animal studies and in one randomized clinical trial, it has been shown that Seprafilm reduces the incidence, extent, and severity of postsurgical adhesions. 17
The incidence of adhesions after (partial) colectomy is high, so this procedure provides a suitable model for studies of adhesion prevention. 18,19 A Hartmann procedure with second-stage restoration of the continuity of the colon was chosen as a model to examine the effectiveness of the Seprafilm membrane.
The aim of this prospective clinical randomized multicenter trial was to assess the effectiveness of this antiadhesions membrane in reducing the number, incidence, and severity of adhesions in patients with diverticulitis or obstruction of the rectosigmoid.
METHODS
Between April 1996 and September 1998, all patients requiring a Hartmann procedure for diverticulitis or obstruction of the rectosigmoid were randomized to receive Seprafilm or to serve as a control patient at eight participating general hospitals. Patients were not included if they were pregnant or had carcinosis peritonei, had received any other investigational product, or had their abdomen irrigated by povidone-iodine, corticosteroids, heparin, salicylates, nonsteroidal antiinflammatory drugs, dextran, or antibiotics. If patients were likely to require reoperation within 3 weeks after the Hartmann procedure or if concomitant disease would probably interfere with restorative surgery, they were not included. Patients were informed about the trial both orally and in writing and signed informed consent. Randomization was achieved by opening a sealed envelope at the time of surgery marked by study number and containing directions whether to use Seprafilm or not. Randomization was obtained according to a balanced computer-generated list, stratified by hospital.
Seprafilm is a membrane developed for the temporary separation of tissues damaged mechanically during surgery. It is composed of chemically modified sodium hyaluronate, a glycosaminoglycan, and carboxymethylcellulose. No adverse or toxic effects have been described with the use of these substances. Seprafilm is commercially available in a size of 12.7 × 15.2 cm.
To evaluate the effectiveness of Seprafilm, a two-stage surgical abdominal procedure was chosen, allowing the application of the antiadhesions material at the initial surgery and the evaluation of adhesions formation at follow-up surgery. We evaluated the effectiveness of Seprafilm after the Hartmann procedure.
Age, sex, weight, height, primary clinical diagnosis, medical history, medications, and abdominal surgical history were noted at admission. Obesity was defined as a body mass index of 30 or more. Abnormalities found during physical examination were documented.
Surgery was performed according to Hartmann: the sigmoid colon was resected, a colostomy was created, and the rectal stump was closed. Documented factors related to the procedure included length of midline incision, description and length of colon segment resection, method of closure of the rectal stump, whether the omentum had been removed, and whether the peritoneum had been sutured. Duration of surgery, complications, and additional surgical procedures were also noted. If the patient was randomized to receive Seprafilm, the number of membranes applied under the midline incision and in the pelvic area was noted. In the pelvic area, the rectal stump was covered with Seprafilm. The organs directly underlying the midline incision just before closing the wound were covered as well. The surgeon was asked to state whether adhesions were present at the time of initial surgery and to score their location, extent, and type. In addition, the surgeon was asked whether the patient had peritonitis and, if so, whether the spread through the abdominal cavity was local, locoregional, or diffuse.
After surgery, wound healing was observed. A mild wound infection was defined as redness surrounding the laparotomy wound, a moderate wound infection was one that produced pus, and a severe infection was defined as wound dehiscence and wound edge necrosis. Results of the histologic examination of the resected colon were documented.
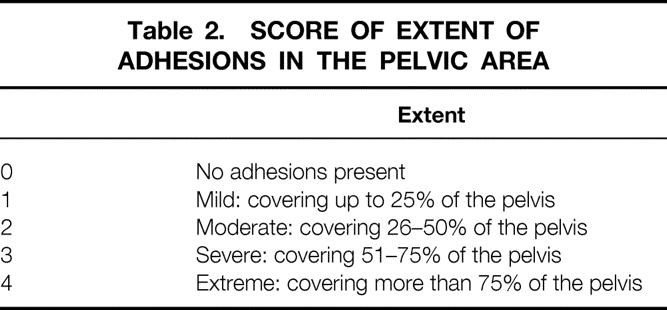
Evaluation of adhesions was performed during surgery for closure of the colostomy and reanastomosis of the rectal stump. Adhesions were assessed by a surgeon unaware of the patient’s random assignment. Evaluation of the incidence, extent, and type of adhesions in the midline was performed through laparoscopy. After mobilization and repositioning of the colostomy in the abdomen, a 10-mm trocar was inserted in the colostomy opening after partial closure. Subsequently, the abdominal cavity was insufflated. Adhesions from the midline incision to intraperitoneal sites or organs were identified and the extent and type were scored. Extent was assessed by estimating the overall length of the incision covered by adhesive tissue by palpating the skin surface along the midline incision while laparoscopically viewing the peritoneal surface of the anterior abdominal wall. The margins of the adhesions along the midline incision were demarcated on the skin surface and the corresponding incisional length was measured. The type of adhesions was determined according to Zühlke et al 20 (Table 1). If subsequent laparotomy was performed, laparoscopic findings were confirmed. Within the pelvic cavity, the incidence of adhesions was evaluated under direct vision or laparoscopically. Organs and intraperitoneal sites involved in a pelvic adhesion were scored. The extent of adhesions in the pelvis was assessed by the percentage of adhesions covering the area (Table 2) and the type was assessed according to Zühlke et al.
Table 1. MACROSCOPIC CLASSIFICATION OF ABDOMINAL ADHESIONS
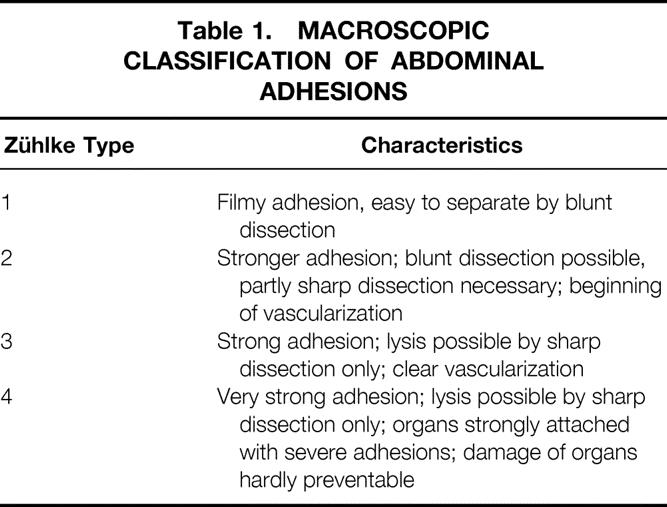
Table 2. SCORE OF EXTENT OF ADHESIONS IN THE PELVIC AREA
Evaluations were recorded on videotape, allowing postoperative masked reevaluation by two independent observers. Severity of formation of adhesions was calculated by multiplying the extent and type of adhesions for both locations. The extent of adhesions to the total midline incision was multiplied by the estimated type of adhesions, and evaluation of the pelvis was done according to the method described above.
Statistical analysis was done with SPSS (Chicago, IL) software. Percentages and continuous variables were compared using the Fisher exact test and the Mann-Whitney test. Increases in the incidence and severity of adhesions after surgery compared with the adhesions present at initial surgery were analyzed using the Wilcoxon signed rank test. The probability values given are two-sided;P = .05 was considered the limit of significance. The analysis was by intention to treat.
The protocol was approved by the Ethical Committee of the University Hospital Rotterdam, and separate approvals were obtained from the Ethical Committee of the Catharina Ziekenhuis, Eindhoven; the Diakonessehuis, Utrecht; The Reinier de Graaf Gasthuis, Delft; the Groene Hart Ziekenhuis, Gouda; the St. Clara Ziekenhuis, Rotterdam; the Merwede Ziekenhuis, Dordrecht; and the Westfries Gasthuis, Hoorn.
RESULTS
A total of 71 patients were randomized, of which 4 patients were found to be ineligible. One patient had dementia of which the surgeon was unaware, and three patients withdrew after randomization.
Of the remaining 67 patients, 32 patients were randomized to receive Seprafilm and 35 to serve as controls. In the Seprafilm group, 11 patients were lost to follow-up: 6 underwent relaparotomy within 3 weeks after initial surgery, 2 died, and 3 had concomitant disease not allowing the second-stage procedure. In the control group, 14 patients were lost to follow-up: 5 underwent relaparotomy within 3 weeks, 5 died, and 4 had concomitant disease not allowing the second-stage procedure.
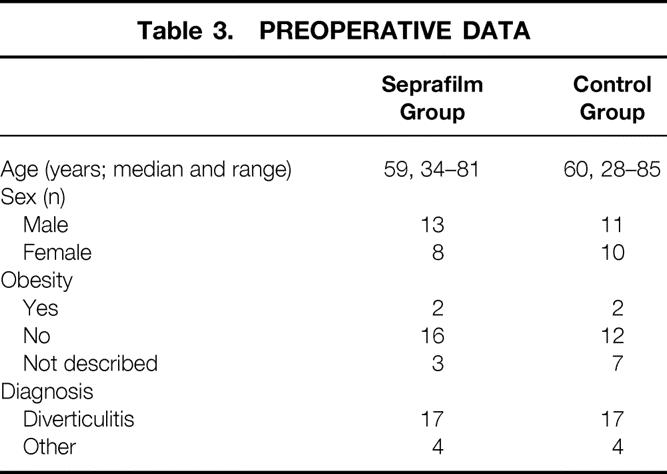
A total of 42 patients could be evaluated, 21 in the Seprafilm group and 21 in the control group. An intention-to-treat analysis was performed. Groups were comparable regarding preoperative data (Table 3). No significant differences were found regarding medical history and preoperative physical examination. Use of medication showed no differences between groups. Fourteen patients in the Seprafilm group and 15 in the control group had no history of previous abdominal surgery. No significant differences were found between the groups for frequency and type of previous abdominal surgery.
Table 3. PREOPERATIVE DATA
Intraoperative data did not differ significantly (Table 4). The resected colon segment classified as “other” in the Seprafilm group was an ileocecal resection. The procedures classified as “other” in the control group were a subtotal colectomy, a left hemicolectomy, and a colostomy for a rectovaginal fistula that had developed after a low anterior resection for a villous adenoma of the rectum. Preexisting adhesions were identified in nine patients in the Seprafilm group; five of these patients showed adhesions to the sites involved in future evaluation. Preexisting adhesions were present in five patients in the control group; three of these patients showed adhesions to the sites involved in future evaluation. These differences were not significant.
Table 4. INTRAOPERATIVE DATA
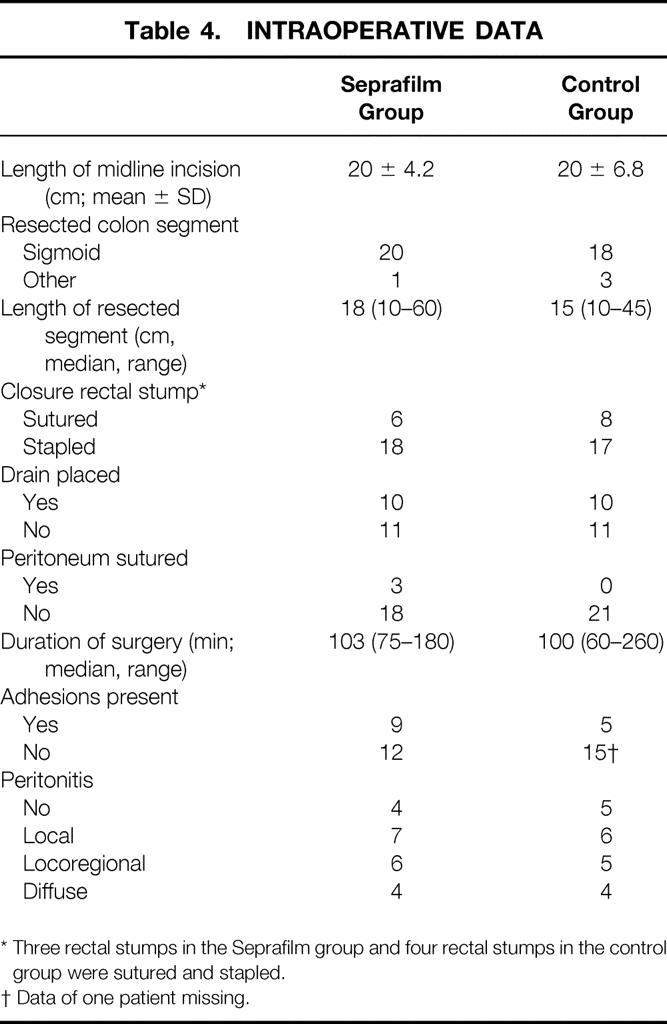
* Three rectal stumps in the Seprafilm group and four rectal stumps in the control group were sutured and stapled.
† Data of one patient missing.
One patient received three Seprafilm membranes at the midline incision, 16 patients received two membranes, and 4 patients received one membrane. The latter four patients had an incision length at initial surgery of 15, 15, 25, and 30 cm, indicating that the area under the midline incision had been only partially covered by Seprafilm. In the pelvic area, two membranes were applied in nine patients, one membrane was applied in nine patients, and no membrane was applied in three patients.
Complications consisted of three accidental bowel perforations occurring in two patients in the Seprafilm group and in one patient in the control group. Accidental injury to the bladder occurred in one patient in the control group.
Additional surgical procedures during the Hartmann procedure occurred in 14 patients. In the Seprafilm group, three patients underwent appendectomy, two patients underwent surgical decompression of the small bowel, one patient had his peritoneal dialysis catheter removed, and one patient underwent resection of an ovarian cyst and partial small bowel resection for accidental bowel perforation. In the control group, three patients underwent additional appendectomy, two patients underwent splenectomy, one patient underwent suturing of an iatrogenic bladder injury, and one patient underwent partial small bowel resection for an abscess in the mesentery. Median blood loss was 350 mL (range 10–1,200) in the Seprafilm group and 400 mL (range 50–2,000) in the control group.
Postoperative wound healing was abnormal in eight patients in the Seprafilm group and in three patients in the control group. In the Seprafilm group, four patients had a mild to moderate wound infection with redness of the wound and/or pus discharge, two patients had an abscess related to the midline incision that required drainage, and two patients showed a dehiscence; they were treated conservatively. In the control group, three patients had an abscess; two were related to the midline incision and one was related to the colostomy. The abscesses were treated with drainage. One patient with a wound infection and one patient with a dehiscence received antibiotics. Pelvic healing was abnormal in one patient in the control group; this patient appeared to have a fistula from the small bowel to the vagina that required reoperation.
In the Seprafilm group, histologic examination of the resected tissue showed diverticulitis in 16 patients and colon carcinoma in 2 patients; in 2 patients no histologic examination was performed. In the control group, histologic examination showed diverticulitis in 13 patients, colon carcinoma in 1 patient, and ischemic colitis in 1 patient; in 6 patients no histologic examination was performed.
Time between initial surgery and follow-up surgery did not differ significantly between groups. In the Seprafilm group the median interval was 5 months (range 2–16) and in the control group the median interval was 4 months (range 1–30).
A significant increase was found for both groups in the severity of adhesions at second-stage surgery compared with initial surgery, in terms of both the total midline incision (P = .007) and the pelvic area (P = .013).
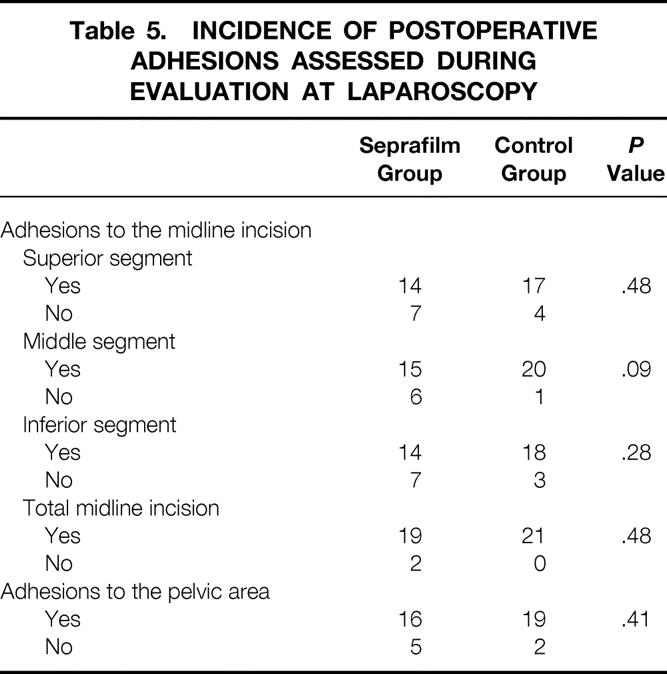
The incidence of adhesions found during evaluation did not differ significantly between the groups (Table 5).
Table 5. INCIDENCE OF POSTOPERATIVE ADHESIONS ASSESSED DURING EVALUATION AT LAPAROSCOPY
The severity of adhesions in the superior, middle, and inferior segment of the midline incision was evaluated in all patients, as well as in the pelvic area. Significant differences in severity between groups were found for the middle and inferior segment of the midline incision and the total midline incision (Fig. 1). In addition, the pelvic area showed a significant difference between groups regarding the severity of adhesions (Fig. 2). Performing a per-protocol analysis by excluding the patients from the Seprafilm group who had not received any membranes during initial surgery showed comparable figures (P = .043).
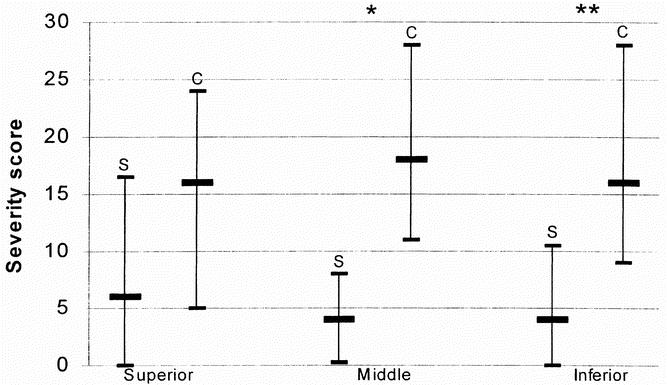
Figure 1. Severity of adhesions per site (extent by type), superior, middle, and inferior part of midline incision (median, 25 percentile, 75 percentile). S, Seprafilm group; C, control group. *P < .0001; **P = .002.
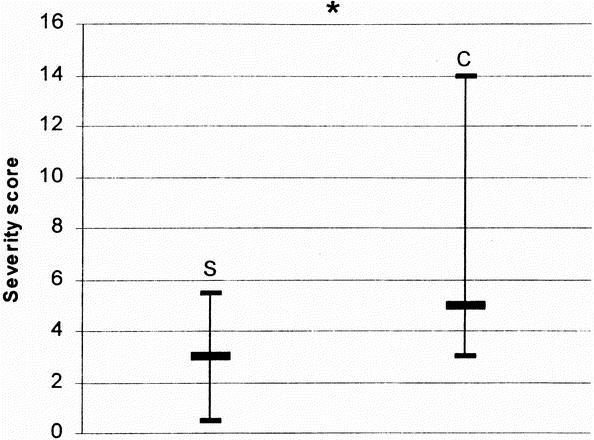
Figure 2. Severity of adhesions in the pelvis (extent by type; median, 25 percentile, 75 percentile). S, Seprafilm group; C, control group. *P = .042.
The median severity of adhesions for the total midline incision showed a significant difference: 18 (25th–75th percentile, 7–44) for the Seprafilm group and 50 (25th–75th percentile, 41–67) for the control group (P = .002).
Videotapes of the second-stage surgery were made in 26 patients, 10 in the Seprafilm group and 16 in the control group. Evaluation of adhesions to the total midline incision was possible for 10 patients in the Seprafilm group and 12 in the control group. Evaluation of adhesions in the pelvis was possible for 6 patients in the Seprafilm group and 10 in the control group. Severity score for the midline incision was 14 (25th–75th percentile, 8–25) for the Seprafilm group and 53 (25th–75th percentile, 46–66) for the control group. Severity score in the pelvis was 0 (25th–75th percentile, 0–2) in the Seprafilm group and 5 (25th–75th percentile, 2–10) in the control group. These severity scores were not significantly different from the values scored at restorative surgery by the surgeon.
DISCUSSION
Adhesions develop in the vast majority of patients after abdominal surgery 1,3,4 and may lead to complications. Assessment of the postoperative incidence, severity, and location of adhesions has not frequently been described because no noninvasive method is available. The design of the current randomized clinical study allowed evaluation of the development of adhesions after insertion of Seprafilm during a Hartmann procedure. Prevention of adhesions has been evaluated in only one other randomized study. 17
It is generally assumed that filmy adhesions lead to less complaints and complications than more dense adhesions. However, data on this subject are not available.
The severity of adhesions was significantly less in the patients who received Seprafilm compared with the group who served as controls. This finding corresponds to the results of Becker et al, 17 who performed a randomized clinical study to assess the value of Seprafilm in reducing the incidence and severity of adhesions in patients undergoing colectomy and ileal pouch–anal anastomosis with diverting-loop ileostomy and consequent ileostomy closure with laparoscopic evaluation of formed adhesions. However, Becker et al described a significant decrease in the incidence of adhesions as well, and this could not be confirmed by our results. A possible explanation for this discrepancy is that in the current study, 34 (81%) of 42 patients had peritonitis demanding emergency surgery, whereas in the study mentioned above peritonitis was not present in any patient. Peritonitis has been described as disturbing naturally present mechanisms involved in reducing the formation of adhesions, and therefore theoretically promotes the formation of adhesions. 21 As a consequence, measures aiming at the reduction of postoperative adhesions might be less effective if peritonitis were present.
Blood loss was described as having a diminishing effect on the efficacy of a cellulose barrier for reducing postoperative adhesions. 22 Becker et al 17 found no relation between blood loss and the antiadhesions effect of Seprafilm, and because blood loss was comparable between that study and the present one, blood loss is not a very likely explanation for a reduced effect of the membrane.
Theoretically, the relatively high incidence of preexisting adhesions could explain the absence of reduction of adhesion formation in the Seprafilm group. Reformation of adhesions after adhesiolysis has been described to be high, the recurrence rate possibly depending on the technique of adhesiolysis, applied antiadhesions methods, and time between initial surgery and evaluation of reformation. 8,9,23
Seprafilm is not easy to handle, and some experience is needed to apply it as intended. Application in areas that are more difficult to reach than the areas used in this study may bring about difficulties. Theoretically, dislocation is possible after application, and this may interfere with the membrane’s antiadhesions effect. To prevent dislocation of the membranes, the bowel was not held aside while closing the fascia; theoretically this could result in inadequate closure of the fascia and dehiscence, although no significant difference was found in the incidence of dehiscence between the groups. Devices that would be easier to handle would probably provide a more effective means to reduce postoperative adhesions.
This study describes only the incidence and severity of postoperative adhesions. No results are available yet about the effect of Seprafilm use on reducing the incidence of small bowel obstruction, chronic abdominal pain, and infertility. To assess these clinical parameters and determine the cost-effectiveness of Seprafilm, large studies with a long-term follow-up are needed.
In conclusion, we found a reduction in the severity of formation of adhesions after the application of Seprafilm in patients undergoing the Hartmann procedure compared with controls. Particularly in the case of planned relaparotomy, as with a Hartmann procedure, the application of Seprafilm will facilitate reexploration and may lower the risk of damaging the bowel during surgery. Therefore, it is considered advisable to use Seprafilm as an antiadhesions barrier after colorectal surgery if relaparotomy is expected.
Acknowledgments
The authors thank their data manager, Anneke G. van Duuren, for assistance.
The following local trial coordinators and clinical centers are acknowledged for enrollment and follow-up of patients: J. F. Lange, MD, PhD, St. Clara Ziekenhuis, Rotterdam; J. de Gruyl, MD, PhD, Albert Schweitzer Ziekenhuis, Dordrecht; I. M. C. Janssen, MD, Ziekenhuis Rijnstate, Arnhem; J. W. D. de Waard, MD, PhD, and M. W. C. de Jonge, MD, PhD, Westfries Gasthuis, Hoorn; and R. M. H. Wijnen, MD, Catharina Ziekenhuis, Eindhoven.
Footnotes
Correspondence: Hans Jeekel, MD, PhD, Department of General Surgery, University Hospital Rotterdam-Dijkzigt, Dr. Molewaterplein 40, 3015 GD Rotterdam, The Netherlands.
E-mail: jeekel@hlkd.azr.nl
Accepted for publication May 22, 2001.
References
- 1.Ellis H. The clinical significance of adhesions: focus on intestinal obstruction. Eur J Surg 1997; 577: 5–9. [PubMed] [Google Scholar]
- 2.Jenkins SD, Klamer TW, Parteka JJ, et al. A comparison of prosthetic materials used to repair abdominal wall defects. Surgery 1983; 94: 392–398. [PubMed] [Google Scholar]
- 3.Luijendijk RW, de Lange DC, Wauters CC, et al. Foreign material in postoperative adhesions. Ann Surg 1996; 223: 242–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menzies D, Ellis H. Intestinal obstruction from adhesions: how big is the problem? Ann R Coll Surg Engl 1990; 72: 60–63. [PMC free article] [PubMed] [Google Scholar]
- 5.Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 1999; 353: 1476–1480. [DOI] [PubMed] [Google Scholar]
- 6.Kresch AJ, Seifer DB, Sachs LB, et al. Laparoscopy in 100 women with chronic pelvic pain. Obstet Gynecol 1984; 64: 672–674. [PubMed] [Google Scholar]
- 7.Goldstein DP, de Cholnoky C, Emans SJ, et al. Laparoscopy in the diagnosis and management of pelvic pain in adolescents. J Reprod Med 1980; 251–256. [PubMed] [Google Scholar]
- 8.Operative Laparoscopy Study Group. Postoperative adhesion development after operative laparoscopy: evaluation at early second-look procedures. Fertil Steril 1991; 55: 700–704. [PubMed] [Google Scholar]
- 9.Trimbos-Kemper TC, Trimbos JB, van Hall EV. Adhesion formation after tubal surgery: results of the eighth-day laparoscopy in 188 patients. Fertil Steril 1985; 43: 395–400. [DOI] [PubMed] [Google Scholar]
- 10.Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod 1999; 14: 333–337. [DOI] [PubMed] [Google Scholar]
- 11.Mecke H, Heuchmer R, Lehmann-Willenbrock E. [Complications in 5,000 pelviscopies at the Kiel University Gynecologic Clinic]. Geburtshilfe Frauenheilkd 1996; 56: 449–452. [DOI] [PubMed] [Google Scholar]
- 12.Jeekel H. Cost implications of adhesions as highlighted in a European study. Eur J Surg Suppl 1997; 579: 43–45. [PubMed] [Google Scholar]
- 13.Wilson MS, Hawkswell J, McCloy RF. Natural history of adhesional small bowel obstruction: counting the cost. Br J Surg 1998; 85: 1294–1298. [DOI] [PubMed] [Google Scholar]
- 14.Ray NF, Larsen JW Jr, Stillman RJ, Jacobs RJ. Economic impact of hospitalizations for lower abdominal adhesiolysis in the United States in 1988. Surg Gynecol Obstet 1993; 176: 271–276. [PubMed] [Google Scholar]
- 15.Ray NF, Denton WG, Thamer M, et al. Abdominal adhesiolysis: inpatient care and expenditures in the United States in 1994. J Am Coll Surg 1998; 186: 1–9. [DOI] [PubMed] [Google Scholar]
- 16.Raftery AT. Regeneration of parietal and visceral peritoneum: an electron microscopical study. J Anat 1973; 115: 379–392. [PMC free article] [PubMed] [Google Scholar]
- 17.Becker JM, Dayton MT, Fazio VW, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg 1996; 183: 297–306. [PubMed] [Google Scholar]
- 18.Beck DE, Opelka FG, Bailey HR, et al. Incidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum 1999; 42: 241–248. [DOI] [PubMed] [Google Scholar]
- 19.Nieuwenhuijzen M, Reijnen MM, Kuijpers JH, van Goor H. Small bowel obstruction after total or subtotal colectomy: a 10-year retrospective review. Br J Surg 1998; 85: 1242–1245. [DOI] [PubMed] [Google Scholar]
- 20.Zühlke HV, Lorenz EMP, Straub EM, Savvas V. Pathophysiologie und Klassifikation von Adhäsionen. Langenbecks Arch Chir Suppl II Verh Dtsch Ges Chir 1990; 345: 1009–1016. [PubMed] [Google Scholar]
- 21.Holmdahl L. The role of fibrinolysis in adhesion formation. Eur J Surg 1997; 577: 24–31. [PubMed] [Google Scholar]
- 22.Interceed (TC7) Adhesion Barrier Study Group. Prevention of postsurgical adhesions by Interceed (TC7), an absorbable adhesion barrier: a prospective, randomized multicenter clinical study. Fertil Steril 1989; 51: 933–938. [PubMed] [Google Scholar]
- 23.Diamond MP, Daniell JF, Martin DC, et al. Tubal patency and pelvic adhesions at early second-look laparoscopy following intraabdominal use of the carbon dioxide laser: initial report of the intraabdominal laser study group. Fertil Steril 1984; 42: 717–723. [DOI] [PubMed] [Google Scholar]


