Abstract
Objective
To review a single-center experience with 201 multivisceral resections for primary colorectal cancer to determine the accuracy of intraoperative prediction of potential curability, to identify prognostic factors, and to examine the effect of surgical experience on immediate outcome and long-term results.
Summary Background Data
Locally advanced colorectal cancer may require an intraoperative decision for en bloc resection of surrounding organs or structures to achieve complete tumor removal. This decision must weigh the risk of complications and death of multivisceral resection against a potential survival benefit. Little is known about prognostic factors and the influence of surgical experience on the outcome of multivisceral resection for colorectal cancer.
Methods
Patients undergoing multivisceral resection for primary colon or rectal cancer between 1982 and 1998 were identified from a prospective database. Patients were followed up according to a standard protocol.
Results
Multivisceral resection was performed in 201 of 2,712 patients with a median age of 64 years. Postoperative rates of complications and death in 201 patients were 33% and 7.5%, respectively. A potentially curative resection was possible in 130 of 201 patients (65%) and histologic tumor infiltration was shown in 44% of patients with curative resection. Intraoperative assessment of curability was unreliable. After curative resection, the local recurrence rate was 11% and the overall 5-year survival rate was 51%. Multivariate analysis identified intraoperative blood loss (relative risk 1.7–6.4, P < .001), age 64 years or older (RR 3.7;P < .001), and UICC stage as independent prognostic factors (RR 2.0;P = .009). No prognostic significance was found for histologic tumor infiltration, the number of resected organs, or surgical experience.
Conclusions
Multivisceral resection is safe, and long-term survival after curative resection is similar to that after standard resection. Because palliative resections cannot be predicted accurately at the time of surgery, every effort should be made to achieve complete tumor resection. Major blood loss but not surgical experience per se is an independent prognostic factor.
Until 50 years ago, colorectal carcinoma appearing to infiltrate surrounding tissue was considered nonresectable. 1 Since then, extensive surgical procedures have been performed aimed at complete resection of locally advanced primary colorectal carcinoma. Results from several small series indicated that multivisceral en bloc resection of locally advanced tumors results in cure in many patients. 2,3 Undoubtedly such operations are demanding for both patient and surgeon, and the associated risks of complications and death must be weighed against a potential survival benefit.
The decision to perform a multivisceral resection for primary colorectal carcinoma is usually made at the time of surgery, because the need for multivisceral resection is rarely recognized before surgery. In this situation it is important to evaluate the accuracy with which curative or palliative outcome of the treatment can be predicted during surgery. It may also be speculated that surgical expertise has a major impact on the success of such complex procedures.
Few series have included sufficient patients to allow a meaningful analysis of prognostic factors, 4,5 and no attempt has yet been made to evaluate surgical experience as a potential prognostic factor in multivisceral resections. Therefore, we reviewed our experience with 201 multivisceral resections for primary colorectal cancer to determine the accuracy of intraoperative prediction of potential curability, to identify prognostic factors, and to examine the effect of surgical experience on immediate outcome and long-term results.
PATIENTS AND METHODS
Between 1982 and 1998, clinical and pathologic data of the primary tumor and follow-up information of all patients undergoing treatment for adenocarcinoma of the colon or rectum at the Department of Surgery, University of Heidelberg, were entered into a prospective database.
Imaging studies to determine local tumor infiltration were not routinely performed for colon cancer, and preoperative assessment by computed tomography or endosonography for rectal tumors became standard practice only later in the series. Resection for colorectal cancer was performed using the no-touch isolation technique with primary ligation of the draining lymphovascular bundle. The UICC classification of 1992 was used to categorize pathohistologic and clinical data.
Multivisceral resection was defined as en bloc removal of any organ or structure to which the primary tumor was adherent. Intraoperative frozen section to determine the extent of resection was discouraged to avoid tumor contamination. Emergency treatment was defined as colorectal resection within 24 hours of admission. Removal of unattached organs such as liver resection for hepatic metastases, cholecystectomy for symptomatic gallbladder disease, splenic resection for iatrogenic injury, or resection of synchronous tumors was not considered multivisceral resection for the purpose of this study.
Experience of the surgeons was classified as low or high depending on whether a particular surgeon had performed 15 or more multivisceral resections. 6 The assessment as to whether the operation was potentially curative or palliative was made at the end of the operation without knowledge of the final histology.
All patients were followed up according to a standard protocol including colonoscopy, abdominal ultrasound, chest radiography, and tumor marker studies in our outpatient clinic or by the family physician. If the most recent outpatient visit dated back more than 3 months, current follow-up information was obtained from the patient or the patient’s physician by telephone.
Data were analyzed using SAS statistical software (Release 6.12, SAS Institute Inc., Cary, NC). Patient characteristics were compared by the two-tailed Fisher exact test or by the chi-square test with Yates correction where appropriate. Quantitative variables are expressed as median and interquartile range (IQR). Multiple logistic regressions were performed to identify factors associated with an intraoperative blood loss of 1,000 mL or more. The distribution of quantitative variables between subgroups of patients was compared by the Mann-Whitney test. Overall survival from the date of large bowel resection was calculated by the Kaplan-Meier estimate. Patients alive at the last follow-up were censored, as were two patients lost to follow-up after 72 and 96 months, respectively. The univariate associations between clinicopathologic variables and overall survival were examined by the log-rank test. Factors independently associated with overall survival were identified by proportional hazard regression analysis (Cox model). Stepdown regression was used to build a parsimonious statistical model for the association of prognostic factors with overall survival among patients with complete data Fig 1.

Figure 1. Location of colorectal cancer treated by multivisceral resection (n = 201).
RESULTS
Sex and Age
Between 1982 and 1998, 2,712 patients were treated for primary colorectal carcinoma. T3 or T4 tumors were diagnosed in 1,948 patients with a median age of 66 years (IQR 57–74). Colon cancer was present in 1,213 patients and rectal cancer in 735 patients. Two hundred one patients (139 colon cancer, 62 rectal cancer) underwent multivisceral resection for suspected local tumor infiltration (Fig. 1). Median age in this group was 64 years (IQR 54–72). The male:female ratio was 1.4 for all 1,948 patients and 0.83 for patients undergoing multivisceral resection. During the past 17 years the percentage of patients undergoing multivisceral resection has increased steadily from 6.9% to 12.2% and more than tripled in absolute numbers (Table 1).
Table 1. MULTIVISCERAL RESECTION 1982–1998: COLON AND RECTUM (ONLY pT3 AND pT4)

* Excludes nine pT2 tumors.
Surgical Treatment
Ileus or perforation necessitated emergency treatment in 27 of the 201 patients. This concerned mainly patients with colon cancer (24 of 139 patients [17%]) and rarely rectal cancer (3 of 62 patients [5%];P = .023). A total of 341 additional organs or surrounding structures were resected together with the malignant tumor in 201 patients (Table 2). The most frequently removed organs were small bowel (29% of patients) and urinary bladder (24%). Median operative time was 180 minutes (IQR 150–240) for colon cancer and 260 minutes (IQR 210–360) for rectal cancer (P < .001).
Table 2. ADJACENT ORGANS RESECTED AND TUMOR INFILTRATION: COLON AND RECTUM
Multimodal Therapy
During the entire observation period, 40 of 130 patients undergoing curative surgery received some form of adjuvant or neoadjuvant treatment. Notably, only 15 patients with colon cancer were treated by adjuvant 5-fluorouracil-based chemotherapy; one patient each received neoadjuvant radiotherapy or chemotherapy. Neoadjuvant treatment was administered more frequently to patients with rectal cancer. Seven patients were treated by radiochemotherapy and two by radiotherapy only. Fourteen patients with rectal cancer received adjuvant therapy (radiotherapy in six, radiochemotherapy in six, and chemotherapy alone in two).
Blood Loss and Transfusion
Median intraoperative blood loss was 600 mL (IQR 400–1,000) for colon cancer and 1,500 mL (IQR 700–2,300) for rectal cancer (P < .001). A total of 141 patients (70%) required transfusion. Operations with resection of two or more organs were associated with a significantly increased blood loss (median 1,200 mL, IQR 500–2,000) compared with operations with one resected organ (median 600 mL, IQR 400–1,000;P < .001). At a cutoff volume of 1,000 mL, tumor location and the number of resected organs were independently associated with intraoperative blood loss on multivariate analysis. Surgical experience, patient age, histologically confirmed organ infiltration, and UICC stage were not significantly related to blood loss.
Complications
In colon cancer, 39 of 139 (28%) patients had postoperative complications (Table 3). Twenty patients had surgical and 19 patients had nonsurgical complications. In rectal cancer, postoperative complications were recorded in 28 of 62 patients (45%). Fourteen patients each had surgical and nonsurgical complications. There was no significant difference in surgical complication rates between patients with colon or rectal cancer, but the overall complication rate was greater in patients with rectal cancer (45 vs. 28%;P = .018). The postoperative complication rate was also greater after emergency operations (16/27 [59%]) compared with elective multivisceral resections (51/174 [29%];P = .002). The postoperative complication rates of potentially curative and palliative operations were not significantly different (32 vs. 34%;P = .87).
Table 3. POSTOPERATIVE DEATH AND COMPLICATION RATES: COLON AND RECTUM

Deaths
Fifteen of 201 patients died after surgery (7.5%). Causes of death were septic complications in five patients and hemorrhage in one patient. Nine patients died of general medical illness (cardiac insufficiency in four patients, tumor cachexia in two patients, and pneumonia, cerebral bleeding, and pulmonary embolism in one patient each). Four of the five patients with septic complications died subsequent to an anastomotic leak, and one patient presenting with perforation died of primary peritonitis. The death rate was greater in patients with colon cancer compared with those with rectal cancer (9.4 vs. 3.2%;P = .016). Six of 27 patients died after emergency surgery (22%) compared with 9 of 174 after elective surgery (5.2%;P = .007).
Accuracy of Intraoperative Assessment
Because the final decision for multivisceral resection must be made at the time of laparotomy, the accuracy of intraoperative assessment of potential curability is of prime importance. In most patients the intraoperative assessment was confirmed by postoperative pathohistologic evaluation and staging (Table 4). However, pathohistologic examination showed clear margins in 11 of the 63 specimens (17%) in which the surgeon considered tumor resection to be incomplete. The accuracy of predicting a potentially curative operation was similar for colon (86%) and rectum (84%) cancer, for an overall accuracy rate of 85%. The positive predictive value for potential curability was 86%. Perhaps more importantly, the diagnosis of a palliative resection was unreliable, with a negative predictive value of only 83% for all patients. This confirms that intraoperative assessment should rarely be used to exclude a patient from multivisceral resection with curative intent and that every effort should be made to resect macroscopically invasive tumors completely.
Table 4. INTRAOPERATIVE ASSESSMENT OF CURABILITY AND PATHOHISTOLOGICAL EVALUATION: COLON AND RECTUM
Pathohistologic Findings
Tumor infiltration was detected in 116 of 341 resected organs (34%) and in 100 of 201 patients undergoing multivisceral resection (50%). In colon cancer, the most frequently infiltrated organs were small bowel and bladder (see Table 2). The abdominal wall, although frequently suspected of tumor infiltration, was histologically infiltrated in only 3 of 28 patients. In rectal cancer, the most frequently infiltrated organs were small bowel, uterus, vagina, and bladder. Suspected infiltration was histologically confirmed in half of the patients. After surgery, treatment was considered potentially curative in 130 patients, and 33% of patients were UICC stage IV (Table 5). Tumor resection was incomplete in 71 patients, and incomplete resection of the primary was the only site of residual tumor in 25 of 201 patients (12%).
Table 5. POSTOPERATIVE UICC CLASSIFICATION: COLON AND RECTUM

Surgical Experience
The success of complex procedures such as multivisceral resections should depend on the expertise of the surgeon. Between 1982 and 1998, 201 multivisceral resections were performed by 29 surgeons. Four of the 29 surgeons performed 15 or more operations each and were, therefore, designated as “experienced.” These four surgeons were responsible for 106 operations altogether (53%). No significant differences were found between “experienced” and other surgeons regarding the proportion of curative operations, intraoperative blood loss, postoperative complications, and long-term survival.
Follow-Up
Two patients were lost to follow-up immediately after surgery and were therefore excluded from survival analysis. Median follow-up is 71 months (confidence interval 59–86) with a minimum follow-up of 5 months for patients still alive. A total of 117 patients have died of tumor-related causes and 8 have died from unrelated causes. Seventy-four patients are alive, and 64 of them are free of disease.
Site of Recurrence
The site of first recurrence in 81 patients with colon cancer surviving a potentially curative operation was distant metastasis in 13 patients, local recurrence in 4, and both distant and local recurrence in another 3. The median time to recurrence was 16 months (IQR 10–24). In 11 of 38 patients with rectal cancer, the median time to recurrence was 7 months (IQR 5–16). Five patients developed distant metastases, one a local recurrence, and five both. The local recurrence rate was therefore 9% for colon cancer and 16% for rectal cancer (overall 11%).
Overall Survival
Overall survival was determined by residual tumor after multivisceral resection (P < .001;Fig. 2). No patient with residual tumor (R1 or R2) survived for 5 years. For patients with curative resection, overall survival was compared by stage and location with the overall survival of patients treated during the same time interval with similar pathologic tumor stage, but not requiring multivisceral resection (Table 6). Survival after multivisceral resection was worse for every tumor location and for every stage compared with patients not treated by multivisceral resection, but this appeared to be related to early postoperative deaths (Fig. 3;P = .14). Univariate analysis determined organ infiltration (Fig. 4;P = .041), UICC stage (Fig. 5;P = .001), intraoperative blood loss (Fig. 6;P < .001), lymphatic invasion (Fig. 7;P = .002), and age (P < .001) to be significant prognostic factors. Experience of the surgeon, number of resected organs, blood transfusion, and emergency operation were not related to survival in curatively operated patients (Table 7). Multivariate analysis was performed in 122 patients undergoing potentially curative surgery. Only blood loss, age, and UICC stage were identified as independent prognostic factors (Table 8). Local tumor infiltration as opposed to inflammatory infiltration was not an independent prognostic factor on multivariate analysis.

Figure 2. Overall survival after multivisceral resection.
Table 6. OVERALL 5-YEAR SURVIVAL AFTER R0 RESECTION BY STAGE AND LOCATION: COLON AND RECTUM T3 AND T4 TUMORS ONLY


Figure 3. Overall survival after conventional versus multivisceral R0 resection (only T3/T4 tumors).

Figure 4. Overall survival after multivisceral R0 resection.

Figure 5. Overall survival after multivisceral R0 resection.
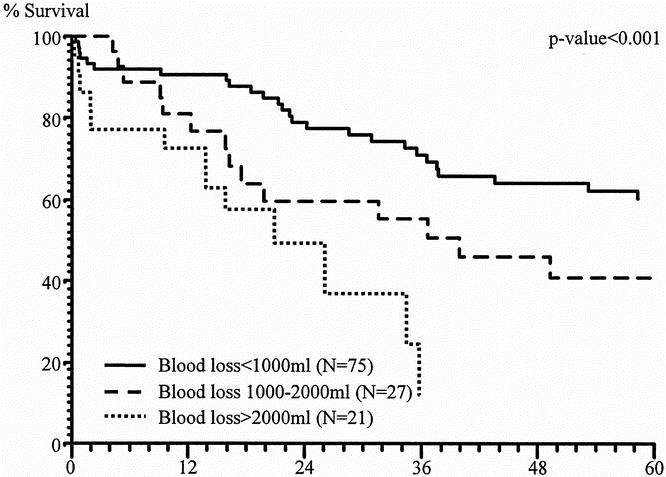
Figure 6. Overall survival after multivisceral R0 resection.

Figure 7. Overall survival after multivisceral R0 resection.
Table 7. UNIVARIATE ANALYSIS OF PROGNOSTIC FACTORS FOR OVERALL SURVIVAL AFTER R0 RESECTION

Table 8. MULTIVARIATE ANALYSIS OF PROGNOSTIC FACTORS FOR OVERALL SURVIVAL: COLON AND RECTUM

DISCUSSION
In our experience, the proportion of patients with colorectal cancer treated by multivisceral resection has increased during the past 15 years, and multivisceral resections are now performed in more than 10% of all patients with primary colon or rectal carcinoma (see Table 1). Multivisceral resection is planned before surgery in only a minority of patients; the decision to extend the resection to include surrounding organs or structures is made during surgery in most instances.
True tumor infiltration to surrounding tissue was shown pathohistologically in 43% to 70% of patients, whereas only inflammatory changes were found in the remaining patients (Table 9). This has led some to suggest dissecting the colon free from an organ that appears macroscopically infiltrated, extending the operation only if such separation is not feasible. 7 When this concept was followed, the local recurrence rate was 26% and the 5-year survival rate was only 30% in 35 patients, 7 probably because dissection caused dissemination of tumor cells. Others have confirmed a detrimental effect of intraoperative incision of the tumor on recurrence rates. Local recurrence rates were exceedingly high when adherent organs were separated from the tumor (69 vs. 18%). 8 After inadvertent dissection or rupture of the tumor, the 5-year survival rate was only 17%, compared with 49% after complete en bloc resection. 9 This was confirmed in a subsequent study by the German Colorectal Cancer Study Group, when intraoperative tumor cell dissemination resulted in a 5-year survival rate of 19% and 21% for colon and rectal cancer, respectively, even if the tumor could be completely resected, in contrast to a 5-year survival rate of 49% to 53% if spillage was avoided by en bloc resection. 10 Frozen section to identify local infiltration is not helpful in this situation. 8 Any attempt to dissect a macroscopically infiltrating tumor from its surroundings is, therefore, strongly discouraged.
Table 9. MULTIVISCERAL RESECTION FOR COLORECTAL CANCER: SURVEY OF STUDIES REPORTING 5-YEAR SURVIVAL RATES FOR CURATIVELY RESECTED PATIENTS
Before deciding on a major operation, its potential benefits are weighed against its hazards. In a survey of six studies, postoperative complication rates have been recorded as 20% to 42%, but the perioperative death rate appears quite acceptable at a median of 5% (range 3–13%; see Table 9). In recent large studies, the 5-year survival rate has consistently been reported as 51% to 52% after multivisceral resection if all tumor is removed. 10–13 Our analysis confirms that overall survival of lesions treated by multivisceral resection is similar to that of tumors not requiring resection of additional organs, if complete resection is accomplished.
In addition to this relatively favorable general outlook, an individual risk assessment could support the decision to perform a major cancer operation. To date, two studies have examined prognostic factors after potentially curative multivisceral resection by multivariate analysis. 5,14 Lymph node status was the only factor significantly related to survival. However, because lymph node status can be determined only after surgery, this does not aid in the decision for or against a major operation.
In accordance with previous studies, we identified lymph node status as a significant independent predictor of survival, and we could not attribute prognostic significance to whether the tumor was truly infiltrating adjacent organs. 14 In contrast to the other two studies, 5,14 we identified age (64 years or older) as a significant risk factor. Most importantly, however, we found intraoperative blood loss to be the strongest predictor of long-term survival, with a more than sixfold increase in risk if blood loss exceeded 2 L (see Table 8). This factor was not examined by other studies performing multivariate analyses and may, therefore, have gone unrecognized. The transfusion of blood had no effect on survival (see Table 7).
Several reports have stressed that individual surgical training, experience, and practice are important factors related to the prognosis of colorectal surgery. 15–18 Somewhat unexpectedly, our analysis did not show a beneficial effect of surgical experience on long-term survival. We then hypothesized that surgical experience could have translated into lower blood loss and therefore did not attain prognostic significance itself. Intraoperative blood loss, however, was determined by tumor location and the number of resected organs, but it was not significantly associated with surgical experience. It would seem, therefore, that the use of standardized surgical procedures by all surgeons and the overall high hospital volume of colorectal surgery (see Table 1) 18 reduced the impact of the individual surgeon variation on long-term outcome.
Footnotes
Correspondence: Thomas Lehnert, MD, Section of Surgical Oncology, Department of Surgery, University of Heidelberg, Im Neuenheimer Feld 110, D-69120 Heidelberg, Germany.
E-mail: thomas_lehnert@med.uni-heidelberg.de
Accepted for publication May 22, 2001.
References
- 1.Sugarbaker ED. Coincident removal of additional structures in resections for carcinoma of the colon and rectum. Ann Surg 1946; 123: 1036–1046. [PubMed] [Google Scholar]
- 2.Bonfanti G, Bozzetti F, Doci R, et al. Results of extended surgery for cancer of the rectum and sigmoid. Br J Surg 1982; 69: 305–307. [DOI] [PubMed] [Google Scholar]
- 3.Devine R, Dozois R. Surgical management of locally advanced adenocarcinoma of the rectum. World J Surg 1992; 16: 486–489. [DOI] [PubMed] [Google Scholar]
- 4.Curley SA, Carlson GW, Shumate CR, et al. Extended resection for locally advanced colorectal carcinoma. Am J Surg 1992; 163: 553–559. [DOI] [PubMed] [Google Scholar]
- 5.Rowe VL, Frost DB, Huang S. Extended resection for locally advanced colorectal carcinoma. Ann Surg Oncol 1997; 4: 131–136. [DOI] [PubMed] [Google Scholar]
- 6.Hermanek P, Mansmann U, Staimmer D, et al. The German experience: The surgeon as a prognostic factor in colon and rectal surgery. Surg Clin North Am 2000; 9: 33–49. [PubMed] [Google Scholar]
- 7.Montesani C, Ribotta G, De Milito R, et al. Extended resection in the treatment of colorectal cancer. Int J Colorectal Dis 1991; 6: 161–164. [DOI] [PubMed] [Google Scholar]
- 8.Hunter JA, Ryan JA, Schultz P. En bloc resection of colon cancer adherent to other organs. Am J Surg 1987; 145: 67–71. [DOI] [PubMed] [Google Scholar]
- 9.Gall FP, Tonak J, Altendorf A. Multivisceral resections in colorectal cancer. Dis Colon Rectum 1987; 30: 337–341. [DOI] [PubMed] [Google Scholar]
- 10.Hermanek P. Multiviscerale Resektion beim kolorektalen Karzinom—Erfahrungen der SGKRK-Studie. Langenbecks Arch Chir 1992; 377: 95–100. [PubMed] [Google Scholar]
- 11.Gebhard C, Meyer W, Ruckriegel S, Meier U. Multivisceral resection of advanced colorectal carcinoma. Langenbecks Arch Surg 1999; 384: 194–199. [DOI] [PubMed] [Google Scholar]
- 12.Heslov SF, Frost DB. Extended resection for primary colorectal cancer involving adjacent organs or structures. Cancer 1988; 62: 1637–1640. [DOI] [PubMed] [Google Scholar]
- 13.Reiner G, Teleky B, Wunderlich M, Schiessel R. Die Organerweiterung bei der Resektion colorektaler Carcinome. Langenbecks Arch Chir 1987; 371: 281–290. [DOI] [PubMed] [Google Scholar]
- 14.Poeze M, Houbiers JGA, van de Velde CJH, et al. Radical resection of locally advanced colorectal cancer. Br J Surg 1995; 82: 1386–1390. [DOI] [PubMed] [Google Scholar]
- 15.Holm T, Johansson H, Cedermark B, et al. Influence of hospital- and surgeon-related factors on outcome after treatment of rectal cancer with or without preoperative radiotherapy. Br J Surg 1997; 84: 657–663. [PubMed] [Google Scholar]
- 16.Porter GA, Soskolne CL, Yakimets WW, et al. Surgeon-related factors and outcome in rectal cancer. Ann Surg 1998; 227: 157–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of patient care. J Clin Oncol 2000; 18: 2327–2340. [DOI] [PubMed] [Google Scholar]
- 18.Harmon JW, Tang DG, Gordon TA, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann Surg 1999; 230: 404–413. [DOI] [PMC free article] [PubMed] [Google Scholar]





