Abstract
Objective
To identify the incidence and outcomes of emergent and semiemergent intubations in hospitalized trauma patients with cervical fractures and/or dislocations treated with halo fixation.
Summary Background Data
Intubating a trauma patient in halo fixation can be extremely difficult, with the potential for dire consequences.
Methods
The authors retrospectively reviewed the medical records of trauma patients with cervical injuries requiring halo fixation admitted to a level 1 trauma center between January 1992 and January 1997. The in-hospital need for emergent or semiemergent intubation was assessed and correlated with a variety of patient characteristics, including outcome.
Results
Of the 105 patients identified, 14 (13%) required an emergent or semiemergent intubation. Injury Severity Score, cardiac history, and intubation on arrival were significant indicators of the need for an in-hospital emergent or semiemergent intubation or reintubation. A total of seven deaths were reported, six of which were associated with an emergent or semiemergent in-hospital intubation. Although age did not appear significant in predicting the need for an emergent intubation, it was significant in predicting arrest-related deaths. A total of 17 tracheostomies were performed. Eight were considered “initial” in that they were performed before an emergent intubation, and nine were performed after an emergent intubation. Patients in the initial tracheostomy group did not differ in terms of the variables investigated from those who required an emergent intubation. None of the patients who underwent initial tracheostomy, however, had an airway emergency or died.
Conclusions
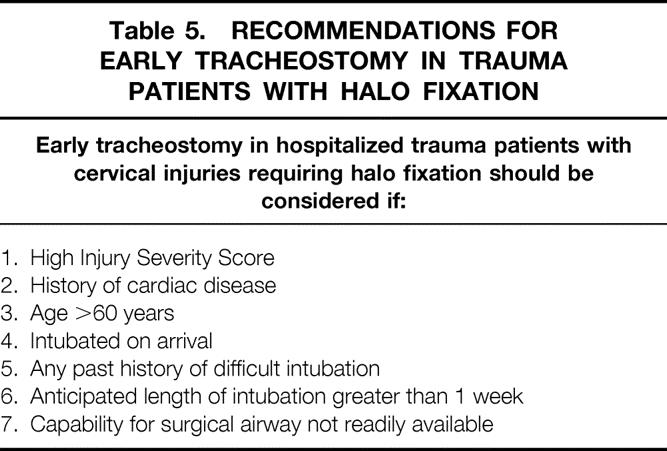
A significant number of trauma patients treated with halo fixation ultimately require an in-hospital emergent or semiemergent intubation. Given the difficulty and potential lethality associated with these intubations, heightened vigilance regarding the airway is warranted. The authors recommend that early tracheostomy be considered in patients with a history of cardiac disease, especially when a high Injury Severity Score is present. Older patients (older than 60 years) are more at risk for arrest-related death and may also benefit from early tracheostomy.
The incidence of cervical spine injuries in trauma patients ranges from 1.2% to 24% in the United States. 1–3 The vast majority of these patients can be initially managed with axial stabilization and oral intubation if necessary. 4 Cervical injuries requiring halo stabilization present a significant airway management challenge. By design, the halo device projects from the shoulders and holds the head in rigid fixation with four metallic struts and a metallic “halo” affixed to the skull with bolts. 5 This cumbersome device prevents easy access to the patient’s airway and also prevents extension of the head, a maneuver that can aid with laryngeal visualization. In the nonemergent setting, fiberoptic bronchoscopy can help overcome the difficulties of intubating these patients, 6 but in the emergent setting, these intubations can be extremely difficult.
To date, there are no published data regarding the incidence and outcomes of emergent intubations in hospitalized trauma patients treated with halo fixation. This retrospective review investigates emergent and semiemergent intubations of hospitalized trauma patients with cervical injuries treated with halo fixation and attempts to identify patient characteristics on arrival that may predict the need for these intubations.
METHODS
The records of patients admitted to the trauma registry at a level 1 trauma center between January 1992 and January 1997 were retrospectively reviewed. One hundred thirty-one patients with cervical fractures and/or dislocations requiring halo stabilization were identified. To ensure treatment consistency, 26 patients who presented more than 24 hours after their injury were excluded. Charts (n = 105) were reviewed for the in-hospital need for emergent or semiemergent intubation. An intubation was considered emergent if it occurred immediately and was part of a documented arrest or “code blue.” An intubation was considered semiemergent if it was described in the medical record as urgent, semiurgent, or semiemergent. Intubations that occurred en route or as part of the initial emergency room evaluation were categorized as “intubated on arrival.” Patients who were intubated on arrival but then extubated during their hospital stay were included in the emergent/semiemergent intubation category if they required an emergent/sem-emergent reintubation. The need for emergent or semiemergent intubation was correlated with patient characteristics including age, sex, Glasgow Coma Score (GCS), Injury Severity Score (ISS), mechanism of injury, intubation status during initial emergency room evaluation, level and extension of cervical fracture/dislocation, cord involvement, evidence of thoracic trauma, presence of retropharyngeal hematoma on radiographic studies, cardiac history (e.g., coronary artery disease), respiratory history (e.g., asthma), evidence of cerebral injury on radiographic studies, and patient outcome. Patients who died as a result of withdrawing care were excluded from outcome analysis. Data were analyzed using standard statistical methods including the Student t test, the Fisher exact test, and forward step-wise logistic regression. Ordinal data were reported as the mean ± standard error of the mean. Results were considered significant at P < .05.
RESULTS
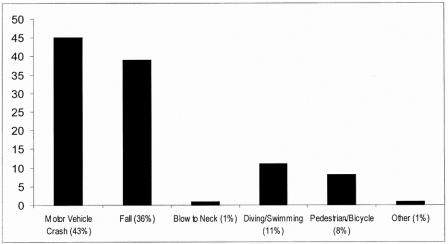
Sixty-one men (58%) and 44 women (42%) ranging from 8 to 94 years were included in this study (Table 1). ISS was 4 to 42 (mean 12.2 ± 8.7). Most of the patients (n = 95) presented with a GCS of 13 to 15. Most injuries were sustained either in motor vehicle crashes (43%) or in falls (36%) (Fig. 1). The most common fracture/dislocation occurred at C2 (44%) (Table 2), although 41 patients (39%) had more than one vertebrae involved. Eighteen patients (17%) presented with temporary or permanent spinal cord involvement, primarily occurring at C4 (n = 3), C5 (n = 9), and C6 (n = 4). Thirty patients (29%) were intubated on arrival and were subsequently placed in halo fixation. Sixteen patients (15%) had concomitant chest trauma (e.g., required thoracostomy tube, had multiple rib fractures, or had a large contusion on chest radiograph). Sixteen patients presented with a retropharyngeal hematoma on radiographic evaluation (15%), and 20 patients (19%) had evidence of cerebral injury by computed tomography. Nine patients (9%) presented with a history of respiratory disease (e.g., asthma), and 21 patients (20%) had a history of cardiac disease (e.g., coronary artery disease, prior myocardial infarction, arrhythmia, or history of cardiac surgery).
Table 1. DEMOGRAPHICS

Figure 1. Mechanism of injury.
Table 2. PATIENT CHARACTERISTICS

Intubation on arrival (P < .05), ISS (P < .01), and history of cardiac disease (P < .01) emerged as significant indicators of the need for in-hospital emergent or semiemergent intubation (Table 3). Neurologic status and GCS scores were not significant in predicting the need for intubation. Both age (P < .05) and a history of cardiac disease (P < .01) were important in predicting arrest-related deaths (Table 4).
Table 3. COMPARISON OF PATIENTS REQUIRING EMERGENT/SEMIEMERGENT INTUBATION WITH THOSE WHO DID NOT

Fisher exact test, Student t test, forward linear stepwise regression;P < .05 considered significant.
Table 4. COMPARISON OF PATIENTS WHO DIED WITH THOSE WHO DID NOT

Fisher exact test and Student t test;P < .05 considered significant.
Of the 105 patients, 30 were intubated on arrival (Table 5). Of these 30 patients, 8 underwent tracheostomy without a trial of extubation, 19 were later extubated, and 3 were intubated but required emergent reintubation secondary to mucus plugging or tube misplacement. Patients were extubated by the attending trauma surgeon or surgical intensivist using clinical judgment and standard guidelines (e.g., spontaneous respiratory rate < 25, minimal support settings, Fio2 < 0.5, Pao2 > 80 mm Hg). Six of 19 extubated patients (31.6%) later required an emergent or semiemergent reintubation. Of the 75 patients not intubated on arrival, 5 ultimately required an emergent or semiemergent intubation.
Table 5. RECOMMENDATIONS FOR EARLY TRACHEOSTOMY IN TRAUMA PATIENTS WITH HALO FIXATION
In this series, 14 of the 105 patients (13%) required emergent or semiemergent intubation or reintubation. Most patients (10/14) had a GCS of 14 or more. The ISS ranged from 9 to 29. The level of cervical injury level varied and was not predictive. Only 4 of the 14 patients had spinal cord involvement from their cervical injuries (C4–C6) (Table 6). Nine of these 14 patients were originally intubated on arrival. A total of seven deaths were reported, six of which were associated with an emergent or semiemergent intubation. Four deaths occurred during the code and two occurred several days later after a diagnosis of hypoxic brain injury.
Table 6. DEMOGRAPHICS OF PATIENTS WHO REQUIRED AN EMERGENT/SEMIEMERGENT INTUBATION
ISS, Injury Severity Score; GCS, Glasgow Coma Scale score; mva, motor vehicle accident.
A total of 17 tracheostomies were performed (Table 7). Eight of these were considered “initial” in that patients in this group were intubated and then converted to tracheostomy without a trial of extubation. The remaining nine tracheostomies were performed after an emergent or semiemergent intubation and were considered “delayed.” Six of the nine patients in the delayed tracheostomy group had been previously intubated. Patients who underwent initial tracheostomy did not differ in terms of the variables investigated from those who required an emergent or semiemergent intubation. None of the patients who underwent an initial tracheostomy went on to develop a respiratory arrest or to die.
Table 7. OUTCOME ANALYSIS

* Excludes patient allowed to expire per family’s request.
DISCUSSION
Early halo immobilization is a common practice in patients with potentially unstable cervical injuries and may facilitate the diagnostic workup and treatment of trauma patients with multiple injuries. 7 Patients with cervical spine injuries treated with halo fixation, however, present unique challenges in terms of airway control. In this series, 14 patients (13%) required emergent or semiemergent intubation, with almost half of these patients dying. The data strongly suggest that emergent intubation in the setting of halo fixation in trauma patients is difficult and often deadly. Of the variables investigated, ISS (P < .01), cardiac history (P < .01), and intubation on arrival (P < .05) strongly correlated with the need for an in-hospital emergent intubation. Cardiac disease (P < .01) and age (P < .05) strongly correlated with the incidence of arrest-related death.
A history of cardiac disease is associated not only with an increased risk of emergent intubation but also with an increased likelihood of dying during the intubation attempt. On careful review of the 14 cases of arrest, all but 4 were clearly preceded by respiratory distress. In the remaining four patients, it was unclear whether a cardiac event preceded or followed the respiratory decompensation. Of the six arrest-related deaths, four patients had a history of cardiac disease. Patients who underwent initial tracheostomy were similar to those patients who arrested in terms of cardiac history and ISS; however, none of these patients went on to die. This suggests that the physiologic stress caused during an emergent intubation may precipitate a lethal cardiac event in patients with a history of cardiac disease. Securing the airway with a tracheostomy before an airway emergency appears to be protective.
Patients who are intubated on arrival also appear to be at increased risk for an emergent or semiemergent intubation (or reintubation) during their hospital stay. Patients in this series were extubated according to the clinical judgment of the attending trauma surgeon or surgical intensivist and met standard extubation criteria (e.g., spontaneous respiratory rate < 25, minimal support settings, Fio2 < 0.5, Pao2 > 80 mm Hg, appropriate mental status). This interesting correlation between intubation status on arrival and the need for reintubation suggests that the criteria used to extubate trauma patients may not be sufficient for patients in halo fixation. Orotracheal intubation for as little as 48 hours has been associated with an increased incidence of clinically silent aspiration after extubation. 8 Patients placed in halo fixation experience a decrease in vital capacity 9 that may reduce their pulmonary reserve and ability to tolerate a pulmonary insult. From a purely biomechanical perspective, regaining the airway in this population can be significantly more challenging. The device prevents easy access to the airway and prevents extension of the head, which can aid in laryngeal visualization.
Naturally, before extubation, patients with halos must be able to maintain an airway, clear secretions, and have the strength to breathe independently. The prior intubation record should be carefully reviewed and anything other than an “easy” intubation should raise red flags. In addition, the patient’s ISS, cardiac history, and age should be considered, because these patient characteristics are associated with an increased incidence of emergent intubation and death. If there is any concern that the patient may need to be reintubated or if the patient is going to require multiple trips to the operating room, the patient should not be extubated. If the patient is deemed safe to extubate, a cricothyroidotomy kit and experienced personnel should be readily available. There should be a low threshold for reintubating these patients under more controlled and elective circumstances. In these situations, a fiberoptic bronchoscope or laryngeal mask airway may be helpful.
Seventeen tracheostomies were performed in this series. The benefits of early tracheostomy in trauma patients requiring long-term ventilation are well described. 10–12 Elective tracheostomy within 7 to 10 days after intubation provides patients with increased mobility and comfort, a better route for pulmonary toilet, and a more secure airway and lowers airway resistance, which may facilitate weaning efforts. 13 Early tracheostomy (1–7 days) is associated with fewer days on the ventilator and shorter intensive care and hospital stays. 14 In this series, eight patients underwent tracheostomy as part of their medical management and before an airway emergency. Patients in this “initial” tracheostomy group did not differ from those who required emergent or semiemergent intubation in terms of the variables investigated. None of the patients who underwent initial tracheostomy developed an airway emergency or died. In contrast, 6 of the 14 patients who required an emergent airway died after multiple intubation attempts that were described as “prolonged,” “difficult,” and “impossible.” In this series, tracheostomy appeared to be protective.
Because postmortem records were not reviewed, we cannot definitively conclude that the six deaths associated with an emergent or semiemergent intubation were not the result of a catastrophic event such as a pulmonary embolism. What is known, however, is that these intubations were described over and over again as “difficult” and “impossible,” with multiple failed attempts at gaining the airway. Possible sequelae of prolonged intubation attempts are known to include cardiac arrest and anoxic brain injury. 15 Of the six patients who died, two were diagnosed with hypoxic brain injury, an injury that was directly attributable to prolonged intubation times. Moreover, because the patients who required emergent or semiemergent intubation did not differ from those who underwent initial tracheostomy, there should be similar rates of respiratory distress, fatal pulmonary embolism, myocardial infarction, and so forth; this is not the case. In fact, no patient who underwent initial tracheostomy had an airway emergency or died. Gaining immediate access to the airway in trauma patients with halo fixation can be exceedingly difficult, and the inability to provide access in a timely fashion may contribute to, if not cause, a patient’s death.
Based on these findings, we suggest that early tracheostomy be considered in hospitalized trauma patients requiring halo fixation who present with a high ISS, a history of cardiac disease, or a condition requiring intubation on arrival. Patients who are intubated on arrival may be more likely to require emergent reintubation during their hospital stay. Older patients (older than 60 years) and those with a history of cardiac disease are more at risk for arrest-related death. Tracheostomy provides a secure airway and protects against the potentially lethal physiologic stress of an emergent intubation. Early surgical stabilization of cervical fractures/dislocations, however, would remove the cumbersome halo device and may obviate the need for airway protection with tracheostomy.
Footnotes
Correspondence: David L. Berger, MD, Department of Surgery, Massachusetts General Hospital, 15 Parkman Street ACC 465, Boston, MA 02114.
E-mail: dberger@partners.org
Accepted for publication July 16, 2001.
References
- 1.Wright SW, Robinson GG, Wright MB. Cervical spine injuries in blunt trauma patients requiring emergent endotracheal intubation. Am J Emerg Med 1992; 10: 104–109. [DOI] [PubMed] [Google Scholar]
- 2.Gbaanador GM, Fruin AH, Taylon C. Role of routine emergency cervical radiography in head trauma. Am J Surg 1986; 152: 643–648. [DOI] [PubMed] [Google Scholar]
- 3.Bucholz RW, Burkhead WZ, Graham W, et al. Occult cervical spine injuries in fatal traffic accidents. J Trauma 1979; 19: 768–771. [DOI] [PubMed] [Google Scholar]
- 4.Ivy ME, Cohn SM. Addressing the myths of cervical spine injury management. Am J Emerg Med 1997; 15: 591–595. [DOI] [PubMed] [Google Scholar]
- 5.Manthey DE. Halo traction device. Emerg Med Clin North Am 1994; 12: 771–778. [PubMed] [Google Scholar]
- 6.Mlinek EJ Jr, Clinton JE, Plummer D, et al. Fiberoptic intubation in the emergency department. Ann Emerg Med 1990; 19: 359–362. [DOI] [PubMed] [Google Scholar]
- 7.Heary RF, Hunt CD, Krieger AJ, et al. Acute stabilization of the cervical spine by halo/vest application facilitates evaluation and treatment of multiple trauma patients. J Trauma 1992; 33: 445–451. [DOI] [PubMed] [Google Scholar]
- 8.Leder SB, Cohn SM, Moller BA. Fiberoptic endoscopic documentation of the high incidence of aspiration following extubation in critically ill trauma patients. Dysphagia 1998; 13: 208–212. [DOI] [PubMed] [Google Scholar]
- 9.Lind B, Bake B, Lundqvist C, Nordwall A. Influence of halo vest treatment on vital capacity. Spine 1987; 12: 449–452. [DOI] [PubMed] [Google Scholar]
- 10.Kane TD, Rodriguez JL, Luchette FA. Early versus late tracheotomy in the trauma patient. Respir Care Clin North Am 1997; 3: 1–20. [PubMed] [Google Scholar]
- 11.Armstrong PA, McCarthy MC, Peoples JB. Reduced uses of resources by early tracheotomy in ventilator-dependent patients with blunt trauma. Surgery 1998; 124: 763–766. [DOI] [PubMed] [Google Scholar]
- 12.Kluger Y, Paul DB, Lucke J, et al. Early tracheostomy in trauma patients. Eur J Emerg Med 1996; 3: 95–101. [DOI] [PubMed] [Google Scholar]
- 13.Mulder DS, Marelli D. Evolution of airway control in the management of injured patients. J Trauma 1992;1991: 33: 856–862. [PubMed] [Google Scholar]
- 14.Rodriguez JL, Steinberg SM, Luchetti FA, et al. Early tracheostomy for primary airway management in the surgical critical care setting. Surgery 1990; 108: 655. [PubMed] [Google Scholar]
- 15.Sandur S, Stoller JK. Pulmonary complications of mechanical ventilation. Clin Chest Med 1999; 20: 223–247. [DOI] [PubMed] [Google Scholar]