Abstract
Objective
To compare the results of open versus laparoscopic repair for perforated peptic ulcers.
Summary Background Data
Omental patch repair with peritoneal lavage is the mainstay of treatment for perforated peptic ulcers in many institutions. Laparoscopic repair has been used to treat perforated peptic ulcers since 1990, but few randomized studies have been carried out to compare open versus laparoscopic procedures.
Methods
From January 1994 to June 1997, 130 patients with a clinical diagnosis of perforated peptic ulcer were randomly assigned to undergo either open or laparoscopic omental patch repair. Patients were excluded for a history of upper abdominal surgery, concomitant evidence of bleeding from the ulcer, or gastric outlet obstruction. Patients with clinically sealed-off perforations without signs of peritonitis or sepsis were treated without surgery. Laparoscopic repair would be converted to an open procedure for technical difficulties, nonjuxtapyloric gastric ulcers, or perforations larger than 10 mm. A Gast- rografin meal was performed 48 to 72 hours after surgery to document sealing of the perforation. The primary end-point was perioperative parenteral analgesic requirement. Secondary endpoints were operative time, postoperative pain score, length of postoperative hospital stay, complications and deaths, and the date of return to normal daily activities.
Results
Nine patients with a surgical diagnosis other than perforated peptic ulcer were excluded; 121 patients entered the final analysis. There were 98 male and 23 female patients recruited, ages 16 to 89 years. The two groups were comparable in age, sex, site and size of perforations, and American Society of Anesthesiology classification. There were nine conversions in the laparoscopic group. After surgery, patients in the laparoscopic group required significantly less parenteral analgesics than those who underwent open repair, and the visual analog pain scores in days 1 and 3 after surgery were significantly lower in the laparoscopic group as well. Laparoscopic repair required significantly less time to complete than open repair. The median postoperative stay was 6 days in the laparoscopic group versus 7 days in the open group. There were fewer chest infections in the laparoscopic group. There were two intraabdominal collections in the laparoscopic group. One patient in the laparoscopic group and three patients in the open group died after surgery.
Conclusions
Laparoscopic repair of perforated peptic ulcer is a safe and reliable procedure. It was associated with a shorter operating time, less postoperative pain, reduced chest complications, a shorter postoperative hospital stay, and earlier return to normal daily activities than the conventional open repair.
Peptic ulcer perforation is a common surgical emergency and a major cause of death in elderly patients. 1,2 There is, however, disagreement as to the relative merits of nonoperative treatment, simple closure, or a definitive acid-reduction procedure for perforated peptic ulcers. Nonoperative treatment of perforated peptic ulcers was shown to be effective. 3 However, the uncertainty in diagnosis, the potential delay for treatment in nonresponders, and the unreliable response in elderly patients make it difficult to be applied to all clinical situations.
In the past two decades, there has been a change in the pattern of perforated peptic ulcer disease in affecting old and infirm patients, with a high association with nonsteroidal antiinflammatory agents. 4–11 They seldom require any definitive procedure, which is associated with increased rates of perioperative death and complications. 12Helicobacter pylori is now the recognized culprit of the majority of patients with duodenal and gastric ulcers, and posteradication ulcer recurrence is uncommon. 13–15 Acid-reduction procedures are not required for this group of patients. As a result, simple closure of the perforation with an omental patch has become the favored management approach in many institutions. It is technically straightforward and reliable and is also the preferred approach for high-risk patients. 16–22
Laparoscopic cholecystectomy has become the standard procedure for removal of diseased gallbladder, superseding open cholecystectomy because it reduces pain, the wound complication rate, and the length of hospital stay. 23 The advantages of laparoscopic repair of perforated peptic ulcers are less apparent. We conducted a randomized trial to compare the outcome of laparoscopic and open omental patch repair for perforated peptic ulcers.
PATIENTS AND METHODS
All patients diagnosed clinically with perforated peptic ulcers were prospectively randomized to undergo either conventional open or laparoscopic suture omental patch repair. The study protocol was approved by the hospital ethics committee before the trial began. Informed consent for randomization to laparoscopic or open omental patch repair was obtained from all patients, with no refusals.
Patients older than 16 with a perforated peptic ulcer were eligible for the study unless they had previous upper abdominal surgery, concomitant evidence of peptic ulcer bleeding, or gastric outlet obstruction. No patient was excluded because of poor surgical risk. Patients with clinically sealed-off perforations without signs of peritonitis or sepsis were treated without surgery. Patients with a surgical diagnosis other than perforated peptic ulcer were excluded at surgery and the clinical details were recorded.
Randomization was performed after the decision was made for surgery; it took place in the operating room control room by a person not otherwise involved in the clinical setting, after obtaining consent from the patient. Randomization was undertaken by consecutively numbered opaque sealed envelopes containing the treatment options, which were assigned by computer-generated random numbers.
Surgical Procedures
All patients received intravenous fluids, nasogastric catheter decompression, and parenteral analgesics before surgery. Intravenous Cefuroxime (Glaxo-Wellcome, Middlesex, UK) (750 mg) was given every 8 hours after the clinical diagnosis of perforated peptic ulcer was made, and surgery was to be performed as soon as the operating room was ready.
All open repairs were performed according to standard techniques described in surgical textbooks and were done by registrars supervised by consultants. 24,25 We used an upper midline incision. After identification of the site of the perforation, a healthy piece of omentum was drawn under an arch of full-thickness polygalactin (Vicryl; Ethicon, Johnson & Johnson, Brussels, Belgium) sutures placed on either side of the perforation, and the sutures were tied. Thorough peritoneal toilet followed. No drain was left in accordance with the standard routine at our institution. The abdominal wound was infiltrated with 0.25% Bupivacaine (Astra Pharmaceuticals Pty Ltd, NSW, Australia) at the end of the procedure.
Laparoscopic repair was performed by a team of four surgeons (one consultant, two senior registrars, one registrar) who were experienced in laparoscopic cholecystectomy and had undergone laboratory laparoscopic suturing training. Under general anesthesia and muscle relaxation, the patient was placed in a Lloyd-Davis position with reverse Trendelenburg tilt. The operating surgeon stood between the patient’s thighs. The open method was used for insertion of the initial 10-mm umbilical port. A 30° laparoscope was then introduced. Two additional working ports were inserted at the level of the transpyloric plane at the midclavicular line on both sides. A 10-mm cannula was inserted in the left subcostal region to facilitate the insertion of sutures. After initial exploration of the peritoneal cavity, the pyloroduodenal region was meticulously searched for the perforation. If the omentum was attached to the suspected perforation site, the omentum was gently pulled away with forceps to assess the underlying pathology. Instrumental compression of the antrum of the stomach and the first part of the duodenum facilitated identification by inducing escape of fluid and bubbles from the perforations. The degree of peritoneal soiling was noted, and peritoneal fluid was sampled by a suction device for microbiologic examination. The size of the perforation was measured with reference to the size of the jaws of a laparoscopic grasper. Laparoscopic procedures were to be converted to open for nonpyloric gastric ulcer perforation, perforations larger than 10 mm, or whenever technical difficulties were encountered. A 10-mm perforation was arbitrarily chosen as the cut-off point for large perforation, for which patch repair may not be the procedure of choice.
We have reported our single-stitch laparoscopic repair method previously. 26 A Szabo-Berci “parrot jaws” needle driver (Karl-Storz, Tuttlingen, West Germany) was used for suturing. The needle and suture were introduced through the 10-mm operating port on the left. Liver retraction was maintained by blunt dissection forceps placed in the right subcostal port. A single stitch (3-0 polygalactin half-circle round-bodied needle) was applied with a good bite of full-thickness healthy tissue taken longitudinally across the middle of the perforations. The ulcer edges were approximated by intracorporeal knotting, with two identical half knots forming a square knot followed by a third and opposite half knot. The same stitch was then passed through a piece of omentum and another three throws of knot was performed to anchor the omental patch over the repaired site. Thorough peritoneal lavage was performed with pressurized warm normal saline, and all the purulent exudates and irrigation fluid were aspirated before closure. No drain was used. All the port sites were infiltrated with 0.5% bupivacaine after closure.
Postoperative Management and Follow-Up
After surgery, a standardized analgesic regimen was administered (1 mg/kg intramuscular pethidine every 4 hours on request) for pain relief. Intravenous cefuroxime was continued for at least 5 days. An independent assessor visited every patient in the morning to record the clinical progress, analgesic requirements, and pain score (by visual analog scale of a 10-cm horizontal line without graduations) on postoperative days 1 and 3. All patients received a Gastrografin meal through the nasogastric tube 48 to 72 hours after surgery to document sealing off of the perforation. Feeding was resumed as soon as ileus subsided. Patients were assessed by independent surgeons for discharge if they could tolerate a normal diet, could fully ambulate, and required only oral analgesics. Both the independent assessor and in-charge surgeons were not blinded with respect to study groups.
All patients received the same instructions to return to normal activity and to work, and they were requested to keep a diary of the date of resumption of full daily activities and work. Patients were then reviewed at the outpatient department at 4 weeks, 3 months, and 6 months after surgery. Upper gastrointestinal endoscopies were performed 8 weeks after surgery to assess healing of the ulcers and evaluate the Helicobacter status, and the patients were then treated accordingly.
Endpoints
The primary endpoint was perioperative parenteral analgesic requirement. Secondary endpoints were operating time, postoperative pain score, length of postoperative hospital stay, complications and deaths, and the date of return to normal daily activities.
Data Collection
Standardized data collection was performed by the registrar in charge of the patients. Operative time was defined as the time from the first incision to the placement of the last suture. We noted all operative and postoperative complications. Conversion of a laparoscopic procedure to an open procedure was not regarded as a complication. Wound infection was defined as the presence of pus or sanguinopurulent discharge at the surgical site. Chest infections were diagnosed by radiographic evidence of pulmonary changes with or without a fever of more than 39°C or positive cultures from sputum. The length of postoperative stay was defined as the number of days in the hospital after surgery, inclusive of the day of surgery. Systolic blood pressure less than 90 mm Hg on admission was defined as shock. Patients with severe abdominal pain more than 24 hours before admission were defined as having a delayed presentation.
Statistical Analysis
Data were collected on standard forms and were prospectively entered into a computer database. Preoperative data comprised characteristics of the patients, history, physical examination findings, and laboratory and imaging tests.
In a previous report by Tate et al, 27 laparoscopic repair of perforated peptic ulcers required significantly fewer analgesic injections than open repair (median 2 vs. 4 doses, P = .048, Mann-Whitney test). Based on our data, we estimated the median number of analgesic injections was three for laparoscopic and five for open repair. Assuming a pooled standard deviation of three, and assigning α = 0.05 and β = 0.1, a minimum of 47 patients had to be recruited in each limb. Assuming a 10% rate of nonperforated peptic ulcer operative diagnosis, the sample size needed was calculated to be 60 patients per group.
We analyzed data according to the intent-to-treat principle; all patients with a surgical diagnosis of perforated peptic ulcer were included in the final analysis. For descriptive purposes data are presented as mean with standard deviations or medians with quartiles for quantitative variables, and as absolute and relative frequencies for qualitative variables. Discrete variables were expressed as counts and percentages. Continuous data are expressed as mean with standard deviation, with calculation of the probability value to measure the significance of differences. The Student t test was used for comparisons of continuous variables. Categorical and binary variables were tested by the two-tailed Pearson chi-square test with Yates correction or Fisher exact test if more than 20% of the cells in the frequency tables had an expected frequency below 5. The Mann-Whitney test was used for other non-parametric quantitative data. All statistical tests were two-tailed at the probability level of 0.05. Calculations were done with SPSS/PC statistical software (Chicago, IL, version 8.0).
RESULTS
From January 1994 to June 1997, 146 patients with a preoperative diagnosis of perforated peptic ulcer were identified, 16 of whom were excluded from randomization (9 patients with previous upper abdominal operations, 5 with concomitant ulcer bleeding, 2 with evidence of gastric outlet obstruction). One hundred thirty patients were randomized and nine patients recruited into the study with a surgical diagnosis other than perforated peptic ulcer were excluded after randomization from the final data analysis (Fig. 1). During the same period, another 10 patients with perforated peptic ulcer who underwent laparotomies were not recruited because of an uncertain preoperative diagnosis.
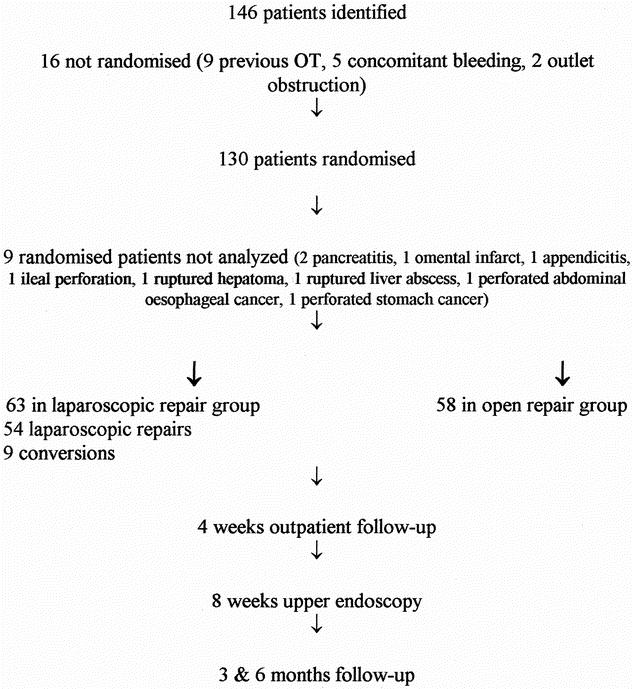
Figure 1. Trial profile.
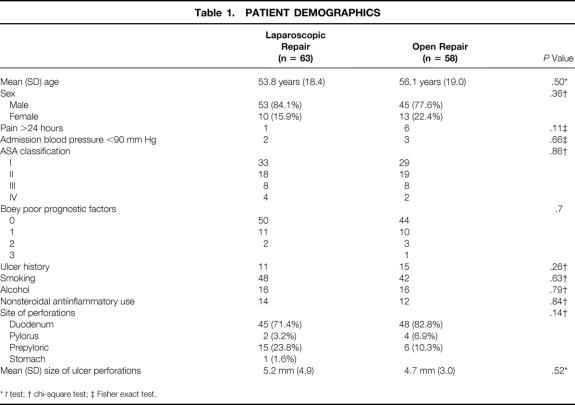
Sixty-three patients in the laparoscopic group and 58 patients in the open group entered final analysis. The demographic characteristics of the two groups are shown in Table 1. They were similar in age range, sex distribution, and American Society of Anesthesiology (ASA) classification status. The sites and sizes of ulcer perforations were comparable in both groups. The two groups were also comparable in other preoperative characteristics such as shock on admission, duration of pain longer than 24 hours, previous history of peptic ulcer disease, and recent consumption of nonsteroidal antiinflammatories. No patient was reported to have a history of recent cocaine consumption. Boey et al 28 reported that major medical illness, preoperative shock, and longstanding perforation (more than 24 hours) were considered poor prognostic factors. The two groups in this study were similar in these characteristics. In our study, we found that hypotension could not reliably predict outcome, and all patients admitted with hypotension survived.
Table 1. PATIENT DEMOGRAPHICS
*t test;
† chi-square test;
‡ Fisher exact test.
Five patients (two in the laparoscopic group, three in the open group) were found to have omentum adhered to the perforated ulcers; the omentum was gently removed to uncover the perforations, and repairs were performed accordingly. Laparoscopic repair was completed in 54 patients (87%). There were nine conversions: three patients had perforated nonpyloric gastric ulcers, three had unidentifiable perforations, two had perforations larger than 10 mm, and one had bleeding during suturing.
A comparison of various outcome parameters for the two groups is shown in Tables 2 and 3.
Table 2. RESULTS
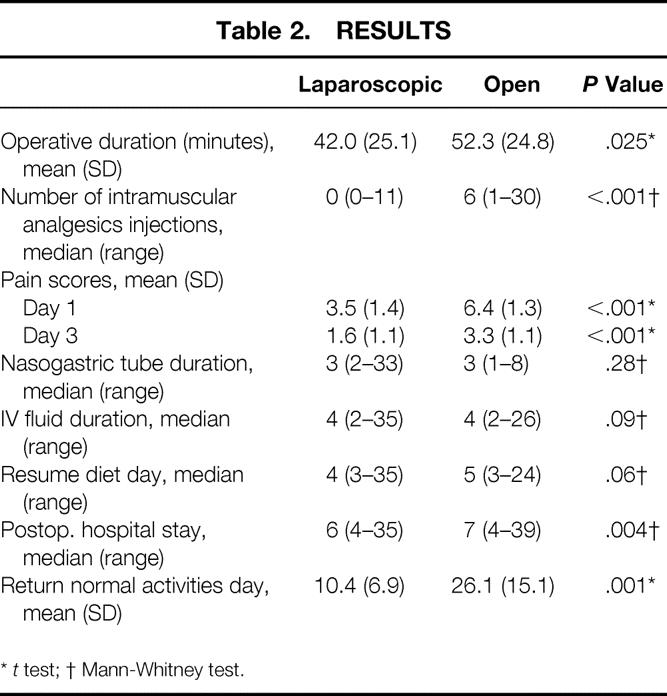
*t test;
† Mann-Whitney test.
Table 3. OUTCOME ACCORDING TO BOEY’S ADMISSION POOR PROGNOSTIC FACTORS
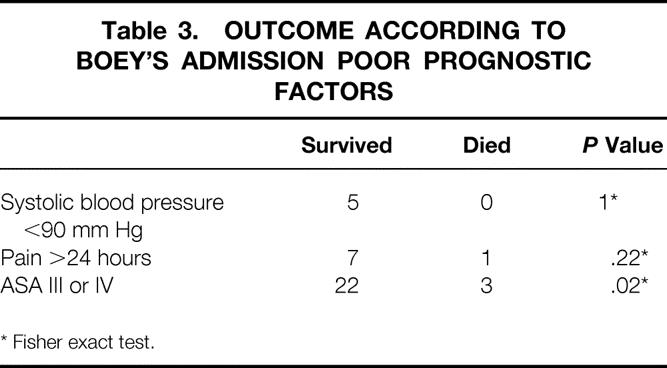
* Fisher exact test.
The mean operative time for laparoscopic repair was 42 minutes, significantly shorter than for open repair (52.3 minutes). Patients who underwent laparoscopic repair required significantly less parenteral analgesics than the open group, and more than half of the patients in the laparoscopic group did not ask for any pethidine injection. Patients in the laparoscopic group had a lower visual analog pain score on postoperative days 1 and 3 (P < .001). There was no difference between the two groups in the timing of removal of nasogastric tube or intravenous fluids or the timing of full diet resumption.
There were significantly fewer chest infections in the laparoscopic group than in the open group (0 vs. 7, P = .005). One patient in the laparoscopic group early in our series had leakage after repair and required open drainage. Another patient in the open group had a confined radiologic leak that responded to conservative treatment. Wound complications occurred in two converted patients in the laparoscopic group; one had a wound infection and the other had wound dehiscence. Although there were seven wound infections in the open group, the difference did not reach statistical significance when compared with the laparoscopic limb. There were two patients with intraabdominal collections in the laparoscopic group: one of them had leakage from the repaired site and required reoperation, and the other patient was managed by percutaneous drainage. Three patients in the laparoscopic group were reoperated on, one for leakage, another for gastric outlet obstruction, and the last one for wound dehiscence. A patient in the open group required a second operation for wound dehiscence.
One patient in the laparoscopic group and three in the open group died in the postoperative period. All of these patients belonged to ASA III or IV groups and were older than 75. One patient with a narcotic overdose died of chest infection. Another diabetic patient had perioperative aspiration and died of adult respiratory distress syndrome. The third patient died of multiorgan failure secondary to sepsis. The only patient in the laparoscopic group to die did so of multiorgan failure; this patient had diabetes, hypertension, atrial fibrillation, nephropathy, thyrotoxicosis, and recent cerebrovascular accident (Table 4).
Table 4. DEATH AND COMPLICATIONS
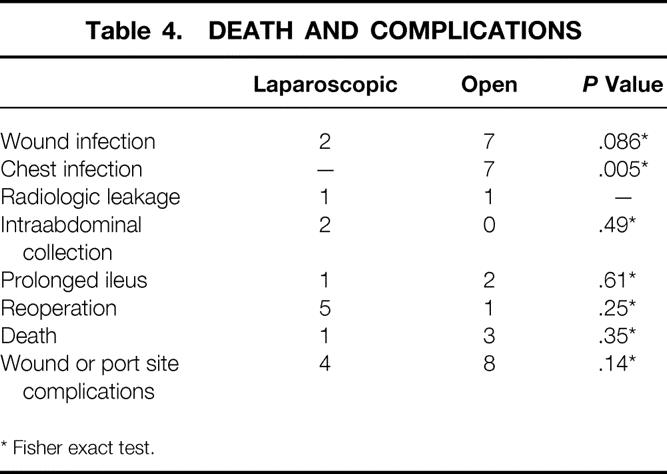
* Fisher exact test.
Patients in the laparoscopic group were discharged earlier than patients who had open procedures. Patients in the laparoscopic group were also able to return to normal activities earlier than patients in the open group (10.4 vs. 26.1 days, P = .001) (see Table 2).
Four patients in the laparoscopic group were found to have late wound complications. Umbilical sepsis developed in one patient, and another patient reported persistent pain in the umbilical wound. In one patient, a port site hernia developed at 3 months follow-up and required surgical repair. The patient who underwent conversion had incisional hernia after reoperation for wound dehiscence. Five patients in the laparoscopic group required reoperation; when compared with the open group, there was no significant difference.
Eight patients in the open group had delayed wound problems: two patients with hypertrophic scars and six with persistent painful abdominal scars.
DISCUSSION
Advances in the medical treatment of peptic ulcer disease have led to a dramatic decrease in the number of elective ulcer surgeries performed. Nonetheless, the number of patients requiring surgical intervention for complications such as perforations remains relatively unchanged. 1,4–7 Minimal access surgery has assumed an ever-expanding role in gastrointestinal surgery since the introduction of laparoscopic cholecystectomy. Laparoscopic cholecystectomy has rapidly become a standard practice in most parts of the world for elective cholecystectomy, but the role of laparoscopic surgery for perforated peptic ulcer is not well defined.
The total trauma incurred by a patient undergoing an operation is the sum of the access trauma and the surgical procedural trauma. When the access trauma of a midline laparotomy is relatively large compared with the procedural trauma of patch repair for perforated peptic ulcer, the benefit of minimal-access laparoscopic surgery will be maximized. 27 The laparoscopic approach reduces the access trauma, can confirm or refute the diagnosis, and can be used to perform the same repair procedure and lavage as open omental patch repair. 26,29–53 It has been advocated by others as a way of performing diagnostic laparoscopy to confirm or disprove the diagnosis, and if the perforation is already sealed off by omentum, it is left alone and peritoneal lavage is performed laparoscopically. 40,41
After the initial reports 30,31 of laparoscopic treatment of perforated peptic ulcer, different techniques of ulcer closure had been tried; suturing, 35 gelatin sponge and fibrin glue, 29,46,47 stapled omental patch repair, 38,39 and gastroscopy-aided insertion of the ligamentum teres hepatis. 32 Other workers advocated the use of a gastroscopic-guided omental plug to close the perforation. 51 In our series of laparoscopic repairs, we adopted the suture closure method because it is based on the principle of conventional open repair and does not require additional foreign bodies.
The first randomized trial comparing laparoscopic versus open repair of perforated peptic ulcer showed that laparoscopic repair took significantly longer but required fewer postoperative analgesics. 47 The laparoscopic repair method used in that trial was different from our reported method;26 the reported operative times for laparoscopic suture and laparoscopic sutureless method were 112.9 and 74.8 minutes, respectively. The short operative time in the laparoscopic repair was largely related to our modification of the laparoscopic closure technique. By applying one single stitch across the perforation and using the same suture to anchor the omentum, cumbersome multiple interrupted suturing is avoided. 26 The majority of the ulcer perforations were small, and we found this single-suture closure technique safe in such circumstances. Laparoscopic repair is, however, technically more demanding, and surgeons need specific training in laparoscopic suturing technique.
The results of our randomized controlled study in a large group of patients showed that when compared with open repair, laparoscopic repair is associated with a shorter operative time, reduced postoperative pain and analgesic requirements, a shorter hospital stay, and earlier return to normal daily activities. The complication rate for laparoscopic repair was low; the laparoscopic procedure was associated with fewer chest infections and potentially less wound infection compared with open repair.
Laparoscopic surgery minimizes postoperative wound pain and encourages early mobilization and return to normal daily activities. The benefit of early discharge and early return to work may outweigh the consumable cost incurred in the execution of the laparoscopic procedures.
The role of laparoscopic surgery in emergencies is well documented. 54 The change of disease pattern in perforated peptic ulcer favors a simple repair procedure. With the demonstrated benefit in our trial, laparoscopic repair of perforated peptic ulcers should be the procedure of choice. Laparoscopy should be incorporated into the general surgeon’s armamentarium for the management of patients with peritonitis.
In conclusion, this study has shown that laparoscopic suture omental patch repair confers benefits on patients in the form of reduced postoperative pain, less chest infection, a shorter hospital stay, and an earlier return to normal activities.
Footnotes
Correspondence: Michael K. W. Li, MBBS, MRCS, LRCP, FRCS, FRCSEd, Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong, SAR, China.
E-mail: siuwt@hongkong.com
Accepted for publication October 5, 2001.
References
- 1.Koo J, Ngan YK, Lam SK. Trends in hospital admissions, perforation and mortality of peptic ulcer in Hong Kong from 1970 to 1980. Gastroenterology 1983; 84: 1558–1562. [PubMed] [Google Scholar]
- 2.Alagaratnam TT, Wong J. No decrease in duodenal ulcer surgery after cimetidine in Hong Kong. J Clin Gastroenterol 1988; 10: 25–27. [DOI] [PubMed] [Google Scholar]
- 3.Crofts TJ, Park KGM, Steel RJC, et al. A randomized trial of non-operative treatment for perforated peptic ulcer. N Engl J Med 1989; 320: 970–973. [DOI] [PubMed] [Google Scholar]
- 4.Gunshefski L, Flancbaum L, Brolin RE, Frankei A. Changing patterns in perforated peptic ulcer disease. Am Surg 1990; 56: 270–274. [PubMed] [Google Scholar]
- 5.Cocks JR. Perforated peptic ulcer: the changing scene. Dig Dis 1992; 10: 10–16. [DOI] [PubMed] [Google Scholar]
- 6.Walt R, Katschinski B, Logan R, et al. Rising frequency of ulcer perforation in the United Kingdom. Lancet 1986; 3: 489. [DOI] [PubMed] [Google Scholar]
- 7.Kulber DA, Hartunian S, Schiller D, Morgenstern L. The current spectrum of peptic ulcer disease in the older age groups. Am Surg 1990; 56: 737. [PubMed] [Google Scholar]
- 8.Gilinsky NH. Peptic ulcer disease in the elderly. Gastroenterol Clin North Am 1990; 19: 255. [PubMed] [Google Scholar]
- 9.Agrez MV, Henry DA, Senthiselvan S, Duggan JM. Changing trends in perforated peptic ulcer during the past 45 years. Aust NZ J Surg 1992; 62: 729. [DOI] [PubMed] [Google Scholar]
- 10.Svanes C, Salvesen H, Stangeland L, et al. Perforated peptic ulcer over 56 years: time trends in patients and disease characteristics. Gut 1993; 34: 1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lanas A, Serrano P, Bajador E, et al. Evidence of aspirin use in both upper and lower gastrointestinal perforation. Gastroenterology 1997; 112: 683–689. [DOI] [PubMed] [Google Scholar]
- 12.Blomgren LG. Perforated peptic ulcer: long-term results after simple closure in the elderly. World J Surg 1997; 21: 412–414. [DOI] [PubMed] [Google Scholar]
- 13.Graham DY. Treatment of peptic ulcers caused by Helicobacter pylori. N Engl J Med 1993; 328: 349–350. [DOI] [PubMed] [Google Scholar]
- 14.NIH consensus development panel. Helicobacter pylori in peptic ulcer disease. JAMA 1994; 272: 65–69. [PubMed] [Google Scholar]
- 15.Sung JJ, Chung SC, Ling TK, et al. Antibacterial treatment of gastric ulcers associated with Helicobacter pylori. N Engl J Med 1995; 332: 139–142. [DOI] [PubMed] [Google Scholar]
- 16.McGuire HH, Horsley JS. Emergency operation for gastric duodenal ulcers in high-risk patients. Ann Surg 1986; 203: 551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feliciano DV, Bitondo CG, Burch JM, et al. Emergency management of perforated peptic ulcers in the elderly patients. Am J Surg 1984; 148: 764–767. [DOI] [PubMed] [Google Scholar]
- 18.Jordan GL, DeBakey ME, Duncan JM. Surgical management of perforated peptic ulcer. Ann Surg 1974; 179: 628–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson-Macdonald J, Mortensen NJMcC, Williamson RCN. Perforated gastric ulcer. Postgrad Med J 1985; 61: 217–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collier D, Pain JA. Perforated peptic ulcers. J R Coll Surg Edinb 1985; 30: 26–29. [PubMed] [Google Scholar]
- 21.Turner WT, Thompson WM, Thal ER. Perforated gastric ulcers. A plea for management by simple closure. Arch Surg 1988; 123: 960–964. [DOI] [PubMed] [Google Scholar]
- 22.Bornman PC, Theodorou NA, Jeffery PC, et al. Simple closure of perforated duodenal ulcer: a prospective evaluation of a conservative management policy. Br J Surg 1990; 77: 73–75. [DOI] [PubMed] [Google Scholar]
- 23.The Southern Surgeons Club. A prospective analysis of 1,518 laparoscopic cholecystectomies. N Engl J Med 1991; 324: 1073–1078. [DOI] [PubMed] [Google Scholar]
- 24.Kirk RM. Stomach and duodenum. In: Kirk RM, ed. General surgical operations, 3d ed. London: Churchill Livingstone, 1994: 190–192.
- 25.Sawyers JL. Acute perforations of peptic ulcer. Surgery of the stomach, duodenum, and small intestine, 2nd ed. In:Scott HW, Sawyers JL, eds. Boston: Blackwell Scientific, 1992:566–572.
- 26.Siu WT, Leong HT, Li MKW. Single stitch laparoscopic omental patch repair of perforated peptic ulcers. J R Coll Surg Edinb 1997; 42: 92–94. [PubMed] [Google Scholar]
- 27.Tate JJ, Dawson JW, Lau WY, Li AKC. Sutureless laparoscopic treatment of perforated duodenal ulcer. Br J Surg 1993; 80: 235. [DOI] [PubMed] [Google Scholar]
- 28.Boey J, Wong J, Ong GB. A prospective study of operative factors in perforated duodenal ulcers. Ann Surg 1982; 195–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuschieri A. Whither minimal access surgery: tribulations and expectations. Am J Surg 1995; 169: 9–19. [DOI] [PubMed] [Google Scholar]
- 30.Mouret P, Francois Y, Vagnal J, et al. Laparoscopic treatment of perforated peptic ulcer. Br J Surg 1990; 77: 1006. [DOI] [PubMed] [Google Scholar]
- 31.Nathanson LK, Easter DW, Cuschieri A. Laparoscopic repair/peritoneal toilet of perforated duodenal ulcer. Surg Endosc 1990; 4: 232–233. [DOI] [PubMed] [Google Scholar]
- 32.Costalat G, Dravet F, Noel P, et al. Coelioscopic treatment of perforated gastroduodenal ulcer using the ligamentum teres hepatis. Surg Endosc 1991; 5: 154–155. [DOI] [PubMed] [Google Scholar]
- 33.Fletcher DR, Jones RM. Perforated peptic ulcer. A further application of laparoscopic surgery. Aust NZ J Surg 1992; 62: 323–324. [DOI] [PubMed] [Google Scholar]
- 34.Sigman HH, Garzon J, Marelli D. Laparoscopic closure of perforated duodenal ulcer. J Laparoendosc Surg 1992; 2: 325–327. [DOI] [PubMed] [Google Scholar]
- 35.Sunderland GT, Chisholm EM, Lau WY, et al. Laparoscopic repair of perforated peptic ulcer. Br J Surg 1992; 79: 785. [DOI] [PubMed] [Google Scholar]
- 36.Fletcher DR, Jones RM. Perforated peptic ulcer. A further application of laparoscopic surgery. Aust NZ Surg 1992; 62: 323–324. [DOI] [PubMed] [Google Scholar]
- 37.Benoit J, Champault GG, Labhar E, Sezeur A. Sutureless laparoscopic treatment of perforated duodenal ulcer [letter]. Br J Surg 1993; 80: 1212. [DOI] [PubMed] [Google Scholar]
- 38.Darzi A, Cheshire NJ, Somers SS. Laparoscopic omental patch repair with an automated stapler. Br J Surg 1993; 80: 1552. [DOI] [PubMed] [Google Scholar]
- 39.Nassar A. Laparoscopic omental patch repair of perforated duodenal ulcer with automated stapler [letter]. Br J Surg 1994; 81: 1393. [DOI] [PubMed] [Google Scholar]
- 40.Walsh CJ, Khoo DE, Motson RW. Laparoscopic repair of perforated peptic ulcer [letter]. Br J Surg 1993; 80: 127. [PubMed] [Google Scholar]
- 41.Schein M. Laparoscopic repair of perforated peptic ulcer [letter]. Br J Surg 1993; 80: 1212. [DOI] [PubMed] [Google Scholar]
- 42.Urbano D, Rossi M, De Simone P, et al. Alternative laparoscopic management of perforated peptic ulcers. Surg Endosc 1994; 8: 1208–1211. [DOI] [PubMed] [Google Scholar]
- 43.Mutter D, Evrard S, Keller P, et al. Treatment of perforated duodenal ulcer: the celioscopic approach. Ann Chir 1994; 48: 339–344. [PubMed] [Google Scholar]
- 44.Eypasch E, Spangenberger W, Ure B, et al. Laparoscopic and conventional suture of perforated peptic ulcers: a comparison. Chirurgie 1994; 65: 445–450. [PubMed] [Google Scholar]
- 45.Matsuda M, Nishiyama M, Hanai T, et al. Laparoscopic omental patch repair for the perforated peptic ulcer. Ann Surg 1995; 221: 236–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lau WY, Leung KL, Zhu XL, et al. Laparoscopic repair of perforated peptic ulcer. Br J Surg 1995; 82: 814–816. [DOI] [PubMed] [Google Scholar]
- 47.Lau WY, Leung KL, Kwong KH, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg 1996; 224: 131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miserez M, Eypasch E, Spangenberger W, et al. Laparoscopic and conventional closure of perforated peptic ulcer. A comparison. Surg Endosc 1996; 10: 831–836. [DOI] [PubMed] [Google Scholar]
- 49.Johansson B, Hallerback B, Glise H, Johnsson E. Laparoscopic suture closure of perforated peptic ulcer. A nonrandomized comparison with open surgery. Surg Endosc 1996; 10: 656–658. [DOI] [PubMed] [Google Scholar]
- 50.Druart ML, Hee RV, Etienne J, et al. Laparoscopic repair of perforated duodenal ulcer: a prospective multicenter clinical trial. Surg Endosc 1997; 11: 1017–1020. [DOI] [PubMed] [Google Scholar]
- 51.Pescatore P, Halkic N, Calmes JM, et al. Combined laparoscopic-endoscopic method using an omental plug for therapy of gastroduodenal ulcer perforation. Gastrointest Endosc 1998; 48: 411–414. [DOI] [PubMed] [Google Scholar]
- 52.Naegaard JM, Edwin B, Reiertsen O, et al. Laparoscopic and open operations in patients with perforated peptic ulcer. Eur J Surg 1999; 165: 209–214. [DOI] [PubMed] [Google Scholar]
- 53.Katkhouda N, Mavor E, Mason R, et al. Laparoscopic repair of perforated duodenal ulcers. Outcome and efficacy in 30 consecutive patients. Arch Surg 1999; 134: 845–850. [DOI] [PubMed] [Google Scholar]
- 54.Paterson-Brown S. Emergency laparoscopic surgery. Br J Surg 1993; 80: 279–283. [DOI] [PubMed] [Google Scholar]