Abstract
Objective
To measure the effects of laparoscopic and open placement of synthetic mesh on recurrence and persisting pain following groin hernia repair.
Summary Background Data
Synthetic mesh techniques are claimed to reduce the risk of recurrence but there are concerns about costs and possible long-term complications, particularly pain.
Methods
Electronic databases were searched and experts consulted to identify randomized or quasi-randomized trials that compared mesh with non-mesh methods, or laparoscopic with open mesh placement. Individual patient data were sought for each trial. Aggregated data were used where individual patient data were not available. Meta-analyses of hernia recurrence and persisting pain were based on intention to treat.
Results
There were 62 relevant comparisons in 58 trials. These included 11,174 participants: individual patient data were available for 6,901 patients, supplementary aggregated data for 2,390 patients, and published data for 1883 patients. Recurrence and persisting pain were less after mesh repair (overall recurrences: 88 in 4,426 vs. 187 in 3,795; OR 0.43, 95% CI 0.34–0.55;P < .001) (overall persistent pain: 120 in 2,368 vs. 215 in 1,998; OR 0.36, 95% CI 0.29–0.46;P < .001), regardless of the non-mesh comparator. Whereas the reduction in recurrence was similar after laparoscopic and open mesh placement (OR 1.26, 95% CI 0.76–2.08;P = .36), persistent pain was less common after laparoscopic than open mesh placement (OR 0.64; 95% CI 0.52–0.78;P < .001).
Conclusions
The use of synthetic mesh substantially reduces the risk of hernia recurrence irrespective of placement method. Mesh repair appears to reduce the chance of persisting pain rather than increase it.
Repair of groin hernia is performed over 700,000 times each year in both the United States and Europe. Although there are many variants, the standard technique changed little over the 100 years up to the late 1980s. Conventional open repair relies on the suture line to close the hernia defect. Its major drawback is hernia recurrence, commonly the reason for 10 to 15% of operations. 1 In some countries, this has largely been replaced by methods using a synthetic mesh to cover the defect, placed either directly through a groin incision or, less commonly, indirectly using a laparoscope. These methods are associated with more rapid return to normal activities and with low recurrence rates. 2,3 Mesh techniques are little used in some other countries, however, because the mesh is an additional cost and there are concerns about possible long-term problems, particularly persistent pain. 4 Placing the mesh with a laparoscope takes longer than through an open incision, and has been linked to rare, serious complications. 3
The least biased evaluation of mesh techniques will come from randomized trials. Individual trials are generally too small to give sufficiently precise estimates of effects and few reports have included data on long-term performance. The EU Hernia Trialists Collaboration is a group of surgical trialists who have participated in randomized trials of open mesh or laparoscopic groin hernia repair. 5 This is a report of a systematic review of these trials. In most cases this was based on reanalysis of individual patient data (IPD), i.e., raw datasets, because of the greater reliability of this approach. 6 The aims were to assess whether mesh techniques reduce the risk of recurrence and whether they are associated with more persisting pain.
METHODS
Collaboration members met face to face at three meetings, with workshops to develop and agree the protocol. The work was coordinated by a statistical secretariat. Our methods followed those of the Cochrane Collaboration. 6,7
Selection of Studies
Studies were eligible for inclusion if they were randomized or quasi-randomized (such as coin toss or alternation) trials comparing laparoscopic with open methods or open mesh with non-mesh methods of groin hernia repair. The electronic bibliographic databases MEDLINE and The Cochrane Central Controlled Trials Registry 7 were first searched. In MEDLINE, the first two stages of the standard Cochrane search strategy 8 were used with the appropriate specific search terms for inguinal hernia repair. There was no language restriction. Further trials were identified from the reference lists of reports of known trials, relevant websites, and by word of mouth through the Collaboration. Trials were identified up to June 2000 and data collection was closed in July 2000.
Data Collection and Analysis
Individual patient data were sought for all patients randomized in all eligible published and unpublished trials for reanalysis by a statistical secretariat. Detailed checks were made on each dataset received, including for randomization integrity. Queries were clarified and the results of the reanalysis verified by the trialist. All analyses were based on the original allocation regardless of the actual method of repair performed (“intention to treat”). If patients had been excluded because they did not receive the allocated procedure, details were sought and included where possible. Where IPD were not available, aggregated data were used; the trialists were asked to verify information abstracted from their publications and supplement this where possible.
Separate analyses were conducted for mesh (whether open or laparoscopic) versus non-mesh methods (e.g., Shouldice 9 or other) and for laparoscopic versus open mesh repair, stratified by the types of mesh repair. Open mesh operations were classified as flat mesh (e.g., Lichtenstein 10), plug and mesh, or preperitoneal mesh (e.g., Stoppa 11), and laparoscopic operations as transabdominal preperitoneal (TAPP) or totally extraperitoneal (TEP).
Three-arm trials were included in all appropriate sections of the meta-analyses. To avoid double counting, the data for trial groups appearing in two comparisons in the same table were divided equally when generating the bottom line estimate. Some trial arms were a mixture of techniques, for example some laparoscopic groups contain a mixture of TAPP and TEP repairs. Where possible, we used the IPD to split a trial into two groups of centers or surgeons that mainly used the different types of repair, and included the resulting two strata of the trial separately in our meta-analyses. Where this was not possible, the trial has been included according to the most common type of repair used.
Possible effect modification by type of non-mesh operation was explored in secondary analyses after stratification by whether they were Shouldice repairs. Hernia recurrence data were based on the method of ascertainment used in individual trials. Persisting pain was defined as any pain (including slight) in the groin region (including testicular) persisting at 1 year after the operation, or at the closest timepoint to 1 year provided this was more than 3 months after surgery.
Statistical Analysis
The observed minus the expected number of events with its variance were derived for each trial to calculate individual and overall odds ratios with 95% confidence intervals using the fixed effects model. 12 Where there was evidence of significant heterogeneity between the trials we also conducted a secondary analysis based on a random effects model. Sensitivity analyses were also performed to assess any impact of non-IPD data and study quality on the effect estimates. Life table analysis using yearly intervals was used to calculate the annual and cumulative recurrence rates using the IPD studies only. We did this rather than deriving pooled survival curves because the times when recurrences were identified tended to be at fixed points after the operation (coinciding with standard follow-up appointments) rather than when the recurrence actually occurred. In order to calculate the numbers of participants exposed to risk those lost to follow-up were assumed to withdraw halfway through each interval.
RESULTS
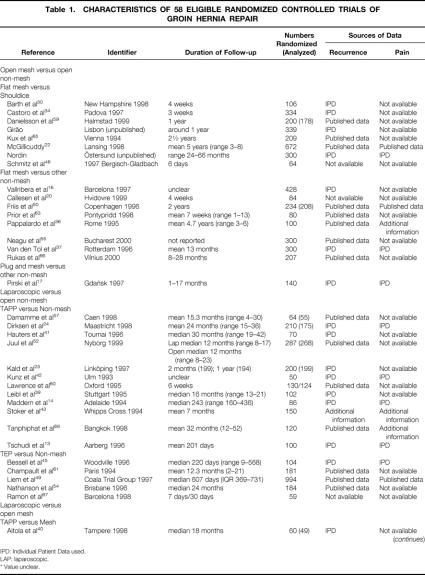
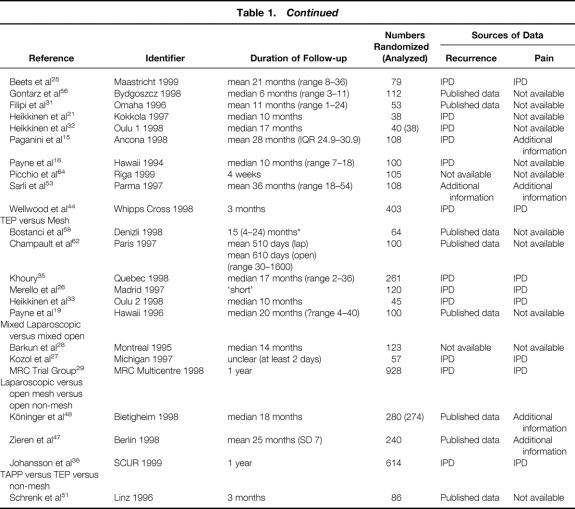
The trials are summarized in Table 1. There were 62 relevant comparisons in 58 eligible trials (11,174 participants), because four trials had three arms. Individual patient data were provided for 35 trials, 13–45 (P Nordin, R Girão: personal communication, 2000) (6,901 participants), two of which have no published report (P Nordin, R Girão: personal communication, 2000), and additional aggregated data for a further nine (2,390 participants). 46–53 Published data only were available for the other 14 (1,883 participants). 54–66 Four of these were identified too late to approach the authors, 55,56,66,67 with information available limited to a conference abstract. All trials were restricted to elective groin hernia repair. Twenty-one included recurrent as well as primary her-nias, 13–15,17,18,23,27,29,31,35,38,40,43,44,49,50,53,58,61,62,68 24 were limited to primary hernias only, 16,21,24,28,30,32–34,36,37,39,41,42,46–48,51,57,60,63–65 (P Nordin, R Girão: personal communication, 2000) one included recurrent hernias only 25, and these details were not reported for 12. 19,20,22,26,45,52,54–56,59,66,67 Based on IPD, participants had a mean age of 54.6 (SD 15.6) years, 95.3% were men, 8.7% had recurrent hernias, 7.0% bilateral, and 1.0% femoral. The comparisons in the 58 trials were: open mesh versus open non-mesh (17 trials, 16,17,20,22,30,34,36,37,46,50,55,59,63,65,66 [P Nordin, R Girão: personal communication, 2000] 3,880 participants); laparoscopic versus open non-mesh (17 trials, 13,14,23,24,39,41–43,45,49,52,54,57,60,61,67,68 3,065 participants); laparoscopic versus open mesh (17 trials, 15,18,19,21,25,26,31–33,35,40,44,53,56,58,62,64 1,898 participants); laparoscopic versus a mixture of open repairs (three trials, 27–29 1,109 participants); laparoscopic versus open mesh versus open non-mesh (three trials, 38,47,48 1,136 participants), and two types of laparoscopic repair versus open non-mesh (one trial, 51 86 participants).
Table 1. CHARACTERISTICS OF 58 ELIGIBLE RANDOMIZED CONTROLLED TRIALS OF GROIN HERNIA REPAIR
IPD: Individual Patient Data used.
LAP: laparoscopic.
* Value unclear.
Table 1A. Continued
The method of randomization used was stated explicitly for 47 of 58 trials: central randomization service in seven, 15,29,34,36,37,39,49 sealed envelopes in 27, 13,14,17–19, 24,25,27,28,32,33,38,41–46,51–53,57,61–63,68 (P Nordin: personal communication, 2000) computer generated random numbers in two 31,47 and random number tables in five 16,20,23,60,64 (although concealment details were not de-scribed), the coin-toss method in two, 22 (R Girão: personal communication, 2000) by alternation in two, 26,40 by birth date in one, 21 and random selection by cards in one. 35 In 11 trials, the allocation was said to be “randomized” but the method was not specified. 30,48,50,54–56,58,59,65–67 The trials ranged in size from 38 to 994 randomized patients. The mean or median duration of follow-up ranged from 6 days to 6 years (Table 1). The method of follow-up was by clinical assessment in 31 trials, by a combination of questionnaire and clinical assessment in three, and was not described in 24 trials.
Hernia Recurrence
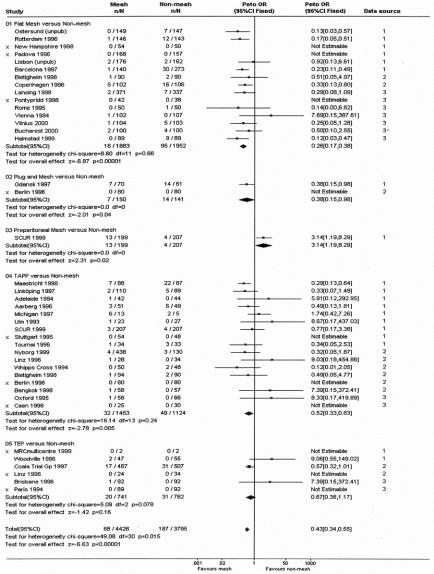
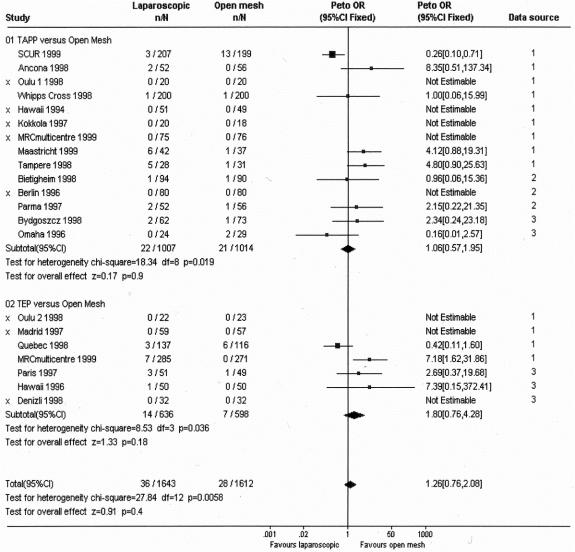
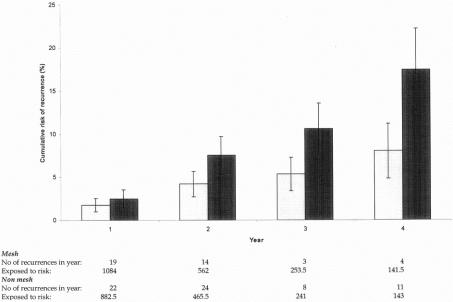
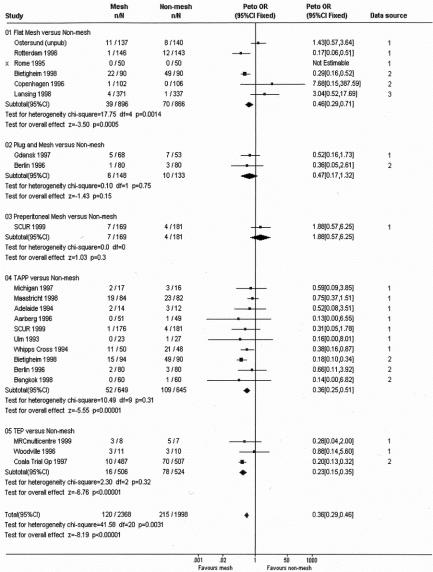
The odds of recurrence varied between trials, in part because of the variable length of follow-up. The odds were lower in the group managed with mesh in 21 of 31 trial comparisons with reported recurrences, irrespective of the method used to place the mesh (Fig. 1). Overall, 88 (2.0%) recurrences were reported after 4,426 mesh repairs compared with 187 (4.9%) after 3,795 conventional repairs (OR 0.43; 95% CI 0.34–0.55; [z = 6.63]P < .001). The pattern was similar regardless of the method of mesh replacement (except the single preperitoneal mesh trial 38 [Fig. 1]) and whether the non-mesh method was Shouldice (OR 0.46 95% CI 0.29–0.72 for mesh versus Shouldice repair, and 0.37, 0.26–0.52, for mesh versus non-Shouldice; data not shown). There was no significant difference in recurrence rates when laparoscopic mesh was compared with open mesh methods (overall 36 of 1,643 (2.2%) versus 28 of 1,612 (1.7%); OR 1.26; 95% CI 0.76 to 2.08) (Fig. 2). The cumulative recurrence rates over time (Fig. 3) suggest that the differences between mesh and non-mesh methods become more marked after the first year. The confidence intervals around these estimates are wide, however, reflecting the relatively few follow-up data available for later years.
Figure 1. Mesh versus non-mesh: hernia recurrence. X denotes no recurrences in either mesh or non-mesh group. The solid squares denote individual odds ratio and the horizontal lines represent 95% confidence intervals. The diamonds denote pooled odds ratio. CI, confidence interval; df, degrees of freedom; OR, Odds Ratio; TAPP, transabdominal preperitoneal; TEP, totally extraperitoneal; MRC, Medical Research Council; SCUR, Scandinavian Clinics United Research. Data source codes: 1 = individual patient data; 2 = additional aggregate data; 3 = published data only.
Figure 2. Laparoscopic versus open mesh: hernia recurrence. X denotes no recurrences in either laparoscopic or open mesh group. The solid squares denote individual odds ratio and the horizontal lines represent 95% confidence intervals. The diamonds denote pooled odds ratio. CI, confidence interval; df, degrees of freedom; OR, Odds Ratio; TAPP, transabdominal preperitoneal; TEP, totally extraperitoneal; MRC, Medical Research Council; SCUR, Scandinavian Clinics United Research. Data source codes: 1 = individual patient data; 2 = additional aggregate data; 3 = published data only.
Figure 3. Cumulative recurrence rates (individual patient data studies only) with 95% confidence intervals.
Persisting Pain
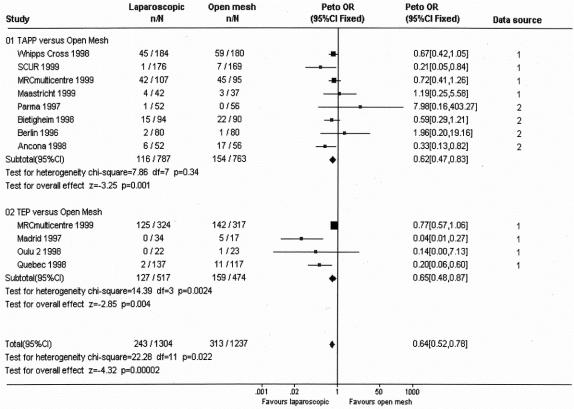
Odds of persisting pain varied considerably between trials reflecting the varying definitions used and the varying times of follow-up. Within trials, the odds were less after mesh repair in 17 of the 21 comparisons for which data could be derived (OR 0.36; 95% CI 0.29–0.46; [z = 8.19]P < .001 [Fig. 4]). Again, this pattern was observed within all the strata characterized by the method of mesh placement and irrespective of the type of non-mesh repair, other than the single preperitoneal mesh trial. 38 Analysis of trials comparing laparoscopic placement with open mesh placement showed fewer reports after laparoscopic repair (OR 0.64; 95% CI 0.52–0.78;[z = 4.32]P < .001[Fig. 5]).
Figure 4. Mesh versus non-mesh: persisting pain. X denotes no pain in either mesh or non-mesh group. The solid squares denote individual odds ratio and the horizontal lines represent 95% confidence intervals. The diamonds denote pooled odds ratio. CI, confidence interval; df, degrees of freedom; OR, Odds Ratio; TAPP, transabdominal preperitoneal; TEP, totally extraperitoneal; MRC, Medical Research Council; SCUR, Scandinavian Clinics United Research. Data source codes: 1 = individual patient data; 2 = additional aggregate data; 3 = published data only.
Figure 5. Laparoscopic versus open mesh: persisting pain. The solid squares denote individual odds ratio and the horizontal lines represent 95% confidence intervals. The diamonds denote pooled odds ratio. CI, confidence interval; df, degrees of freedom; OR, Odds Ratio; TAPP, transabdominal preperitoneal; TEP, totally extraperitoneal; MRC, Medical Research Council; SCUR, Scandinavian Clinics United Research. Data source codes: 1 = individual patient data; 2 = additional aggregate data; 3 = published data only.
Analyses restricted to IPD data alone gave similar estimates for recurrence to the overall results (50/1,773 versus 111/1,846: OR 0.47; 95% CI 0.35–0.65), but more conservative estimates for persisting pain (65/1,004 versus 95/999: OR 0.60; 95% CI 0.42–0.84). Secondary analyses using a random effects model where there was evidence of significant heterogeneity had no qualitative effect on the findings. However, the difference observed in persisting pain between flat mesh and non-mesh (top of Fig. 4) was no longer statistically significant.
DISCUSSION
The Collaboration identified data for 11,000 randomized patients, 10 times more than the single largest trial. These data indicate that the use of synthetic mesh reduces the risk of groin hernia recurrence by around 50%, regardless of method of placement. Persisting pain was also less frequent among the groups allocated to mesh repair, and apparently less common after laparoscopic than after open placement of mesh.
To our knowledge, this is the first time that general surgeons have collaborated to agree on a protocol and contribute raw data to a central reanalysis of trials. This process led to much more data being available in a format suitable for meta-analysis than when relying on published data alone. 2,3 This collaborative framework also means that it is unlikely that we have missed eligible studies, although we do know that one large trial with long term follow-up is currently unreported and recruitment to another is ongoing. Despite our best efforts, IPD were not available for all trials. For nine, trialists checked aggregated data and supplied additional information when available. Of the remaining 14 without IPD, four were identified from conference abstracts just before we closed data collection. The collection of IPD for 35 trials did enhance the information available on recurrence, but was particularly important for the analyses of persisting pain, as few published reports have included this. 2,3 Also, the IPD suggest that the available non-IPD data overestimate the reduction in persisting pain following mesh repair.
The trials did vary in methodological quality. The effect sizes estimated from those with known more secure methods of randomization were smaller but still significant (ORs for mesh vs. non-mesh recurrence: 0.55; 0.40–0.75; persisting pain: 0.40; 0.31–0.53). The OR for mesh versus non-mesh recurrence was lower among trials with follow-up rates above 90%.
The method of repair used in the non-mesh groups varied between trials (Table 1). There were, however, no differences in recurrence reduction in analyses stratified by whether the Shouldice method was used. Also, lower odds of recurrence were observed after mesh repair, regardless of whether the method of placement was by open or laparoscopic surgery (Fig. 1). The only possible exception was preperitoneal mesh and this reflected one trial only. 38 Trials that were direct comparisons between different methods of mesh placement (Fig. 2) also suggested that these two methods of placement were equally effective in this respect. The reduction in hernia recurrence attributable to mesh repair appears to increase over time (Fig. 3). Although relatively few data are available to assess this for later years, an absolute reduction of 6% or more is likely; this equates to one fewer recurrence for every 17 repairs performed, or 42,000 fewer recurrences each year in Europe or the United States.
Worldwide, there is a widely varying use of mesh techniques for groin hernia repair. One reason for not using mesh is concern about long-term morbidity. We found only two cases of mesh infection (one laparoscopically placed 56 and one placed by an open procedure 52). The 7,157 people repaired with mesh had very variable follow-up, however (Table 1). A second concern is the possibility of groin pain. 4 Our data indicate that it is more likely that mesh reduces rather than increases persisting pain. This finding should be interpreted cautiously. We adopted a broad definition and included any pain in the groin region (including testicular pain), regardless of severity or impact, reported around 1 year after the operation. As a consequence, prevalence rates differed widely between trials. There are currently few published data and most of those reported here came from IPD analysis. Even with IPD such data were available from only about 50% of relevant trials. Two trials 48,49 contribute half the “weight” to this analysis; after their removal, the difference is more modest (OR 0.63, 95% CI 0.45–0.87). Another reason for not using mesh repair is the extra cost of the mesh. Our findings suggest that these costs are offset by savings associated with reduced risk of recurrence over 1 to 4 years (the time depending on the local costs or charges for repeat surgery).
The clinical role of laparoscopic mesh repair remains controversial. There are short-term benefits in terms of less pain and more rapid recovery. However, it is associated with an estimated 4.7 serious adverse events per 1,000 procedures3 and formal economic analyses show that it is not cost-effective for routine use, principally because it takes longer to perform and may involve the use of disposable equipment. 69 This study now indicates that recurrence rates are similar after laparoscopic and open mesh repair. Persisting pain appears less common after laparoscopic repair. However, the caveats discussed above also apply to this finding. Furthermore, one trial has suggested that while laparoscopic repair reduces groin pain, it may increase testicular pain. 29 We were not able to address this within our current dataset and it needs further investigation. Laparoscopic repair might be most useful in specified sub-groups of patients, such as those with bilateral or recurrent hernias. Secondary analyses limited to such patients for whom we had IPD had too few data to address this reliably.
The EU Hernia Trialists Collaboration:
The Steering Committee—Adrian Grant (Project Leader; UK), Peter Go (Chairman; The Netherlands), Abe Fingerhut (France), Andrew Kingsnorth (UK), Jesús Merello (Spain), Paddy O’Dwyer (UK), John Payne (USA)
Other Members of the Writing Committee: Kirsty McCormack (UK), Sue Ross (Canada), Neil Scott (UK), Luke Vale (UK).
Collaborators
Petri Aitola (Finland), Bo Anderberg (Sweden), Jeffrey Barkun (Canada), Richard Barth Jnr (USA), Morten Bay-Nielsen (Denmark), Geerard Beets (The Netherlands), Reinhard Bittner (Germany), Sven Bringman (Sweden), Torben Callesen (Denmark), Carlo Castoro (Italy), Coala Trial Steering Committee (The Netherlands), Carmen Dirksen (The Netherlands), Charles Filipi (USA), Robert Fitzgibbons (USA), Esbern Friis (Denmark), Ricardo Girão (Portugal), Paul Graham (UK), Efthimios Hatzitheoklitos (Greece), Philippe Hauters (Belgium), Timo Heikkinen (Finland), Hans Jeekel (The Netherlands), Bo Johansson (Sweden), Poul Juul (Denmark), Anders Kald (Sweden), Henrik Kehlet (Denmark), Najib Khoury (Canada), Anton Klingler (Austria), J Köninger (Germany), Robert Kozol (USA), Bernhard Leibl (Germany), Ian Macintyre (UK), Guy Maddern (Australia), James McGillicuddy (USA), Bertrand Millat (France), Erik Nilsson (Sweden), Pär Nordin (Sweden), Alessandro Paganini (Italy), Giuseppe Pappalardo (Italy), Joan Sala Pedrós (Spain), Leopoldo Sarli (Italy), Rainer Schmitz (Germany), Peter Schrenk (Austria), Andreas Schwarz (Germany), Mark Sculpher (UK), Siegfried Shah (Germany), Zbigniew Sledziñski (Poland), Maciej S̆mietañski (Poland), David Stoker (UK), Arthur Tanner (Eire), Chanvit Tanphiphat (Thailand), Robert Taylor (UK), Jürgen Treckmann (Germany), Jerome Tschudi (Switzerland), Francesc Vallribera (Spain), Petrousjka van den Tol (The Netherlands), Wietske Vrijland (The Netherlands), James Wellwood (UK), Piotr Witkowski (Poland), Jürgen Zieren (Germany).
Footnotes
The EU Hernia Trialists Collaboration was supported by a grant from the European Union BIOMED II work program. The Health Services Research Unit is core funded by the Scottish Executive Health Department. The views expressed are those of the authors and not necessarily those of the funding bodies.
Correspondence: Professor Adrian M. Grant, DM, EU Hernia Trialists Collaboration Secretariat, Health Services Research Unit, University of Aberdeen, Polwarth Building Foresterhill, Aberdeen AB25 2ZD UK.
E-mail: a.grant@abdn.ac.uk
Accepted for publication December 1, 2001
References
- 1.Liem MSL, van Vroonhoven TJMV. Laparoscopic inguinal hernia repair. Br J Surg 1996; 83: 1197–204. [PubMed] [Google Scholar]
- 2.EU Hernia Trialists Collaboration. Mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 2000; 87: 854–9. [DOI] [PubMed] [Google Scholar]
- 3.EU Hernia Trialists Collaboration. Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 2000; 87: 860–7. [DOI] [PubMed] [Google Scholar]
- 4.Condon RE. Groin pain after hernia repair. Ann Surg 2001; 233: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.EU Hernia Trialists Collaboration. Overview of randomised trials of inguinal hernia repair - A European Concerted Action. Surg Endosc 1999; 13: 1030–1. [DOI] [PubMed] [Google Scholar]
- 6.Stewart LA, Clarke MJ. Practical methodology of meta-analyses (overviews) using updated individual patient data. Stat Med 1995; 14: 2057–79. [DOI] [PubMed] [Google Scholar]
- 7.Clarke M, Oxman AD. Cochrane reviewers’ handbook 4.0 [updated July 1999]. The Cochrane Library [Database on CDROM]. In:The Cochrane Collaboration. Oxford: Update Software; 2000, issue 1. Version 4.0.
- 8.Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. BMJ 1994; 309: 1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glassow F. Short stay surgery (Shouldice technique) for repair of inguinal hernia. Ann R Coll of Surg Engl 1976; 58: 133–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Lichtenstein IL, Shulman AG, Amid PK, et al. The tension-free hernioplasty. Am J Surg 1989; 157: 188–93. [DOI] [PubMed] [Google Scholar]
- 11.Stoppa R, Warlaumont CH, Verhaeghe P, et al. Tulle de Dacron et cure chirurgicale des hernies de l’aine. Chirurgie 1983; 109: 847–54. [PubMed] [Google Scholar]
- 12.Sutton AJ, Abrams KR, Jones DR, et al. Systematic reviews of trials and other studies. Health Technol Assess 1998; 2: 19. [PubMed] [Google Scholar]
- 13.Tschudi J, Wagner M, Klaiber CH, et al. Controlled multicenter trial of laparoscopic transabdominal preperitoneal hernioplasty vs Shouldice hernioplasty. Surg Endosc 1996; 10: 845–7. [DOI] [PubMed] [Google Scholar]
- 14.Maddern GJ, Rudkin G, Bessell JR, et al. A Comparison of laparoscopic and open hernia repair as a day surgical procedure. Surg Endosc 1994; 8: 1404–8. [DOI] [PubMed] [Google Scholar]
- 15.Paganini AM, Lezoche E, Carle F, et al. A randomized, controlled, clinical study of laparoscopic vs open tension-free hernia repair. Surg Endosc 1998; 12: 979–86. [DOI] [PubMed] [Google Scholar]
- 16.Vallribera F, Oms LM, Giménez M, et al. Groin hernia repair: comparison of three open techniques. Br J Surg 1997; Supplement II:84.
- 17.Pirski MI, Gacyk W, Witkowski P, et al. Mesh-plug operation for treating inguinal hernia. Randomized studies (Polish). Wiad Lek 1997; L suppl 1:cz. 1. [PubMed]
- 18.Payne JH, Grininger LM, Izawa MT, et al. Laparoscopic or open inguinal herniorrhaphy. A randomized prospective trial. Arch of Surg 1994; 129: 973–81. [DOI] [PubMed] [Google Scholar]
- 19.Payne J, Izawa M, Glen P, et al. Laparoscopic or tension-free inguinal hernia repair? A cost benefit analysis of 200 prospective randomized patients. SAGES, Philadelphia 1996.
- 20.Callesen T, Bech K, Andersen J, et al. Pain after primary inguinal herniorrhaphy: influence of surgical technique. J Am Coll Surg 1999; 188: 355–9. [DOI] [PubMed] [Google Scholar]
- 21.Heikkinen TJ, Haukipuro K, Leppälä; J, et al. Total costs of laparoscopic and Lichtenstein inguinal hernia repairs: A randomized prospective study. Surg Laparosc Endosc 1997; 7: 1–5. [PubMed] [Google Scholar]
- 22.McGillicuddy JE. Prospective randomized comparison of the Shouldice and Lichtenstein hernia repair procedures. Arch Surg 1998; 133: 974–98. [DOI] [PubMed] [Google Scholar]
- 23.Kald A, Anderberg B, Carlsson P, et al. Surgical outcome and cost-minimisation-analyses of laparoscopic and open hernia repair: A randomised prospective trial with one year follow-up. Eur J Surg 1997; 163: 505–10. [PubMed] [Google Scholar]
- 24.Dirksen CD, Beets GL, Go PMNYH, et al. Bassini repair compared with laparoscopic repair for primary inguinal hernia: a randomised controlled trial. Eur J Surg 1998; 164: 439–47. [DOI] [PubMed] [Google Scholar]
- 25.Beets GL, Dirksen CD, Go PMNYH, et al. Open or laparoscopic preperitoneal mesh repair for recurrent inguinal hernia? A randomized controlled trial. Surg Endosc 1999; 13: 323–7. [DOI] [PubMed] [Google Scholar]
- 26.Merello J, Guerra AG, Madriz J, et al. Laparoscopic TEP versus open Lichtenstein hernia repair. Randomized trial. Surg Endosc 1997; 11: 545. [Google Scholar]
- 27.Kozol R, Lange PM, Kosir M, et al. A prospective, randomized study of open vs laparoscopic inguinal hernia repair. Arch Surg 1997; 132: 292–5. [DOI] [PubMed] [Google Scholar]
- 28.Barkun JS, Wexler MJ, Hinchey EJ, et al. Laparoscopic versus open inguinal herniorrhaphy: Preliminary results of a randomized controlled trial. Surgery 1995; 118: 703–10. [DOI] [PubMed] [Google Scholar]
- 29.The MRC Laparoscopic Groin Hernia Trial Group. Laparoscopic versus open repair of groin hernia: a randomised comparison. Lancet 1999; 354:185–90. [PubMed]
- 30.Barth RJ, Burchard KW, Tosteson A, et al. Short-term outcome after mesh or Shouldice herniorrhaphy: A randomized, prospective study. Surgery 1998; 123: 121–6. [PubMed] [Google Scholar]
- 31.Filipi CJ, Gaston-Johansson F, McBride PJ, et al. An assessment of pain and return to normal activity. Laparoscopic herniorrhaphy vs open tension-free Lichtenstein repair. Surg Endosc 1996; 10: 983–6. [DOI] [PubMed] [Google Scholar]
- 32.Heikkinen T, Haukipuro K, Hulkko A. A cost and outcome comparison between laparoscopic and Lichtenstein hernia operations in a day-case unit. Surg Endosc 1998; 12: 1199–203. [DOI] [PubMed] [Google Scholar]
- 33.Heikkinen T, Haukipuro K, Koivukangas P, et al. A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus Lichtenstein hernia operation among employed patients. Surg Laparosc Endosc 1998; 8: 338–44. [PubMed] [Google Scholar]
- 34.Castoro C, Polo P, Pignataro M, et al. Shouldice vs Lichtenstein technique of inguinal hernia repair: preliminary results of a multicentric randomized prospective trial. Br J Surg 1996; 83 Supplement II: 72.
- 35.Khoury N. A randomized prospective controlled trial of laparoscopic extraperitoneal hernia repair and mesh-plug hernioplasty: A study of 315 cases. Journal of Laparoendoscopic & advanced surgical techniques 1998; 8: 367–72. [DOI] [PubMed] [Google Scholar]
- 36.Pappalardo G, Guadalaxara A, Illomei G, et al. The Bassini techniques versus Tension-free repair. A prospective randomised trial. Chirurgia 1995; 8: 293–5. [Google Scholar]
- 37.van den Tol MP, de Lange DCD, Luijendijk RW, et al. Conventional vs open ’tension-free’ hernioplasty: preliminary results of a prospective multicentre randomized trial. Br J Surg 1996; 83 Supplement II: 72.8653371 [Google Scholar]
- 38.Johansson B, Hallerbäck B, Glise H, et al. Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair. A randomized multicenter trial (SCUR hernia repair study). Ann Surg 1999; 230: 225–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leibl B, Däubler P, Schwarz J, et al. Standardized laparoscopic hernia repair (TAPP) vs Shouldice repair. Results of a randomized trial (German). Chirurg 1995; 66: 895–8. [PubMed] [Google Scholar]
- 40.Aitola P, Airo I, Matikainen M. Laparoscopic versus open preperitoneal inguinal hernia repair: A prospective randomised trial. Ann Chir 1998; 87: 22–5. [PubMed] [Google Scholar]
- 41.Hauters P, Meunier D, Urgyan S, et al. Prospective randomised study comparing laparscopic and Shouldice technique in the treatment of unilateral inguinal hernia (French). Ann Chir 1996; 50: 776–81. [PubMed] [Google Scholar]
- 42.Kunz R, Schwarz A, Beger HG. Laparoscopic transperitoneal hernia repair vs Shouldice herniorrhaphy - Preliminary results of a prospectively randomised trial. Chirurgie Endoscopique, Numero Hors Serie 1993; 7: 12–3. [Google Scholar]
- 43.Stoker DL, Spiegelhalter DJ, Singh R, et al. Laparoscopic versus open inguinal hernia repair: randomised prospective trial. Lancet 1994; 343: 1243–5. [DOI] [PubMed] [Google Scholar]
- 44.Wellwood J, Sculpher MJ, Stoker D, et al. Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ 1998; 317: 103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bessell JR, Baxter P, Riddell P, et al. A randomised controlled trial of laparoscopic extraperitoneal hernia repair as a day surgical procedure. Surg Endosc 1996; 10: 495–500. [DOI] [PubMed] [Google Scholar]
- 46.Schmitz R, Treckmann J, Schneider K. The tension-free technique in open inguinal hernia repair. A prospective randomised study concerning postoperative pain (German). Chirurg 1997; 68: 259–63. [DOI] [PubMed] [Google Scholar]
- 47.Zieren J, Zieren HU, Said S, et al. Prospective randomized study comparing laparoscopic and open tension-free inguinal hernia repair with Shouldice’s operation. Am J Surg 1998; 175: 330–3. [DOI] [PubMed] [Google Scholar]
- 48.Köninger JS, Oster M, Butters M. Management of inguinal hernia: a comparison of current methods (German). Chirurg 1998; 69: 1340–4. [DOI] [PubMed] [Google Scholar]
- 49.Liem MSL, Van der Graaf Y, Van Steensel CJ, et al. Comparison of conventional anterior surgery and laparosopic surgery for inguinal hernia repair. N Engl J Med 1997; 336: 1541–7. [DOI] [PubMed] [Google Scholar]
- 50.Friis E, Lindahl F. The tension-free hernioplasty in a randomized trial. Am J Surg 1996; 172: 315–9. [DOI] [PubMed] [Google Scholar]
- 51.Schrenk P, Woisetschlager R, Reiger R, et al. Prospective randomised trial comparing postoperative pain and return to physical activity after transabdominal preperitoneal, total preperitoneal or Shouldice technique for inguinal hernia repair. Br J Surg 1996; 83: 1563–6. [DOI] [PubMed] [Google Scholar]
- 52.Juul P, Christensen K. Randomized clinical trial of laparoscopic versus open inguinal hernia repair. Br J Surg 1999; 86: 316–9. [DOI] [PubMed] [Google Scholar]
- 53.Sarli L, Pietra N, Choua O, et al. Prospective randomised comparative study of laparoscopic hernioplasty and Lichtenstein tension-free hernioplasty (Italian). Acta Biomed Ateneo Parmense 1997; 68: 5–10. [PubMed] [Google Scholar]
- 54.Nathanson L, Adib R, Branild F. Randomised trial of open and laparoscopic inguinal hernia repair. SAGES, Philadelphia 1996.
- 55.Neagu S, Costea R, Badea V, et al. Not “gold standard” but “gold option” of inguinal hernia repair. A prospective randomized study. Hernia in the 21st century. Toronto: 2000.
- 56.Gontarz W, Wolanski L, Leksowski K. A comparison of two “tension free” inguinal hernia repair methods - laparoscopic hernioplasty vs anterior mesh technique. Br J Surg 1998; 85 Supplement II: 101.9462395 [Google Scholar]
- 57.Damamme A, Samama G, D’Alche-Gautier MJ, et al. Medicoeconomic evaluation of inguinal hernia repair: Shouldice repair vs laparoscopy (French). Ann Chir 1998; 52: 11–6. [PubMed] [Google Scholar]
- 58.Bostanci BE, Tetik C, Ozer S, et al. Posterior approaches in groin hernia repair with prosthesis: open or closed. Acta Chir Belg 1998; 98: 241–4. [PubMed] [Google Scholar]
- 59.Danielsson P, Isacson S, Hansen MV. Randomised study of Lichtenstein compared with Shouldice inguinal hernia repair by surgeons in training. Eur J Surg 1999; 165: 49–53. [DOI] [PubMed] [Google Scholar]
- 60.Lawrence K, McWhinnie D, Goodwin A, et al. Randomised controlled trial of laparoscopic versus open repair of inguinal hernia: early results. BMJ 1995; 311: 981–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Champault G, Benoît J, Lauroy J, et al. Inguinal hernia in adults. Laparoscopic surgery vs Shouldice’s operation. Controlled randomised study in 181 patients. Preliminary results (French). Ann Chir 1994; 48: 1003–8. [PubMed] [Google Scholar]
- 62.Champault GG, Rizk N, Catheline JM, et al. Inguinal Hernia Repair. Totally preperitoneal laparoscopic approach versus Stoppa operation: Randomized trial of 100 cases. Surg Laparosc Endosc 1997; 7: 445–50. [PubMed] [Google Scholar]
- 63.Prior MJ, Williams EV, Shukla HS, et al. Prospective randomized controlled trial comparing Lichtenstein with modified Bassini repair of inguinal hernia. J R Coll Surg Edinb 1998; 43: 82–86. [PubMed] [Google Scholar]
- 64.Picchio M, Lombardi A, Zolovkins A, et al. Tension-free laparoscopic and open hernia repair: randomized trial of early results. World J Surg 1999; 23: 1004–1009. [DOI] [PubMed] [Google Scholar]
- 65.Kux M, Fuchsjäger N, Feichter A. Lichtenstein-Patch versus Shouldice-Technique in primary inguinal hernia at high risk of recurrence (German). Chirurg 1994; 65: 59–62. [PubMed] [Google Scholar]
- 66.Rukas R, Strupas K, Rukiene A. The comparison of Lichtenstein and Bassini repairs for inguinal hernia. Hernia in the 21st century. Toronto: 2000.
- 67.Ramon JM, Carulla X, Hidalgo JM, et al. Study of quality of life in relation with the health after the surgery of the endoscopic inguinal hernia vs conventional. Br J Surg 1998; 85 Supplement II: 18. [Google Scholar]
- 68.Tanphiphat C, Tanprayoon T, Sangsubhan C, et al. Laparoscopic vs open inguinal hernia repair. A randomized, controlled trial. Surg Endosc 1998; 12: 846–51. [DOI] [PubMed] [Google Scholar]
- 69.Vale L, McCormack K, Scott N, et al. The effectiveness and cost-effectiveness of laparoscopic compared to open surgery for inguinal hernia repair. Report commissioned by National Institute of Clinical Effectiveness, January 2001, www.nice.org.uk