Abstract
Objective
To break out subcategories of atypical and suspicious cytologic interpretations of thyroid aspirations and correlate those with final histologic diagnosis.
Summary Background Data
Fine-needle aspiration (FNA) of thyroid nodules has become the primary diagnostic tool in the initial evaluation of thyroid nodules. Management of thyroid nodules is based on statistical data correlating a specific cytologic reading with the probability of malignancy. Two particular cytologic readings that frustrate both cytopathologists and surgeons are follicular neoplasms and cells that show atypia. In most reported series, follicular neoplasms and cells showing atypia are included in a broad “suspicious” category, with reported overall malignancy rates generally between 20% and 30%. However, there is interest in determining whether these suspicious lesions can be subcategorized, allowing a more accurate assessment of the risk of malignancy. In addition, there is recent evidence that the incidence of follicular cancer may be declining in this country, possibly decreasing the probability that a “follicular neoplasm” will prove to be a follicular cancer.
Methods
From January 1994 through December 2000, 709 thyroid FNAs were performed at a single institution. Those interpreted as suspicious and the subsequent histologic reports were reviewed. From this set, four specific categories were defined, and the clinical records for patients whose cytology matched these categories form the subject of this study. These four categories are follicular neoplasms without atypia, follicular neoplasms with atypia, atypia, and suspicious for malignancy. In addition, lesions with nondiagnostic cytology were reviewed. Only lesions for which there was histologic follow-up were considered.
Results
Ninety-eight aspirates were categorized as follicular neoplasms without atypia, follicular neoplasms with atypia, or atypia alone. Of 74 follicular neoplasms without atypia, only 5 (6.8%) were malignant, and none of these were follicular thyroid cancers. Nine of the lesions were follicular neoplasms with atypia, and four (44.4%) of these were malignant, including two that were invasive follicular cancers. Of 15 lesions showing atypia alone, 3 (20%) were malignant, all of which were papillary thyroid cancers. Twenty-five additional patients had lesions highly suspicious for malignancy. Twenty-one (84%) of these lesions were malignant, the majority being papillary thyroid cancers. Only one was a follicular cancer. Fifty patients with nondiagnostic cytology had subsequent action taken. Thirty-one of these lesions were resected, with five (16.1%) proving to be malignant.
Conclusions
Thyroid nodules whose FNA is diagnosed as highly suspicious for malignancy should be resected unless there are significant contraindications to a surgical procedure. The extremely low rate (2%) of invasive follicular cancers among all follicular neoplasms may reflect changing histologic criteria for follicular carcinoma, a true change in the disease frequency, or both. For thyroid nodules whose cytology shows a follicular neoplasm without atypia, malignancy rates of 8% or less may allow nonsurgical options, including reevaluation in selected populations. Continued efforts to correlate malignancy rates to specific cytologic criteria will allow patients to make more informed decisions regarding their medical care.
Fine-needle aspiration (FNA) of the thyroid gland has become the dominant modality used to assess the need for resection of thyroid nodules. In the United States, its utility was popularized during the late 1970s and early 1980s through a series of articles from a number of institutions. 1–7 In classifying the aspiration samples, the majority of pathologists grouped the specimens into one of four general diagnostic categories: malignant, suspicious, benign, and indeterminate or nondiagnostic. 1–5,7,8 Although cytologic discrimination in the malignant and benign categories was considered excellent, with low false-negative rates and high predictive values, lesions falling into the suspicious category were reported to have malignancy rates in the 20% to 40% range. 4,5,7 This category is largely composed of follicular neoplasms as well as lesions with features of malignancy but not quite meeting the histologic criteria for classification into the malignant group.
The cytologic diagnosis of follicular neoplasm has continued to be a frustrating entity for pathologists, surgeons, and patients. The major issue has been the concern that such a lesion will be a follicular cancer. The definition of a follicular cancer is primarily based on histologic evidence of capsular or vascular invasion, extrathyroidal tissue invasion, or nodal or distant metastasis. 9 Thus, there has been the perceived need to completely excise the lesion to allow a complete examination of the capsule, given the relatively high reported probability of cancer. 10
Recently, two factors that may affect the management of follicular neoplasms have received attention. The first is preliminary evidence that the true incidence of invasive follicular cancers may be declining in this country. 11,12 The second is growing expertise among cytopathologists and evidence that cytologic atypia by itself or in conjunction with a follicular pattern may define a subgroup that is more likely to be malignant. 13,14
Given these recent observations, the hypotheses driving this current study are that the probability that a “follicular neoplasm” is a follicular cancer is quite low, and that thyroid lesions traditionally lumped in the “suspicious” category can be separated out, and individual assessments of the risk for malignancy can be determined.
METHODS
Using a computerized database, all thyroid cytology reports at Vanderbilt University from January 1994 through December 2000 were retrieved. Each cytology report was reviewed and the corresponding surgical pathology report, if resection had been performed, was retrieved and reviewed. From this set, five specific subcategories were defined, and the clinical records for patients whose cytology matched these categories form the subject of this study. These five categories are follicular neoplasms without atypia, follicular neoplasms with atypia, atypia, suspicious for malignancy, and nondiagnostic. Individual cytology slides were not reevaluated unless the original cytology report was so ambiguous that a category assignment could not be reliably made. This was done to preserve the prospective relationship between a cytology report and the action taken based on that report. Cytology reports classified as adequate and consistent with a benign process are not included in this report unless the lesion was ultimately resected. Cytology reports that were considered diagnostic of malignancy are also not the subject of this report. Aspirates were signed out according to standard criteria, as follows.
Adequacy was evaluated according to guidelines published by the Papanicolaou Society 15 and Goeller et al. 16 In brief, a sample was considered adequate if there were five or six well-visualized, well-preserved groups of follicular epithelium, each group containing at least 10 cells; aspirates with fewer epithelial cells were deemed adequate if the clinical features and cytologic pattern were those of a colloid nodule or benign cyst. Aspirates that fell short of the adequacy criteria were designated “nondiagnostic.”
Lesions diagnosed as “follicular neoplasm without atypia” (Fig. 1) were characterized by a high degree of cellularity, small uniform follicles or syncytial sheets, uniform cytology without atypia of cells, and scant or absent colloid. 17
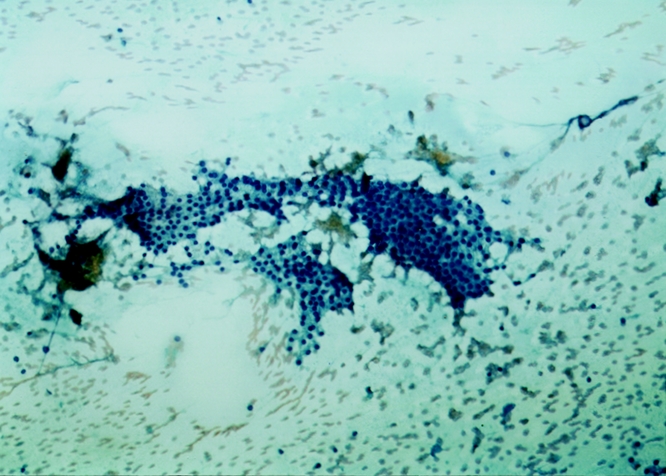
Figure 1. Follicular neoplasm without atypia. This field shows two large sheets of evenly spaced uniform follicular cells; no colloid is apparent. Papanicolaou stain, ×62.5 original magnification.
A designation of “follicular neoplasm with atypia” (Fig. 2) was assigned to cellular aspirates with scant or absent colloid if any of the following were present: crowding of cells in follicles; irregular or variably sized follicles; significant numbers of single cells; or cytologic atypia including pleomorphism, enlarged nuclei, nuclear grooves, coarse or irregular chromatin, prominent or multiple nucleoli, or atypical or numerous mitotic figures. 17
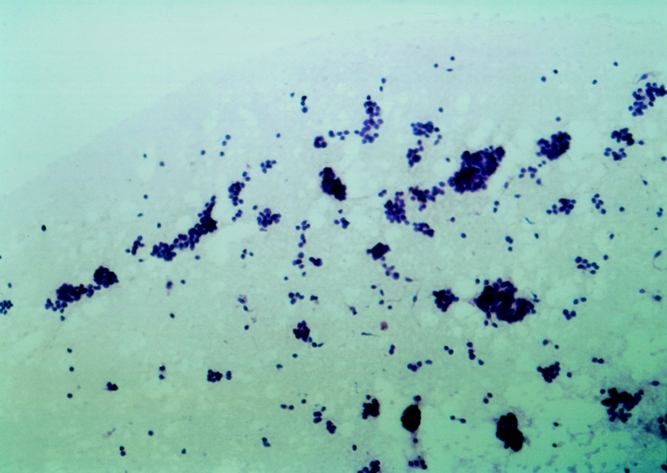
Figure 2. Follicular neoplasm with atypia. Numerous follicular epithelial cells are in microfollicules, some of which show crowding. Follicle size varies. Hematoxylin and eosin, ×62.5 original magnification.
Aspirates were called “atypical” (Fig. 3) if individual epithelial cells manifested mild abnormalities not within the spectrum of normal epithelial cells, and the low-power pattern criteria for follicular neoplasm were not met. These included cells that showed pleomorphism, enlarged nuclei, or nuclear grooves. 17
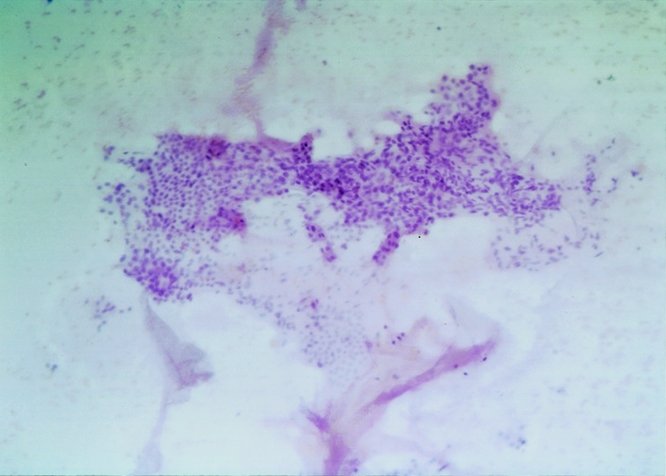
Figure 3. Atypia. Colloid and follicular cells are present in approximately equal amounts, but the sheet of epithelium shows crowding and disorganized architecture. Hematoxylin and eosin, ×62.5 original magnification.
Aspirates diagnosed as suspicious for malignancy (Fig. 4) manifested varying cytologic abnormalities associated with malignancy (nuclear membrane irregularity, nucleolar abnormalities, abnormal nucleus-to-cytoplasm ratios) but were not frankly malignant on cytologic grounds alone.
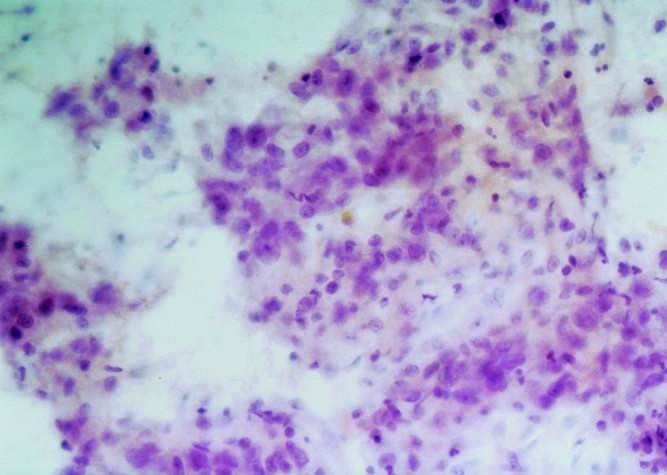
Figure 4. Suspicious for malignancy. This sheet of cells shows crowding, disorganization, nuclear pleomorphisms, and variation in the presence and size of nucleoli. Nuclear membranes are irregular as well. Hematoxylin and eosin, ×250 original magnification.
FNAs were performed using either a 23- or 25-gauge needle on a 10-cc3 syringe attached to a pistol-type handle. Nodules were sampled with or without ultrasound guidance two or three times, each pass continuing for 15 to 20 excursions until material was apparent in the needle hub.
Smears were prepared by cytotechnologists using a two-slide contact-and-smear technique. Smears were fixed in 90% ethanol and stained with either Papanicolaou or hematoxylin and eosin stains. Needles were rinsed in saline and the rinsings were processed with a cytocentrifuge and stained with Papanicolaou’s stain. 18 Histopathologic diagnoses were rendered according to standard practice. 19
Statistical analysis was performed using the Mann-Whitney test and by determining the phi coefficient. 20 Calculations were performed using SPSS-Mac version 10 (SPSS Inc., Chicago, IL). P < .05 was the limit of statistical significance.
RESULTS
From January 1994 through December 2000, 709 FNAs were performed at Vanderbilt University. Of these, 98 were categorized as follicular neoplasm without atypia, follicular neoplasm with atypia, or atypia alone. These 98 patients were 93% female, 95% white, and 3% African American. The patients had a mean age of 49 years (range 16–83). Only two patients had a history of radiation exposure.
Follicular Neoplasms
Of these 98 patients, 74 had cytology consistent with a follicular neoplasm without atypia (Table 1). Nine patients had cytology consistent with a follicular neoplasm with atypia. Overall, 10.8% of all follicular neoplasms proved malignant on permanent sections. However, 44.4% of the follicular lesions with atypia were malignant, whereas only 6.8% of the follicular lesions without atypia proved malignant on permanent section (P < .001 follicular neoplasms with atypia vs. follicular neoplasms without atypia). The malignant lesions associated with a follicular neoplasm with atypia included two follicular cancers, one minimally invasive follicular cancer, and one follicular variant of papillary thyroid cancer. The malignant lesions associated with a follicular neoplasm without atypia included four follicular variants of papillary thyroid cancer and one papillary thyroid cancer. There were no follicular cancers in this latter group.
Table 1. PATHOLOGY ON PERMANENT SECTION
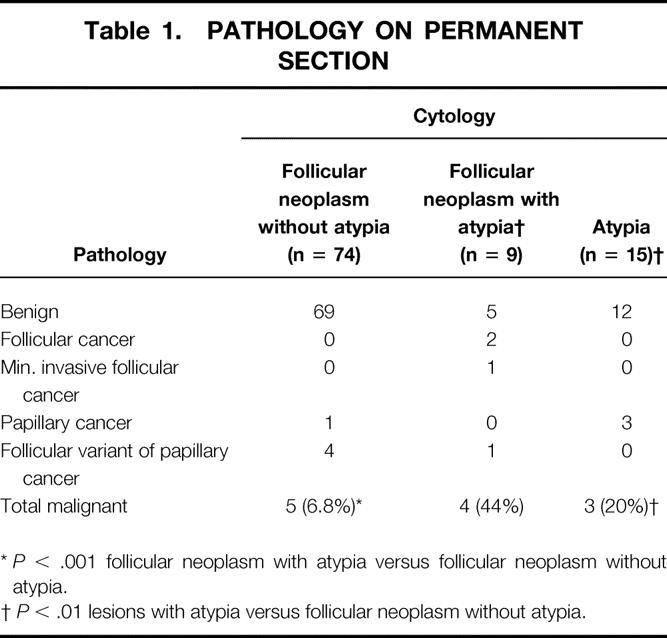
*P < .001 follicular neoplasm with atypia versus follicular neoplasm without atypia.
†P < .01 lesions with atypia versus follicular neoplasm without atypia.
Atypia
Fifteen of the 98 patients had thyroid lesions showing atypia but lacked pattern criteria for a follicular neoplasm (see Table 1). On permanent sections, 3 of the 15 (20%) lesions were malignant; all 3 were papillary thyroid cancers (P < .01 all lesions with atypia vs. follicular neoplasms without atypia).
Histologically Benign Lesions
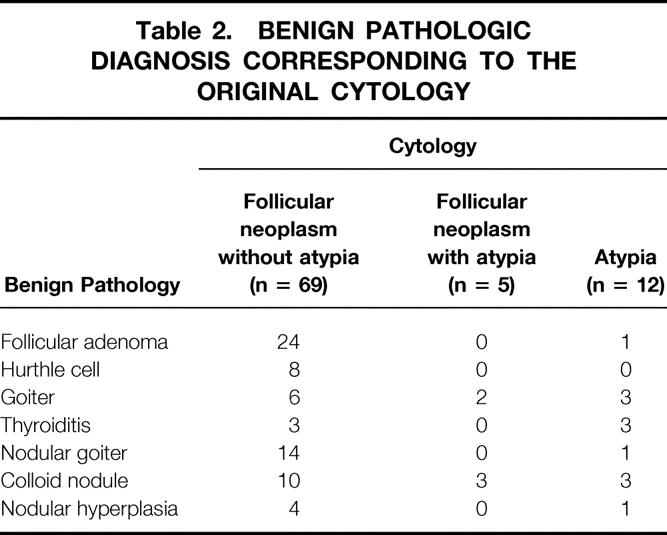
Eighty-six of the 98 patients with either follicular neoplasms or atypia were diagnosed with benign lesions on permanent sections (Table 2). Sixty-nine had been diagnosed as follicular neoplasms without atypia, and only 32 (46.4%) were follicular adenomas or Hurthle cell adenomas. The 24 follicular adenomas had a mean maximum diameter of 2.3 ± 1.1 cm (mean ± SD, range 0.5–4.5); the eight Hurthle cell adenomas had a mean maximum diameter of 3.1 ± 1.26 cm (range 1.5–4.5). In comparison, the two invasive follicular thyroid cancers had maximum diameters of 4.0 and 5.8 cm and occurred in men 48 and 67 years of age.
Table 2. BENIGN PATHOLOGIC DIAGNOSIS CORRESPONDING TO THE ORIGINAL CYTOLOGY
Nondiagnostic FNA
Fifty patients who had initially nondiagnostic FNAs had subsequent action taken (Fig. 5). On repeat aspiration, 10 were again nondiagnostic, and 8 of these lesions were resected. Of these eight lesions, seven were benign. On repeat aspiration, 21 were adequate and consistent with a benign lesion. Four of these lesions were resected and all were benign. Nineteen of the lesions that initially had nondiagnostic cytology were resected without repeat aspiration. Four of the lesions were malignant. Overall, 31 of these patients underwent thyroidectomy and 5 had malignant lesions (16.1%), none of which were follicular cancers.
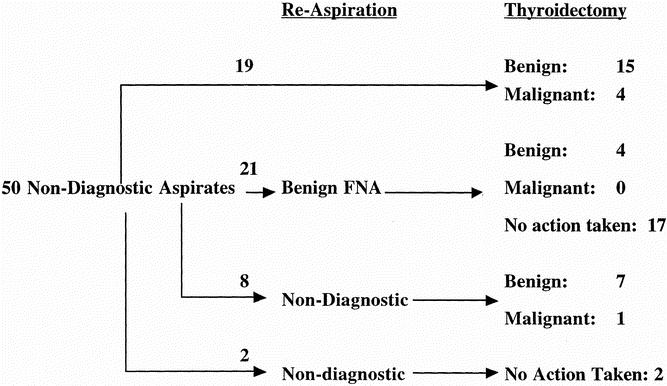
Figure 5. Actions taken on 50 thyroid aspirates that were initially considered to be nondiagnostic by cytologic criteria.
Suspicious for Malignancy
Twenty-five additional patients had thyroid nodules suspicious for malignancy. Twenty-one (84%) were malignant on permanent section (P < .001 vs. follicular neoplasms without atypia). These included 1 follicular cancer, 1 medullary thyroid cancer, 1 lymphoma, 15 papillary cancers, and 3 follicular variants of papillary thyroid cancer. Four of the lesions were benign on permanent section. These included two colloid nodules and two follicular adenomas.
False-Negative FNA
Forty patients who had FNA results consistent with a benign process underwent thyroidectomy for various reasons. Thirty-six of these lesions were benign on permanent section. Four of the resected specimens contained thyroid malignancies, all of which were papillary thyroid cancer. One of these cancers was an occult lesion that clearly was not the lesion originally aspirated. These data yield a known false-negative rate of 7.5% (P = NS vs. follicular neoplasm without atypia).
DISCUSSION
The definitive distinction of follicular adenomas from well-differentiated and low-grade follicular carcinomas rests on examination of multiple permanent sections of lesion and capsule and may be difficult even then. Invasion of the lesion’s capsule or vascular spaces is the only reliable criterion for a definite diagnosis of malignancy but is not a feature that may be recognized on an aspirate. This fact has hindered acceptance of thyroid FNA beyond general triage to surgical versus medical management. In addition, despite its extensive use in Europe, acceptance of FNA cytology by pathologists as a standard diagnostic technique came late to the United States, primarily due to the absence of architectural information in aspirates, but also due to concern about needle tract seeding, an issue that has essentially been resolved with the use of “fine” (22 gauge or less) needles. 18,21 The use of FNA cytology for the evaluation of thyroid nodules in the United States finally gained attention in the late 1970s and 1980s through a number of clustered publications. 4–6 Acceptance was obtained because adequate aspirations were obtained greater than 95% of the time, 4,22 false-positive rates were quite low, 5 and false-negative rates were considered acceptable. 22 Through the use of FNA, the percentage of patients who underwent thyroid operations decreased while the yield of thyroid carcinomas increased and the cost of medical care per patient decreased. 6
Because the use of FNA for the evaluation of thyroid nodules did not really come into widespread use until the mid-1980s, systematic and detailed information regarding the aspiration biopsy features of various thyroid lesions was therefore slow to accumulate. Searching the Ovid medical literature database for the combination of “fine-needle aspirates” and “thyroid” yields 36 papers between 1960 to 1980, and 398 and 404 between 1981 to 1990 and 1991 to 2000, respectively. The past 20 years have therefore seen great advances in the pathologist’s knowledge of thyroid cytopathology. Studies that examine large series of aspirates with careful and thorough correlation with surgical pathology have greatly refined the ability of the cytopathologist to classify thyroid lesions in general as “surgical” or “medical” and to identify features of cellular aspirates that permit subcategorization of biopsied lesions into groups with significantly differing likelihoods of being malignant. The data from the current study show that an aspirate that meets the criteria for a follicular neoplasm but is lacking in cytologic and architectural atypia is quite unlikely to be malignant. These data suggest that such subcategorization can be sufficiently precise to allow differential management of individual patients with differing risk levels and additional medical comorbidities.
An issue against which all FNA results need to be compared is the false-negative rate associated with FNA. This tends to be the more difficult number to obtain reliably because it is based only on lesions that are resected after FNA has suggested benign pathology. Walfish et al 2 in 1977 reported a false-negative rate of 4% to 11%, depending on the type of thyroid lesion aspirated. Grant at al 5 reported a false-negative rate of 0.7% on 439 lesions with benign aspirates. In 1986, Boey et al 22 reported a false-negative rate of approximately 5%, depending on what lesions were included, but also summarized the false-negative rates reported in 13 other studies and derived a combined false-negative rate of 5.0%, with individual rates ranging from 1.7% to 16.1%, based on a total of 846 resected lesions. In the current study, 40 lesions with aspirates consistent with a benign process were resected, yielding a fairly comparable false-negative rate of 7.5%. Although it is highly likely that the actual false-negative rate is slightly less than what is reported in the literature, it would be a correct assumption that there are well-differentiated thyroid carcinomas that are never resected.
The focus of the current study was thyroid aspirates that have traditionally been placed in what is often defined as the “suspicious” and “atypical” category. Early reports tended to group adequate cytologic specimens into one of three categories. 3–5,7 All included categories of aspirates that were diagnostic for malignancy or consistent with a benign process, but the suspicious category was defined as intermediate, atypical, suspicious for malignancy, or suspicious in these various publications. In the suspicious category, Grant et al 5 defined suspicious as suggestive but nonconclusive for malignancy, containing significant nuclear atypia, or having a pattern consistent with a follicular neoplasm. Overall, 23% of the lesions in this category proved to be malignant. Another report from the same institution focused specifically on thyroid aspirates from the suspicious category. 7 Of 253 patients with suspicious cytology, 71% of these lesions were follicular or Hurthle cell neoplasms. The other 29% were either highly suggestive of malignancy or notable for significant atypia. Overall, 24% of the lesions in this group were malignant, including 14 follicular cancers. However, from the subset of only the follicular and Hurthle cell neoplasms, the malignancy rate was 12%. In general, subsequent studies have maintained the concept of three categories in reporting adequate thyroid aspirations.
In 1995 Chen et al 10 retrospectively reviewed follicular neoplasms from 73 patients who underwent thyroidectomies from 1984 to 1994. In this series, 31% proved to be malignant. Of the malignant lesions, 18 were either follicular or Hurthle cell carcinomas; only 5 were papillary or follicular variants of papillary thyroid cancers. Recently, Udelsman et al 23 reported a prospective study on 61 patients with follicular neoplasms from the same institution as Chen et al 10 but from a more recent group of patients with no overlap (personal communication). Of these, 10 (16%) were malignant, 1 of which was a follicular cancer (presumably a widely invasive follicular carcinoma) and 4 were minimally invasive follicular or Hurthle cell carcinomas. McHenry et al 24 recently reported on 75 indeterminate lesions, which included follicular and Hurthle cell neoplasms. Of these, 23% were malignant and included 7 follicular or Hurthle cell carcinomas and 10 papillary lesions. In the current study, only 10.8% of follicular neoplasms proved malignant, a rate significantly less that that reported by Chen et al 10 and McHenry et al 24 and only somewhat less than that reported by Udelsman et al 23 but quite similar to that reported by Gharib et al. 7 The fact that there was such a large number of follicular and Hurthle cell carcinomas in the report by Chen et al 10 and the fact that these lesions were more frequent than papillary thyroid cancers may reflect an unusual patient grouping during that period.
In the study reported by Grant et al, 5 the overall malignancy rate of lesions in the suspicious category was 23%. In the current study, collating the lesions that were follicular neoplasms, with or without atypia, the lesions with atypia alone, and the lesions highly suspicious for malignancy yielded an overall malignancy rate of 26.8%, similar to that reported by Grant et al. However, notable in the current study was the fact that only 3 of 83 follicular neoplasms (3.6%) were follicular cancers.
In countries with adequate iodine intake, the frequency of follicular thyroid cancers among thyroid malignancies is approximately 10%. 19,25 However, high dietary iodine intake may promote papillary thyroid cancer over follicular cancer. 25 Several recent reports have raised the question of whether the incidence of follicular thyroid cancer is decreasing in the United States. LiVolsi and Asa 12 reported that fewer than 2% of malignant thyroid lesions seen in LiVolsi’s consultation practice were minimally invasive follicular thyroid cancers and that widely invasive follicular thyroid cancers were even rarer. The authors raised the point that the decline in follicular carcinoma may be attributable not only to changing diagnostic criteria but also to a relative increase in the incidence of papillary carcinoma. The latter may be secondary to increased dietary intake of iodine in the United States. 12 Along this same theme, DeMay 11 recently reported that of 197 histologically documented thyroid malignant neoplasms at the University of Chicago from 1994 to 1998, including 164 papillary thyroid carcinomas, there were only 2 follicular carcinomas, and 1 of these was minimally invasive. In the current study, of 83 “follicular neoplasms,” where traditionally a significant concern prompting surgical resection has been the “high” probability of follicular thyroid cancer, only 3 of the lesions (3.6%) were follicular cancers, and 1 of these was minimally invasive. These data are consistent with the hypothesis that the incidence of widely invasive follicular carcinoma may be decreasing.
Atypia has generally been considered as a separate feature within the suspicious category and has generally not been considered in combination with follicular neoplasms. 7 When the 83 follicular neoplasms were subdivided into those with and without atypia, no follicular carcinomas, minimally invasive or widely invasive, were associated with a follicular neoplasm without atypia. However, 7 of 24 lesions with atypia were malignant and 44% of follicular neoplasms with atypia were malignant. Although these numbers are small, they raise the issue of atypia (as defined above) as an independent risk factor in interpreting cytology. This issue of atypia, whether considered alone or as a feature in association with follicular neoplasms, and its relationship to malignancy has been the subject of recent interest and debate. Greaves et al 26 reported on 96 patients diagnosed with follicular lesions and found no relationship between atypia and malignancy. Similarly, McHenry et al 24 found no relationship between atypia and malignancy in follicular neoplasms. However, Carpi et al 14 reported that follicular neoplasms without atypia had a risk of malignancy of 7%, and this risk increased to 21% with atypia. Similarly, Kelman et al 13 reported on 368 surgical cases with 484 corresponding cytology reports. In their study, atypia alone or in association with a follicular thyroid neoplasm was associated with a higher risk of malignancy. The authors reported that follicular neoplasms without atypia had a malignancy rate of 6.5%. This rate increased to 44% with atypia, rates almost identical to those reported in the current study. In fact, by separating out the follicular neoplasms without atypia, the rate of malignancy in the current study was indistinguishable from cytologically benign lesions (false-negative group), which had a rate of malignancy of 7.5%.
Our data support a reexamination of how suspicious thyroid aspirates are evaluated and grouped. By defining such lesions more specifically and categorizing them into follicular neoplasms without atypia, follicular neoplasms with atypia, atypia, and highly suspicious for malignancy, it is likely that physicians and patients will have a more accurate estimation of risk, allowing more informed decisions to be made. Although we believe that all patients with follicular lesions or atypia should be considered for surgical resection, patients with significant underlying medical conditions or small follicular neoplasms without atypia may be candidates for either nonoperative management or specific protocols designed to further investigate this group. Because the majority of the malignancies in this group were papillary thyroid cancers or follicular variants of papillary cancer, protocols that may be aimed at better identifying follicular variants of papillary thyroid cancer 27–29 or that may be designed to evaluate the role of reaspiration may need to be considered. For patients with significant underlying medical conditions and aspirates considered low risk, thyroxine suppression may also be an option.
Discussion
Dr. Terry C. Lairmore (St. Louis, MO): This report represents a careful retrospective review of thyroid fine-needle aspirations at a single institution. The major focus of the study is to define the true risk of malignancy in nodules that are characterized as follicular neoplasms by fine-needle aspiration. In current practice, nodules with this cytologic diagnosis are likely to be included in a broad category of indeterminate lesions that are usually subjected to thyroid lobectomy. In this study the authors present data to suggest that subcategorization of follicular neoplasms according to the presence or absence of atypia provides a critical separation of high and low malignant potential. I have the following specific comments and questions for Dr. Goldstein.
My first question relates to the potential for selection bias in the current study. During the study time period of about 6 years, a total of 709 fine-needle aspirations were performed. For obvious reasons, the analysis was limited to those specimens for which a final pathology result was available; therefore, the data set represents a select group of patients that underwent surgical resection on the basis of either suspicious cytology, the presence of symptoms or enlarging mass, or the preference of the patient and/or surgeon. What is the potential effect of selection bias on your results, and do you think that the true rate of malignancy is higher or lower than that reported for this group?
My second question relates to the potential for variability in the accuracy of the cytologic interpretation. Although fine-needle aspiration represents our first-line tool for the prediction of malignant risk, the clinical usefulness of the technique is highly dependent on the skill and experience of the cytopathologist interpreting the results. In this study there are clear criteria that are defined for the presence of atypia, the critical factor in a follicular lesion, and based on these distinctions there is a very large discrepancy in the prevalence of malignant lesions in the final pathology; specifically, about 6.8% for those lesions without atypia versus 44% for follicular lesions that do have atypia present. How would you reconcile these potential pitfalls and subtleties of interpretation with the placement of a thyroid nodule in the low-risk group?
Third, the conclusion offers a suggestion that patients with a low-risk cytologic diagnosis might reasonably be assigned to conservative management or medical therapy according to other patient factors or comorbidities. The prevailing practice of performing a diagnostic thyroid lobectomy in patients with a solitary nodule that is interpreted as indeterminate really reflects the low morbidity of the intervention and the very high cure rate of small, differentiated thyroid cancers that are completely resected. Even if you consider the carefully defined group of follicular lesions without atypia, a final malignancy rate of 6% to 10% might still be too high to recommend observation alone, and I ask for your comments regarding these factors.
I concur with you that follicular lesions, certainly in my practice, seem to be vanishingly small.
Then finally, I would like to ask Dr. Goldstein to comment on the emerging role of molecular genetic techniques such as the telomerase assay, RAS protooncogene, and others to discriminate between cytologic specimens with high and low malignant potential. In the current era of defining the neoplastic potential of malignancies at the molecular level, these techniques might provide a further tool for the discrimination of patients with high-risk lesions.
This is an important paper that offers support for two essential tenets: the suggestion that follicular lesions without atypia have a very low malignant potential, and then support for the apparent decline in the incidence of invasive follicular cancers. I commend Dr. Goldstein for his contribution, and I thank the Association for the privilege of the floor.
Dr. Robert Udelsman (New Haven, CT): Dr. Goldstein and his colleagues from Vanderbilt have addressed an important problematic and contentious area in thyroid disease. The heterogeneous group of follicular neoplasms of the thyroid contain both benign and malignant disease, and unfortunately cytopathologists are rarely able to discriminate benign from malignant lesions. The data presented very nicely by Dr. Goldstein today suggest that he and his group in Nashville can discriminate based on atypia or lack thereof in this group of patients. This is not an observation that has been observed elsewhere and may in fact be a very important observation. I must comment, however, that in Vanderbilt the incidence of follicular cancers appears to be quite distinct and different from that observed by myself in Baltimore and my colleagues, as well as in New Haven, and I look forward to long-term follow-up to determine whether this is a real finding that will be substantiated over time.
Some surgeons have suggested that intraoperative frozen-section analysis may differentiate benign from malignant lesions in this group of patients, whereas others have found that frozen section is essentially worthless for the majority of these patients. Although you did not comment about it in your presentation or in your manuscript, perhaps, Dr. Goldstein, you could comment whether you used frozen section in these patients, and, if so, was the information useful to you?
Once again I would like to compliment Dr. Goldstein on the manuscript. It is beautifully written. And I would like to thank the Society for the privilege of the floor.
Dr. Karen R. Borman (Jackson, MS): A couple of questions, one that has already been alluded to. About half of what you would expect in the numbers of follicular aspirates in this series were operated on, so what were the selection criteria that led to that operation? Second, there was a recent paper that mentioned nuclear overlapping and the amount of colloid—that is, scant or no colloid—as being highly predictive, more so even than some of your numbers, for nuclear overlapping as predictive cytologic features. Do you have any experience with that feature or with thyroid peroxidase antibodies?
Dr. Charles S. Turner (Winston-Salem, NC): We do have children under the age of 16 who have thyroid neoplasms, and I would like to ask Dr. Goldstein how would he follow these, his criteria for following, and how would he suppress them, and, if so, how long he would suppress them, and, if so, what is to be expected from that suppression.
Dr. John B. Hanks (Charlottesville, VA): I think it is a nice paper also and very important. I may be asking the same question Dr. Lairmore did, coming from a different angle, though.
I notice that the vast majority of patients in your series are female. The older male with follicular carcinoma is a particular risk group. And I think it would be a wrong message to send out that you might be watching a larger follicular lesion in a male. Did you have much more experience or did you break out your 1% that must be males in order to look at that?
Finally, can you say anything about lesion size in your groups with atypia or without atypia? Again, size has something to do with prognosis ultimately.
This is a very nice study. I look forward to reading it.
Dr. Michael Roe (Chattanooga, TN): I have one other question. Does everyone at Vanderbilt undergo FNA? Or is there a subset, due to patient desires, local symptoms, or physical findings, who undergo surgery without reliance on FNA, and if you added those in might your rate of malignancy be a little different? I was just curious about that.
Dr. Roger R. Perry (Norfolk, VA): I may have missed this in the presentation, but were the cytopathologists who were deciding on atypia versus no atypia blinded as to the final pathology?
Dr. Richard E. Goldstein (Nashville, TN): I very much appreciate everyone’s comments. I tried to write these down quickly, and hopefully we will get to it.
Dr. Lairmore, as far as an actual selection bias, I don’t think we had much because our policy is to offer thyroid surgery to all patients who have follicular lesions. So as I look back at the 709 aspirates, yes, I did find some cytologic readings that were consistent with follicular lesions. There are possibly 10 that for some reason got lost or were not operated on. I think probably that doesn’t alter our results much.
As far as the variability of cytopathologists, and actually I think this will also deal with the last question that was asked, we did not review any of these cytologic slides unless from the reading that was listed it was so ambiguous that we could not classify it. And we purposely did that to try to preserve the sense that what happened afterwards was based on the reading at that time. Also, all the actions that were taken were based on the cytologic reading done by our cytopathologists, and we had seven or eight cytopathologists. So rather than trying to recohort it and have it read by only one or two, I think that would have made this a very different study and taken it out of the time course in which it was actually done. But I do think that overall if you asked cytopathologists, they would have the sense that they are being better trained than they were 20 years ago. So although it would be a difficult thing to get at, I would suspect that overall there is probably less variability in cytopathologists than there may have been 20 years ago or so.
Dr. Lairmore brings up the issue of operating on low-risk patients. And to me part of what the study was about was the fact that when we get a fine-needle aspiration and we say that it appears to be benign, we know that there is a certain percent chance that we are in fact wrong. And yet we tell those patients the lesion is benign and we follow it loosely. And yet here there is this other group of patients in which the probability of malignancy may only be 6% to 7%, it may only be a few percent higher than what we call benign and don’t recommend come out. So to me it is an interesting phenomenon that for a difference of a percentage point perhaps of only 2% to 3%, we are saying that one lesion can stay in and that another lesion must come out. I don’t think that has been reconciled, and I bring this up mainly for people to think about.
What I do think this study does is it allows us to tell patients, based on making the efforts to subcategorize these lesions, what the risk of thyroid cancer is, and I think it allows them to make more informed choices based on that data. For instance, in elderly patients who have a certain amount of cardiac disease and have a very small, 5-mm lesion that is read as a follicular lesion, it may in fact potentially be an option to reaspirate it; or there may be an option to consider thyroid suppressive therapy, place that patient on Synthroid, and drop their TSH. However, I would not recommend thyroid suppressive therapy for children.
As far as Dr. Lairmore’s question on the issue of molecular techniques, I think that they have promise. And I would theorize that eventually that we will take thyroid aspirates, run a panel on them, and we will have specific enough markers to potentially tell whether a lesion is benign or whether it is malignant. I don’t think that we are there yet. Some of the studies that were done looking at HTERT, H-T-E-R-T, have had some overlap between the lesions that have turned out to be malignant versus benign. So I don’t think that those techniques are there yet. But I think that they do have a lot of promise.
I would add also that a majority of the malignant lesions, including the follicular lesions without atypia, were papillary thyroid cancer or they were follicular variants of papillary thyroid cancer. There is a lot of interest in the pathology literature at trying to better identify those lesions. So I think that physicians are coming at this from several different disciplines.
Dr. Udelsman raises a very interesting point, and in the paper I make note of the fact that he and his group have had a long-standing interest in these lesions. In a study that came out from Dr. Udelsman’s group looking at the incidence of follicular cancer at Johns Hopkins in the ’80s and early ’90s, there was a fairly high rate of follicular cancers in this group which was higher than what we saw. In a later paper in which he examined a group that was seen after that time, the rate of follicular cancer was in fact somewhat less; I think it was 16%. But it may be that there are different regions of the country who are seeing changes in the prevalence of follicular cancer. I still think that we need larger databases and potentially to look at this across institutions to get a better handle on whether this rate really is changing.
Dr. Borman brought up another potential area in which atypia is being looked at. I would also say that there was a recent study that came out after our abstract was in from Mount Sinai in which follicular lesions, lesions with atypia, also had a higher probability of being malignant versus those lesions that did not have atypia.
I think I addressed the statement by Dr. Turner. I think at this point that I would not feel comfortable putting children on thyroxine. I don’t think we really have an answer. And certainly most children are looking at a very long life expectancy. I just found it interesting that although we have an active pediatric surgical group, we did not have any children under 16 that had follicular neoplasms.
Dr. Hanks raised the issue of size of the lesions. Most of our follicular cancers were in lesions 4.0 cm or larger. So certainly I think that lesions that are large should come out no matter what, especially in men.
Partially in answer to Dr. Rowe’s question, we really offer thyroidectomy to all patients that have FNAs that are consistent with follicular neoplasms. And it is our policy to, in most instances, offer fine-needle aspiration to all patients who have thyroid modules. We think it is a very easy thing to do. We do it with and without ultrasound guidance, depending on how comfortable we are that we can adequately place the needle in these lesions.
I hope I have answered all the questions, and I thank the Association for the privilege of the floor and for the opportunity to have presented these data.
Footnotes
Presented at the 113th Annual Session of the Southern Surgical Association, December 3–5, 2001, Hot Springs, Virginia.
Correspondence: Richard E. Goldstein, MD, PhD, 597 Preston Research Building, Vanderbilt University Medical Center, Nashville, TN 37232.
E-mail: richard.goldstein@mcmail.vanderbilt.edu
Accepted for publication December 2001.
References
- 1.Rosen IB, Wallace C, Strawbridge H, et al. Reevaluation of needle aspiration cytology in detection of thyroid cancer. Surgery 1981; 90: 747–756. [PubMed] [Google Scholar]
- 2.Walfish PG, Hazani E, Strawbridge H, et al. Combined ultrasound and needle aspiration cytology in the assessment and management of hypofunctioning thyroid nodule. Ann Intern Med 1977; 87: 270–274. [DOI] [PubMed] [Google Scholar]
- 3.Miller JM, Hamburger JI, Kini S. Diagnosis of thyroid nodules: use of fine-needle aspiration and needle biopsy. JAMA 1979; 241: 481–483. [PubMed] [Google Scholar]
- 4.Gershengorn MC, McClung MR, Chu EW, et al. Fine-needle aspiration cytology in the preoperative diagnosis of thyroid nodules. Ann Intern Med 1977; 87: 265–269. [DOI] [PubMed] [Google Scholar]
- 5.Grant CS, Hay ID, Gough IR, et al. Long-term follow-up of patients with benign thyroid fine-needle aspiration cytologic diagnoses. Surgery 1989; 106: 980–986. [PubMed] [Google Scholar]
- 6.Hamberger B, Gharib H, Melton LJ III, et al. Fine-needle aspiration biopsy of thyroid nodules: impact on thyroid practice and cost of care. Am J Med 1982; 73: 381–384. [PubMed] [Google Scholar]
- 7.Gharib H, Goellner JR, Zinsmeister AR, et al. Fine-needle aspiration biopsy of the thyroid: the problem of suspicious cytologic findings. Ann Intern Med 1984; 101: 25–28. [DOI] [PubMed] [Google Scholar]
- 8.Hamming JF, Golsings BM, van Steenis GJ, et al. The value of fine-needle aspiration biopsy in patients with nodular thyroid disease divided into groups of suspicion of malignant neoplasms on clinical grounds. Arch Intern Med 1990; 150: 113–116. [PubMed] [Google Scholar]
- 9.Stojadinovic A, Ghossein RA, Hoos A, et al. Hurthle cell carcinoma: a critical histopathologic appraisal. J Clin Oncol 2001; 19; 2616–2625. [DOI] [PubMed] [Google Scholar]
- 10.Chen H, Nicol TL, Udelsman R. Follicular lesions of the thyroid: does frozen-section evaluation alter operative management? Ann Surg 1995; 222: 101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeMay RM. Follicular lesions of the thyroid. Am J Clin Pathol 2000; 114: 681–683. [DOI] [PubMed] [Google Scholar]
- 12.Livolsi VA, Asa SL. The demise of follicular carcinoma of the thyroid gland. Thyroid 2001; 4: 233–236. [DOI] [PubMed] [Google Scholar]
- 13.Kelman AS, Rathan A, Leibowitz J, et al. Thyroid cytology and the risk of malignancy in thyroid nodules: importance of nuclear atypia in indeterminate specimens. Thyroid 2001; 11: 271–277. [DOI] [PubMed] [Google Scholar]
- 14.Carpi A, Ferrari E, Toni MG, et al. Needle aspiration techniques in preoperative selection of patients with thyroid nodules: a long-term study. J Clin Oncol 1996; 14: 1704–1712. [DOI] [PubMed] [Google Scholar]
- 15.Papanicolaou Society of Cytopathology. Guidelines of the Papanicolaou Society of Cytopathology for the examination of fine-needle aspiration specimens from thryoid nodules. Mod Pathol 1996; 9: 710–715. [PubMed] [Google Scholar]
- 16.Goeller JR, Gharib H, Grant CS. Fine-needle aspiration cytology of the thyroid, 1980 to 1986. Acta Cytol 1987; 31: 587–590. [PubMed] [Google Scholar]
- 17.DeMay RM. Thyroid. In: The art and science of cytopathology. Chicago: ASCP Press; 1996: 724–729.
- 18.DeMay RM. Cytology. In: The art and science of cytopathology. Chicago: ASCP Press; 1996: 471–474.
- 19.Rosai J, Carcangiu ML, DeLellis RA. Follicular carcinoma. In: Rosai J, Carcangiu ML, DeLellis RA, eds. Tumors of the thyroid gland. Washington DC: Armed Forces Institute of Pathology; 1990: 49–63.
- 20.Ferguson GA. Statistical analysis in psychology and education. New York: McGraw-Hill, Inc.; 1981.
- 21.Gerfo P, Colacchio T, Caushaj F, et al. Comparison of fine-needle and coarse-needle biopsies in evaluating thyroid nodules. Surgery 1982; 92: 835–838. [PubMed] [Google Scholar]
- 22.Boey J, Hsu C, Collins RJ. False-negative errors in fine-needle aspiration biopsy of dominant thyroid nodules: a prospective follow-up study. World J Surg 1986; 10: 623–630. [DOI] [PubMed] [Google Scholar]
- 23.Udelsman R, Westra WH, Donovan PI, et al. Randomized prospective evaluation of frozen-section analysis for follicular neoplasms of the thyroid. Ann Surg 2001; 233: 716–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McHenry CR, Thomas SR, Slusarczyk SJ, et al. Follicular or Hurthle cell neoplasm of the thyroid: Can clinical factors be used to predict carcinoma and determine extent of thyroidectomy? Surgery 1999; 126: 798–804. [PubMed] [Google Scholar]
- 25.Williams ED, Doniach I, Bjarnason O, et al. Thyroid cancer in an iodide-rich area: a histopathological study. Cancer 1977; 39: 215–222. [DOI] [PubMed] [Google Scholar]
- 26.Greaves TS, Olvera M, Florentine BD, et al. Follicular lesions of thyroid: a 5-year fine-needle aspiration experience. Cancer 2000; 90: 335–341. [PubMed] [Google Scholar]
- 27.Mesonero CE, Jugle JE, Wilbur DC, et al. Fine-needle aspiration of the macrofollicular and microfollicular subtypes of the follicular variant of papillary carcinoma of the thyroid. Cancer 1998; 84: 235–244. [PubMed] [Google Scholar]
- 28.Yan Z, Yang GCH, Waisman J. A low-power, “architectural,” clue to the follicular variant of papillary thyroid adenocarcinoma in aspiration biopsy. Acta Cytologica 2000; 44: 211–217. [DOI] [PubMed] [Google Scholar]
- 29.Chang TC, Lai SM, Wen CY, et al. Three-dimensional cytomorphology and its relationship with clinical stage in fine-needle aspiration biopsy of papillary thyroid carcinoma. Acta Cytol 2000; 44: 633–639. [DOI] [PubMed] [Google Scholar]


