Abstract
Objectives
To assess the utility of advanced tests performed before surgery on patients who needed emergent abdominal operations, and to assess the outcomes of these patients relative to their diagnoses.
Summary Background Data
Patients with a potential abdominal catastrophe may have various presentations, contributing to the difficulty of the decision about whether an operation is indicated. Advanced tests can be valuable, but the use of these adjuncts should be appropriate to the clinical status of the patient so that treatment is not delayed. The role of these tools in the evaluation of the patient who may need an emergent abdominal operation is less well defined.
Methods
Data were reviewed on adult patients undergoing emergent abdominal operations. Entrance criteria included patients who had an emergent abdominal operation, defined as one performed for presumed gastrointestinal perforation, infarction, or hemorrhage within 6 hours of admission or surgical consultation. Advanced tests were those that were time-consuming or invasive or required scheduling with other departments so that the risk/benefit ratio of these tests could be questioned. A useful test was one that provided information that contributed to a change in the patient’s management.
Results
During a 5-year period, 300 consecutive adult patients (158 perforations, 66 hemorrhage, 53 ischemia/infarction, and 23 “other”) underwent emergent nontrauma celiotomies. Overall, the death rate was 20%. Advanced preoperative tests were performed in 135 (45%) of the 300 patients, and 40 of these patients had delayed treatments. Preoperative localization of bleeding sites was accomplished in 77% of patients with upper gastrointestinal bleeding and 86% of patients with lower gastrointestinal bleeding.
Conclusions
Most patients in need of emergent abdominal operations should not undergo advanced tests. The primary role of advanced tests in these patients is in the localization of a bleeding site. With the exception of patients who present with hemorrhage, advanced tests frequently cause a delay in treatment.
A rapid and accurate diagnosis in the patient with an acute abdomen is essential to ensure that optimal care and a satisfactory outcome are obtained. Although many of these patients are referred to surgeons from other physicians, it is the surgeon who must decide whether an operation is indicated and when it is to be performed. Recent advances in technology and diagnostic imaging have been shown to be valuable aids in this decision-making process, 1 but the use of these adjuncts should be appropriate to the clinical status of the patient so that treatment is not delayed. The role of these tools in the evaluation of the patient who may need an emergent abdominal operation is less well defined. The hypothesis of this study was that advanced diagnostic imaging studies or procedures (tests) have little impact on the evaluation of patients who may need emergent operations. The objectives of this study were to assess the utility of advanced tests that were performed before surgery on patients who needed emergent abdominal operations, and to assess the outcomes of these patients relative to their diagnoses.
METHODS
Data were reviewed on adult patients undergoing emergent abdominal operations. To be included in the study, patients had to have an emergent abdominal operation, defined as one performed for presumed gastrointestinal perforation, infarction, or hemorrhage within 6 hours of admission or surgical consultation. Injured patients as well as those who were inpatients on the general surgery service were excluded from the study.
Patients were identified through the Department of Surgery patient registry, and data were obtained from patient charts, morbidity and mortality records, and the Department of Radiology records. All advanced diagnostic tests and procedures were interpreted by attending surgeons, gastroenterologists, or radiologists. Data recorded included patient demographics, mode of presentation, physiologic status on admission or consultation, advanced diagnostic tests and procedures performed, anesthetic risk (American Society of Anesthesiologists Physical Status classification system, ASA ≥ 3), 2 operative findings, confirmed diagnosis, treatment, length of stay (LOS), complications, and outcome. Advanced diagnostic studies (tests) were defined as those that were time-consuming or invasive or required scheduling with the radiology or gastroenterology department so that the risk/benefit ratio of these tests could be questioned. These tests included gastrointestinal contrast studies, ultrasound, computed tomography (CT) scans, technetium-labeled erythrocyte scintigraphy, arteriography, esophagoduodenoscopy (EGD), colonoscopy, and laparoscopy. A useful test was defined as one that provided information that contributed to a change in the patient’s management. Laboratory tests and the three-film radiographic abdominal series (erect and supine abdominal views and erect chest film) were considered components of the routine evaluation of these patients and were not considered advanced tests.
Comparisons between groups were assessed by the t test and analysis of variance for parametric data and by chi-square analysis for nonparametric data.
RESULTS
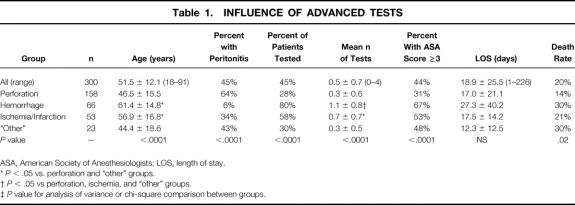
From 1996 to 2001, 300 consecutive adult patients (189 men [63%]) at a mean age of 51.5 ± 17.1 years (range 18–91) underwent emergent nontrauma celiotomies. There were 158 patients who suffered perforations of the gastrointestinal tract, 66 who had intraabdominal or gastrointestinal hemorrhage, 53 with gastrointestinal or other visceral ischemia or infarction, and 23 “others” (Table 1).
Table 1. INFLUENCE OF ADVANCED TESTS
ASA, American Society of Anesthesiologists; LOS, length of stay.
*P < .05 vs. perforation and “other” groups.
†P < .05 vs perforation, ischemia, and “other” groups.
‡P value for analysis of variance or chi-square comparison between groups.
The patients with hemorrhage or ischemia/infarction were significantly older than those in the perforation or “other” groups (P < .05). Although the mean LOS for the 300 patients was 18.9 ± 25.5 days (range 1–226), those with hemorrhage had the longest LOS, with a mean of 27.3 ± 40.2 days (not significant vs. the “other” groups).
A high risk for general anesthesia (ASA ≥ 3) was present in 44% of the 300 patients. The mean age of the patients who survived was 49.0 ± 16.6 years versus 61.2 ± 15.8 years for those who died (P < .001). Overall, the death rate for the 300 patients was 20%; for those in the hemorrhage or “other” groups, it increased to 30% (P < .0001).
Advanced preoperative tests were performed in 135 (45%) of the 300 patients. In general, women were more likely to have preoperative tests or procedures (P = .04), as were patients who were older (57.1 ± 16.5 vs. 46.9 ± 16.3, P < .0001), who presented with hemorrhage or an immunosuppressed disease state, or who had extensive comorbid factors (ASA ≥ 3, P < .0002). Further, patients who had peritonitis on examination were less likely to undergo advanced tests than those without peritonitis (27% vs. 60%, P < .0001). Also, there was no significant difference in the number of negative or nontherapeutic celiotomies in patients who had peritonitis present on the physical examination versus those who did not.
Two patients were pregnant, and both were evaluated with ultrasound before surgery. One of the patients was 38 weeks’ pregnant, had peritonitis on examination, and underwent a laparoscopic cholecystectomy for a gangrenous gallbladder. The other patient had an incarcerated ventral hernia but presented in hypovolemic shock from vaginal bleeding secondary to an incomplete spontaneous abortion. She underwent a partial resection of ischemic small bowel and an emergent evacuation of the fetus.
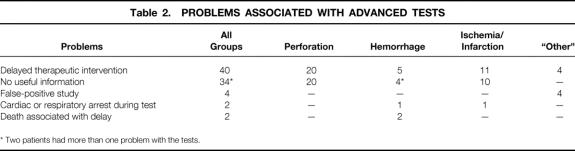
A delay in treatment occurred in 40 of the 135 patients (29.6%) who underwent advanced preoperative tests (Table 2). Of these 40 patients, no useful diagnostic information was obtained from the tests in 34 patients. Four of the patients (three with hemorrhage, one with ischemia/infarction) suffered serious adverse events (cardiopulmonary arrest) during these advanced studies, and two died later.
Table 2. PROBLEMS ASSOCIATED WITH ADVANCED TESTS
* Two patients had more than one problem with the tests.
Laparoscopy was performed in 10 patients (70% women); in three of them it was the definitive procedure. In the first patient, laparoscopy detected an ovarian cyst as the cause of the abdominal pain. In the other two patients, ascites was noted in one and no pathology was shown in the other. The latter patient underwent an incidental laparoscopic appendectomy. The other seven patients went on to have celiotomies.
The following is an analysis of the data by patient group.
Perforation
Perforations occurred in 158 patients and included 88 gastric or duodenal ulcers, 33 bowel, 31 appendixes, 3 gastric, 1 pancreatic pseudocyst, 1 urinary bladder, and 1 tuboovarian abscess. The mean LOS was 17.0 ± 21.1 days, and there was a 14% death rate. Peritonitis was present on the physical examination of 102 (64.5%) of these patients, and advanced tests were performed in 24 of them. The advanced test provided useful information in only 25% (6/24) of these patients. A pneumoperitoneum was present on the abdominal radiographic series of 71 of the 158 (44.9%) patients and was found most frequently (86%) in patients with perforated duodenal or gastric ulcers. The combination of pneumoperitoneum and peritonitis was present in 60 of these patients, but only 1 patient with that combination benefitted from an advanced test. That patient had two problems, an upper gastrointestinal hemorrhage and a perforated colon. Before his operation, he underwent an EGD that was both diagnostic and therapeutic for a duodenal ulcer.
Hemorrhage
The sources of bleeding for the 66 patients who had intraabdominal or gastrointestinal tract bleeding included 28 lower gastrointestinal (26 diverticulosis, 1 unknown, 1 sigmoid colonic ulcer), 26 upper gastrointestinal (22 ulcers, 4 Mallory Weiss tears), 7 major abdominal vessels (3 abdominal aortic aneurysms, 2 aortoenteric fistulas, 2 mesentery), 3 hepatic, and 2 other. The mean LOS was 27.3 ± 40.2 days, and there was a 30% death rate. Only four patients had peritonitis on physical examination, and pneumoperitoneum was not present on any of the abdominal radiographs. Advanced tests were performed in 52 of the 66 patients with hemorrhage (Table 3). Twenty of the 26 (77%) patients with upper gastrointestinal bleeding had preoperative localization of their bleeding sites, 19 with EGD and 1 by an upper gastrointestinal contrast study. Of the 28 patients who had bleeding of the lower gastrointestinal tract, 24 (86%) had successful preoperative localization of the bleeding site, 21 by Tc-99m scan and 3 by colonoscopy.
Table 3. ADVANCED TESTS IN PATIENTS WITH INTRA-ABDOMINAL/GI HEMORRHAGE
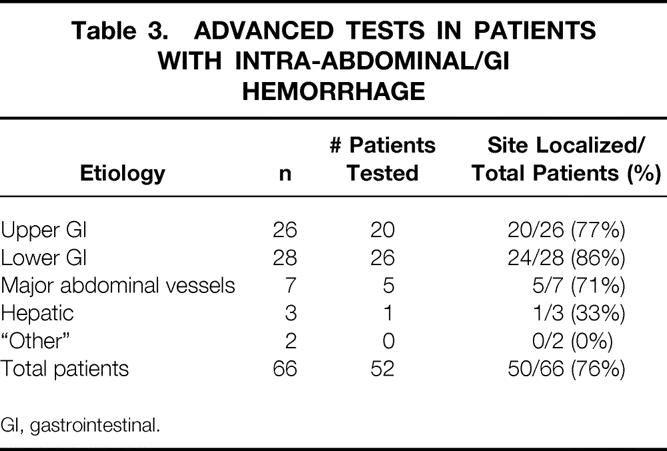
GI, gastrointestinal.
Advanced tests localized bleeding sites before surgery in five of the seven patients whose source of hemorrhage was a major abdominal vessel. One patient who was bleeding from his liver underwent an arteriogram with an attempt at embolization. The bleeding site was localized, but the embolization procedure failed to control the hemorrhage. The other two patients were too hemodynamically unstable to undergo tests and were moved rapidly to the operating room.
Ischemia or Infarction
Ischemia or infarction of the gastrointestinal tract or other viscera was present in 53 and included 32 small bowel, 10 colon, 6 gallbladder, 3 combination of organs, 1 kidney, and 1 omentum. The mean LOS was 17.5 ± 14.2 days, and the death rate was 21%. Although 31 patients had advanced tests, only 21 (68%) benefitted from the test. Even the presence of peritonitis in 18 patients did not significantly change the percentage (11/18 [61%]) of useful tests.
Other
The “other” group included 23 patients who had nine therapeutic, eight negative (no pathology found at operation), and six nontherapeutic celiotomies. The nine therapeutic celiotomies included patients with obstructing colon cancer (n = 3), an intraabdominal abscess (n = 1), Ogilvie’s syndrome (n = 1), ovarian carcinomatosis (n = 1), a ruptured ovarian cyst (n = 1), an pancreatic abscess with abdominal compartment syndrome (n = 1), and a necrotizing pancreatic abscess (n = 1). The six nontherapeutic celiotomies included pancreatitis (n = 3), pelvic inflammatory disease (n = 2), and primary peritonitis (n = 1).
The mean LOS was 12.3 ± 12.5 days, and the death rate was 30%. A CT scan was performed in 7 of the 23 patients, but only 2 provided useful clinical information (multiple intraabdominal abscesses and a pancreatic abscess). Three of the other CT scans that were performed showed false-positive findings (i.e., free air or intussusception).
Peritonitis was present in 10 (44%) of the 23 patients. Eight of those 10 patients had no advanced tests and nontherapeutic celiotomies. Only one patient with peritonitis had a CT scan that was considered useful (multiple intraabdominal abscesses followed by a therapeutic celiotomy). Pneumoperitoneum was present on the abdominal radiographs of 4 (17.4%) of the 23 patients, all of whom had negative celiotomies.
DISCUSSION
The patient with a potential abdominal catastrophe may have an altered mental status, various presentations, or significant comorbid factors, all of which contribute to the difficulty of the decision-making process about whether an operation is indicated. Although the history and physical examination are the cornerstones of diagnosis, advanced diagnostic tests, when indicated, can be valuable aids for the surgeon.
In general, almost half of our study population had significant comorbid factors and were deemed a high risk for general anesthesia (see Table 1). In addition, if compared with patients undergoing nonemergent operations, our patients had longer hospital stays and higher death rates. These characteristics underscore the degree of illness of our patients and emphasize the need to make rapid and accurate decisions about their management.
Advanced Tests
Preoperative advanced tests were performed in 135 of the 300 patients (45%) in our study, but not all of them were without consequences. Forty patients had delayed treatment because of the tests. Among these 40 patients, other test-related problems included false-positive findings resulting in nontherapeutic celiotomies and a lack of useful information from the test (see Table 2). Three of the 40 patients suffered adverse events during the tests or procedures, including 2 who died later. The first patient was a woman who was symptomatic from a 3.5-cm abdominal aortic aneurysm that was diagnosed with an ultrasound examination. She subsequently underwent a CT scan of her abdomen and an angiogram of her abdominal and extremity vessels. Later, she experienced a cardiopulmonary arrest and died of her ruptured aneurysm. The second patient had peritonitis on examination and a massive hemoperitoneum on CT scan. He had a cardiopulmonary arrest during the CT scan and subsequently underwent a diagnostic peritoneal lavage before his operation, but then died. These data emphasize the importance of determining the need for the test as well as knowing the specific information that it will provide relative to the patient’s clinical condition. An excellent example of this principle was the use of ultrasound in the two pregnant patients in our study. One patient had an excellent history for gallbladder disease and underwent evaluation with ultrasound. This noninvasive, rapid, painless examination (which afforded no ionizing radiation to her unborn child) confirmed the suspected diagnosis, and she subsequently underwent cholecystectomy. The other patient, who had an incarcerated incisional hernia, was hypotensive from massive vaginal bleeding secondary to an incomplete spontaneous abortion. With the use of a surgeon-performed, bedside ultrasound examination, 3 hemoperitoneum was excluded as a primary site of hemorrhage. Subsequently, the patient had an evacuation of the fetus and a hernia repair.
In general, patients in our study who had peritonitis on examination (n = 135) were less likely to undergo advanced tests than those without peritonitis (27% vs. 60%, P < .0001). A total of 35 patients (27%) who had peritonitis did undergo advanced tests, but the test was helpful in only 7 patients. In these seven patients, multiple comorbid factors (n = 5), previous abdominal surgery (n = 1), and pancreatitis (n = 1) confounded the history and physical examination, and the tests helped to identify the patient’s pathology.
For the purpose of proposing some practical guidelines for the management of these patients, the data from each group are discussed below.
Perforation
The 158 patients with a perforated viscus or other organ represented 53% of the study population, indicating that this is a common etiology among patients who will need an emergent operation. In addition to the history, common findings such as the presence of peritonitis on the physical examination and pneumoperitoneum on the abdominal radiographs can be very helpful in the evaluation of these patients. In our study, 64.5% of these patients had peritonitis on the physical examination and almost half (44.9%) had pneumoperitoneum on the abdominal radiographs. As expected, pneumoperitoneum was present more frequently (86%) on the abdominal radiographs of patients with perforated ulcers compared with the other sites described. Of the 158 patients, 60 had peritonitis with pneumoperitoneum present on the abdominal radiographs; with that combination, only 1 patient benefitted from an advanced test. Considering the delayed treatment and adverse events in those who underwent advanced tests, the risk of an advanced test in this group outweighs its benefit (see Table 2). Based on the data from this group of patients, the combination of a good history for perforation, the finding of peritonitis on the physical examination, and the finding of pneumoperitoneum on the abdominal radiographs warrants an operation. No other advanced test is needed.
Hemorrhage
The unique characteristic of this group of 66 patients was that the bleeding was frequently visible (82% of the patients had upper or lower gastrointestinal bleeding), and therefore the challenge was that of localization of the bleeding site rather than a diagnosis. These patients were significantly older and had higher death rates than the study population in general. Therefore, in these patients, localizing the bleeding site and decreasing the amount of time spent under general anesthesia are worth the risk of the test. The advanced tests most frequently used included the EGD for patients with upper gastrointestinal hemorrhage and the Tc-99m scan for those with bleeding from the lower gastrointestinal tract. It is logical to assume that the patients in our study who suffered intraabdominal or gastrointestinal hemorrhage were bleeding briskly and, therefore, the Tc-99m scans were likely to show a higher-than-reported positive rate. 4–7 Nonetheless, based on these data, tests that are focused on localizing the bleeding site relative to the patient’s clinical condition should be used early, before hemodynamic instability occurs (Fig. 1). Unlike patients who suffered perforations of the gastrointestinal tract or other viscera, only four of these patients had peritonitis on their physical examinations, and none had pneumoperitoneum on the abdominal radiographic series. These data support the concept that the presence of peritonitis and/or pneumoperitoneum is much less important in the successful management of the patient with hemorrhage.

Figure 1. A 41-year-old man with posterior duodenal ulcer. Bleeding site was identified with esophagoduodenoscopy.
Ischemia or Infarction
The wide variation of presentations of these 53 patients, as well as the spectrum of pathology in this group, was probably responsible for the rather infrequent presence of peritonitis (34%) found on physical examination. Although 31 patients had advanced tests, only 21 (68%) of the tests were useful. Considering that most of the patients had ischemic or infarcted small bowel from either a hernia or bowel obstruction, the physical examination and the abdominal radiographic series would be important factors in deciding whether an operation was indicated (Fig. 2).

Figure 2. Portion of small bowel entrapped in omentum (internal hernia). Peritonitis was present on physical examination, and the findings on the abdominal radiographic series were consistent with a small bowel obstruction.
Other
Similar to the patients with ischemia or infarction of the gastrointestinal tract, these 23 patients had a wide variety of presentations and pathology (Fig. 3). Appropriate evaluation of these patients includes a proper balance between the use of advanced tests and early operation, if indicated. Examination of the data from this group supports the use of surgeon-performed diagnostic tests such as ultrasound, laparoscopy, and diagnostic peritoneal lavage. For example, in the patient with primary peritonitis who had a nontherapeutic celiotomy, surgeon-performed bedside ultrasound could have been used to identify the ascites, perform a diagnostic and therapeutic peritoneal tap, and avoid the unnecessary operation.
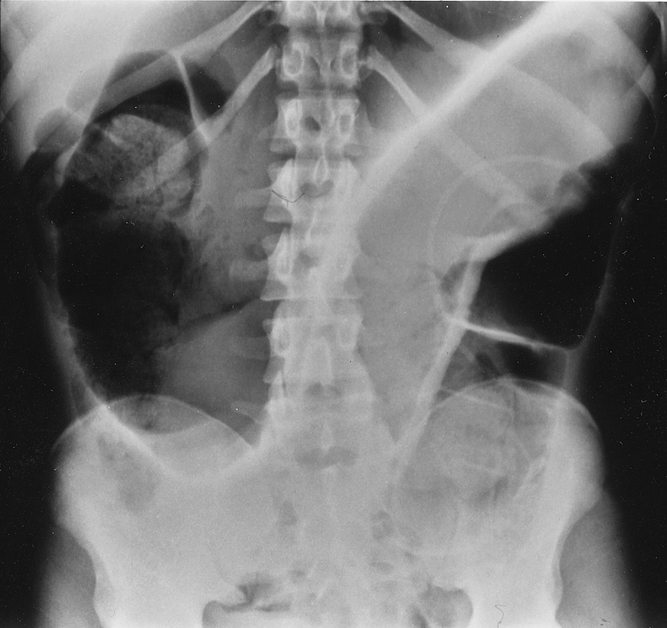
Figure 3. Abdominal radiographic finding consistent with sigmoid volvulus.
As a diagnostic and therapeutic tool, it is well accepted that laparoscopy is useful in the evaluation and treatment of select patients with abdominal pain from gynecologic, operative, and nonoperative etiologies. 8–17 Of particular interest in our study is how this tool may have been used more frequently to avoid or minimize the nontherapeutic celiotomies, especially for patients whose CT scans showed false-positive findings. In general, laparoscopy may not have been used as frequently as it could have been for two reasons. First, these patients were considered to be at high risk for general anesthesia, and in the surgeon’s clinical judgment a celiotomy may have been less time-consuming; second, not all surgeons are equally skilled in this technique. Notwithstanding these issues, our number of negative/nontherapeutic celiotomies (14/300 [4.6%]) is acceptable but may have been lower if laparoscopy had been used more frequently.
Potential Deficiencies
Potential deficiencies in this investigation include those associated with a retrospective study. For example, all of the details about each patient’s history relative to a disease process may not have been recorded in the medical chart, making it difficult to determine whether the diagnosis could have been made based on the patient’s history alone. Further, not all patients who died underwent postmortem examinations, so other unknown pathology may have contributed to the death.
In this investigation, we examined only patients who survived long enough to undergo surgery. Further, those who waited longer than 6 hours before they underwent surgery were not included in the study. For example, certain patients, although in need of an operation, are anticipated to have an improved postoperative outcome if they undergo preoperative resuscitation, including blood transfusion and/or invasive hemodynamic monitoring. 18 Although our data may be slightly biased, it is estimated that the addition of these few patients would not significantly change the conclusions of our investigation, especially because our study population was a consecutive group.
During the 5-year time span of this study, several upgrades of the helical CT scanners resulted in more rapid scanning and improved image quality. Related to this issue is that of the interpretation of advanced diagnostic imaging studies. The official readings by the attending radiologists sometimes differed from those of the radiology residents. These discrepancies were subsequently discussed with the radiologists, but often not before the patient’s operation. Because the surgeons in our practice group read the CT scans that they order, it is difficult to determine the effect of this issue.
Finally, the type and number of tests ordered may have varied with the attending surgeon and the resident who evaluated the patient as well as whether the patient was initially seen in the emergency department, admitted to the medicine service, or directly admitted to the surgery service. Notwithstanding those issues, our data indicate that in select patients with a potential abdominal catastrophe, advanced tests do have a role in their management.
CONCLUSIONS
Based on this review of 300 patients who underwent emergent celiotomies, we conclude the following:
Adult patients who need an emergent abdominal operation have significant comorbid factors, are at high risk for general anesthesia, and have a high death rate.
In a patient who needs an abdominal operation, perforation of the gastrointestinal tract is the most common process.
Most patients in need of an emergent abdominal operation should not have advanced tests.
The primary role of advanced tests in the evaluation of the patient with a potential abdominal catastrophe is in the localization of a bleeding site.
With the exception of patients who present with hemorrhage, advanced tests frequently cause a delay in the treatment of the patient.
The patient who presents with peritonitis on physical examination in combination with pneumoperitoneum on the plain abdominal radiographic series needs no advanced test before undergoing surgery.
We recommend that for the evaluation of the patient with a potential abdominal catastrophe, the initial assessment based on history, physical examination, and, if appropriate, plain abdominal radiographic series should categorize the patient as presenting with intraabdominal or gastrointestinal hemorrhage or visceral perforation, ischemia, or infarction (Fig. 4).
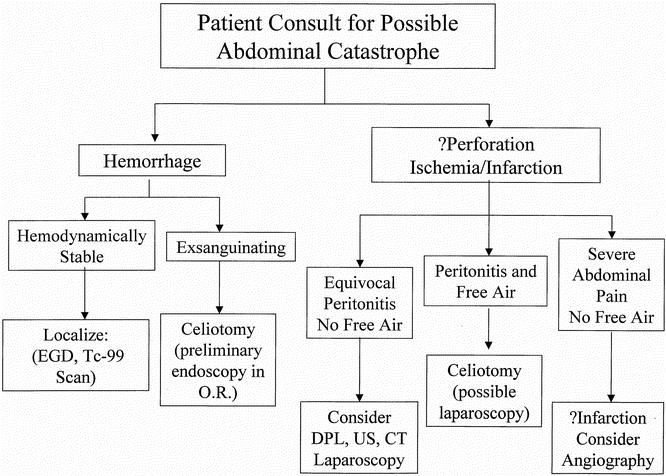
Figure 4. Algorithm for assessment of the patient with a potential abdominal catastrophe.
Patients with an obvious gastrointestinal hemorrhage who are hemodynamically stable or can be stabilized rapidly should undergo further testing to localize the bleed. If they are hemodynamically unstable, intraoperative endoscopy followed immediately by celiotomy is indicated. Patients who present with peritonitis and pneumoperitoneum on the abdominal radiographic series should proceed to surgery.
Advanced tests, especially surgeon-performed ultrasound and laparoscopy, should be considered when a diagnosis of peritonitis is equivocal and there is no pneumoperitoneum on the abdominal radiographic series. Mesenteric angiography is another advanced test that should be considered when the patient’s abdominal pain is out of proportion to the clinical findings and the diagnosis of peritonitis is equivocal.
Enthusiasm for new technology should not overwhelm sound clinical judgment. 19 In this era of ever-increasing emphasis on the use of minimal access surgery, surgeons must be able to recognize the patient with a potential abdominal catastrophe, rapidly determine which patients would benefit from advanced tests, and be able to operate on a wide variety of catastrophic conditions to save the patient. These principles, especially the application of sound clinical judgment, should be emphasized in surgical residency training programs.
Discussion
Dr. Harvey J. Sugerman (Richmond, VA): This is a very interesting report by Dr. Rozycki and her colleagues. She did answer some of the questions I had from the manuscript in her presentation. They clearly have a large exposure to many critically ill general surgery patients at Grady Memorial Hospital.
I would certainly agree with the premise that there is no indication for an advanced diagnostic test of any kind in a patient with clear evidence of peritonitis and free air on their acute series. I wonder why any of these patients, 39% according to the data, underwent further study. I was worried that this was a resident decision without communication with the attending surgeon. But since you and your colleagues take in-house call, I was wondering how this could possibly occur. I gather it probably occurred because the emergency room doctors and referring physicians saw these patients first.
I try to emphasize to our medical students and residents the importance of a careful, complete history and physical examination. So often our house staff and emergency room physicians jump to a CT scan, especially now that we have a scanner in our emergency room, when the patient is often telling the physician what is really wrong with him. It seems that physicians, perhaps because of their clinical demands, fail to listen to the patient.
CT scanning for appendicitis is the latest rage. One of our anesthesia residents came to the emergency room with signs and symptoms he thought were consistent with appendicitis. A CT scan was obtained that was read as negative, and they wanted to discharge him. But he insisted on seeing an attending surgeon, and I took out a severely inflamed appendix. His history and physical findings should have been adequate for the diagnosis. When the issue of the normal CT scan was discussed with the attending radiologist the next day, we were told it was an inadequate study as enough contrast hadn’t reached the cecum.
I would also support the use of advanced diagnostic tests in patients with gastrointestinal bleeding. I was surprised that all patients in this series didn’t have such a study. There is nothing more exasperating than operating on a GI bleeder and not have the least inkling as to the source. Furthermore, endoscopic or angiographic intervention may obviate the need for surgical intervention. In that regard, how many patients had advanced diagnostic studies that permitted a definitive treatment and prevented an emergency laparotomy, such as percutaneous drainage of a gangrenous gallbladder in a very critically ill patient or bipolar coagulation or injection sclerotherapy for bleeding?
I would recommend a follow-up study in which all patients with a suspected “acute abdominal process” were evaluated rather than only the patients who had undergone emergency surgical intervention. Of course, the ideal would be a randomized, prospective trial. However, this would obviously not be ethically or clinically reasonable, and would certainly not be supported by an IRB.
Dr. Kenneth W. Sharp (Nashville, TN): Dr. Rozycki, I appreciate the opportunity to discuss this paper from Emory. I found this to be a paper with simple intent: let’s decrease unnecessary tests that delay appropriate patient management. But ultimately it is a very difficult paper. Because in essence this is a paper about judgment, and what is equivocal peritonitis to a resident may be clear-cut peritonitis to you, Dr. Rozycki.
Specifically, I think clinical judgment in this group of patients who are very ill, multiple comorbid illnesses, are extremely challenging, many of these patients had difficult diagnoses to confirm. You and your residents should be congratulated for achieving a very acceptable mortality in a gravely ill group of patients.
Clearly, judgment is the key here, and good judgment is related to the level of experience. I would like to know the level of resident experience in making these judgments in your patients. Because clearly, even though you are in house, you are going to have to take the call initially from the resident, who has already made some evaluation and made some judgment about the patient.
Clearly, junior residents are going to be more hesitant in their diagnosis and more hesitant in determination of the patient who needs to go expeditiously to the operating room. Senior-level residents and faculty are going to be more definitive in their management. So I have a few questions for you.
Can you give us any idea of the level of training of those residents or faculty making decisions about advanced tests? Even though you have excluded patients who were admitted to the medicine service—I think, I am still a little confused over this—is there any issue of the admitting service ordering tests at the same time that you are consulted, so therefore the patient who is on the way to the CT scan, by the time you are ever consulted on the patient? Do any of these patients have their advanced tests ordered by surgeons, or are these ordered all by the referring service? I am confused on this issue.
Number two, you have shown us that many patients have proper therapy delayed by advanced tests. Similar to Dr. Sugerman’s question, over the past 5 years undoubtedly dozens or hundreds of patients have been benefited by advanced tests who had abdominal pain—and abdominal findings, no doubt. So I always like to ask questions that you have no data assembled. So how many patients were benefited by CT scans? How many had pancreatitis diagnosed who had an acute abdomen? How many had diverticulitis or diverticular abscesses diagnosed and were spared celiotomy? If you have that data, we have another paper coming.
Finally, as one of the most outstanding surgeon ultrasonographers in the nation, what can you offer with surgeon-performed ultrasound? I teach my medical students that in the next 10 years they are going to throw away their stethoscopes, they are going to be carrying a Palm Pilot that has a beeper, a phone, a PDA, some sort of communicator device to a network of information or clinical repository, and it is going to have an ultrasound head. They are going to take the beeper off their belt and the patient with abdominal pain is going to be scanned at the bedside. We are not going to do as many CAT scans as we are doing now. Give us a view of the future here of where surgeon-performed ultrasound with acute abdominal conditions is going.
I appreciate the opportunity to discuss this paper. As this paper is an issue of judgment, I think it is a difficult area to study.
Dr. Richard J. Howard (Gainesville, FL): This paper certainly adds a lot to our literature, and confirms the prejudice of most of us that when the laboratory studies and x-ray studies aren’t helpful it is time to do a history and physical. That is something we have to keep reminding our residents about.
What we find at our institution, and I would like to ask if it occurs in your institution, is that for the residents and in many practices for the attending physician and surgeon as well, the most valuable commodity isn’t the dollars it cost to get a CT scan or some other x-ray study, but their time. So when they are consulted or asked to come to the emergency room to see a patient, they say, get a CT scan person, call me when it is done, and then I will either come to the emergency room, or for attendings in private practice and, for our own attendings as well, then I will come into the hospital.
We did a study in our own emergency room just asking the value of a plain film of the abdomen in patients who come in with acute abdominal pain, not signs or symptoms of obstruction but signs and symptoms of peritonitis, whether they had an operation or not, and found that it led to valuable information in only 4% of the cases. If they have free air, that is better seen on a CT scan or on a chest x-ray than on a plain film of the abdomen.
I would like to ask the authors about the issue I previously raised, whether resident time was such a valuable commodity that many of these tests may have been asked for to facilitate their own schedules.
Dr. Robert R. Nesbit, jr. (Augusta, GA): Two quick questions.
I understand that there are surgical attending physicians in the hospital involved in making decisions on these patients, but I wonder if the other services, which are seeing the patients first and may be ordering the tests, have attending levels there and involved as well.
Also, one of my younger colleagues tells me that he can get a CT scan as quickly as he can get plain films of the abdomen—and since he may need it anyway, he goes ahead and gets a CT initially. Would you comment on that approach?
Dr. Greg Timberlake (Jackson, MS): Dr. Rozycki, I enjoyed your presentation very much. I think all of us in academic centers with training programs struggle with this decision of whose judgment is being used in ordering these advanced imaging tests. That would be my question. Who did make the decision for these tests? Was it the referring physician? Your surgical residents? Some combination? Second, since you have identified this significant issue at Emory, can you tell us what are your plans to try and reduce this? How are you going to give these people who don’t have good judgment good judgment in the next 5 years?
Dr. Peter Nichol (Madison, WI): I am actually a resident, so I feel like I could stand up here and give a little input. First of all, I enjoyed the discussion, I enjoyed the paper. But one problem we have had as residents is that, of course, a lot of these patients get screened by ER physicians, and a fair number of them receive narcotics for belly pain before our examining them. And I am just wondering if you guys have looked at that factor in your study and physical examination.
Two, I have found as a resident there certainly is a learning curve for the abdominal exam. I still find it very challenging. Although I think I am fairly good and reliable at abdominal exam, it certainly helps to have somebody senior to you guiding you through that a number of times before you start making the decisions about, yes, this patient needs to go to the OR; no, we need to get a CT scan.
Dr. Grace S. Rozycki (Atlanta, GA): I would like to thank the discussants for their insightful comments.
The primary issue in this study is that of the need for advanced tests in critically ill surgical patients. All of the patients in this study were referred from other physicians, and therefore most of these studies were already ordered before the surgeon evaluated the patient. Generally, consults for general surgery patients are evaluated by the PGY-3 surgery resident, but because these patients were so sick, the higher-level surgery residents and the in-house attending were rapidly involved in the patient’s evaluation and management.
Patients who suffered a gastrointestinal bleed rarely benefited from a CT scan but frequently had their bleeding sites localized, 77% of those patients with lower GI bleeds and 86% with upper GI bleeds. Of the 53 patients who had an ischemic or infarcted organ, 31 had advanced tests but only 20 of those were useful. Of the 14 patients who had nontherapeutic or negative celiotomies, 6 had advanced tests, 5 of whom had false-positive CT scans. Some patients had equivocal peritonitis, and if they also received narcotics, their examinations were difficult to clarify. In select patients who fall into this category, the advanced test may have a role in clarifying the physical examination.
Ultrasound may be useful as a screening tool for the detection of gallbladder disease, abdominal aortic aneurysms, and ascites. Considering that our ultrasound machines are in the emergency department as well as our intensive care unit, this modality should be used more often by surgeons for the evaluation of these patients.
Finally, a comment on the value of advanced tests for these patients. In general, our colleagues in emergency and internal medicine should be aware of our data in order to expedite the evaluation of these patients. There is no substitute for sound clinical judgment and a good history and physical examination. It may take time for residents to learn the fine points of examining a patient with an acute abdomen, especially if the patient has comorbid factors and needs an operation emergently. This further underscores the importance of the attending’s presence and examination of these patients.
Footnotes
Presented at the 113th Annual Session of the Southern Surgical Association, December 3–5, 2001, Hot Springs, Virginia.
Correspondence: Grace S. Rozycki, MD, RDMS, FACS, Director, Trauma/Surgical Critical Care, Associate Professor of Surgery, Emory University School of Medicine, 69 Butler Street, SE, Atlanta, GA 30303.
E-mail: grozyck@emory.edu
Accepted for publication December 2001.
References
- 1.Suzman MS, Talmor M, Jennis R, et al. Accurate localization and surgical management of active lower gastrointestinal hemorrhage with technetium-labeled erythrocyte scintigraphy. Ann Surg 1996; 244: 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA 1961; 178: 261. [DOI] [PubMed] [Google Scholar]
- 3.Rozycki GS, Ballard RB, Feliciano DV, et al. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1,540 patients. Ann Surg 1998; 228: 557–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen FS, Sohn N. Lower gastrointestinal bleeding. In: Cameron JL. Current surgical therapy, 7th ed. St. Louis: Mosby; 2001: 322–327.
- 5.Rantis PC, Harford FJ, Wagner RH, Henkin RE. Technetium-labelled red blood cell scintigraphy. Is it useful in acute lower gastrointestinal bleeding? Int J Colorectal Dis 1995; 10: 210–215. [DOI] [PubMed] [Google Scholar]
- 6.Richter JM, Christensen MR, Kaplan LM, Nishioka NS. Effectiveness of current technology in the diagnosis and management of lower gastrointestinal hemorrhage. Gastrointest Endosc 1995; 41: 93–98. [DOI] [PubMed] [Google Scholar]
- 7.Hunter JM, Pezim ME. Limited value of technetium 99m-labeled red cell scintigraphy in localization of lower gastrointestinal bleeding. Am J Surg 1990; 159: 504–506. [DOI] [PubMed] [Google Scholar]
- 8.Sugarbaker PH, Bloom BS, Sanders JH, Wilson RE. Preoperative laparoscopy in diagnosis of acute abdominal pain. Lancet 1975; 442–444. [DOI] [PubMed] [Google Scholar]
- 9.Cortesi N, Zambarda E, Manenti A, et al. Laparoscopy in routine emergency surgery. Am J Surg 1979; 137: 647–649. [DOI] [PubMed] [Google Scholar]
- 10.Anteby SO, Schenker JG, Polishuk WZ. The value of laparoscopy in acute pelvic pain. Ann Surg 1975; 181: 484–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brandt CP, Priebe PP, Eckhauser ML. Diagnostic laparoscopy in the intensive care patient: avoiding the nontherapeutic laparotomy. Surg Endosc 1993; 7: 168–172. [DOI] [PubMed] [Google Scholar]
- 12.Larson GM. Laparoscopy for abdominal emergencies. Scand J Gastroenterol 1995; 30 (suppl 208): 62–66. [DOI] [PubMed] [Google Scholar]
- 13.Boyd WP, Nord HJ. Diagnostic laparoscopy. Endoscopy 2000; 32: 153–158. [DOI] [PubMed] [Google Scholar]
- 14.Reiertsen O, Rosseland AR, Hoivik B, Solheim K. Laparoscopy in patients admitted or acute abdominal pain. Acta Chir Scand 1985; 151: 521–524. [PubMed] [Google Scholar]
- 15.Mouret P, Francois Y, Vignal J, et al. Laparoscopic treatment of perforated peptic ulcer. Br J Surg 1990; 77: 1006. [DOI] [PubMed] [Google Scholar]
- 16.Sunderland GT, Chisholm EM, Lau WY, et al. Laparoscopic repair of perforated peptic ulcer. Br J Surg 1992; 79: 785. [DOI] [PubMed] [Google Scholar]
- 17.Memon MA, Brow G. Laparoscopic closure of acutely perforated duodenal ulcer: an early experience. Irish Med J 1993; 86: 106–107. [PubMed] [Google Scholar]
- 18.Feliciano DV. The acute abdomen. In: Beahrs RW, Beart RW, Pemberton JH. Surgical consultations, 1st ed. St. Louis: Mosby; 1993: 1–28.
- 19.Shaff MI, Tarr RW, Partain CL, et al. Computed tomography and magnetic resonance imaging of the acute abdomen. Surg Clin North Am 1988; 68: 233–254. [DOI] [PubMed] [Google Scholar]