Abstract
Introduction
During World War II, failure to treat penetrating colon injuries with diversion could result in court martial. Based on this wartime experience, colostomy for civilian colon wounds became the standard of care for the next 4 decades. Previous work from our institution demonstrated that primary repair was the optimal management for nondestructive colon wounds. Optimal management of destructive wounds requiring resection remains controversial. To address this issue, we performed a study that demonstrated risk factors (pre or intraoperative transfusion requirement of more than 6 units of packed red blood cells, significant comorbid diseases) that were associated with a suture line failure rate of 14%, and of whom 33% died. Based on these outcomes, a clinical pathway for management of destructive colon wounds was developed. The results of the implementation of this pathway are the focus of this report.
Methods
Patients with penetrating colon injury were identified from the registry of a level I trauma center over a 5-year period. Records were reviewed for demographics, injury characteristics, and outcome. Patients with nondestructive injuries underwent primary repair. Patients with destructive wounds but no comorbidities or large transfusion requirement underwent resection and anastomosis, while patients with destructive wounds and significant medical illness or transfusion requirements of more than 6 units/blood received end colostomy. The current patients (CP) were compared to the previous study (PS) to determine the impact of the clinical pathway. Outcomes examined included colon related mortality and morbidity (suture line leak and abscess).
Results
Over a 5.5-year period, 231 patients had penetrating colon wounds. 209 survived more 24 hours and comprise the study population. Primary repair was performed on 153 (73%) patients, and 56 patients had destructive injuries (27%). Of these, 40 (71%) had resection and anastomosis and 16 (29%) had diversion. More destructive injuries were managed in the CP group (27% vs. 19%). Abscess rate was lower in the CP group (27% vs. 37%), as was suture line leak rate (7% vs. 14%). Colon related mortality in the CP group was 5% as compared with 12% in the PS group.
Conclusions
The clinical pathway for destructive colon wound management has improved outcomes as measured by anastomotic leak rates and colon related mortality. The data demonstrated the need for colostomy in the face of shock and comorbidities. Institution of this pathway results in colostomy for only 7% of all colon wounds.
Few injuries have caused as much controversy with respect to management over the years as penetrating colon injuries. While in the Civil War and even World War I abdominal wounds were almost uniformly fatal, improved triage and transport during World War II meant large numbers of casualties survived until surgical care could be administered. Reviews of colon wound outcomes during this time led the U.S. Surgeon General to mandate exteriorization or proximal diversion for all colon wounds during the war. 1
In the years following the war, there was growing recognition that civilian colon injuries were generally less destructive and that many were amenable to primary repair. 2 This premise has been examined by a number of authors, and due to this body of work, primary repair of nondestructive colon wounds regardless of risk factors is considered the standard of care at most institutions. 3–8
Optimal management of destructive colon wounds requiring resection remains controversial, however. In 1994, we reviewed our experience with destructive colon injuries, in which a requirement of greater than 6 units/blood intraoperative transfusion or underlying medical illness were found to contribute to anastomotic breakdown. 9 In this high-risk group, leak rate was 42% as opposed to only 3% in the low risk patients. Death rate in the high-risk patients with anastomotic leak was 40%. Due to these findings, a clinical pathway was developed for the management of destructive colon wounds, suggesting diversion rather than repair in such high-risk patients.
In the current study, our recent experience with penetrating colon injury is examined with special consideration of outcome in destructive injuries after clinical pathway institution.
METHODS
Patients
All patients treated for penetrating colon injury over a 5.5-year interval were identified from the trauma registry of the Presley Regional Trauma Center. Records were reviewed for demographics, injury characteristics, hospital course, and outcome. Studied outcomes included suture line failure, intraabdominal abscess, colon related death, and total mortality. Variables studied as possible factors related to suture line disruption were Injury Severity Score (ISS), AAST Injury Scaling and Scoring System Colon Injury Score (CIS), 10 moderate or massive fecal contamination, admission systolic blood pressure, admission base deficit, systolic blood pressure < 90 in the 24 hours following operation, operative transfusion requirement, left sided colon injury, and number of suture lines. Fecal contamination was defined as minimal if there was only a small amount confined to the area of the injury, moderate if a single quadrant of the abdomen was involved, and massive if more than one quadrant of the abdomen was soiled. Injuries were classified as left or right sided based on their relationship to the middle colic vessels. Patients with both left and right-sided injuries were analyzed as left sided with respect to leak risk.
Patient Management
Patients determined on evaluation to have peritoneal penetration underwent laparotomy. After initial control of hemorrhage, the colon injury was assessed while attempting to minimize fecal spillage. Injuries amenable to primary repair underwent debridement and closure in a two layer fashion (000 absorbable suture in an inner running layer followed by an outer layer of 000 silk in an interrupted Lembert fashion). Injuries requiring segmental resection were treated with two-layer anastomosis or end colostomy based on the surgeons’ evaluation of concomitant risk factors. Since development of a clinical pathway in 1995, patients with destructive injuries and a transfusion requirement greater than 6 units/blood before or during surgery or patients with significant underlying medical illness were classified as high risk, and received diversion. Other patients were classified as low risk and underwent resection and anastomosis. Surgeons were free to diverge from this pathway based on clinical judgment.
Statistical Analysis
Statistical analysis was performed using Statview 5.0 (SAS Institute Inc., Cary, NC). Dichotomous variables were compared using Chi-square or Fisher exact test where appropriate. Continuous variables were compared using Student’s t-test. Factors contributing to the development of suture line leak were determined using logistic regression analysis. Significance is defined as P < .05.
RESULTS
General Population
From December 1995 through May 2001, 231 patients were admitted with penetrating colon injuries. Of these, 209 (187 male/22 female) survived greater than 24 hours and contributed to the data analysis. One hundred and seventy-one (82%) sustained gunshot wounds, 25 (12%) were stab wounds, and 13 (6%) were shotgun injuries. Mean ISS for the group was 14 and the mean CIS was 2.4. Forty-two percent of injuries involved the right colon, 56% were left sided, and 2% had both right and left-sided injuries. Suture line leak occurred in 7 patients (3%) and 8 patients died (4%).
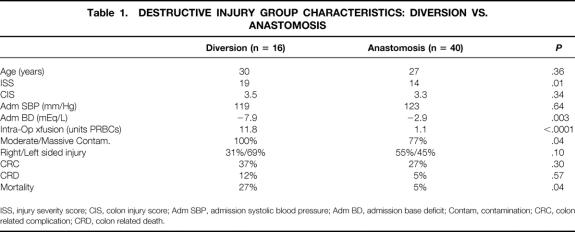
Destructive colon injuries requiring resection comprised 27% (56 patients) of the population. The overall incidence of colon related complications (abscess, suture line leak, wound infection) in this group was 25%. Forty patients (71%) underwent resection/anastomosis (ANAST) and 16 (29%) underwent diverting colostomy (DIV). Subgroup characteristics and outcomes are compared in Table 1. As expected, the DIV group was more severely injured with higher ISS and lower base deficit on admission than the ANAST group. This was accompanied by a larger intraoperative blood requirement. There was also more extensive contamination in the DIV group. Colon related complications and colon related death rates were not statistically different, but overall death rate was higher in the DIV group. Of the 16 patients in the DIV group, 8 have undergone colostomy reversal. Complication rate in this group was 37% (3/8) and included subcutaneous abscess, intraabdominal abscess, and peri-operative pneumonia. None of these patients died.
Table 1. DESTRUCTIVE INJURY GROUP CHARACTERISTICS: DIVERSION VS. ANASTOMOSIS
ISS, injury severity score; CIS, colon injury score; Adm SBP, admission systolic blood pressure; Adm BD, admission base deficit; Contam, contamination; CRC, colon related complication; CRD, colon related death.
Effects of Clinical Pathway
Overall compliance with the clinical pathway was 90%. In order to determine the effect of pathway institution on outcome and ostomy rates, the current group (CP) was compared to the group cared for during the previous study (PS) before pathway development. A larger proportion of destructive injuries were managed in the CP group (56/209, 27%) as compared to the PS group (60/316, 19%:P = .03). Resection and anastomosis was performed in 71% versus 72% of cases in the CP and PS groups respectively. Colon related outcome in these patients is shown in Table 2. Abscess and suture line leak rates were lower in the CP group, but this did not reach statistical significance.
Table 2. COMPLICATIONS AND OUTCOME IN PATIENTS UNDERGOING RESECTION/ANASTOMOSIS: CLINICAL PATHWAY VS. PREVIOUS STUDY
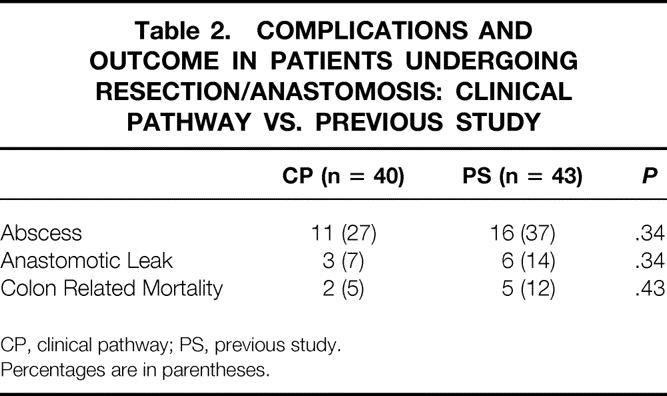
CP, clinical pathway; PS, previous study.
Percentages are in parentheses.
Of the destructive injuries, 25% were classified as high risk (underlying medical illness, > 6 units PRBC transfusion) in both the CP and PS groups. In the remaining low risk patients, introduction of the clinical pathway decreased the number of patients undergoing diversion 31% (14/45) to 9% (4/42:P = .01)
If the 153 patients in the CP group with nondestructive injuries undergoing simple repair are compared the ANAST group, some expected differences emerge. ANAST patients had a higher mean colon injury score (3.3 vs. 2;P < .0001) than those with simple repair. This, combined with a larger proportion of patients with moderate or massive intraabdominal contamination in the resection group (77% vs. 23%:P < .0001), explains the higher abscess rate in the ANAST group (27% vs. 11%:P = .01). The leak rates of the two groups, however, are not statistically different, with leaks occurring in 3 (7%) in the ANAST group versus 4 (3%) in the simple repair group (P = .16). This is in contrast to the PS group before pathway development, in which a larger proportion of suture lines leaked in the group requiring resection (14%) than in the group treated with simple colon repair (3%, P = .002).
Resection and Anastomosis: Analysis of Suture Line Breakdown
The three patients with suture line leak in the ANAST group were analyzed individually. Two of these were otherwise healthy males without significant shock or transfusion requirements. Both sustained isolated gunshot wounds to the left colon requiring resection and anastomosis. One developed fever on postoperative day 12, and was found to have a left flank abscess, which was drained. He subsequently developed an enterocutaneous fistula from his colon repair but was lost to follow-up after 3 weeks post discharge. The second patient developed an abscess discovered on postoperative day 7. On re-operation, the segment of colon with the repair was found to have herniated into the large blast cavity from the high velocity from the projectile, causing local ischemia and necrosis with suture line disruption. He underwent diverting colostomy with reversal 5 months later, which was uneventful. The third leak occurred in a patient with injuries to the duodenum and jejunum, both of which were repaired primarily. He required 8 units of blood intraoperatively and was left in discontinuity after resection of his destructive sigmoid colon injury. He underwent anastomosis 48 hours later when he had stabilized and cleared his metabolic acidosis, representing a deviation from the clinical pathway. On postoperative day 8, he was found to have an abscess associated with a disrupted colon anastomosis and underwent diversion. The patient went on to develop multiple organ failure and eventually died.
In order to determine if factors that could have predicted whether or not these patients’ risk of anastomotic leak were identifiable, admission hemodynamics and injury characteristics were compared between the patients who developed leaks and those who did not leak. These data are shown in Table 3. There were no differences between those with leaks and those without leaks in age, ISS, CIS, admission blood pressure, admission base deficit, delay until repair, degree of contamination, intraoperative hypotension intraoperative transfusion requirement, or presence of colo-colostomy.
Table 3. HEMODYNAMICS AND INJURY CHARACTERISTICS IN PATIENTS UNDERGOING RESECTION AND ANASTOMOSIS: SUTURE LINE LEAK VS. NO LEAK
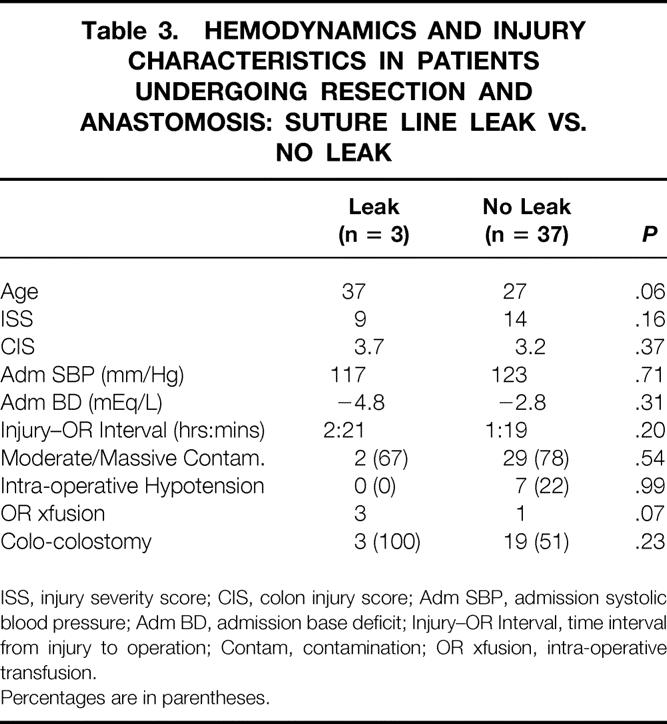
ISS, injury severity score; CIS, colon injury score; Adm SBP, admission systolic blood pressure; Adm BD, admission base deficit; Injury–OR Interval, time interval from injury to operation; Contam, contamination; OR xfusion, intra-operative transfusion.
Percentages are in parentheses.
All Suture Lines: Analysis of Risk Factors
Because suture line leak rate was similar in the simple repair group and the ANAST group, the relationship between commonly reported risk factors for colon suture line breakdown and leak rate for all colon repairs was examined. Of 193 patients with suture lines (40 ANAST, 153 simple repair), 7 developed leaks. Univariate analysis of risk factors (ISS, CIS, admission SPB, admission base deficit, left sided injury, massive/moderate contamination, OR transfusion, hypotension following surgery, number of suture lines, OR transfusion requirement) showed only number of suture lines as significantly different between patients who leaked and those who did not, with more average suture lines per patient in the group developing colon repair leak. However, regression analysis using variables with P ≤ .20 on univariate analysis (ISS, CIS, number of suture lines, massive/moderate contamination, episodes of hypotension in the 24 hours following surgery and OR transfusion requirement) failed to demonstrate any of these conditions as independent risk factors in suture line failure.
DISCUSSION
In the second half of the 20th century, management of penetrating colon injury has shifted 180 degrees. Mandatory colostomy in World War II for all colon injuries has been supplanted by the idea that the majority of (if not all) colon wounds can be repaired without diversion. Several investigators have contributed to the body of knowledge leading to this change. Stone and Fabian first prospectively studied this idea in 1979 and concluded that in patients without concomitant risk factors, repair was safer than diversion with respect to complications. 11 This work has been expanded by prospective series 12–14 as well as three prospective, randomized trials 15–17 demonstrating that primary repair of all civilian nondestructive colon wounds should be considered the standard of care. Controversy remains, however, concerning optimal management of injuries requiring resection. Work from our institution (the PS group) has shown a leak rate of 14% in unselected patients with destructive injuries undergoing anastomosis. 9 Subgroup analysis of these leaks demonstrated that patients with an intraoperative transfusion requirement greater than 6 units/blood or underlying medical illness were at very high risk for leak (42%), while only 3% of low risk patients leaked. This 14% is higher than the leak rates of 0%–5% reported in previous literature 14–18 for injuries requiring simple repair, and these findings prompted institution of a clinical pathway recommending diversion for patients with destructive colon injuries in this high risk group. This project demonstrates that using these guidelines significantly reduces the number of colostomies done in low risk patients. Suture line leak rate appears to be lower, and is now not statistically different that in patients undergoing simple colonic repair.
A growing body of evidence supports the concept that method of colon wound management does not affect the incidence of intraabdominal complications. George et al. in 1988 found an overall septic complication rate of 33%, and this was unrelated to primary repair. 19 This has been echoed by others; most recently by Demetriades et al. in the AAST multicenter prospective study on destructive colon wounds. 20 This study found that transfusion requirement ≥ 4 units/blood, severe fecal contamination and single agent antibiotic prophylaxis were independent risk factors for abdominal complications, while surgical method of colon wound management was not. Our current work supports this. While the DIV group was generally more severely injured, colon-related complications and colon-related mortality were the same. Colon injury related complications, although related to leak rate, occur commonly in the absence of suture line leak. Thus, decisions aimed at avoiding suture leak might not be expected to influence colon-related complications. While colon related mortality did not differ between the ANAST and DIV groups, overall death rate was higher in the DIV group. This may indicate that overall severity of injury and shock contributes more to mortality than colon management.
Analysis of leakage in colonic repairs may lead to identification of factors contributing to suture line failure. Patients in the current study underwent diversion if they were deemed high risk based on transfusion requirement or underlying medical illness. This led to a trend toward fewer leaks as compared to the PS group (14%–7%). One suture line failure was due to technical factors (ischemia after herniation of colon repair into a blast cavity), and one was in a patient that would not have undergone anastomosis had the pathway been followed. If these two are excluded from the analysis, the leak rate attributable to clinical pathway failure is only 3%, – a rate similar to elective colon resection.
Current standard of care for nondestructive wounds is primary repair, which has a low attendant leak rate. Incidence of suture line disruption has historically been higher for patients undergoing resection and anastomosis than in patients requiring simple repair. With more careful selection of patients eligible for anastomosis, leak rates are now similar. Other factors which have been proposed as risk factors for suture line leak include need for colo-colostomy, significant fecal contamination, and the presence of left sided colon injury. 21 The current data fail to identify these as risk factors, with similar rates of colo-colostomy, moderate to massive fecal contamination, and left sided injuries in those developing leaks and those without leaks. ISS, CIS, and interval from injury to surgery were also similar in the two groups, suggesting that these factors, while related to overall outcome, do not predict suture leak. The group with suture line leak is small, however. Leak from colon anastomosis, while potentially devastating, is an uncommon complication, occurring in only 3 patients in the current series. Analysis of associated risk factors in such small numbers of patients is problematic, and makes data interpretation difficult.
Authors have advised that complications due to colostomy takedown need to be considered in the overall morbidity of diversion. 22,23 Takedown carried significant morbidity (abscess, pneumonia) in the current group with approximately a third experiencing complications of some kind. Certainly ostomy commits patients to an additional operation with potential morbidity, to which low risk patients need not be exposed.
In summary, careful scrutiny of past leak rates at our institution has identified an intraoperative transfusion requirement greater than 6 units/blood or underlying medical illness as conditions associated with suture line leak. In the current study, diversion rather than primary repair was performed in this high-risk group. With this, leak rates have improved, and are no longer distinguishable from leak rates in patients managed with the current standard of care for nondestructive wounds: primary repair. In patients with destructive colon wounds but without these risk factors, resection and anastomosis has a low associated leak risk and should be performed regardless of wound location, degree of contamination, or associated injury. Some advocate primary repair in all destructive injuries despite associated risk factors. Prospective, randomized data supporting this viewpoint do not exist, and until such data are available, we do not support anastomosis in the most severely injured patients (approximately 7% of all patients with penetrating colon injury). While the institution of the clinical pathway did not result in statistical differences relative to colon-related complications (293 per group by power analysis), there were statistically fewer colostomies performed in the low risk group and the complication rates were lower. We feel these differences are clinically relevant.
Discussion
Dr. H. Harlan Stone (Phoenix, AZ): I enjoyed this presentation greatly, but, unfortunately, the volume of cases was not so great as to reach statistical significance in any all category. This is the only problem that one faces with the paper.
Otherwise I think it is a beautiful demonstration of how problems can be identified, how they can be avoided, and then subsequently how to apply such to the management of future patients. After all, that is what these meetings are for.
I have just two comments. The first I am going to phrase in the form of a question.
Since almost all bowel anastomoses seal by a fibrin gel, unless there is this fibrin clot there can be no microbiological seal. I would like to see the same data reanalyzed on the basis of coagulopathy. I think the third patient’s leak, as mentioned by Dr. Croce, might demonstrate that coagulopathy played a major role. There are many factors that influence clotting, not just shock itself, but also massiveness of transfusion, hypothermia and the like. So I wonder if it would be possible from your data to reanalyze that concern.
Second, it is with regret that one must face the fact that the randomized study in the shock-trauma patient is a thing of the past, because there is really no way you can obtain a valid, informed consent under these circumstances. No family members are present and, if so, they certainly are not in a mental state to where they can give such. Thus, we must now resort to retrospective reviews, testimonials, and, if you are sophisticated, meta-analysis. One of my most treasured faculty members in Phoenix looks down on this concept of meta-analysis and has coined an adage that I think it is quite true: meta-analysis is to analysis as metaphysics is to physics.
Dr. R. Phillip Burns (Chattanooga, TN): As already mentioned by Dr. Stone, this paper is a nice demonstration of the application of outcomes result to the formulation of a clinical pathway.
The initial study by this group in 1994 derived presumably as a result of surgeons figuratively carrying a pathway around in their head and showed risk factors that indicate there should be limitations to the application of primary colon resection. The results of this study was then presumably applied to a pathway for care that was written on the wall in the OR – or, I suppose in Memphis, on a Palm Pilot.
Many of us, while respectful of the time-honored principles of independent clinical and operative judgment, have felt that similar such pathways would help in continued improvement of patient care in the surgical arena. This should also make the study of a larger number of patients across the surgical spectrum easier and hopefully give us more objective information to counter arbitrary and at times inaccurate information suggested by some of our critics. I appreciate the fact that your pathway does leave room for individual clinical judgment by the surgeon.
Most of us applaud efforts to reduce the incidence of Hartman resection and ostomy formation for colorectal injury because all of us have at one time or another been victimized by a bad outcome or complication in a patient at the time of ostomy closure, several months after surviving a significant injury. Your paper details this attitude very nicely. I do have several questions.
You detailed comorbid factors. But did the type of combined injury have any impact on outcome, and most especially genitourinary tract injuries within that group, especially injuries to the ureter?
Were any of these procedures done as part of a damage control laparotomy and were any of these treated with either a second-look procedure, an open abdomen technique or Vacpack technique? If so, do you have any special recommendations in regard to inspection or evaluation of the anastomosis at that time?
In patients with primary anastomosis or closure, do you make any effort to cleanse or irrigate the colon or rectum at the time of the procedure as recommended by some colorectal surgeons?
The anastomoses presumably were all two-layered and hand-sewn. Was the type of suture material used the same? Do you do anything special to evaluate for ischemia? And what are your feelings about the use of staplers in this situation?
Lastly, in certain situations some of us feel that a subtotal colectomy and primary ileoproctostomy may be a safer way to manage these colon injuries or colon disease especially when both the right and left colon is involved. Do you have any feelings about this?
I enjoyed this paper very much. It was beautifully presented, as always.
Dr. Loring W. Rue, III (Birmingham, AL): This presentation represents another contribution of the Memphis group toward our understanding of the proper management of civilian colon injuries. It is driven by logic, by reason, and by data, and not by fiat, such as the Army Surgeon General’s orders of 1943. It is also an excellent example of how a periodic review of one’s clinical experience can lead to a modification of treatment algorithms to optimize patient outcomes. I have three questions for the authors.
First, regarding the preexisting medical conditions and the association with leak and the recommendation for diversion. As alluded to in your earlier reports, much of this information may be determined in a retrospective fashion. Help us put this in clinical context in the heat of battle. For example, would you divert a slightly obese patient with an initial glucose of 200 in whom you suspect has undiagnosed type 2 diabetes? Would a patient with chronic hypertension be considered as having a preexisting medical condition warranting diversion? Please elaborate on what “preexisting medical condition” really means.
Second, have you analyzed the time of injury to the time of surgery and whether this potentially contributes to the leak rate? As a tertiary care center, you must receive a number of patients from afar. Should colostomy be considered in patients with significant time delays to surgery?
Third, do associated organ injuries increase the propensity for anastomotic leak? In other words, do concomitant vascular, pancreatic, or duodenal injuries contribute to your complication rates and should colostomy be performed for destructive lesions in these situations?
Though the authors lament in their manuscript the difficulty of undertaking statistical analyses of small numbers of patients, the fact that only three colon leaks occurred in their series speaks volumes. There is much to learn from the data presented here today, and the Memphis group have clearly shown that though colostomy should be rarely performed, it should be selectively performed in certain circumstances.
Despite my earlier sarcasm regarding the World War II Army Surgeon General’s mandate, I do believe colon wounds sustained in a combat environment are different from civilian wounds. Many combat injuries are the consequence of high-velocity artillery fragmentation wounds with significant tissue destruction and entrainment of foreign debris and no tests of the management principles outlined here have been undertaken in a wartime environment. With American forces deployed in harm’s way today, until concrete data such as that presented by the Memphis group can be determined, the Surgeon General’s dictum of 1943 may still be appropriate in the combat wounded of 2001.
Dr. Harvey J. Sugerman (Richmond, VA): One of our failures was similar to one that you had in that a gunshot wound without any of the risk factors described underwent a resection but also required a nephrectomy. We performed a colon resection with a primary anastomosis. This occurred on the sixth postoperative day, necessitating resection and colostomy. So I ask whether if you have a nephrectomy beneath your a injury, whether that should be a contraindication to a primary anastomosis. I guess the answer to that question would require a multi-center retrospective study such as could be performed by the AAST or the Western Trauma.
Dr. Michael L. Hawkins (Augusta, GA): I want to ask you about the small subset of blunt trauma patients with mesenteric injury and ischemia with or without perforation. Do you use the same guidelines for colostomy or primary repair?
Dr. Basil A. Pruitt, jr. (San Antonio, TX): I was wondering whether you assessed nutritional status as one of the risk factors, since that can influence wound healing. If you did evaluate nutritional status, how was that done?
Dr. Louis G. Britt (Memphis, TN): I have one question. Does surgical judgment overrule algorithms or do algorithms overrule surgical judgment? I would just like for you to tell me what is next.
Dr. Preston R. Miller (Memphis, TN): Thank you all for your kind comments. We appreciate it.
This project illustrates the use of a clinical pathway and how it can be used to determine who would benefit from a colostomy in the face of destructive colon. If you look at the number of colostomies performed in the prior study and the number in this current study, they don’t differ. The difference is the accuracy with which colostomy is assigned to patients who will or will not need it.
The risk factors underlying comorbid condition and large transfusion requirements that were outlined by Dr. Stewart and the rest were used to carefully determine which patients in the current study would benefit, or, maybe more importantly, would not benefit or were not likely to benefit from colostomy. And because of this, there were significantly fewer colostomies performed in these low risk patients during the current study.
In response to the comments by the reviewers, I appreciate your comments, Dr. Stone, you mentioned the statistics. And there is no question about it, that is the difficulty with this type of analysis. Unfortunately for the people performing the statistics, and fortunately for the patients, this type of injury is uncommon; that is, leak and complication in this type of injury is uncommon. Because of that, coming up with P values that are striking is also difficult. We do believe that a decrease in the leak rate from 14% to 7%, although not statistically significant is certainly clinically significant.
You mentioned coagulopathy. I think that is a very good point. We haven’t looked at the data that way. But it would make sense in that in the previous studies the patients who were the sickest ones were more likely to leak, and that may certainly play a role in it.
Dr. Burns, you mentioned various associated injuries, and Dr. Sugerman also asked about nephrectomy. If you look at associated injuries, what you find is that in the three patients that Dr. Croce showed that leaked, only one of them had any associated injury with respect to other organs. The number of organs injured does not appear to relate to whether the patient leaks. It is related to complication, certainly, but not related to suture line leak.
Specifically, you asked about renal injuries. There was one patient who developed an abscess, and that patient had a ureter injury, which was not initially picked up. But as far as suture line leak, there doesn’t seem to be a relationship to other injuries. In the setting of damage control laparotomy, there was one patient who leaked who did undergo damage control laparotomy with a planned second look. He, because of his transfusion requirement, was a protocol, was a clinical pathway violation, and he unfortunately leaked and died. The rest of the patients that underwent damage control eventually received ostomy, whether at the first operation or at one of the second-look operations.
Dr. Rue, you also asked about the underlying medical conditions; exactly what sort of conditions are we looking at and is there a way to predict it on the front end? Well, that is difficult to sort out because you don’t always know the past medical history of these people. But what we are talking about is severe diabetes, HIV infection, cirrhosis – in this series there was one patient with leukemia, that type of thing. I think you are left with clinical judgment with respect to the patient who is hypertensive or the patient who may have borderline diabetes, and that has just been, unfortunately, varied from case to case.
As far as interval from injury to definitive operation, or initial operation, I was surprised when I looked at this data that although we do have a lot of patients who come from referring institutions, the intervals were all lower than six hours. They were all small. There was no relationship between injury interval and whether the patient leaked.
Dr. Sugerman, you asked about nephrectomy. It did not seem to be related. Associated organ injuries in general did not seem to be related to suture line leak but were related to complications.
Dr. Hawkins, the decision as to whether a resection in anastomosis is appropriate in a blunt trauma patient is fraught with a lot more complications, or a lot more potential problems, as you mentioned, with the possibility of mesenteric disruption in ischemia. And although we do try to follow this algorithm, it is left up to surgeon judgment, which ultimately is probably more important than algorithm. And in response to Dr. Britt’s question, my answer would be that surgeon judgment certainly is more important than an algorithm. Dr. Croce suggested that I also mention that it does depend on the surgeon.
I would like to thank the Association for the opportunity to close this paper. I would also like to thank Dr. Croce and Dr. Fabian in addition to the opportunity to close this paper for their continued mentorship and guidance.
Footnotes
Correspondence: Timothy C. Fabian, MD, Professor & Chairman, Department of Surgery, University of Tennessee Health Science Center, 956 Court Avenue, Suite G228, Memphis, TN 38163.
E-mail: tfabian@utmem.edu
Presented at the 113th Annual Session of the Southern Surgical Association, December 3–5, 2001, Hot Springs, Virginia.
Accepted for publication December 2001.
References
- 1.Office of the Surgeon General, Circular Letter No 178, October 23, 1943.
- 2.Woodhall JP, Ochsner A. The management of perforating injuries of the colon and rectum in civilian practice. Surgery 1951; 29: 305–320. [PubMed] [Google Scholar]
- 3.Flint LM, Vitale GC, Richardson JD, et al. The injured colon: relationship of management to complications. Arch Surg 1981; 193: 619–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haygood FD, Polk HC, Jr. Gunshot wounds of the colon: a review of 100 consecutive patients, with emphasis on complications and their causes. Am Surg 1976; 131: 213–218. [DOI] [PubMed] [Google Scholar]
- 5.Nallathambi MN, Ivatury RR, Rohman M, et al. Penetrating colon injuries, exteriorization vs. loop colostomy. J Trauma 1987; 27: 876–882. [PubMed] [Google Scholar]
- 6.Lucas CE, Ledgerwood AM. Management of the injured colon. Curr Surg 1986; 43: 190–193. [PubMed] [Google Scholar]
- 7.Thompson JS, Moore EE, Moore JB. Comparison of penetrating injuries of the right and left colon. Ann Surg 1981; 193: 414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shannon FL, Moore EE. Primary repair of the colon: when is it a safe alternative? Surgery 1985; 98: 851–860. [PubMed] [Google Scholar]
- 9.Stewart RM, Fabian TC, Croce MA, et al. Is resection with primary anastomosis following destructive colon wound always safe? Am J Surg 1994; 168: 316–319. [DOI] [PubMed] [Google Scholar]
- 10.Web Page. http://www.aast.org/injury/t15–20.html#colon.
- 11.Stone HH, Fabian TC. Management of perforating colon trauma: randomization between primary closure and exteriorization. Ann Surg 1979; 190: 430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Demetriades D, Charalambides D, Pantonowitz D. Gunshot wounds of the colon: role of primary repair. Ann R Coll Surg Engl 1992; 74: 381–384. [PMC free article] [PubMed] [Google Scholar]
- 13.Ivatury RR, Gaudino J, Nallathambi MN, et al. Definitive treatment of colon injuries: a prospective study. Am Surg 1993; 59: 43–49. [PubMed] [Google Scholar]
- 14.Cornwell ET, Velmahos GC, Berne JV, et al. The fate of colonic suture lines in high risk trauma patients: a prospective analysis. J Am Coll Surg 1998; 187: 58–63. [DOI] [PubMed] [Google Scholar]
- 15.Sasaki LS, Allaben RD, Golwala R, et al. Primary repair of colon injuries: a prospective randomized study. J Trauma 1995; 39: 895–901. [DOI] [PubMed] [Google Scholar]
- 16.Chappuis CW, Frey DJ, Dietzen CD, et al. Management of penetrating colon injuries: a prospective randomized trial. Ann Surg 1991; 213: 492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gonzales RP, Merlotti GJ, Holevar MR. Colostomy in penetrating colon injury: is it necessary? J Trauma 1996; 41: 271–275. [DOI] [PubMed] [Google Scholar]
- 18.Durham RM, Pruitt C, Moran J, et al. Civilian colon trauma: factors that predict success by primary repair. Dis Colon Rectum 1997; 40: 685–692. [DOI] [PubMed] [Google Scholar]
- 19.George SM, Fabian TC, Voeller GR, et al. Primary repair of colon wounds: a prospective trial in nonselected patients. Ann Surg 1989; 209: 728–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demetriades D, Murray JM, Chan L, et al. Penetrating colon injuries requiring resection: diversion or primary anastomosis? An AAST Prospective Multicenter Study. J Trauma 50: 765–775. [DOI] [PubMed] [Google Scholar]
- 21.Burch JM, Martin RR, Richardson RJ, et al. Evolution of the treatment of the injured colon in the 1980s. Arch Surg 1991; 126: 979–984. [DOI] [PubMed] [Google Scholar]
- 22.Thal ER, Yeary EC. Morbidity of colostomy closure following colon trauma. J Trauma 1980; 20: 287–291. [DOI] [PubMed] [Google Scholar]
- 23.Taheri PA, Ferrara JJ, Johnson CE, et al. A convincing case for primary repair of penetrating colon injuries. Am J Surg 1993; 166: 39–44. [DOI] [PubMed] [Google Scholar]