Abstract
Objective
To assess the quality of life (QOL) of patients after surgical reconstruction of a major bile duct injury from laparoscopic cholecystectomy (LC).
Summary Background Data
The incidence of bile duct injuries has increased dramatically since the introduction and widespread use of LC. Previous reports show that at long-term follow-up, most patients surgically repaired will have a successful outcome as measured by standard clinical parameters. However, there is a general impression that these patients have an impaired QOL. Data addressing QOL of these patients are limited.
Methods
A standard QOL questionnaire was sent to 89 patients after successful surgical repair of a major bile duct injury from a LC treated at the Johns Hopkins Hospital between 1990 and 2000. The instrument consisted of 30 items on a visual analog scale categorized into physical (15 items), psychological (10 items), and social (5 items) domains. The same questionnaire was sent to age- and sex-matched healthy controls (n = 100) and to patients who underwent uncomplicated LC (n = 100). An additional portion of the questionnaire inquired about outcome measures and legal action undertaken by patients.
Results
Overall QOL scores for bile duct injury patients in the three domains (physical, psychological, and social) were 76%, 77%, and 75%, respectively. QOL scores were comparable to those of patients undergoing uncomplicated LC and healthy controls in the physical and social domains but were significantly different in the psychological domain. Presenting symptoms, prior repair, level of injury, number of stents, length of postoperative stenting, and length of follow-up did not influence QOL scores. Repaired patients reported similar rates of abdominal pain, change in bowel habits, use of pain medications, and recent symptoms of fever or chills as LC controls. Thirty-one percent of responding bile duct injury patients reported having sought legal recourse for their injury. All QOL domain scores were significantly lower in the patients who pursued a lawsuit versus those who did not.
Conclusions
This study provides formal data evaluating QOL after surgical repair of major bile duct injuries from LC. Although there was a significant difference in the QOL as evaluated from a psychological dimension, bile duct injury patients reported QOL scores in the physical and social domains comparable to those of control patients. The decreased QOL assessment in the psychological dimension may be attributable to the prolonged, complicated, and unexpected nature of these injuries. The presence of a lawsuit appears to be associated with a poorer QOL assessment.
The introduction and widespread use of laparoscopic cholecystectomy (LC) in the 1990s have resulted in an increased frequency of biliary injuries and associated bile duct strictures. The estimated incidence of major bile duct injuries, which was 0.1% to 0.3%1,2 during the open cholecystectomy era, has risen to an estimated 0.4% to 0.6%3–6 for LC. Despite the hope that surgeons would undergo a “learning curve” with the new procedure and that the incidence would decline, the rate of bile duct injury with LC appears to be stable. 3–5 Major bile duct injuries from LC continue to be a problem, with substantial costs to our healthcare system. 7
When assessing outcome, it is important to consider the patient’s perspective on health-related quality of life (QOL). The concept of overall “health,” as defined by the World Health Organization in 1948, is “a state of complete physical, mental, and social well-being, and not merely the absence of disease and infirmity.”8
Quality of life is a broad concept that encompasses a patient’s assessment of all aspects of his or her experience. Health-related QOL encompasses several dimensions of health status that are directly experienced by the person. As it relates to surgical patients after a procedure, health-related QOL seeks to measure the impact of the disease process and/or procedure on the physical, psychological, and social aspects of the person’s life and feelings of well-being. 9
The early management and short-term results after surgical management of LC bile duct injuries have been previously reported and are generally considered to be excellent. 10–15 More recently, our institution has reported the clinical results of a series of 156 patients after surgical repair of major bile duct injuries with median follow-up of approximately 5 years. 16 In this series, more than 90% of patients surgically repaired after a LC major bile duct injury had a successful outcome as measured by standard clinical parameters. Despite these reports, there is a general impression that these patients may have an impaired QOL. Further, objective data addressing the QOL of these patients are limited.
This study was designed to assess the QOL of patients after successful surgical reconstruction from an LC bile duct injury and to provide comparison with patients having undergone an uncomplicated LC and with healthy controls. A separate portion of this study involved a questionnaire that asked patients about several outcome measures that might be expected as a result of biliary surgery and whether patients had pursued legal action as a result of their injury.
METHODS
Approval by the Joint Committee on Clinical Investigation of the Johns Hopkins Hospital was obtained for the data collection and methodology of this study. A standard QOL questionnaire 17 was mailed in November 2000 to 89 patients after successful surgical repair of a major bile duct injury from LC. Major bile duct injuries included transections or significant lacerations of the common hepatic duct, common bile duct, or major segmental ducts at the porta hepatis that required surgical reconstruction. Minor leaks from the cystic duct or gallbladder bed were excluded. Bile duct strictures after other surgical procedures or resulting from trauma were excluded, as were strictures from other benign inflammatory processes or malignant causes.
Clinical Management
Between January 1, 1990, and December 31, 1999, 118 patients underwent surgical reconstruction for their bile duct injury after LC at the Johns Hopkins Hospital. The presentation, management, and clinical outcome of these patients have been reported previously. 16 Of these, 107 patients had completed treatment at the time of follow-up, and 101 (94%) were considered to have a successful outcome. Five of the 101 patients with successful repair subsequently died of unrelated causes and 7 patients were lost to follow-up, resulting in a total of 89 patients who were sent QOL surveys and who form the basis of this report.
Patients were initially managed with percutaneous transhepatic cholangiography and placement of percutaneous biliary catheters. When the injury or stricture was at or near the bifurcation, both the right and left hepatic ductal systems were accessed with transhepatic catheters. Surgical reconstruction was generally performed as an elective procedure. If there was evidence of ongoing bile leak or sepsis, a period of 4 to 6 weeks was usually allowed to pass before repair, with the aim of reducing associated inflammation. During the intervening time, patients were discharged with catheters in place and then readmitted for definitive repair.
Surgical management consisted of a Roux-en-Y hepaticojejunostomy. The proximal hepatic duct was identified and mobilized in the cephalad direction with injured or strictured ductal tissue resected back to normal duct. The preoperative biliary catheters were exchanged for larger soft Silastic stents. After stent placement, a Roux-en-Y jejunal limb, approximately 60 cm long, was prepared for the biliary–enteric anastomosis. The anastomosis was performed as an end-to-side hepaticojejunostomy using a single layer of interrupted absorbable 4-0 sutures, with the transhepatic stent placed through the anastomosis. Individual anastomoses were performed for cases involving more than one major duct. The perianastomotic area was drained with closed-suction Silastic drains.
In the immediate postoperative period, the Silastic stents were connected to external drainage. On postoperative day 4 or 5, a cholangiogram was performed. If the study was satisfactory, the stents were internalized and the patient was discharged.
After discharge, the Silastic stents were exchanged on a routine 2- to 3-month basis by the interventional radiology staff. The overall length of postoperative stenting was determined by the treating surgeon based on injury location, clinical status, and follow-up cholangiography. A biliary manometric perfusion study or a 2-week clinical trial with the stent positioned above the anastomotic site, or both, was often completed before stent removal. 18 The length of postoperative stenting, calculated from the date of definitive repair at Johns Hopkins until the date of final stent removal, was defined as short (<4 months), intermediate (4–9 months), or long (>9 months).
Treatment was considered complete at the time of removal of all biliary stents. A patient was considered to have a successful repair if he or she had no or mild symptoms, not requiring investigation or treatment, attributable to the biliary tract injury or reconstruction. This definition is consistent with earlier reports from our institution. 15,16,19 The length of follow-up was calculated from the date of definitive surgical repair.
QOL Assessment and Analysis
The QOL instrument was a minor modification of the City of Hope Medical Center Quality of Life Survey, which was developed from work by Padilla et al. 20 and Present et al. 21 The survey consisted of 30 items categorized into physical (15 items), psychological (10 items), and social (5 items) domains. Each question requires a response on a visual analog scale (measuring 100 mm) with word extremes as anchors at each end, and responses were graded with a continuous percentile score. This survey, or minor modifications of it, has been used to assess QOL in patients with cancer, patients after pancreaticoduodenectomy for both benign and malignant etiologies, 22 patients with cardiovascular disease, 23 and patients after colostomy. 24 The survey instrument was subjected to psychometric analysis with assessment of reliability and validity using 686 subjects from the National Coalition for Cancer Survivorship, showing that this survey adequately measured QOL in this group using five measures of validity (content, predictive, concurrent, construct, and discriminant). 25 Reliability was measured using test–retest (r = 0.89) and internal consistency (r = 0.93).
The same questionnaire was sent to age- and gender-matched healthy controls (n = 100) and patients who had previously undergone an uncomplicated LC (n = 100). LC patients had undergone the procedure at least 6 months previously. Healthy controls consisted of volunteers drawn from personnel at the Johns Hopkins Hospital. LC patients were chosen as a comparable group for statistical analysis because these patients had undergone the same original procedure without the complications of a major bile duct injury and subsequent surgical reconstruction.
A separate portion of the questionnaire was sent to patients with surgically repaired LC bile duct injury and patients with uncomplicated LC that inquired about specific outcome measures. The questionnaire specifically asked about the following items, which might be expected after biliary tract surgery: change in bowel habits, symptoms of abdominal pain, use of pain medications, and recent episodes of fever or chills. A final question was sent to the patients with surgically repaired LC bile duct injury asking whether legal remedies had been pursued as a result of their injury.
Comparisons between groups were performed with the Student t test and chi-square statistics as appropriate. Results are reported as mean ± standard error or median. Significance was accepted at the 5% level.
RESULTS
Study Populations
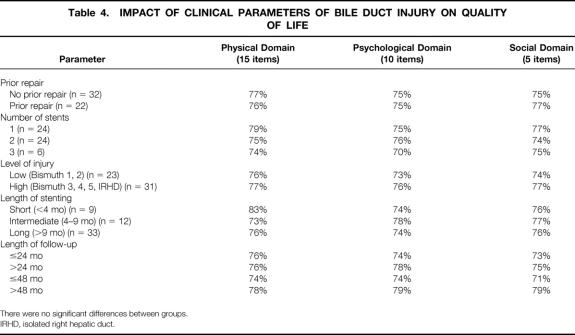
Of a total of 89 patients sent surveys who had undergone surgical reconstruction for an LC bile duct injury, 54 (61%) completed questionnaires were returned. In comparison, the response rate of LC patients was 50% (n = 50) and of healthy controls was 45% (n = 45). Study groups were similar with respect to gender, age, race, and follow-up time (Table 1). The mean age of LC bile duct injury patients was 46 ± 14 years, with 70% (n = 38) female and 81% (n = 44) white. Uncomplicated LC patients had a mean age of 49 ± 13 years, with 72% (n = 36) female and 86% (n = 43) white. The mean age of healthy controls was 48 ± 11 years; 71% (n = 32) of healthy controls were female and 87% (n = 39) were white. The median follow-up times for bile duct injury patients and uncomplicated LC patients were 59 ± 33 months and 43 ± 14 months, respectively.
Table 1. DEMOGRAPHICS AND LENGTH OF FOLLOW-UP OF THE STUDY POPULATIONS
BDI, bile duct injury; LC, laparoscopic cholecystectomy; HC, healthy controls.
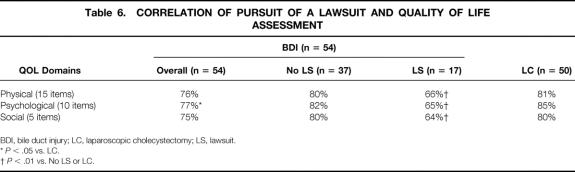
Patients with surgically repaired LC bile duct injury represent a diverse and complex group of patients in terms of prior management and presentation (Table 2). Only 12 patients (22%) had their injury discovered during their initial LC with an immediate attempt at repair. Of the patients whose injury was discovered in the postoperative period (n = 42, 78%), 10 patients (24%) underwent an attempt at repair before referral to Johns Hopkins. In total, 22 (41%) bile duct injury patients had undergone an attempt at repair before definitive repair at Hopkins. The primary clinical mode of presentation to Johns Hopkins was distributed among cholangitis (n = 21 [39%]), biliary leak (n = 17 [31%]), jaundice (n = 13 [24%]), or recognition during initial LC at Johns Hopkins (n = 3 [6%]).
Table 2. PRIOR MANAGEMENT, PRESENTATION, NATURE OF INJURY, AND USE OF STENTS IN SURGICALLY REPAIRED LAPAROSCOPIC CHOLECYSTECTOMY BILE DUCT INJURY PATIENTS
JHH, Johns Hopkins Hospital.
The level of obstruction or injury to the biliary tree of the 54 patients was classified as Bismuth 1 in 3 patients (6%), Bismuth 2 in 20 patients (37%), Bismuth 3 in 14 patients (26%), Bismuth 4 in 8 patients (14%), Bismuth 5 in 4 patients (7%), and an isolated right hepatic duct in 5 patients (9%). Overall, the majority of patients (n = 31 [57%]) had a high Bismuth level (Bismuth 3, 4, 5) or included an isolated segmental hepatic duct injury. The level of injury or obstruction is also reflected in the number of stents used: 24 patients (44%) with one stent, 25 patients (46%) with two stents, and 5 patients (9%) with three stents. The length of postoperative stenting after repair was classified as short (<4 months) in 10 patients (19%), intermediate (4–9 months) in 14 patients (26%), and long (>9 months) in 30 patients (55%).
QOL Assessment
The overall QOL scores for bile duct injury patients, uncomplicated LC patients, and healthy controls are shown in Table 3. For patients with surgically repaired LC bile duct injury, QOL scores in the physical, psychological, and social domains were 76%, 77%, and 75%, respectively. These QOL scores were comparable to those of the uncomplicated LC group (81%, 85%, and 80%, respectively) in the physical and social domain but were significantly lower in the psychological domain (P < .05). Similarly, healthy controls had QOL scores of 80%, 84%, and 80%, respectively, which were comparable to bile duct injury patients in the physical and social domains but were also significantly different in the psychological domain (P < .05). There were no statistically significant differences in QOL scores between the two control groups in any of the three QOL domains.
Table 3. OVERALL QUALITY OF LIFE (QOL) ASSESSMENT
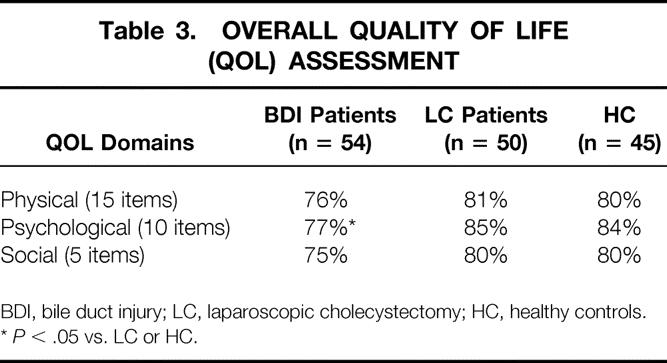
BDI, bile duct injury; LC, laparoscopic cholecystectomy; HC, healthy controls.
*P < .05 vs. LC or HC.
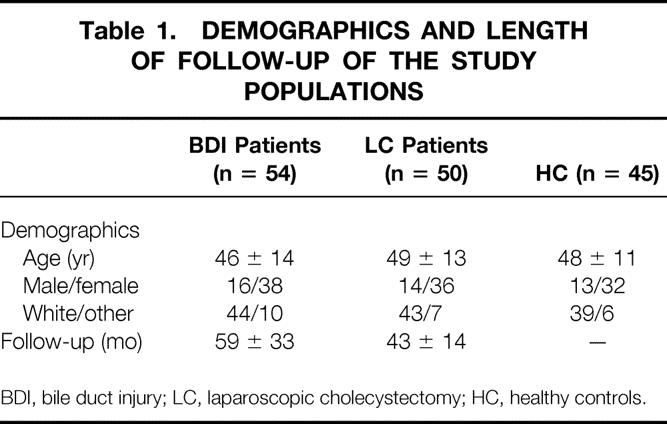
Analysis of clinical and management factors of patients with surgically repaired LC bile duct injury and the effect on QOL assessment is shown in Table 4. Factors such as presenting symptom, prior repair, level of injury, number of stents, and length of postoperative stenting did not significantly influence QOL scores for patients with surgically repaired LC bile duct injury. Further, the length of follow-up after definitive surgical repair did not affect QOL scores.
Table 4. IMPACT OF CLINICAL PARAMETERS OF BILE DUCT INJURY ON QUALITY OF LIFE
There were no significant differences between groups.
IRHD, isolated right hepatic duct.
The results of the specific outcome measurement assessment comparing patients with surgically repaired LC bile duct injury and uncomplicated LC patients are depicted in Table 5. Both groups reported comparable rates of abdominal pain, change in bowel habits, use of pain medications, and recent symptoms of fever or chills.
Table 5. OUTCOME MEASURES RESULTS
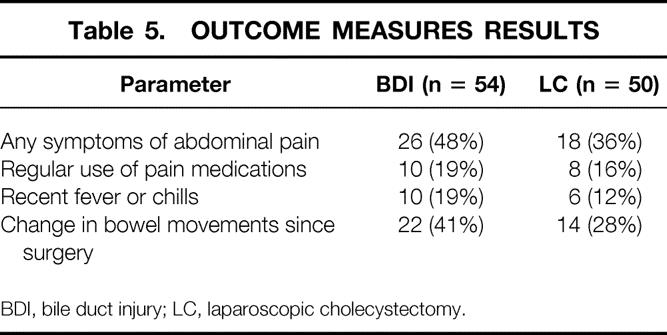
BDI, bile duct injury; LC, laparoscopic cholecystectomy.
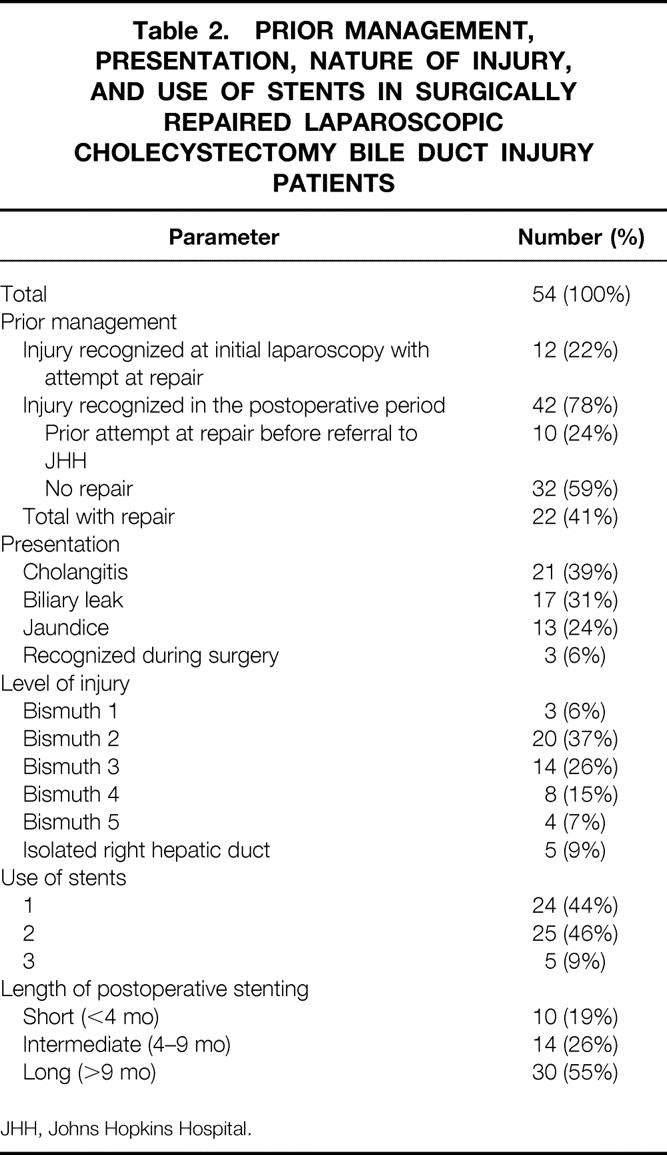
A substantial number of responding LC bile duct injury patients reported having sought legal action as a result of their injury (n = 17 [31%]). The QOL assessment of patients with surgically repaired LC bile duct injury subgrouped by those who pursued a lawsuit is shown in Table 6. QOL domain scores were significantly lower in the physical, psychological, and social domains in the patients who pursued a lawsuit (66%, 65%, and 64%, respectively) compared with those who did not (80%, 82%, and 80%, respectively) (P < .01). Further, there was no statistical difference in QOL scores between the LC bile duct injury patients who did not pursue a lawsuit and either control group in any of the three QOL domains (healthy control patient scores not shown).
Table 6. CORRELATION OF PURSUIT OF A LAWSUIT AND QUALITY OF LIFE ASSESSMENT
BDI, bile duct injury; LC, laparoscopic cholecystectomy; LS, lawsuit.
*P < .05 vs. LC.
†P < .01 vs. No LS or LC.
Because of the marked differences of QOL assessment in the subgroup that pursued legal remedies, an analysis of factors that might be predictive of pursuit of a lawsuit was completed (Table 7). Factors such as demographics, including age, race, and gender; presenting symptom; prior repair; level of injury; number of stents; and length of postoperative stenting were not predictive of whether patients pursued legal action for their injury.
Table 7. FACTORS ASSOCIATED WITH LAWSUIT (LS)
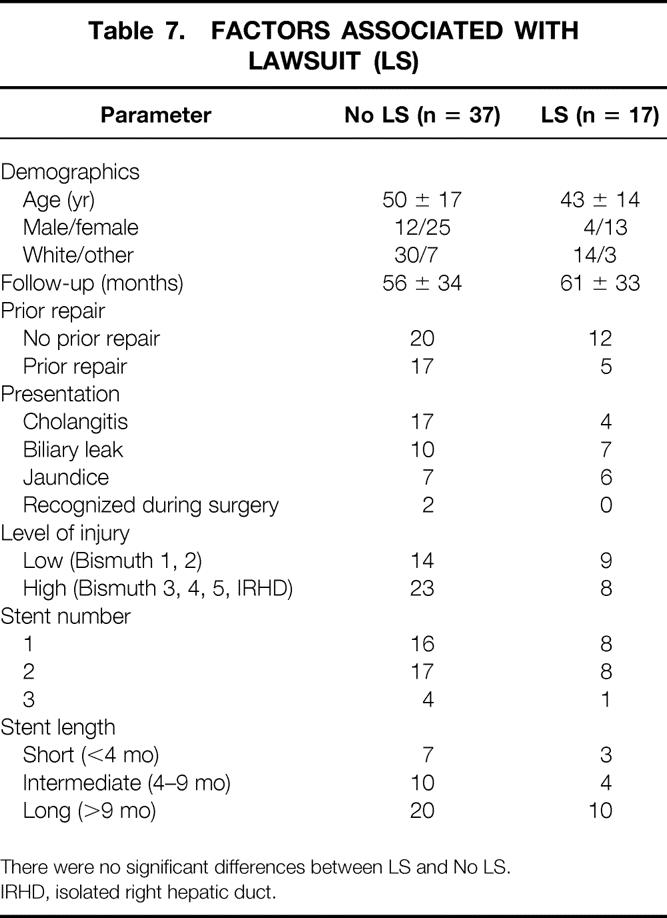
There were no significant differences between LS and No LS.
IRHD, isolated right hepatic duct.
DISCUSSION
The outcomes of patients after LC bile duct injury repair have been reported via several means. Studies have addressed outcomes in terms of postoperative complications, death, and hospital charges. Other reports have described large single-institution experiences of patient success in terms of standard clinical parameters. 7,16 During the last several years, QOL has been an issue of increasing importance in medicine and surgery. 9,26–28 However, to date, there are only limited available QOL data after the surgical repair of major LC bile duct injuries.
The current cohort of 54 patients with successful surgical reconstruction of an LC bile duct injury represents the first such published analysis formally addressing the issue of QOL. The cohort is representative of the current population of patients undergoing LC: the median age was 46 years, with a predominant female distribution. When the entire cohort of 54 patients with surgically repaired LC bile duct injury was compared with 50 uncomplicated LC patients and 45 healthy controls, there were no differences in the QOL assessment in the physical and social domains, but a significantly lower score was observed in the psychological QOL domain (see Table 3). When the bile duct injury patients were subgrouped and analyzed using clinical parameters that might influence QOL or length of follow-up, no differences in QOL scores were observed (see Table 4).
The explanation for the lower QOL scores in the psychological domain is uncertain but may be partly due to the unexpected, complicated, and prolonged nature of LC injuries and their treatment. Uncomplicated LC is generally associated with either outpatient surgery or a short hospital stay, a quick recovery, and expected reasonable hospital bills, and without loss of significant earning power. 29,30 Further, even in the era of informed consent, most LC patients, when asked after signing “informed” consent, cannot recall the risks associated with the procedure. 31 Major bile duct injuries associated with LC create a substantial, unexpected cost to individuals and to our healthcare system. 7 It is therefore not surprising that despite excellent long-term clinical results, patients are adversely affected psychologically by their injury, which often involves a prolonged recovery, disruption of lifestyle, loss of earning power, and large hospital bills associated with multiple, often painful, diagnostic and therapeutic procedures.
Only limited data are available in the literature addressing the issue of QOL after repair of a major bile duct injury. In a recent report by Boerma et al. 32 from the Netherlands, 106 patients who had sustained a variety of biliary injuries, ranging from cystic duct leaks to major transection, underwent QOL assessment. Only 31 of the patients, however, had undergone surgical reconstruction, with the majority managed with endoscopic or percutaneous balloon dilatation. Despite an overall excellent clinical outcome in the series, QOL was found to be reduced in both the physical and mental domains. Interestingly, QOL was reduced regardless of the extent of injury (minor leaks vs. major transection) or the type of treatment (endoscopic vs. surgical). These results would appear to be in stark contrast to the results in the current series, especially considering the magnitude of injury and nature of repair in our patients.
In the only comparable American series, published in abstract form, 17 patients who had undergone successful hepaticojejunostomy for repair of bile duct injury were compared with age- and sex-matched control patients who had undergone uncomplicated LC. 33 In this series, bile duct injury patients scored significantly lower in a different QOL instrument in five of eight domains, including physical, general health, emotional role, and mental health. Further details of the series are not available, but the findings with respect to emotional and mental health effects would certainly be consistent with our results.
Finally, an interesting component of our analysis was the finding that the subgroup of bile duct injury patients who pursued a lawsuit had a significantly worse QOL assessment in all domains compared with the subgroup of patients who did not pursue a lawsuit. Moreover, there was no difference in QOL assessment for patients with surgically repaired bile duct injury who did not pursue legal remedies and the control groups (see Table 6). It is well recognized that bile duct injury associated with LC can and frequently does result in lawsuits, often with settlements or decisions awarding plaintiffs large sums of money. 34,35 Whether QOL issues drive the pursuit of a lawsuit or the pursuit of a lawsuit factors into QOL assessment raises a seminal question of “the chicken or the egg” that is not answered by our analysis. Further, our analysis did not reveal any objective measure that was different between patients who pursued a lawsuit versus those who did not (see Table 7). It would clearly be informative to evaluate QOL in patients at different stages in the process of pursuing legal remedies.
In summary, the current study adds substantially to the literature on QOL after surgical repair of an LC bile duct injury. QOL assessment in biliary surgery is still in the early stages. There are opportunities for future evaluation of these patients. Future studies incorporating QOL at various time points of management would be especially illustrative in understanding these patients and their recovery. Analysis completed before definitive repair of the sustained injury, at the time of repair, before percutaneous transhepatic stent removal, and at serial postoperative time intervals could provide valuable data as to the longitudinal QOL that these patients experience throughout the duration of their disease and its treatment. Moreover, comparison studies are needed with patients treated via nonsurgical means, such as percutaneous or endoscopic balloon dilatation and stenting of an existing biliary stricture. Based on the data of this study, patients surgically repaired after LC compare favorably with age- and sex-matched patients who underwent uncomplicated LC and healthy controls in all domains with the exception of the psychological domain, which was significantly worse for the bile duct injury patients. Substantial differences in the QOL assessment in all domains were observed for patients who pursued legal remedies as a result of their injury.
Acknowledgments
The authors thank the surgical house staff and the surgical nurses of the Johns Hopkins Hospital for their skill and devotion; the institution’s interventional radiologists for their expertise and technical abilities; and Rebecca Baumbusch for assistance in preparing the manuscript.
Discussion
Dr. Selwyn M. Vickers (Birmingham, AL): I want to commend the authors, who have helped us understand how to take care of these difficult patients. You first showed us in your first paper that repair of these injuries and the operation can be done safely and that in fact there was a significant benefit with your technique over a 5-year period. And now you have taken the next appropriate step, to ask the question, is there a perceived benefit by the patients who receive this repair? I have three simple questions that hopefully you can address. Number one, many people use the SF-36 as a quality of life score, particularly in benign diseases. How did you select the quality of life score, and is it valid in a nonmalignant disease population? Number two, it is obvious that you have had a large number of patients to repair, and it is hard to control who responds in a series when you send out questionnaires. You received 54 responders out of your 89. Was there anything identified about the nonresponders in their management that would predict that they had a worse quality of life, even though you didn’t get their report? And third, I have a few repairs to perform at home that were recently referred to me, and as I sit down and talk to my patients—and as you know, I perform these repairs similar to you—one of the questions I have a hard time telling my patients is when their stents will be removed. So what criteria do you use now to remove your biliary stents? Finally, can you correlate early removal of your stents to an increased quality of life score, suggesting that a patient having a longer stent placement or in fact if they require multiple dilatations have lower quality of life scores?
Dr. Gene Branum (Harrisonburg, VA): Drs. Melton, Lillemoe, Cameron, and Yeo have brought to our attention several salient points about the quality of life after lap-chole injury. The manuscript is excellent, and I commend it to you when it becomes available. Some survey studies have shown that the most important way to prevent lawsuits is to communicate effectively with our patients. It would be interesting to interview those suing patients to see why. Excellent surgeons at Hopkins and Duke and Emory and Wash. U. and San Francisco can repair these lesions with excellent long-term results. May it never be said by a patient who sues his surgeon that he or she did so because of what he or she heard from a medical student, referral surgeon, or nursing staff implicitly or explicitly encouraging them to do so. My questions are relatively simple as well. Do you as a service give specific instructions to house staff, nursing staff, ancillary personnel to be circumspect in their conversations in patients with potentially litigious issues such as these? Second, might there not be subtle differences in management, such as early versus late recognition of the injury, socioeconomic status, or overall postinjury course, as a reason for later suit? I really applaud your spectacular results in these patients and look forward to seeing more work from you in the future.
Dr. Leonard T. Furlow, jr. (Gainesville, FL): If you break the suing patients down into those whose suits are still underway, those who lost and those who won, is there any difference in the outcome in those patients? In other words, was the greenback poultice curative?
Dr. Timothy C. Fabian (Memphis, TN): This is an excellent study. I compliment the authors. Associated with the quality of life survey, were you concerned in any way that simply by asking the question if there was a lawsuit that you could have provoked malpractice litigation?
Dr. Greg Timberlake (Jackson, MS): I also enjoyed this presentation tremendously. And I wonder about your conclusion that lawsuits made people feel worse. Is it not more possible that the people who did not psychologically feel well after their surgical repair were the ones who developed lawsuits? Can you tell us any more about their demographics? Was there any difference in socioeconomic status? Is there a difference in level of education? Are there other criteria that might have separated out this group that was more prone to file lawsuits?
Dr. Frederick L. Greene (Charlotte, NC): I just have a quick question. Did return to meaningful employment play any role in the outcome of the quality of life assessment or the institution of a legal action?
Dr. Louis G. Britt (Memphis, TN): Would you also tell me how long you keep drains in and why you keep them in how long you keep them in?
Dr. Keith D. Lillemoe (Baltimore, MD): I would like to thank the discussants for their kind comments and insightful questions. First, for Dr. Vickers’ question. We chose the City of Hope questionnaire recognizing that it was primarily designed for cancer patients because of familiarity with that at our institution, having used it and presented a paper at this Society on quality of life in patients after pancreatic resection. It has also been used by other institutions for benign diseases. We looked through the questionnaire very carefully; there is no reference to any real cancer-specific problems, and I think it is simple and easy for patients to use. Dr. Vickers also asked the important question concerning those individuals who did not respond and how might their results have affected our analysis. Obviously, as we learned at our business meeting, not everybody gets a high percentage response from such questionnaires. Our response rate of 61% was actually better than we see in a lot of similar surveys, and interestingly, the bile duct injury patients responded at a higher percentage than did the lap-chole patients or healthy volunteers who were hospital employees. Why those who didn’t respond did not respond is unclear. We have done statistical analysis comparing those who responded and who did not and there were no obvious characteristics with respect to their outcomes or their clinical characteristics. Furthermore, all the patients who were sent the survey had been classified previously as having a successful clinical outcome. Perhaps they may still be unhappy with their situation, or perhaps maybe their lawyers urged them not to respond, I don’t know.
Both Dr. Vickers and President Britt asked about the somewhat controversial topic with respect to the role and length of postoperative stenting. Historically at our institution we have stented patients for up to a year. Gradually, over the last decade of repairing patients following lap-chole injury, we have found that some injuries, based on their clinical characteristics, their location, their presentation, prior repair, are amenable to earlier stent removal, and therefore, as you can see from the data, there is a fairly wide range of time for stent removal. Currently we use those factors that I just enumerated, plus supporting objective data based on biliary manometric flow studies across the anastomosis conducted by our interventional radiologist and clinical trials where the stents are actually left above the level of the anastomosis for a period to see if there are any symptoms.
I would like to reiterate that all stents had been removed before the survey and, again, that the length of stenting did not influence outcome. Granted, had we asked the questions when the stents were in place their quality of life may very well have been somewhat upset.
The questions brought up by Dr. Branum are very important. I think it is very key that people at tertiary referral centers treat these patients and the referring physicians with the utmost respect and dignity, that comments made even out in the hall through a open door can sometimes be heard by patients. We do talk to our residents concerning their interactions and comments with these patients. In fact, as the RRC has stressed the role of teaching ethics, we conduct sessions with residents on how to manage patients with complications occurring both at our own hospital and outside hospitals. I really hope that in no way has our institution’s treatment contributed to the patient’s decision to sue.
Dr. Branum and Dr. Timberlake asked about subtle differences in clinical outcomes. We are not able by the characteristics we had available to make a distinction. The questions about return to employment and socioeconomic status are excellent questions, and certainly in retrospect we wish we could have asked those. The question of the timing of the questionnaire and the survey with respect to the status of the lawsuit is unknown. We did not ask the patients whether they had won the lawsuit, whether they lost the lawsuit, or whether it was still in progress because we did not want to promote lawsuits by this survey. If you look at the median follow-up for these patients, it is actually in excess of the statute of limitations of lawsuits in most states. So hopefully we did not precipitate any problems for any of the referring surgeons.
Just to close with Dr. Timberlake’s question and the point he made about our conclusions, we do not feel we can answer the chicken-and-egg question—that is, did the presence of a lawsuit lead to worse quality of life or is their worse quality of life leading to a lawsuit? Although our survey does not answer that question, and I am not sure there is any way we could have; it is clearly the question that remains.
Footnotes
Correspondence: Keith D. Lillemoe, MD, The Johns Hopkins Hospital, 600 North Wolfe Street, Blalock 679, Baltimore, MD 21287.
E-mail: klillemo@jhmi.edu
Presented at the 113th Annual Meeting of the Southern Surgical Association, December 3–5, 2001, The Homestead, Hot Springs, Virginia.
A portion of this work was presented at the American College of Surgeons Surgical Forum, October 7–11, 2001, in New Orleans, Louisiana, and has been published in abstract form (Surg Forum 2001).
Accepted for publication December 2001.
References
- 1.Roslyn JJ, Pinns GS, Hughes GS, et al. Open cholecystectomy: a contemporary analysis of 42,474 patients. Ann Surg 1993; 218: 129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995; 180: 101–125. [PubMed] [Google Scholar]
- 3.Wherry DC, Marohn MR, Malanoski MP, et al. An external audit of laparoscopic cholecystectomy in the steady state performed in medical treatment facilities of the Department of Defense. Ann Surg 1996; 224: 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Windsor JA, Pong J. Laparoscopic biliary injury: more than a learning curve problem. Aust NZ Surg 1998; 68: 186–189. [DOI] [PubMed] [Google Scholar]
- 5.Adamsen S, Hansen OH, Funch-Jensen P, et al. Bile duct injury during laparoscopic cholecystectomy: a prospective nationwide series. J Am Coll Surg 1997; 184: 571. [PubMed] [Google Scholar]
- 6.Fletcher DR, Hobbs MST, Tan P, et al. Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography. A population-based study. Ann Surg 1999; 229: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Savader SJ, Lillemoe KD, Prescott CA, et al. Laparoscopic cholecystectomy bile duct injuries: a health and financial disaster. Ann Surg 1997; 225: 268–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19–22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
- 9.Velanovich V. Using quality of life instruments to assess surgical outcomes. Surgery 1999; 126: 1–4. [DOI] [PubMed] [Google Scholar]
- 10.Davidoff AM, Pappas TN, Murray EA, et al. Mechanisms of major biliary complications after laparoscopic cholecystectomy. Ann Surg 1992; 215: 196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Branum G, Schmitt C, Baillie J, et al. Management of major biliary complications after laparoscopic cholecystectomy. Ann Surg 1993; 217: 532–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ress AM, Sarr MG, Nagorney DM, et al. Spectrum and management of major complications of laparoscopic cholecystectomy. Am J Surg 1993; 165: 655–662. [DOI] [PubMed] [Google Scholar]
- 13.Woods MS, Taverso LW, Kozarek RA, et al. Characteristics of biliary tract complications during laparoscopic cholecystectomy; a multi-institutional study. Am J Surg 1994; 167: 27–34. [DOI] [PubMed] [Google Scholar]
- 14.Bergman JJGHM, van den Brink GR, Rauws EAJ, et al. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut 1996; 38: 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lillemoe KD, Martin SA, Cameron JL, et al. Major bile duct injuries during laparoscopic cholecystectomy. Ann Surg 1997; 225: 459–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lillemoe KD, Melton GB, Cameron JL, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg 2000; 232: 430–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrell BR, Wisdom C, Wenzl C. Quality of life as an outcome variable in the management of cancer pain. Cancer 1989; 63: 2321–2327. [DOI] [PubMed] [Google Scholar]
- 18.Savader SJ, Cameron JL, Lillemoe KD, et al. The biliary manometric perfusion test and clinical trial: long-term predictive value of success after treatment of bile duct strictures: 10-year experience. J Vasc Intervent Radiol 1998; 9: 976–985. [DOI] [PubMed] [Google Scholar]
- 19.Pitt HA, Kaufman SL, Coleman J, et al. Benign postoperative biliary strictures: operate or dilate? Ann Surg 1989; 210: 417–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Padilla G, Present C, Grant M, et al. Quality of life index for patients with cancer. Research Nurs Health 1983; 6: 117–126. [DOI] [PubMed] [Google Scholar]
- 21.Present C, Klahr C, Hogan L. Evaluating quality of life in oncology patients: pilot observations. Oncol Nurs Forum 1981; 8: 26–30. [PubMed] [Google Scholar]
- 22.Huang JL, Yeo CJ, Sohn TA, et al. Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg 2000; 231: 890–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rukholm E, McGirr M, Potts J. Measuring quality of life in cardiac rehabilitation clients. Int J Nurs Stud 1998; 35: 210–216. [DOI] [PubMed] [Google Scholar]
- 24.Padilla GV, Grant MM. Quality of life as a cancer nursing outcome variable. ANS Adv Nurs Sci 1985; 8: 45–60. [DOI] [PubMed] [Google Scholar]
- 25.Ferrell BR, Hassey Dow K, Grant M. Measurement of the quality of life in cancer survivors. Quality Life Res 1992; 1: 375–384. [DOI] [PubMed] [Google Scholar]
- 26.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. JAMA 1995; 273: 59–65. [PubMed] [Google Scholar]
- 27.Guyatt GH, Naylor CD, Juniper E, et al. Users’ guides to the medical literature: XII. How to use articles about health-related quality of life. JAMA 1997; 277: 1232–1237. [DOI] [PubMed] [Google Scholar]
- 28.Testa MA, Simonson DC. Assessment of quality of life outcomes. N Engl J Med 1996; 334: 835–840. [DOI] [PubMed] [Google Scholar]
- 29.Kelley JE, Burrus RG, Burns RP, et al. Safety, efficacy, cost, and morbidity of laparoscopic versus open cholecystectomy: a prospective analysis of 228 consecutive patients. Am Surg 1993; 59: 23–27. [PubMed] [Google Scholar]
- 30.McIntyre RC Jr, Zoeter MA, Weil KC, et al. A comparison of outcome and cost of open vs. laparoscopic cholecystectomy. J Laparoendosc Surg 1992; 2: 143–148. [DOI] [PubMed] [Google Scholar]
- 31.Kriwanek S, Armbruster C, Beckerhinn P, et al. Patients’ assessment and recall of surgical information after laparoscopic cholecystectomy. Dig Surg 1998; 15: 669–673. [DOI] [PubMed] [Google Scholar]
- 32.Boerma D, Rauws EAJ, Keulemans YLA, et al. Impaired quality of life 5 years after bile duct injury during the laparoscopic cholecystectomy: A prospective analysis. Ann Surg 2001; 234: 750–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leuenberger K, Ellison EC, Melvin WS, et al. Effect of bile duct injury during cholecystectomy on quality of life. Gastroenterology 1998; 114: A1405. [Google Scholar]
- 34.Carroll BJ, Birth M, Phillips EH. Common Bile duct injuries during laparoscopic cholecystectomy that result in litigation. Surg Endosc 1998; 12: 310–313. [DOI] [PubMed] [Google Scholar]
- 35.Kern KA. Malpractice litigation involving laparoscopic cholecystectomy. Cost, cause, and consequences. Arch Surg 1997; 132: 392–397. [DOI] [PubMed] [Google Scholar]