Abstract
Objective
To compare the function, complications, and quality of life after ileal pouch-anal anastomosis (IPAA) for patients with indeterminate colitis (IndC) and ulcerative colitis (UC).
Summary Background Data
Reports on the outcome of IPAA for IndC have been inconclusive because of the small numbers available for analysis. Concerns about functional outcome, infectious perineal complications, pouch loss and the development of Crohn’s disease remain, while there is no data on the quality of life after IPAA for IndC.
Methods
One thousand nine hundred and eleven patients undergoing IPAA for Ind and UC from 1983 to 1999 were evaluated. IndC was confirmed by repeat pathologic evaluation in 115 patients. Functional outcome and quality of life were assessed prospectively for all office visits (IndC = 230; UC = 5388) using previously reported systems. Complications were evaluated retrospectively.
Results
Functional results and the incidence of anastomotic complications and major pouch fistulae were the same in UC and IndC patients. Although IndC patients were more likely to develop minor perineal fistulae, pelvic abscess, and Crohn’s disease, the rate of pouch failure was 3.4%, identical to that of UC patients. There was no clinically significant difference in quality of life, or satisfaction with IPAA surgery. Patients were equally happy to recommend surgery to IndC or UC patients, but 3% fewer IndC would undergo the same surgery again for their disease.
Conclusions
While functional outcome, quality of life, and pouch survival rates are equivalent after IPAA for IndC and UC, there is an increase in some complications and the late diagnosis of Crohn’s disease. Over 93% of IndC patients would undergo the same procedure again, and 98% would recommend IPAA to others with IndC. Patients with IndC should not be precluded from having IPAA surgery.
In approximately 10% of cases of colitis, there are inadequate diagnostic criteria to make a definite distinction between Crohn’s disease and ulcerative colitis. 1,2 These patients are labeled as having indeterminate colitis (IndC). 3–6 The diagnosis is classically made in patients whose histologic features are diagnostic of neither ulcerative colitis (UC) nor Crohn’s disease; those who have presented with fulminant colitis and have inflammation too severe to further classify their pathology, or those with clinical features suggestive of Crohn’s disease but histology suggestive of UC.
As long as the patient’s symptoms are controlled by medical means, IndC is managed identically to UC, and restorative proctocolectomy is reserved for those with persistently symptomatic disease, or for those with the complications of colitis or its treatment. 7–9 Once a colectomy is required, the distinction between indeterminate and ulcerative colitis becomes more important. Proctocolectomy and ileal pouch-anal anastomosis (IPAA) has become the gold standard operation for those with UC, but there are concerns about long-term outcome after IPAA for IndC. 10 Several studies have addressed this issue 2,11,12 and have raised questions about increased rates of perineal complications and pouch loss. However, the relatively small number of patients available for analysis has not allowed a clear recommendation to be made.
Several major clinical concerns remain regarding IPAA for IndC, including long-term functional outcome, the incidence of perineal complications, the rate of IPAA loss, and the incidence of late-onset diagnosis of Crohn’s disease. Yu et al. recently published a long-term follow-up on 81 patients with IndC, the largest series published to date. They demonstrated a 15% conversion to Crohn’s disease in IndC patients, with a coincident increased rate of pelvic sepsis, pouch fistula, and pouch failure at 10 years, 13 although they did find that IndC patients who did not convert to Crohn’s disease had a clinical outcome like UC patients.
Our experience with IndC has not been so negative, and patients with UC, IndC, Crohn’s disease, and familial polyposis have been found to have similar functional outcome and quality of life. 8 Thus, once the absence of clinical manifestations of Crohn’s disease has been confirmed, our philosophy has been to approach IPAA for IndC patients quite positively, accepting that if the pouch is ultimately lost these patients have at least avoided an ileostomy for several more years.
To determine whether pouch surgery is appropriate for patients with IndC, we evaluated the current experience with IPAA for patients with IndC at this institution. Colectomy specimens were reexamined to standardize the diagnosis of IndC. Functional outcome and complication rates were determined and compared with patients who underwent IPAA for UC. Quality of life and satisfaction with surgery are also presented, to determine the satisfaction of patients who underwent IPAA for IndC, as this has never been critically evaluated for patients with IndC.
PATIENTS AND METHODS
Patient Cohorts
Between 1983 and 1999, 1,911 patients underwent the IPAA procedure for all indications and had at least 6 months of postoperative follow-up. While IndC was permitted as an indication for surgery, patients with any question of Crohn’s disease, specifically patients with evidence of suspicious perineal disease or those with a history of perineal sepsis or fistula, were not accepted as candidates for pouch surgery. Of the 1,911 patients, 171 had a postoperative pathologic diagnosis recorded as IndC, while 1,399 had a diagnosis of UC. Records for the 171 patients were evaluated. Postoperative diagnoses of IndC were based on gross assessment and permanent hematoxylin-eosin sections in all cases, reviewed by dedicated gastrointestinal pathologists. Frozen section analysis at the time of colectomy is not been performed at this institution due to potential diagnostic uncertainties.
Pathologic Re-evaluation
Specimens were re-evaluated by a gastrointestinal pathologist with a special interest in inflammatory bowel disease (Terry Gramlich, MD) to confirm the pathologic diagnosis of IndC, using a system currently in use at this institution and based on a previously described report from this institution. 14 Briefly, specimens were reported as UC unless the following criteria were met:
• The presence of nonnecrotizing granuloma or transmural lymphoid aggregates outside an area of deep ulceration, particularly in the presence of segmental inflammation diagnosed as Crohn’s disease.
• Colitis that had features suggestive of UC but evidence of deep ulcers, transmural lymphoid aggregates, skip lesions, terminal ileal inflammation (less than 30cm), and/or a cecal patch of inflammation that were classified as IndC favoring UC.
• Colitis with a segmental distribution or rectal sparing not related to topical therapy but without granuloma/transmural lymphoid aggregates, classified as IndC favoring Crohn’s disease.
• Indeterminate colitis that could not be placed in any of the above categories was classified as “true” IndC.
• For the purpose of this study, patients with IndC favoring Crohn’s disease, “true” IndC and IndC favoring UC were grouped together and compared to UC patients.
Functional Outcome and Complications
Functional outcome, pouch salvage rates and quality of life parameters were obtained for all follow-up visits for IndC patients, and also for the whole cohort of 1,399 UC patients, using a previously described follow-up system with prospective data collection. 9 Briefly, patients were required to complete a self-administered, structured questionnaire at each return visit to the office. If the patient did not attend for over 1 year, the information was obtained by means of the same questionnaire delivered by mail.
Patients completed questions on the number of bowel motions during daytime and at night. They were asked whether urgency (inability to defer stool more than 30 minutes) or incontinence occurred never, rarely, sometimes, mostly, or always. They were asked about stool consistency, pad usage, the presence of fecal seepage. Patients were also asked whether they experienced any dietary, work, social, or sexual restrictions.
Complication data were not available on the database and a chart review was performed for the 140 IndC patients, and also for 231 UC patients matched for age, sex, method of anastomosis, presence of defunctioning stoma, and time between surgery and most recent follow-up.
Quality of Life (QOL) and Satisfaction With Surgery.
Quality of life was assessed using the Cleveland Global Quality of Life (CGQL) score, as described and validated recently. 9 This scale determines global quality of life on a serial basis after IPAA. Patients were asked to score three items: current quality of life and health, and current level of energy. Each was graded on a scale of 0 to 10 where 0 was worst and 10 was the best possible score. The final CGQL score was then calculated by dividing the total by 30.
Overall happiness with surgery was graded by the patients from 1 to 10, with 10 representing complete satisfaction with the procedure. Patients were also asked at each office visit whether they would undergo the same operation again if it was needed, and whether they would recommend the operation to someone else with the same diagnosis.
Statistical Analysis
Data for functional outcome and QOL are presented as mean and standard deviation or median and interquartile range (IQR) as appropriate for all variables. The number of office visits, mean length of follow-up, and range of follow-up are also shown. Analysis was performed using the Mann-Whitney Rank Sum test, ANOVA, and the χ-square test as appropriate, using StatView for Windows version 5.0.1 (SAS Institute Inc., Cary, NC).
RESULTS
Pathologic examination for those with available specimens confirmed IndC in 140 patients. Complete follow-up data were available for 115 of these patients (82%), and these formed the IndC study group thereafter. The remaining 18% were comprised of some early patients in the series when data had not been as accurately collected, as well as international and out of state patients who had not attended this institution for long term follow-up after their initial surgical visit, and were attending their own local facilities. The mean time to the follow-up visits were 3.4 ± 3.0 years for IndC, and 5.5 ± 3.4 years for UC patients (P < .001).
Functional Outcome
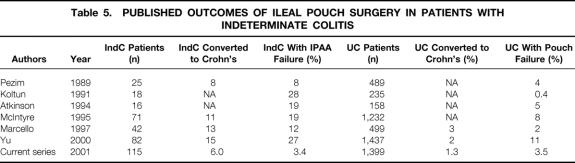
Functional outcome was assessed for all outpatient events, including office visits, and in some cases for questionnaires returned by mail. A total of 230 events for IndC patients was compared to 5374 UC events (Table 1). There was no difference in the time to most recent follow-up event between groups. This ranged from 6 months to 11.1 years for IndC patients, and 6 months to 16.1 years for UC patients.
Table 1. DEMOGRAPHIC, OPERATIVE, AND FOLLOW-UP DATA
*p < .001, Mann-Whitney rank-sum test vs. IndC.
†p < .02, chi-square test vs. IndC.
Median total stool frequency was 7.0 in both groups. Further analysis showed that daytime frequencies were similar in both groups, but there was a doubling in nighttime stool frequency in IndC patients (P < .02). There was no significant difference in incontinence rates between groups. Nighttime seepage was significantly more frequent in UC patients, although no reason was apparent for this change.
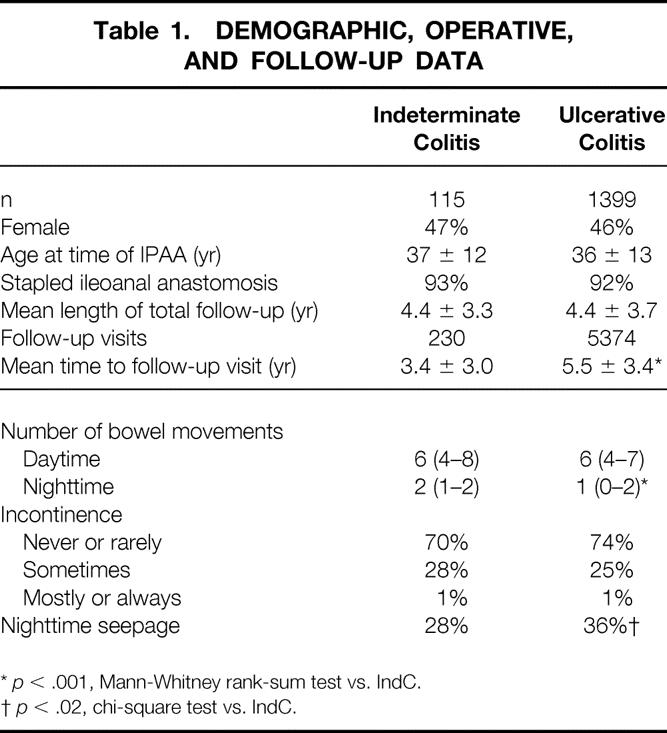
Quality of Life and Satisfaction With Surgery
These results were also compared for all follow-up events for both groups (Table 2). There was no significant difference in median quality of life or health, or level of energy between groups. The calculated CGQL score was slightly but significantly higher for UC patients. IndC and UC patients scored a median of 10/10 for their overall satisfaction with surgery and the outcome of surgery. Approximately 13% of both groups experienced social restrictions related to their surgery or disease process.
Table 2. QUALITY OF LIFE DATA
*p < .001, ANOVA.
†p < .05, chi-square test.
When asked whether they would be happy to undergo their surgery again knowing their ultimate clinical outcome, there was a slight but significant reduction in happiness to 93% in IndC patients. Approximately 98% of both groups would be happy to recommend this type of surgery to other patients with the same diagnosis.
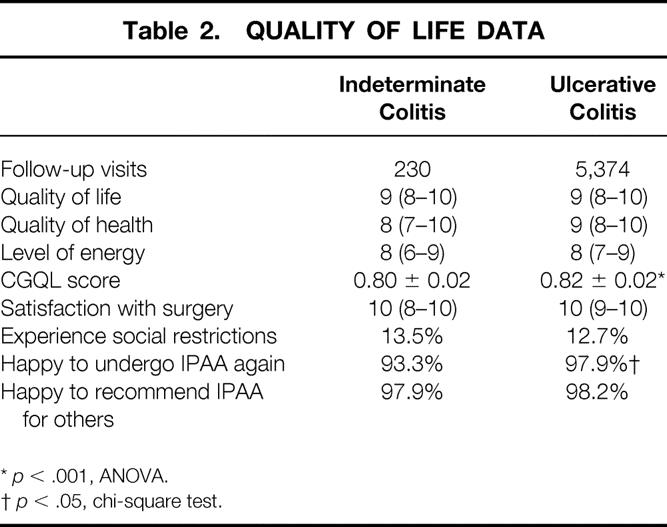
Complications After IPAA
Complications were compared for the 115 IndC patients with 231 matched patients after IPAA for UC (Table 3). There was no difference in anastomotic leak rate, whether detected as a clinical anastomotic dehiscence or a minor sinus from the anastomosis on a routine postoperative contrast enema study. There was a trend to increased fistula formation, with an increased incidence of fistula-in-ano, but not of major fistulae (defined as pouch-vaginal, pouch-vesical, or entero-cutaneous). The incidence of pelvic abscess was also higher in IndC patients.
Table 3. COMPLICATIONS
* Indeterminate colitis: 2 pouch-vaginal, 1 pouch-vesical, 1 pouch-cutaneous; ulcerative colitis: 3 pouch-vaginal, 1 ileostomy closure site. A gastric fistula in an ulcerative colitis patient, secondary to a feeding tube, was not counted in the statistical analysis as it was not pouch-related.
†p < .05, chi-square test vs. IndC.
§p < .01, chi-square test vs. IndC.
Incidence of Crohn’s Disease and Pouch Failure Rates
There was an increased incidence of conversion to a diagnosis of Crohn’s disease in IndC patients, whether defined as definite Crohn’s (histologically proven) or clinical Crohn’s disease (intestinal stricture or pouchitis suggestive of Crohn’s disease, or an antibody profile suggestive of Crohn’s disease) (Table 4). Similarly, although there were more patients with complex peri-anal fistulae in the IndC group, this did not reach statistical significance.
Table 4. INCIDENCE OF CROHN’S DISEASE AND RATE OF POUCH LOSS
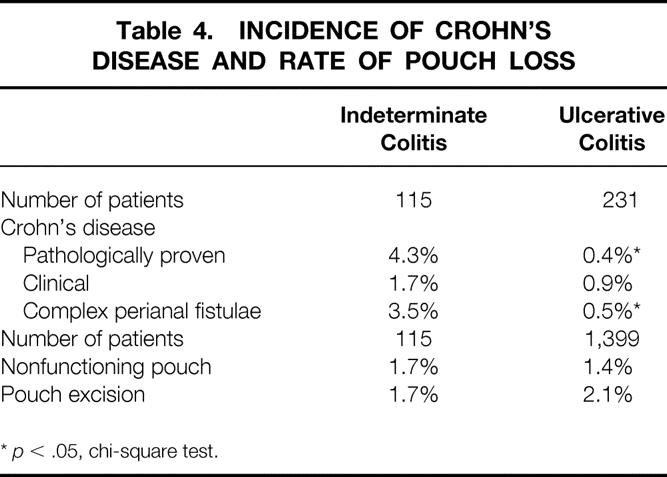
*p < .05, chi-square test.
The most important variable after patient happiness and quality of life score was thought to be pouch survival. This was evaluated for the 115 IndC patients and compared to the 1,399 patients who had undergone IPAA for UC. A nonfunctioning pouch (described as an IPAA present in situ, but disabled with a proximal diverting loop ileostomy for pouch-related problems) was present in 1.7% of IndC patients and 1.4% of UC patients. The ileo-anal pouch was excised at laparotomy in 1.7% of IndC patients and 2.0% of UC patients. Pouch failure occurred in four IndC patients: two patients have a defunctioning ileostomy (one for sepsis after pouch-cutaneous fistula, one for pelvic abscess), and two have had their pouches excised (one for pouch-vesical fistula, one for perianal fistulous disease). Thus, there was no significant difference in the overall rate of IPAA failure; 3.4% in IndC patients and 3.5% in UC patients.
DISCUSSION
Concerns about a poor outcome after restorative proctocolectomy in patients with Crohn’s disease have lead to similar justifiable concerns about the result of IPAA in patients with IndC. Studies of patients who have undergone IPAA and subsequently been shown to have Crohn’s disease suggest that as many as 30% to 45% of patients may ultimately develop pouch failure, manifested by pouch excision or permanent proximal diversion. 15,16
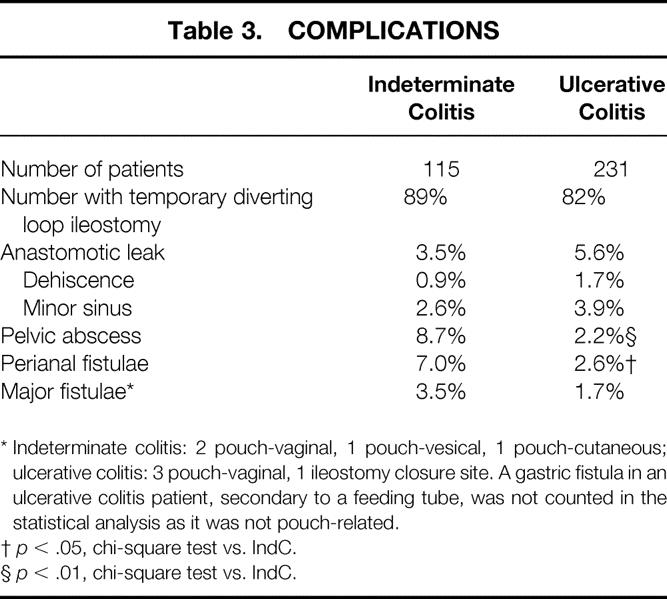
The situation for patients with IndC is less clear. Studies that have evaluated the long-term outcome of IPAA for IndC suggest that when the diagnosis is made with care, these patients have a low incidence of converting to Crohn’s disease over the long-term. 17 However, once an IPAA has been performed, the potential for complications is much greater. Several studies have evaluated the outcome of IPAA in IndC, but the numbers evaluated have been relatively small. Only three studies have evaluated large numbers of patients (Table 5). Marcello et al. studied 42 patients with IPAA for IndC and concluded that the incidence of perineal complications was greater than that seen in UC patients. 2 McIntyre et al. reviewed 71 patients after IPAA for IndC and compared these to 1,232 patients after IPAA for UC. 11 Their conclusions were that although there was no change in the rate of pelvic sepsis or pouchitis, pouch failure increased from 8% in UC patients to 19% in IndC patients. 11 Most recently, Yu et al. updated these results and evaluated 82 patients with IndC. 13 Based on an overall pouch failure rate of 11% for UC at 10 years, they found that patients with IndC who converted to Crohn’s disease did poorly and had a 27% pouch failure rate. Thus, they suggested that the issue of IPAA for indeterminate colitis remained unanswered.
Table 5. PUBLISHED OUTCOMES OF ILEAL POUCH SURGERY IN PATIENTS WITH INDETERMINATE COLITIS
In this manuscript, we compare the outcomes of patients undergoing IPAA for IndC and UC. Patients with IndC had a slightly lower CGQL score and were 3% less likely to be happy to undergo their surgery again (Table 2). Functional results and quality of life outcome parameters were otherwise similar. There was an increase in complication rates after IPAA surgery for IndC patients, relating to the incidence of pelvic abscess and perineal fistulae. There was also a significant difference in the later incidence of Crohn’s disease. Most importantly, there was no difference in the rate of pouch failure (3.4% for IndC patients, and 3.5% for UC patients) (Table 5).
Based on these results, our current practice is to proceed with IPAA in patients with IndC, as long as there are no clinical manifestations suggestive of Crohn’s disease (such as perianal fistulous disease). At surgery there must be no other findings suggestive of Crohn’s disease. Patients are counseled about the potential for the development of Crohn’s disease, but can be advised that at the current time, there is no proven increased rate of pouch loss. Furthermore, the quality of life for patients with IndC is similar to that after IPAA for UC, and 93% would be happy to undergo their surgery again, while 98% would recommend it to others. In the unfortunate event of conversion to a diagnosis of Crohn’s disease, there is increasing evidence of patients having prolonged quality of life, and maintaining their continence and ileal pouch for many years in the majority of cases. 15,16,18
One important consideration with these results and recommendations is that, as with previously published manuscripts, 2,11 the pathologic specimens from these patients were obtained at surgical resection. In practice, many patients are diagnosed with IndC by preoperative endoscopic biopsies. Thus, can recommendations based on surgical pathology be translated to all patients with IndC? We would suggest that one could safely apply these recommendations to most cases of IndC for the following reasons. First, almost 42% of these patients had a prior sub-total colectomy for fulminant colitis before the diagnosis of IndC was made, and thus a major colonic segment was available for evaluation before the IPAA surgery. Second, these recommendations have been in practice at this institution since 1983, and only 5 of the IndC patients have converted to pathologically proven Crohn’s disease during the follow-up period.
Two important distinctions between this paper and many of the other publications on IndC are the lower rate of conversion to Crohn’s disease (6% in this paper, in contrast to up to15% in other manuscripts 13), and the lower rate of pouch failure (3.4% in this paper, in contrast to 10% for UC patients and 20% or more for IndC patients in other manuscripts 2,11,13 (Table 5). The low incidence of conversion to Crohn’s disease attests to the care with which IndC patients are screened for clinical features suggestive of Crohn’s disease before undergoing IPAA. Similarly, it attests to the accuracy with which a diagnosis of IndC is made at this institution. The low risk of pouch failure attests to a combination of careful case selection and attention to surgical detail and postoperative follow-up. Low pouch failure and pelvic sepsis rates are also minimized by frequent use of the double-stapled IPAA without routine mucosal proctectomy and hand-sewn anastomosis, as previously described by this unit. 8,9,19
This paper supports the performance of IPAA in patients with IndC who have no clinical manifestations of Crohn’s disease. These patients have an excellent long-term outcome with a low rate of conversion to Crohn’s disease, and without an increased risk of pouch failure. Nevertheless, these cases may benefit from evaluation in specialized institutions capable of dealing with the potentially complex problems that may occur after restorative proctocolectomy.
Acknowledgments
The authors thank Ms. Jane Bast, Ms. Elena Manilich and Ms. Miriam Preen of the Department of Colorectal Surgery for their help with data collection, and Mr. Jeff Hammel of the Department of Biostatistics for his help with statistical advice.
Footnotes
Conor P. Delaney, MCh, PhD, was the 1999-2000 Surgical Traveling Fellow of the Royal College of Surgeons in Ireland.
Correspondence: Victor W. Fazio, MB, MS, FRACS, Department of Colorectal Surgery/A-111, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, Ohio 44195.
E-mail: faziov@ccf.org
Accepted for publication November 29, 2001.
References
- 1.Lockhart-Mummery HE, Morson BC. Crohn’s disease (regional enteritis) of the large intestine and its distribution from ulcerative colitis. Gut 1960; 1: 87–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marcello PW, Schoetz DJ, Roberts PL, et al. Evolutionary changes in the pathologic diagnosis after the ileoanal pouch procedure. Dis Colon Rectum 1997; 40: 263–9. [DOI] [PubMed] [Google Scholar]
- 3.Price AB. Overlap in the spectrum of non-specific inflammatory bowel disease - “colitis indeterminate.” J Clin Pathol 1978; 31: 567–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka M, Riddell RH. The pathological diagnosis and differential diagnosis of Crohn’s disease. Hepatogastroenterology 1990; 37: 18–31. [PubMed] [Google Scholar]
- 5.Lee KS, Medline A, Shockey S. Indeterminate colitis in the spectrum of inflammatory bowel disease. Arch Pathol Lab Med 1979; 103: 173–6. [PubMed] [Google Scholar]
- 6.Clamp SE, Myren J, Bouchier IA, et al. Diagnosis of inflammatory bowel disease: an international multicenter scoring system. BMJ 1982; 284: 91–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sagar PM, Lewis W, Holdsworth PJ, et al. Quality of life after restorative proctocolectomy with a pelvic ileal reservoir compares favorably with that of patients with medically treated colitis. Dis Colon Rectum 1993; 36: 584–92. [DOI] [PubMed] [Google Scholar]
- 8.Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 1995; 222: 120–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazio VW, O’Riordain MG, Lavery IC, et al. Long term function and quality of life after stapled restorative proctocolectomy. Ann Surg 1999; 230: 575–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bodzin JH, Klein SN, Priest SG. Ileoproctostomy if preferred over ileoanal pull-through in patients with indeterminate colitis. Am Surg 1995; 61: 590–3. [PubMed] [Google Scholar]
- 11.McIntyre PB, Pemberton JH, Wolff BG, et al. Indeterminate colitis: long-term outcome in patients after ileal pouch-anal anastomosis. Dis Colon Rectum 1995; 38: 51–4. [DOI] [PubMed] [Google Scholar]
- 12.Atkinson KG, Owen DA, Wankling G. Restorative proctocolectomy and indeterminate colitis. Am J Surg 1994; 167: 516–8. [DOI] [PubMed] [Google Scholar]
- 13.Yu CS, Pemberton JH, Larson D. Ileal pouch-anal anastomosis in patients with indeterminate colitis. Long-term results. Dis Colon Rectum 2000; 43: 1487–96. [DOI] [PubMed] [Google Scholar]
- 14.Petras RE, Oakley JR. Intestinal complications of inflammatory bowel disease: pathological aspects. Semin Colon Rect Surg 1992; 3: 160–72. [Google Scholar]
- 15.Sagar PM, Dozois RR, Wolff BG. Long-term results of ileal pouch-anal anastomosis in patients with Crohn’s disease. Dis Colon Rectum 1996; 39: 893–8. [DOI] [PubMed] [Google Scholar]
- 16.Hyman NH, Fazio VW, Tuckson WB, et al. Consequences of ileal pouch-anal anastomosis for Crohn’s colitis. Dis Colon Rectum 1991; 34: 653–7. [DOI] [PubMed] [Google Scholar]
- 17.Wells AD, McMillan I, Price AB, et al. Natural history of indeterminate colitis. Br J Surg 1991; 78: 179–81. [DOI] [PubMed] [Google Scholar]
- 18.Panis Y, Poupard B, Nemeth J, et al. Ileal pouch/anal anastomosis for Crohn’s disease. Lancet 1996; 347: 854–7. [DOI] [PubMed] [Google Scholar]
- 19.Tuckson WB, Lavery IC, Fazio VW, et al. Manometric and functional comparison of ileal pouch anal anastomosis with and without anal manipulation. Am J Surg 1991; 161: 90–6. [DOI] [PubMed] [Google Scholar]