Abstract
Objective
To compare the amount of National Institutes of Health (NIH) funding provided to departments of surgery with that provided to other major clinical departments, to examine the relationship between peer-review activity and funding success, and to compare trends in participation in the peer-review process between surgeons and representatives from other clinical departments.
Summary Background Data
Surgical research has made enormous contributions to human health. This work is fundamentally dependent on fair and unbiased distribution of extramural research funds from the NIH. To date, no published report has examined the relative distribution of extramural support between departments of surgery and other major clinical departments.
Methods
Data regarding funding trends and peer-review activity were obtained from the NIH and compared between departments of surgery and four nonsurgical departments (medicine, psychiatry, pediatrics, neurology). Award data were examined during 1996 to 2001. Participation trends were examined during 1998 to 2000.
Results
Success rates of surgical proposals were significantly lower than nonsurgical proposals. Differentials in success rates were greatest for proposals assigned to the National Cancer Institute, although relative underfunding for surgical research spanned all major institutes. Awards for surgical grants averaged 5% to 27% less than nonsurgical grants). Surgeons exhibited 35% to 65% less peer-review activity relative to nonsurgeons when normalized to grant submission activity. Overall, surgeons participated on sections where they made up a relatively smaller proportion of total review members compared to nonsurgeons.
Conclusions
Surgical grant proposals are less likely to be funded and carry significantly smaller awards compared to nonsurgical proposals. Relatively fewer surgeons participate in the review process, and those who do are more likely to be in the minority within study sections. Multiple strategies are needed to address these trends and level the playing field for surgical research.
Surgical research has made significant contributions to human health. Many of the contemporary advances in surgical practice have been made possible through research funding from the National Institutes of Health (NIH). Although several studies have characterized the general distribution of extramural research funding among U.S. medical schools, no published report has examined the relative distribution of grant support between departments of surgery and other major clinical departments. 1,2
The relevance of such an investigation is that many diseases such as cancer command a wide range of research efforts from both surgical and nonsurgical disciplines. Research proposals from different clinical departments investigating along similar themes must compete with each other for support by funding bodies such as the National Cancer Institute (NCI). It is the stated mission of the NIH to ensure a fair and adequate distribution of extramural support throughout the biomedical community. Effective participation by surgeons in the peer-review process would seem prudent to promote this mission for the cause of surgical research. To date, participation trends in the NIH peer-review process by surgeons have not been characterized.
The purpose of this study was threefold: to compare the amount of NIH funding provided to departments of surgery with that provided to other major clinical departments, to examine the relationship between peer-review activity and funding success, and to compare trends in participation in the peer-review process between surgeons and representatives from other clinical departments.
METHODS
We obtained success rate and award data for competitive research proposals from the Information for Management, Planning, Analysis and Coordination (IMPAC) database maintained at the NIH. 3 Departments of surgery were previously identified as submitting the fourth largest number of competitive grant proposals among clinical departments at academic medical centers. The four other clinical departments making up the top five (medicine, psychiatry, pediatrics, neurology) were used as comparison groups against surgery, both individually and as a combined nonsurgical group (referred to here as “nonsurgery”).
We examined the overall success rates of competitive grant proposals for fiscal years (FY) 1995 to 2001. Success rates were also examined at individual NIH institutes reviewing the largest percentage of surgical proposals during FY1995 to 2000. Award data (mean grant award amounts) and total extramural support were examined for each clinical department for FY1995 to 2000. Only newly submitted and competitive renewal research project applications were used in this analysis.
We obtained data regarding NIH peer-review participation from the Center for Scientific Review (CSR). 4 The NIH fiscal year is composed of three separate grant review cycles. Many participants in the review process serve multiple terms on the same study section; therefore, an analysis of rosters from fall review cycles were used to estimate annual participation trends. At the time of publication, complete roster datasets were available for the FY1998 to 2000 fall terms. Complete rosters were obtained for all nine review cycles (fall, winter, and spring, FY1998–2000) for the sections primarily dedicated to surgical research (Surgery & Bioengineering [SB] and Surgery, Anesthesia & Trauma [SAT]).
We identified representatives from departments of surgery as any degree holder (e.g., MD, MD/PhD, or PhD) with a primary appointment in the department of surgery or a recognized division thereof (e.g., vascular surgery, gastrointestinal surgery). Award data for surgical subspecialty fields not routinely considered divisions of departments of surgery are archived within NIH databases under their respective departments (e.g., orthopedic surgery). These data were not included in the analysis. Representatives from divisions of the other four clinical departments being examined were included in their respective departments for analysis (e.g., an adult endocrinologist was counted as representing the department of medicine; a pediatric oncologist was counted as representing the department of pediatrics).
In examining participation trends, we sought to determine if participants from each department were effectively serving on sections where proposals from their own specialties were evaluated. However, specific information regarding the distribution of research proposals (among individual study sections) was not available from the NIH. Alternatively, we examined three surrogate variables in an attempt to estimate relative concentrations between departments. These included the annual ratios of study section members to submitted grant proposals, the relative concentrations of members from each department within study sections in which they participated, and the relative number of study sections dominated by members from each clinical department. Analysis of concentration specifically examined the proportion of members from each clinical department to all members within the sections they participated in. Analysis of dominated sections examined whether the number of members from each clinical department was larger than any other single specialty within the sections in which they participated in.
Differences in success rates between groups were analyzed using one-sample t tests. Analysis of variance was used to analyze differences in mean grant award amounts between departments. The potential relationship between funding success and grant submission activity was examined using the Spearman rank-order coefficient. Analysis of variance using linear modeling was used to examine differences in the members to grant ratios between departments. Chi-square analysis was used to examine the relative number of dominated sections between departments. Two-sample Wilcoxon statistics were used to examine differences in the relative concentrations of members serving on study sections from different departments.
RESULTS
Funding Success
The five most active clinical departments at U.S. medical schools, as ranked by the number of NIH grant submissions during FY1995 to 2001, were (annual mean ± SD): medicine (2,385 ± 125), psychiatry (898 ± 68), pediatrics (683 ± 50), surgery (630 ± 44), and neurology (420 ± 35). Mean annual success rates for competitive research proposals during FY1995 to 2001 ranged from 26.6% to 35.4% for medicine (n = 20,155); 27.6% to 32.3% for psychiatry (n = 6,398); 23.1% to 31.1% for pediatrics (n = 4,936); 22.5% to 27.0% for surgery (n = 4,537); and 24.5% to 34.9% for neurology (n = 3,002) (Fig. 1A). Weighted success rates for the combined nonsurgery group ranged from 26.1% to 34.1% (n = 34,491) (see Fig. 1B). Success rates for surgical proposals were significantly lower than each individual nonsurgical department (P = .017 or less vs. each department) as well as the combined nonsurgery group during the 7-year period (range of absolute difference in annual success: 8–36%;P = .0005). No correlation was found between success rates and the number of annually submitted grants (n = 35 rank pairs;r = 0.57).
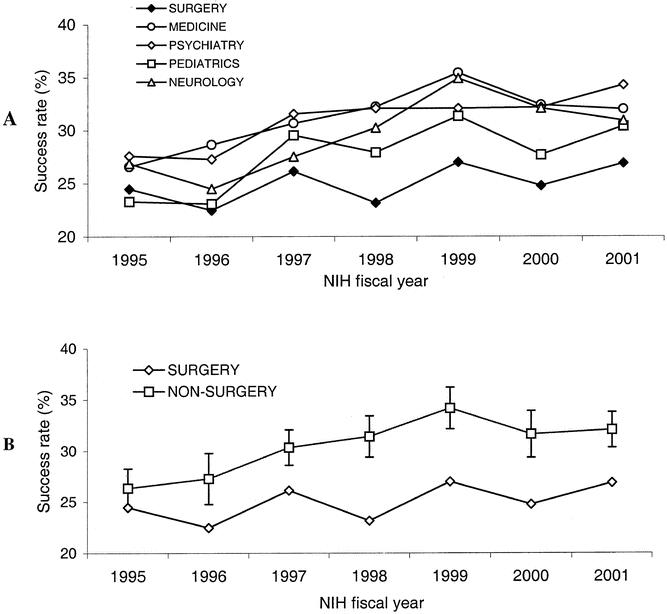
Figure 1. (A) Success rates for competitive research proposals submitted to the NIH by the five most active clinical departments at US medical schools during FY 1995–2001 (P = .017 or less vs. surgery for each nonsurgical department). (B) Success rates for surgical vs. combined nonsurgical clinical departments during the same period (mean ± SD for nonsurgery group, P = .0005 vs. nonsurgery group).
During FY1995 to 1999, six NIH institutes reviewed 84% (2,929) of all grant proposals submitted from departments of surgery: NCI, 23%; National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), 20%; National Heart, Lung and Blood Institute (NHLBI), 16%; National Institute of Neurological Disorders and Stroke (NINDS), 13%; National Institute of General Medical Sciences (NIGMS), 6%; and National Institute of Allergy and Infectious Diseases (NIAID), 6% (Fig. 2A). The remaining 16% of surgical grants were distributed between 11 to 13 additional institutes, depending on fiscal year. Of the 30 annual success rate comparisons made between surgery and nonsurgery at these institutes (six institutes over 5 fiscal years), 90% (27/30) favored nonsurgical proposals. Although success rates for surgical proposals were consistently lower for each of the six institutes examined, statistically significant differences were found only for NCI (P = .005) and NINDS (P = .02) (see Fig. 2B). However, 85% (17/20) of the annual success rate comparisons at institutes where significant differences were not found still favored nonsurgical proposals. Furthermore, collective analysis of success rates across the four individually nonsignificant institutes continued to demonstrate a significant disadvantage for surgical proposals (P = .032).
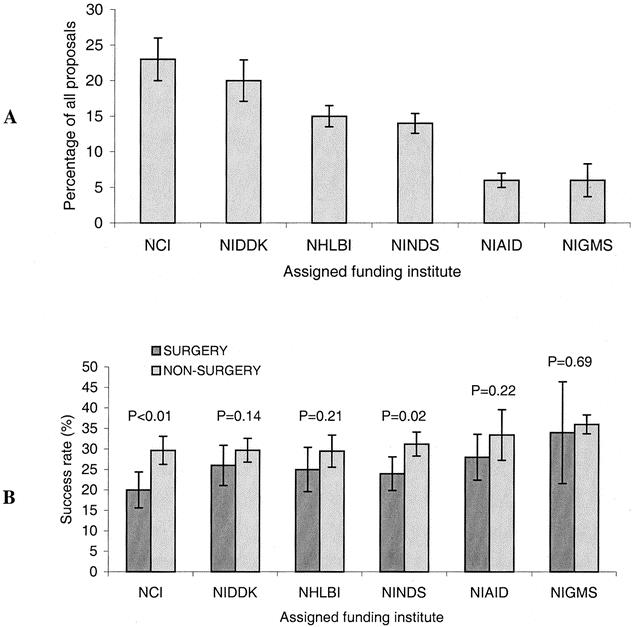
Figure 2. (A) NIH Institutes assigned the largest proportions of surgical grant proposals for potential funding consideration during FY 1995–1999 (mean annual percentage ± SD). (B) Success rates of surgical and nonsurgical grant proposals assigned to these institutes over the same period (mean of annual success rates for 5-year period ± SD).
Award Amounts
Mean award amounts for successfully funded research proposals were consistently lower for surgeons compared to nonsurgeons for each year examined during FY1995 to 2000 (Fig. 3A). Normalization of award data to yearly increases in the NIH budget (relative to FY1995 constant dollars) revealed a significant difference over the 5-year period favoring the nonsurgical group (range of annual differences in mean award amount: 5–27%;P = .0045; n = 1,137 for surgery, n = 10,541 for nonsurgery; see Fig. 3B). Awards from surgical departments were also significantly smaller than those from each individual nonsurgical department, with the exception of pediatrics (P = .07 vs. pediatrics, n = 1,374;P = .03 or less vs. all other departments, n = 892–6,289). There was no difference over time in the relative percentage of the total NIH extramural budget dedicated to surgical and nonsurgical departments (annual mean increase over previous year during 6-year period: surgery 0.6 ± 1.4%, nonsurgery combined 0.9 ± 3.2%, P = .56).
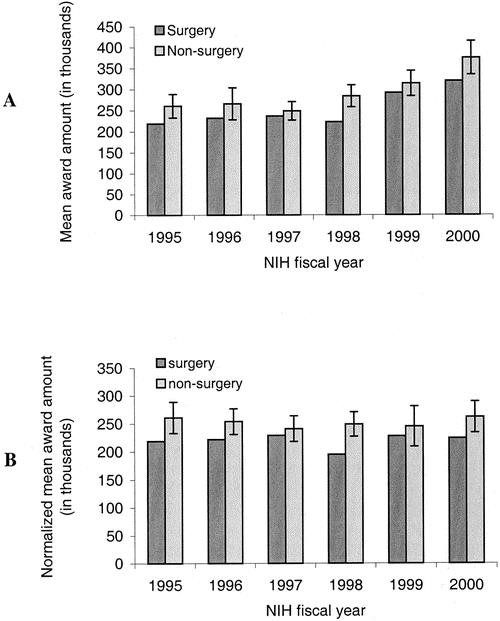
Figure 3. (A) Mean awards for successfully funded proposals from surgical and nonsurgical departments during FY 1995–2000 (mean ± SD for nonsurgery group). (B) Award data after normalization to NIH extramural budget increases during same period (presented in 1995 constant dollars;P = .0045 vs. nonsurgery over 6-year period).
Peer-Review Activity
Analysis of study section rosters during the FY1998 to 2000 fall meeting cycles revealed 2,108 participants within 116 study sections in 1998, 2,490 participants within 129 sections in 1999, and 3,311 participants within 142 sections in 2000. Relative participation in the peer-review process by each department during the 3-year period is presented in Figure 4. Relative increases in participation over the 3-year period (i.e., recruitment) ranged from 46% to 317% for nonsurgical departments and 50% for surgical departments, although this difference was not significant (P = .27).
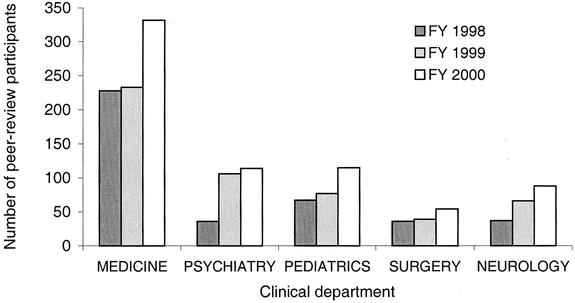
Figure 4. Relative peer-review activity of major clinical departments during FY 1998–2000 fall cycles. There was no difference in the relative increase (recruitment) of participants between surgical and nonsurgical departments during the 3-year period (surgery 50%, nonsurgery 46–317%;P = .27).
The relative ratio of study section members to grant submissions was significantly lower for surgical departments during the 3-year period (annual range for surgery: 0.18–0.23, nonsurgery: 0.24–0.38;P = .015;Fig. 5). This represents 35% to 65% less peer-review activity on behalf of surgeons when normalized to grant submission activity. We found an increasing trend over the 3-year period suggesting nonsurgeons were more likely to dominate the sections they participated in, although this was not significant (annual range of dominated sections: surgery 8.3–15.3%, nonsurgery 17.7–18.3%;P > .26 or greater for each year). Overall, nonsurgeons were concentrated on sections where they made up a relatively greater proportion of all members compared to surgeons for each year examined (FY1998: surgery n = 13, nonsurgery = 120, P = .032; FY1999: surgery 17, nonsurgery n = 163, P = .004; FY2000: surgery n = 24, nonsurgery = 196, P = .002;Fig. 6).
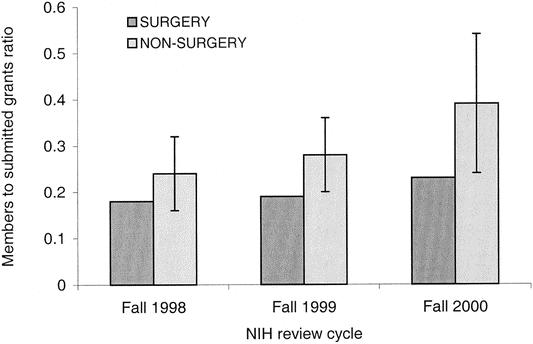
Figure 5. Relative concentration of study section participants to the number of annually submitted grants from surgical and nonsurgical departments (FY 1998–2000 fall cycles). Nonsurgeons exhibited 35 to 65% greater peer-review activity to nonsurgeons when normalized to grant submission activity (P = .015 for the 3-year period; annual mean ratio ± SD for nonsurgery group).
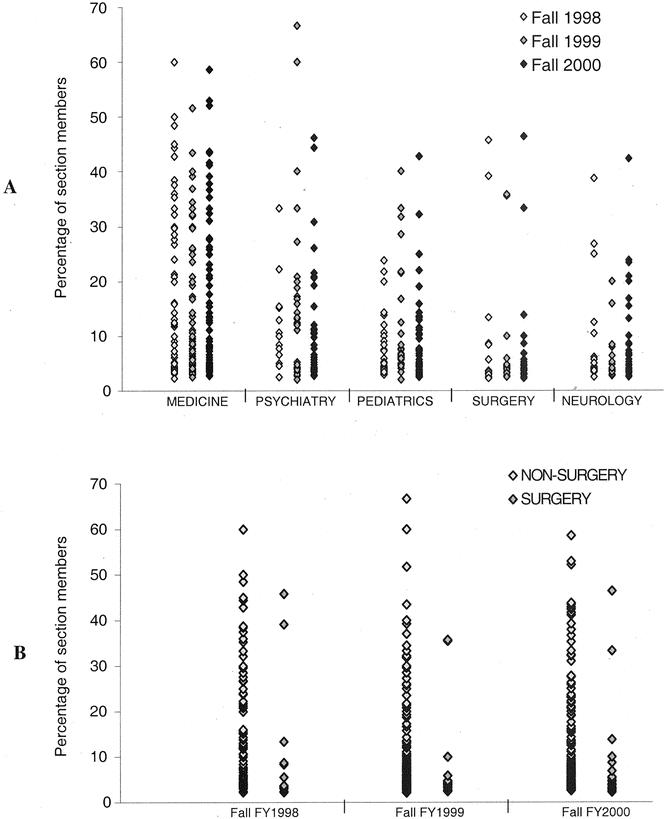
Figure 6. Scatterplot of individual study sections containing members from each clinical department. Each plot represents one section where at least one member from the relavent department was participating. Location of the y-axis represents the percentage of all members in that section. (B) Participants from the nonsurgical group were concentrated on sections with relatively greater proportions than surgeons for each year examined (FY 1998: P = .032; FY 1999: P = .004; FY 2000: P = .002).
The distribution of surgeons participating in the peer-review process during the FY1998 to 2000 fall cycles is presented in Figure 7. Forty-nine percent (64/129) of all surgeons were concentrated in either the SAT or SB study sections during the 3-year period, while the remaining 51% were distributed between 11 and 16 different study sections, depending on fiscal year. Participation of different surgical specialties within the dedicated surgical sections for all nine review cycles is presented in Figure 8. Surgeons (all specialists combined) dominated each of the 18 total study section meetings and made up an average 43% of all members within these sections. Seventy-four percent (70/94) of all surgical positions on SB study sections were held either by a cardiothoracic or vascular surgeon, while 67% (62/93) of surgical positions on SAT study sections were held either by a transplant or trauma surgeon. Of note, the number of total surgery positions held on study sections is different than the absolute number of surgeons over the 3-year period because many participants serve on more than one review cycle.
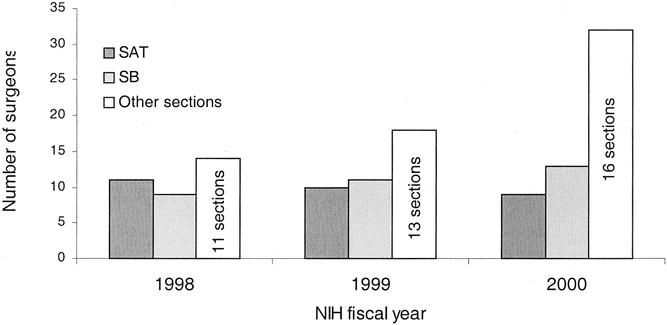
Figure 7. Distribution of surgeons participating in the peer-review process during FY 1998–2000 (data reflect all review cycles – fall, winter, and spring; n = 36 for 1998, n=39 for 1999, and n = 54 for 2000). Forty-nine percent of all surgeons were concentrated in one of two dedicated surgery study sections (Surgery, Anesthesia and Trauma [SAT], or Surgery and Bioengineering [SB]).
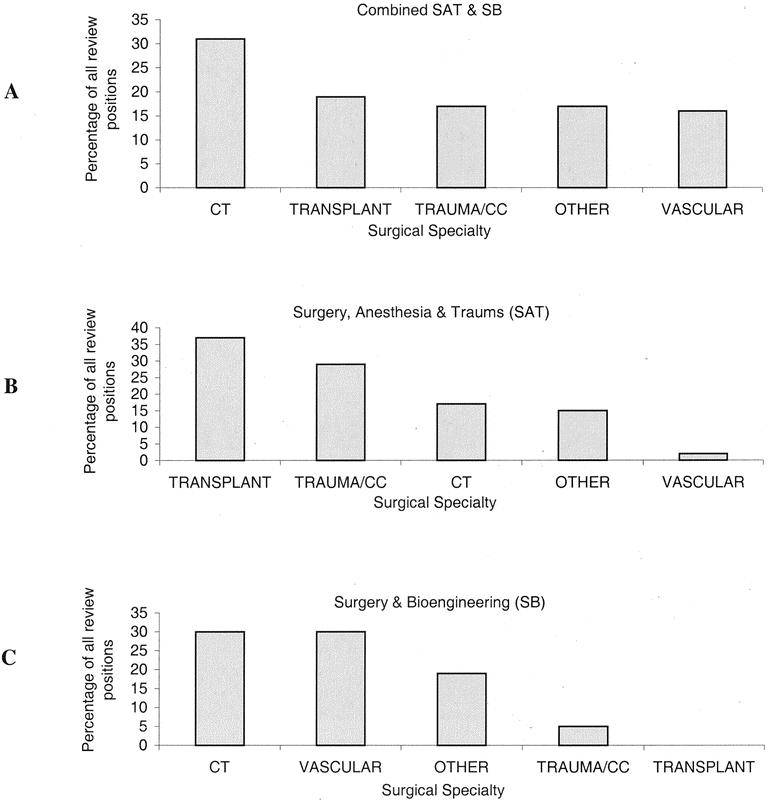
Figure 8. (A–C) Relative peer-review activity of surgical specialties within the two major study sections dedicated to surgical research. Participation data reflects all nine review cycles during FY 1998–2000. A single surgeon may occupy multiple positions if they serve more than one cycle (CC = critical care, CT = cardiothoracic).
DISCUSSION
Is the Playing Field Truly Unlevel?
Over the past decade, the scientific community has witnessed unprecedented growth in biomedical research funding by the NIH. With a budget now exceeding $23 billion for FY2002, the NIH will remain the preeminent source of biomedical research funding for all of academic medicine. 5 Despite this record budget expansion, we found that departments of surgery consistently received less funding support relative to other major clinical departments at academic medical centers. Grants from departments of surgery also carried significantly smaller awards, suggesting an even greater disproportionate allocation of extramural funding than by success rates alone. During FY1995 to 2001, a total of 1,137 competitive research proposals from departments of surgery received funding from the NIH. Success rates equivalent to nonsurgical departments would have predicted an additional 219 (19%) funded proposals during the same period. When taking contemporary award data into account, this deficit would amount to roughly $55 million in lost extramural research support to surgical departments.
The results of our study would suggest that research proposals from departments of surgery are consistently of less quality compared to those from other departments, or that some form of inherent bias exists against surgical research within the peer-review process, or perhaps both. The possibility of internal bias against surgical research cannot be easily dismissed. Recent inquiries originating from within the biomedical community have challenged the NIH’s ability to provide a globally fair and unbiased peer-review process. 6–10 These investigations have identified potential bias resulting in underfunding for many categories of extramural research. These include primarily patient-oriented research, research originating from highly specialized fields, research describing innovative or non-hypothesis-driven methodology, and research from lesser-known institutions and investigators, among others.
It has been proposed that the common denominator of these proposals is their minority status when placed into unfavorable study sections for review. 11–13 Proponents of this view argue that with many focused areas of research, it is often the case that too few members exist within study sections who have an adequate familiarity with the topic of investigation. The influence of “favorable” study section representation on peer-review scoring, either through extensive familiarity with the nature of research outlined in the proposal, or even with its principal investigator, has been well documented in this regard. 7,14,15 Whether such bias ultimately leads to inferior funding success for otherwise sufficiently meritorious proposals remains a very contentious topic. Nevertheless, these observations have led to the global restructuring effort currently taking place within the NIH peer-review process. 16
Whether proposals from departments of surgery similarly fall into minority status has not previously been examined. Although no objective evidence exists to support this, it is commonly held that academic surgeons incur greater clinical responsibilities relative to faculty from nonsurgical departments. Adequate “protected” time for nonclinical endeavors may therefore prove more difficult to secure, potentially resulting in a relative paucity of surgeons participating in the peer-review process. We found indirect evidence to support this in our study, although analysis of dominated sections did not prove statistically significant. Overall, we believe that examining the relative concentrations of review members on study sections may have been the most accurate means of estimating effective participation. This is due to the observation that relatively small numbers of participants from the same department may dominate particularly heterogeneous sections, while at the same time representing a relatively small percentage of all members. The significance of this, with only few exceptions, is that all members within study sections contribute equally to the final priority score.
During the 3-year period examined, the number of surgeons participating in the peer-review process increased by nearly 50%. However, the number of study sections where surgeons participated also increased during that time by nearly 40%. Although this would suggest that surgeons are becoming more actively involved in a broader range of peer-review topics, the net result of this expansion was several newly represented study sections containing only one surgeon each. As study sections frequently contain 25 members or more, one would question the potential influence of a single member in promoting his or her respective area of research.
The relative peer-review activity of different surgical specialties was examined to determine whether bias might exist within departments of surgery. We felt this was a valid line of investigation given that a significant proportion of all surgical proposals may be evaluated within the two surgical study sections, and that these sections were dominated by a relatively heterogeneous group of surgeons. We found an overall disproportionate number of cardiothoracic and transplant surgeons participating on these sections relative to other specialties, and hypothesized that a relative bias might exist against research originating outside these divisions. We further hypothesized that such a bias may translate into relatively improved success rates for surgical proposals assigned to NHLBI and NIAID (given the nature of surgical research reviewed at these institutes). Although the finding that success rates were not significantly different at these institutes may in itself be significant (in the context of the overall trend), success rates were also not statistically different at NIDDK and NIGMS. Furthermore, the relative differentials in success rates between surgical and nonsurgical grants at all six institutes were remarkably similar from year to year. Although interpretation of these data is limited, we feel it is unlikely that internal bias has played a significant role in the overall underfunding of surgical research.
Whether any degree of bias truly exists against surgical research, our data demand that we consider the possibility that research proposals from departments of surgery are consistently of lower quality than those from nonsurgical departments. In the peer review of qualitative merit, the NIH uses a set of five criteria that can be roughly divided into two conceptually different categories: the potential relevance of and to the field of study, and the proposed methodology for carrying out the investigation. 17 With respect to clinical relevance, there is no evidence to suggest that the significant burden of surgical disease on societal health has waned in recent years. In fact, many surgical diseases such as coronary artery disease, traumatic injury, colorectal and breast cancer, among others, continue to rank among the top 10 with respect to overall mortality and years of life lost in the United States. 18 We anticipate that society will continue to place a high priority on supporting scientific advances pertinent to these diseases.
The question of whether fundamental methodological deficits consistently exist within surgical research relative to other clinical fields is somewhat more difficult to address. Attempting to answer this question would entail a comprehensive audit of methodology-derived components of individual priority scores, with comparisons made across departments. Due to the relatively subjective nature of scoring, these results would have to be referenced against an objective, standardized quality assessment instrument that does not exist. Previous attempts at such audits of peer-review forums have been largely unsuccessful. 19 To our knowledge, no study in any context has examined whether quantifiable differences exist between different clinical departments with respect to research quality.
Recent speculation has suggested that surgeons are placed at a relative disadvantage for achieving academic success compared to their nonsurgical peers due to the nature of their training paradigm. This hypothesis is based on the different timelines in which surgeons and nonsurgeons obtain their formal research experience relative to faculty appointments. Physicians from nonsurgical departments often engage in integrated fellowship programs following a period of uninterrupted residency training. Protected time for academic research is incorporated into these clinical fellowships, providing early experience with the grant procurement process and the opportunity to establish their reputation along a focused line of research. As a result, many of these individuals move into their faculty careers with a modest but established track record to facilitate future grant support. Perhaps most importantly, many enter faculty appointments already armed with NIH training grants and other development awards supported by their preceding fellowship work.
In stark contrast, surgeons are encouraged to obtain their research experience early during residency training. After 2 to 3 years of research training in an area that may or may not ultimately reflect their choice of specialty, surgeons engage in 4 to 6 additional years of clinical training before faculty appointment. There are few areas of scientific inquiry that do not change significantly over such a time period. It is therefore highly unlikely that the surgical investigator will be able to seamlessly pursue the same line of work that he or she engaged in years previously. As most surgical fellowships do not integrate a dedicated research component, many newly appointed academic surgeons must invest considerable time simply establishing themselves as new investigators. This occurs at the same time they must also build a practice and establish their clinical reputation.
Studies have indicated that previous NIH support is the best predictor of future funding. 13 Furthermore, lack of preliminary data and lack of recent publications in a proposed field of inquiry are generally viewed as major deficits by the NIH. In the context of these observations, it appears that academic surgeons starting out in their career (and perhaps well into their careers) would be at a definite disadvantage along these lines relative to nonsurgeons. The potential influence of the current surgical training paradigm on the ability to obtain NIH funding support is worthy of further examination.
Limitations of This Investigation
We limited our analysis to competitive research proposals submitted to the NIH. We did not attempt to quantify noncompetitive extramural funding, nor did we examine the degree of support obtained from other federally based entities. Although noncompetitive funding in the way of contracts and other resources may be substantial, this type of support rarely represents more than a very small percentage of total extramural support provided to academic departments. 3 We chose to focus on NIH funding over other federal agencies given its dominant role in supporting biomedical research, providing nearly 83% of all federally mandated healthcare research dollars during FY2000. 20
We also chose to focus on competitive funding from the NIH due to its relative importance for other aspects of academic medicine. Less competitive sources of research funding are available through private industry, philanthropic foundations, academic health centers, and additional government-based agencies, among others. However, none of these carries the same degree of academic prestige as successful negotiation of the rigorous NIH peer-review process. In this regard, the importance of a solid track record in NIH funding for career advancement in the academic setting has been well described. 21 Competitive funding from the NIH also plays a vital role in shaping future academic scientists through a myriad of competitive training grants and fellowship opportunities. 22
Our investigation was also limited in that we examined only the five most active clinical departments, as ranked by research productivity. It would be interesting to characterize the funding trends of smaller clinical departments as well as those oriented primarily along the basic sciences. Analysis of funding trends within the surgical subspecialties would also be particularly interesting given the markedly different academic cultures that exist within these departments (relative to resident teaching, surgical research, and generation of clinical revenue).
Another issue potentially confounding our results surrounds the somewhat arbitrary categorization of research proposals by the NIH. This is particularly true for research originating from departments of urology, plastic surgery, and neurological surgery. Funding data regarding these proposals are most often archived under the category of “other clinical.” However, an unknown number of proposals originating from these departments may have been inadvertently factored into our funding analysis for departments of surgery.
With respect to participation in the peer-review process, our results may suggest but do not prove that surgeons are less active compared to members from other clinical departments. We were unable to obtain information regarding the exact distribution of surgical proposals among study sections and therefore relied on surrogate variables to estimate the relative effectiveness of participation between groups. The assumption that the overwhelming majority of surgical grants are evaluated in the two surgical study sections may not necessarily hold true. Grant review officers at the CSR are responsible for deciding both the Integrated Review Group (IRG) and study section assignments for newly submitted research proposals, and this decision hinges more on the scientific nature and methodology of the proposed investigation rather than the department of origin. This may be particularly true with basic science-oriented proposals. It was with this consideration that we expanded our participation analysis to include all sections where surgeons participated, with the general assumption that at least some amount of surgical research would be evaluated in each of these sections.
A further limitation of this study is that we examined only a cross-section of annual peer-review activity during a relatively short fiscal period. Inability to obtain complete roster sets for earlier years precluded more extensive analysis. We do not know whether similar results would have been obtained if different cycles were analyzed within fiscal years, or if different fiscal periods were examined altogether. However, we found remarkably similar participation patterns from year to year and believe our findings may be a fairly accurate representation of ongoing trends.
Finally, we did not examine the “second” round of peer review that occurs at the level of individual funding institutes. Scientific advisory boards and other advisory counsels function to ensure that the funding practices of institutes are aligned with their stated scientific missions. Such counsels may play a significant role at the institute level in determining which scientific proposals are ultimately funded. It would seem prudent to ensure adequate representation by surgeons on these committees within the relevant institutes, and future investigations should characterize participation trends at this level as well.
What Can We Do to Level the Playing Field?
Our ability to address this question may well affect the future of academic surgery. Several proactive strategies are needed to reverse these trends and increase the level of NIH support to surgical departments. These will include ensuring that research proposals originating from departments of surgery are of the highest methodological quality, that an adequate degree of representation by surgeons exists within the peer-review process, and that the cause of surgical research is effectively promoted within the NIH at the administrative level.
With respect to training, we must continue to do everything possible to educate surgical residents in the process of critical thinking and the use of sound research methods. Although the ability to prepare competent research proposals is essential in the competition for NIH funding, the generation of preliminary data and the ability to demonstrate a recent track record of relevant publications are increasingly important. We must closely examine whether the current training paradigm effectively prepares academic surgeons to compete with their nonsurgical peers in this regard. The American Board of Surgery is currently considering a major restructuring of surgical training. This includes modification of the existing paradigm into a 3- or 4-year core surgical residency followed by subspecialty training. While such changes could have a multitude of impacts beyond the scope of this discussion, they may potentially address some of the relative disadvantages discussed above.
Once a surgeon enters academic practice, the clinical demands on him or her tend to be substantial. Many surgical chairs have observed that surgical faculty cannot be afforded the same degree of protected time available to other academic physicians. 23,24 In the future, innovative financing strategies will be required of surgical departments if their faculty are to receive the necessary protected time to compete with their nonsurgical peers. This should also include effectively addressing the salary caps currently imposed by the NIH on recipients of competitive grant awards. The difference between cap limitations and the salaries of many academic surgeons can be significant, and this may result in relative salary deficits for many surgeons holding extramural support. Unless supplementary sources of income can be identified, there is a relative financial disincentive for surgeons to pursue NIH grants. Today’s department chairs face the daunting task of maintaining the surgical research mission in the face of continued pressure to produce more clinical revenue. The solutions to these unanswered problems must come directly from today’s leaders in surgery.
In an attempt to smooth the transition into academic medicine, the NIH has developed several career development programs designed for the physician-scientist. These include the K08 (Mentored Clinical Scientist Development Award) and K23 development awards (Mentored Patient-Oriented Research Award), among others. These programs provide support to promising young investigators early in their careers before becoming competitive for R01 funding. The number of young surgeons applying for these awards is believed to be quite low and may reflect the relatively heavy commitment of 50% to 75% research effort. 25 However, we believe that leaders in surgery should actively encourage their junior faculty to apply for these awards and provide the necessary infrastructure and financial resources to use these opportunities effectively.
In recognizing the challenges posed to young investigators, many surgical organizations have responded by creating their own career development programs. Some of these fellowships, such as the John Mannik Award for K08 recipients in vascular surgery, are specifically designed to relieve salary deficits brought on by NIH salary caps. The American Surgical Association and the American College of Surgeons combine to sponsor roughly 10 fellowships annually that are open to all areas of surgical research. 24–27 Other fellowship opportunities are limited to specific areas of investigation, such as those sponsored by the Thoracic Surgery Foundation for Research and Education, the American Association for the Surgery of Trauma, the Society for Surgery of the Alimentary Tract, and the Surgical Infection Society, among others. Unfortunately, many of these fellowships are even more competitive than the NIH support they were designed to supplement. In 1999, the American Surgical Association Foundation received 26 applications for only two fellowship awards. 24 Although these programs have provided and will continue to provide many young investigators with much-needed support, additional strategies are warranted to address these issues on a broader scale.
Ensuring adequate representation by surgeons in the peer-review process is paramount to promote the cause of surgical research. The recent expansion of surgeons serving outside the dedicated surgical sections within the peer-review process speaks to the increasing breadth of surgical science. In the future, surgeons must be aware of the rapidly changing profile of science encompassed by their specialty and effectively concentrate themselves within the appropriate study sections. A prospective audit examining the distribution of surgical research proposals may be required to direct future efforts.
In regard to influencing policy changes that may affect our field, we are currently in a very opportune time. The NIH is undergoing a comprehensive restructuring of its peer-review process in an effort to provide a more level playing field for all aspects of biomedical research. 16 Phase I of this effort has already been completed with the proposed formation of a new set of integrated review groups (IRGs). This will include phasing out the present IRG dedicated to the surgical sciences (Surgery, Radiology and Bioengineering) and the creation of a new one entitled Surgical Sciences, Biomedical Imaging and Bioengineering. 28,29 Phase II of this restructuring effort is underway and will involve the formation of study sections within these IRGs by study section boundary teams. Many prominent academic surgeons have been actively involved with these efforts as they pertain to the surgical sciences. Concurrent with these ongoing changes, the NIH plans to vigorously solicit input from the scientific community regarding all aspects of its restructuring plan. This presents a tremendous opportunity for the academic surgical community to voice the need for effective policy changes in the context of current funding trends.
Finally, some have advocated the creation of a separate funding institute dedicated to the surgical sciences. Although this would guarantee a dedicated budget for surgical research funding, the scope of such an institute would likely include the surgical subspecialties as well. Successful funding would still be dependent on the submission of high-quality research proposals and ensuring an adequate degree of participation in the peer-review process. Observations from this study suggest that dedicated institutes are not, in and of themselves, a guarantee of consistent funding support. Of the nonsurgical departments examined in this report, only the department of pediatrics had an institute specifically dedicated to its general scope of research (NICHD). Despite this potential advantage, funding success rates for departments of pediatrics consistently ranked among the lowest within the nonsurgical group.
The NIH has played an integral role in supporting scientific breakthroughs throughout all areas of contemporary academic medicine. Over the last decade, surgeons have lagged behind other clinical academicians in their ability to obtain an equal share of a burgeoning extramural pie. Over the next few years, the NIH will be faced with a markedly attenuated budget due to mandates recently enacted by Congress and the Bush administration. 30 It is anticipated that the number of available grants will be held constant while applications will continue to rise. This will undoubtedly increase the relative intensity of competition. Perhaps now more than ever, proactive strategies will need to be implemented to reverse these trends and level the playing field for surgical research. The future success of academic surgery may depend on it.
Acknowledgments
The authors thank Robert Moore, PhD, for his assistance in gathering the data used in this study, and the Glaser Pediatric Research Network for supporting this research.
DISCUSSION
Dr. Timothy J. Eberlein (St. Louis, MO): Research performed by surgeons has had an enormous impact on human health; for example, vascular anastomoses and suture techniques, endocrine treatment of cancer, surgical nutrition, and transplantation, to name a few. In this manuscript, we see for the first time objective data regarding funding status of surgeons. The authors have utilized NIH funding from the six largest institutes at the NIH. There are obvious limitations to this extrapolation; however, the findings are real. There are really two major issues to be addressed. The first is, are these results a function of bias? Or is it a lack of quality of surgical education?
The authors feel that most likely bias is not involved, and certainly this would be virtually impossible to objectively measure. The potential solution of having a surgical institute at the NIH may also not necessarily be a solution, since departments of pediatrics have access to an institute, and yet success rates for departments of pediatrics consistently rank among the lowest in the nonsurgical group. We therefore must address other issues to improve the quality of surgical applications.
First is to attract the best and the brightest into the field as generation Xers and Nexters are applying for surgical residency programs. We have seen a dramatic reduction in the overall number of applicants and need to change the paradigm of surgical training. Not only does it need to be shorter, but we need to revamp and reinvent the goals of surgical training. We need to make it more attractive for women, who comprise 70% of the top 10% of graduates of American medical colleges. We need to provide the opportunity of having research time, especially following the 4 basic years of surgical training, as proposed by the American Board of Surgery, which, like internal medicine, would provide a smoother transition to junior faculty positions. We need to support the successful programs such as the Young Surgical Investigators Program, whose participants have a 40% success rate of attracting NIH funding, and other such successful programs as the Clinical Trials Course that is sponsored by the American College of Surgeons.
As chairs, we do indeed have a daunting task. We need to provide quality, protected time for our young surgical faculty, as well as what I have termed academic mentors, not necessarily from the department of surgery but perhaps from basic science departments as well. Surgeons need access to contiguous laboratories not dispersed throughout medical centers, because of the efficient nature of their business. They need to be part of a critical mass; I refer to these as research “pods.” Focusing on the last three goals has resulted in a dramatic increase in the number of NIH investigator-initiated awards at our institution, primarily in young surgical investigators.
I have three brief questions for the authors.
One of the criticisms of the lack of surgical funding is the lack of surgical submissions. It appears from your study that there is a direct proportional relationship to the number of faculty and the number of submitted grants. Would you care to comment on the number of submissions by surgeons? And is this an explanation for the lack of surgical funding?
Your study looked at a period of time when there was a relative increase in the number of study sections at the NIH. Did you in fact analyze the new study sections for the specific impact on surgery?
Finally, did you examine the other departments’ specific participation in study sections so as to compare participation of surgical as well as nonsurgical departments with respect to funding levels?
I enjoyed this provocative presentation and would like to thank the authors for providing a copy of the manuscript.
Presenter Dr. R. Lawrence Moss (Palo Alto, CA): Thank you very much, Dr. Eberlein, for your comments and your questions.
Your first question was with respect to the number of grant submissions from departments of surgery. It varies from year to year, but it is roughly 600 per year. The bottom line is we looked at the ratio of success to submissions, so no matter how many grants we submit every year the success rates tend to be markedly lower than the other disciplines. Increasing the number of submissions is certainly a laudable goal, but it isn’t the only solution to the problem.
Your second question surrounded the institution of new study sections. The NIH has instituted some new study sections over the last several years. However, it is our perception and belief that the vast majority of surgical grants either go to the SAT or SB study sections and that there have not been other study sections which have reviewed a significant number of surgical grants.
There are probably some members in the audience who are involved in the NIH restructuring. While we recognize the importance of this effort, it is our belief that the restructuring is not going to significantly impact the surgical disciplines. This is because there are not a significant number of additional surgical study sections being proposed.
Your final question was about other departments and their participation in study sections. We looked at this in a number of ways. Not only are there absolute fewer numbers of surgeons compared to nonsurgeons on study sections, but when we look at the composition of individual study sections, it is exceedingly unlikely or less likely for surgeons to be a majority or a significant proportion of the membership of the study section in comparison to the other departments.
Dr. Alden H. Harken (Denver, CO): I appreciate the opportunity of commenting on this I think very important paper. This is the lifeblood of this organization, and everybody in this room needs to continue to support the concept of basic and surgical clinical investigation. I am going to make several suggestions in the hope that you and Dr. Moss and colleagues will comment on how we can utilize the assembled influence in this room to promote, again, the lifeblood of this organization.
NIH claims that they don’t have enough surgeons that are willing to participate in NIH study sections. As an example, 48 hours ago I chaired a special immunology study section, and there was an x-ray crystallographer, an endotoxin biochemist, and a toll-like receptor guy and a P-38 MAP kinase person, and it soon became apparent I was there as a translator. Surgeons can do that. And I would suggest that we ought to volunteer to participate in that process. We need more translators; we need more people willing to participate.
Now, last year, Olga Jonasson collected names of surgeons that were willing to participate on an NIH study section. You all can submit names. And we can get that information to NIH and they will include those folks in these study sections. But we need the people who are willing to participate and volunteer.
When you get in a study section, I am, you know, astonished in there. And I am reminded, a couple years ago Jo Fischer and I were sitting there watching a very good basic, thoughtful, energetic, industrious, junior surgical investigator absolutely trash a surgical grant, in the way that you and I do an M&M conference. That is what surgeons do: we criticize each other, and we learn from it. But we can’t do it during a study section. We have got to change the paradigm. We then stepped back and watched our anesthesia colleagues exalt the value of yet another malignant hyperthermia application. I mean, there have been more applications funded than there have been patients with the problem.
Dr. Moss, you indicated that the new surgery study sections may not help solve the problem. I should think they will. Several of us were participating in the review of the IRGs last November. We really hammered out an additional surgery study section, which is entitled Systems and Tissue Aspects of Surgery. That is an additional surgery study section in addition to SAT and surgery/bioengineering. And that is going to be the more clinical component of surgery, which I actually think could help us. But again, we need surgical people to participate in that study section.
We need strong surgical applications. Tim Eberlein and Robin McLeod direct two courses run through the College. I think they are very good courses. One is a clinical trials course in November. The other is a “how to write a grant” course run every other year, usually in March. Get your folks to participate in those. They really are good.
And my last suggestion is, when our junior faculty are actively presenting their investigations at the surgical forum sessions in October, to have the people in this room show up at venues like the surgical forum is a big boost. And if everybody in this room just went to one surgical forum session and commented on just one paper and said, “Gosh, you know, this is important, let me tell you how it works,” it would infuse a huge amount of additional enthusiasm into the, again, lifeblood of this organization.
And Dr. Moss, I guess my question to you is, how else can we use the formidable influence of the people in this room to do exactly what we all want to happen?
Thank you again for bringing this to our attention.
Dr. R. Lawrence Moss (Palo Alto, CA): Thank you, Dr. Harken, for your comments and for your leadership in representing our discipline to the NIH. There is no short answer to how we can solve this problem. The most important is to recognize that we do have a problem. And clearly the two answers are: one, to write grants of unassailable quality and take advantage of the opportunities that you pointed out; and two, to be absolutely as involved as possible in the NIH, both in the review process and in administrative roles in the institutes. In this way, we will go from last to first, and we will better represent the interests of our patients.
Footnotes
Presented at the 122nd Annual Meeting of the American Surgical Association, April 24–27, 2002, The Homestead, Hot Springs, Virginia.
Correspondence: R. Lawrence Moss, MD, Division of Pediatric Surgery, Yale University School of Medicine, 333 Cedar Street, PO Box 208062, New Haven, CT 06520-8062.
E-mail: larry.moss@yale.edu
Accepted for publication April 24, 2002.
References
- 1.Moy E, et al. Distribution of research awards from the National Institutes of Health among medical schools. N Engl J Med 2000; 342: 250–255. [DOI] [PubMed] [Google Scholar]
- 2.Sturman LS, et al. Opportunities lost: NIH research funding to New York’s medical schools. J Urban Health. 2000; 77: 86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NIH Office of Extramural Research (http://grants.nih.gov/grants/award/award.htm).
- 4.Center for Scientific Review (CSR) study section roster index webpage (http://www.csr.nih.gov/Committees/rosterindex.asp).
- 5.Malakoff D. U.S. budget. Biomedicine gets record raise as Congress sets 2002 spending. Science. 2002; 295: 24–25. [DOI] [PubMed] [Google Scholar]
- 6.Williams GH, et al. Funding for patient-oriented research. Critical strain on a fundamental linchpin. JAMA. 1997; 278: 227–231. [PubMed] [Google Scholar]
- 7.Peer review: reforms needed to ensure fairness in federal agency grant selection. Washington, DC: GAO, 1994.
- 8.Norman K. Importance of factors in the review of grant proposals. J Appl Psychol. 1986; 71: 156–162. [Google Scholar]
- 9.Wessely S. Peer review of grant applications: what do we know? Lancet 1998; 352: 301–305. [DOI] [PubMed] [Google Scholar]
- 10.Relman AS, Angell M. How good is peer review? N Engl J Med 1989; 321: 827–829. [DOI] [PubMed] [Google Scholar]
- 11.Glantz SA, Bero LA. Inappropriate and appropriate selection of peers in grant review. JAMA. 1994; 272: 114–116. [PubMed] [Google Scholar]
- 12.Agnew B. New NIH procedures to shield clinicians from grants bias. The Scientist. 1998; 12: 1–14. [Google Scholar]
- 13.Zemlo TR, et al. The physician-scientist: career issues and challenges at the year 2000. FASEB J. 2000; 14: 221–230. [DOI] [PubMed] [Google Scholar]
- 14.Fuhrer MJ, Grabois M. Grant application and review procedures of the National Institute of Handicapped Research: survey of applicant and peer-reviewer opinions. Arch Phys Med Rehabil. 1985; 66: 318–321. [PubMed] [Google Scholar]
- 15.Porter A, Rosini F. Peer review of interdisciplinary proposals. Sci Technol Hum Values. 1985; 10: 33–38. [Google Scholar]
- 16.Alberts BM, et al. Proposed changes for NIH’s Center for Scientific Review. Panel on Scientific Boundaries for Review. Center for Scientific Review Advisory Committee, National Institutes of Health. Science 1999; 285: 666–667. [DOI] [PubMed] [Google Scholar]
- 17.Center for Scientific Review (CSR) grant review process webpage. (http://www.csr.nih.gov/Committees/rosterindex.asp).
- 18.Gross CP, Anderson GF, Powe NR. The relation between funding by the National Institutes of Health and the burden of disease. N Engl J Med 1999; 340: 1881–1887. [DOI] [PubMed] [Google Scholar]
- 19.Cicchetti D. The reliability of peer-review for manuscript and grant submissions: a cross-disciplinary investigation. Behav Brain Sci. 1991; 14: 119–186. [Google Scholar]
- 20.Fiscal year 2001 report of the NIH budget allocation.
- 21.Mandel HG. Downsizing of basic science departments in U. S. medical schools: perceptions of their chairs. The National Caucus of Basic Biomedical Science Chairs. Acad Med. 1997; 72: 894–900. [PubMed] [Google Scholar]
- 22.NIH Research training opportunities. Office of Extramural Research website. (http://grants1.nih.gov/training/index.htm).
- 23.Harken A. The role, focus, and funding of research in a department of surgery. Arch Surg 2001; 136: 154–157. [DOI] [PubMed] [Google Scholar]
- 24.Pruitt BA Jr. Centennial changes in surgical care and research. Ann Surg 2000; 232: 287–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kron IL. Getting funded. J Thorac Cardiovasc Surg 2000; 119 (4 Pt 2):S26–28. [DOI] [PubMed] [Google Scholar]
- 26.Yao JS. Research and research funding in vascular surgery. J Vasc Surg 1990; 12: 84–90. [PubMed] [Google Scholar]
- 27.ACS Surgical Research Clearinghouse page. American College of Surgeons website (http://www.facs.org).
- 28.Center for Scientific Review (CSR) website. Update on the Development of Guidelines for the Surgery, Applied Imaging and Applied Bioengineering (SAIAB) Integrated Review Group (http://www. csr.nih.gov/PSBR/SAIAB/SAIAB.htm).
- 29.Center for Scientific Review (CSR) website. Update on Phase 2 of the Panel on Scientific Boundaries for Review Report, February 2002 (http://www.csr.nih.gov/events/updatephase2.htm).
- 30.Malakoff D. NIH prays for a soft landing after its doubling ride ends. Science. 2001; 292: 1992–1995. [DOI] [PubMed] [Google Scholar]


