Abstract
Objective
To compare unilateral and bilateral neck exploration for primary hyperparathyroidism in a prospective randomized controlled trial.
Summary Background Data
Based on the assumption that unilateral neck exploration for a solitary parathyroid adenoma should reduce operating time and morbidity, a variety of minimally invasive procedures have challenged the idea that bilateral neck exploration is the gold standard for the surgical treatment of primary hyperparathyroidism. However, to date, no open prospective randomized trial has been published comparing unilateral and bilateral neck exploration.
Methods
Ninety-one patients with the preoperative diagnosis of primary hyperparathyroidism were randomized to unilateral or bilateral neck exploration. Preoperative scintigraphy and intraoperative parathyroid hormone measurement guided the unilateral exploration. Gross morphology and frozen section determined the extent of parathyroid tissue resection in the bilateral group. The primary end-point was the use of postoperative medication for hypocalcemic symptoms.
Results
Eighty-eight patients (97%) were cured. Histology and cure rate did not differ between the two groups. Patients in the bilateral group consumed more oral calcium, had lower serum calcium values on postoperative days 1 to 4, and had a higher incidence of early severe symptomatic hypocalcemia compared with patients in the unilateral group. In addition, for patients undergoing surgery for a solitary parathyroid adenoma, unilateral exploration was associated with a shorter operative time. The cost for the two procedures did not differ.
Conclusions
Patients undergoing a unilateral procedure had a lower incidence of biochemical and severe symptomatic hypocalcemia in the early postoperative period compared with patients undergoing bilateral exploration. Unilateral neck exploration with intraoperative parathyroid hormone assessment is a valid surgical strategy in patients with primary hyperparathyroidism with distinct advantages, especially for patients with solitary parathyroid adenoma.
Primary hyperparathyroidism (pHPT) is today recognized as a common disease. 1,2 Bilateral neck exploration with identification of at least four parathyroid glands and removal of all hyperfunctioning tissue yields excellent results 3–5 and has thus evolved as the gold standard for the surgical treatment of the disease. 6 However, it is known that 80% to 90% of patients with pHPT have a solitary parathyroid adenoma. 7,8 In these patients, only one gland requires excision for cure. To reduce the risk for postoperative hypocalcemia and to simplify the surgical procedure, the unilateral approach to the solitary parathyroid adenoma was advocated by Wang 9 and later refined by Tibblin et al. 10 Good results have been claimed, with a decreased risk of hypocalcemia 11–14 and vocal cord injury. 11 Since then, better localization modalities such as high-resolution ultrasonography, 15–17 scintigraphy, 18–20 and intraoperative nuclear scanning 21–23 have prompted several groups to modify the original unilateral approach. Furthermore, intraoperative measurement of parathyroid hormone (PTH) has been shown to be a valid method for confirming complete removal of hyperfunctioning parathyroid tissue. 24–30 Most recently, endoscopic or video-assisted unilateral parathyroidectomy, 31–34 as well as focused exploration in local or regional anesthesia, 15,17,24,25 is proposed to improve cosmesis and reduce postoperative pain. 31–34 However, from a principle point of view, the main difference is still between bilateral and unilateral neck exploration.
A recent systemic review comparing unilateral with bilateral neck exploration indicated a tendency to favor the unilateral procedure. 35 To the best of our knowledge, no open prospective randomized controlled trial has been published comparing these two surgical strategies for the treatment of pHPT. Therefore, we designed the present study. We focused on the impact of surgical strategy on early postoperative hypocalcemia.
METHODS
Study Population
Ninety-one patients (18 men, 73 women), referred to the Department of Surgery, Lund University Hospital, Lund, Sweden, for first-time surgery for pHPT between September 1996 and March 2001, were enrolled in the study after written and oral information was given. The exclusion criteria for entering the study were a family history of pHPT (MEN 1, MEN 2, hereditary pHPT), previous neck surgery, other planned operations during the surgical procedure (including thyroid surgery), pregnancy and breast-feeding, emergency operation due to hypercalcemic crisis, and inability to understand information or to comply with scheduled follow-up.
Eight eligible patients were operated on outside the study. Six patients entered a prospective trial for video-assisted surgery of pHPT due to their own preference. Two patients could not be randomized during a short time period when intraoperative PTH analysis was not available due to technical problems. Thus, the 91 randomized patients represented 92% of eligible individuals during the study period.
Informed consent was obtained in all cases. The Ethical Committee of the Medical Faculty, Lund University, approved the study. The preoperative biochemical diagnosis of pHPT was based on a serum calcium level of more than 2.60 mmol/L and a serum PTH level of more than 3.5 pmol/L, with a serum creatinine level of less than 200 μmol/L. The mean age (± SD) of the patients was 67 ± 15 years. The mean (± SD) preoperative serum level of calcium was 2.77 ± 0.15 mmol/L. The mean (± SD) serum PTH level of 10.1 ± 5.2 pmol/L. The mean preoperative serum calcium level of the eight patients operated on outside the study was 2.80 ± 0.16 mmol/L.
Preoperative symptoms and signs were recorded. Thirteen patients were considered asymptomatic.
Planned Intervention
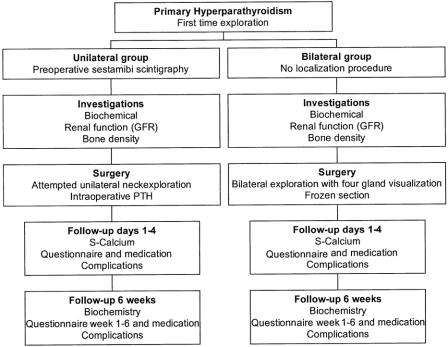
A flow chart summarizing the study is shown in Figure 1.
Figure 1. Flowchart summarizing this prospective randomized trial comparing unilateral with bilateral neck exploration for patients with primary hyperparathyroidism.
During the outpatient visit, eligible patients were randomized to either unilateral neck exploration (study group) or bilateral neck exploration (control group). After randomization, patients in the unilateral group underwent preoperative sestamibi subtraction scintigraphy; no localization procedure was performed in the bilateral group.
Preoperatively, all patients underwent indirect laryngoscopy. Biochemical variables reflecting calcium metabolism and renal function were assessed.
Surgery was performed by three of the authors (A.B., P.L., J.W.), all experienced endocrine surgeons, each performing one third of the operations.
In both groups, surgery was performed through a short (<5 cm) standard Kocher incision. The strap muscles were dissected in the midline and not divided.
In the unilateral group, surgery was started on the side indicated by the preoperative scintigram. If no enlarged parathyroid gland was visualized on the scintigram, the left side was first explored. After finding the first enlarged parathyroid gland, blood samples were drawn for intraoperative measurement of PTH before and at 5 and 15 minutes after gland excision. Surgery was terminated if the PTH levels declined more than 50% after 5 minutes 30 or more than 60% after 15 minutes. 28 No attempts were made per se to visualize normal parathyroid glands.
If no enlarged parathyroid gland was found on the first explored side, or the decline of PTH was insufficient for the diagnosis of a solitary parathyroid adenoma, comprehensive bilateral exploration was performed. Frozen section was not used.
In the bilateral group, surgery was started on the left side and comprehensive bilateral exploration was performed. An attempt was made to visualize four parathyroid glands. The enlarged parathyroid glands were removed for frozen section. The decision to terminate surgery was based on the gross morphology of visualized and excised parathyroid glands in combination with frozen section. Normal parathyroid glands were not routinely biopsied.
Evaluation
Follow-up was done on postoperative days 1 to 4 and 6 weeks after surgery with biochemistry and with a patient questionnaire focusing on the incidence, frequency, and severity of hypocalcemic symptoms. After the first postoperative day, the patients were kept in the patient hotel of the hospital and made individual visits on postoperative days 2 to 4. Patients were given thorough information regarding the specific items on the questionnaire by a registered nurse. The patients were similarly informed by the nurse about hypocalcemic symptoms and were instructed to medicate with oral calcium (T. Kalcitena 250 mg; ACO, Stockholm, Sweden) up to a maximum of 3 g/24 hours when symptomatic. No patient was placed on oral calcium by the surgeon immediately postoperatively. Calcium ingestion and complications were recorded in the study protocol. Indirect laryngoscopy was done before discharge if possible; otherwise, it was performed within 3 weeks postoperatively.
The primary outcome measure was postoperative medication for hypocalcemia during the first 4 postoperative days. The secondary outcome measures were symptomatic hypocalcemia, serum levels of calcium (severe hypocalcemia defined as serum calcium < 2.00 mmol/L), persistent hyperparathyroidism, complications, operative time, and cost.
Sample Size
We previously showed that bilaterally explored patients with pHPT due to a solitary parathyroid adenoma have an increased risk for symptomatic hypocalcemia compared to unilaterally explored patients. They also had lower calcium levels during the first 4 postoperative days. 14 In a pilot study we found that unilaterally explored patients differed in the ingestion of oral calcium during the first 4 postoperative days. Thus, with a type 1 error of 0.05 (two-tailed) and a power of 0.80, it was determined that 44 patients in each arm would be sufficient to detect a difference in 1.0 g oral calcium ingestion in the unilateral group versus 1.75 g calcium in the bilateral group. The difference in calcium medication was considered important since it reflects the severity of early postoperative hypocalcemia.
Statistics
Analysis of outcome for the unilateral and bilateral group was done on an intention-to-treat basis. For numeric data, differences between groups were analyzed with an unpaired t test, except for data with skewed distribution of numbers, when the Mann-Whitney test was used. For categorical data, statistical significance was analyzed using the chi-squared test and the Fisher exact test when expected frequencies were less than 5. A probability level of a random difference of P < .05 was considered significant. Results for continuous variables are reported as mean ± SD if not stated otherwise. For categorical data, absolute numbers in addition to percentage are given.
To estimate early biochemical hypocalcemia, the area under the curve (AUC) for serum calcium concentrations during the first 4 postoperative days was used according to the equation: AUC = T × (0.5f0 + f1 + f2 + . . . + fn-1 + 0.5fn), where T equals the days between sampling and f the calcium concentration of the consecutive samples.
Pain during the first 4 postoperative days, as reported by the patients on a visual analogue scale, was also calculated as the AUC.
Stopping Rules
No particular stopping rules were applied, since previous retrospective comparative studies have not shown the cure rate to differ between unilaterally and bilaterally explored patients.
Assignment
Patients were randomized in blocks of 10 with a sealed envelope to either unilateral or bilateral neck exploration (1:1) during the outpatient visit at the Department of Surgery, Lund University Hospital.
Histopathology
The diagnosis of a parathyroid adenoma and hyperplasia was established by conventional histologic criteria, 37 aided by gross morphology in the bilateral group and in the unilateral group by the perioperative decrease in the serum level of intact PTH.
Sestamibi Scintigraphy
Sestamibi subtraction scintigraphy was performed with 30 MBq 99mTc and 500 MBq 99mTc sestamibi. 38 A result was classified as true positive only if it clearly corresponded to an enlarged parathyroid gland found at the same location at neck exploration.
Renal Function
Glomerular filtration rate was measured using a method for the calculation of plasma clearance of the contrast agent iohexol. 39 The reference values are 20 to 50 years, 80 to 125 mL/min; 51 to 65 years, 60 to 110 mL/min; and 66 to 80 years, 50 to 90 mL/min.
Biochemical Variables
Preoperative blood samples were drawn after an overnight fast the day before surgery. Serum levels of PTH were measured with the intact PTH assay (Incstar, Stillwater, MN). The sensitivity of this assay is 0.13 pmol/L. The interassay coefficient of variation (CV) is less than 11% and the intraassay variation less than 6%. The method has a CV of 2.2% at a value of 5 pmol/L. The reference range is 1.0 to 5.0 pmol/L. To shorten the time for intraoperative analysis, the assay was modified as previously described. 28 The within-assay variation between 0.8 and 10 pmol/L is less than 8% for the rapid method. The correlation between the two methods is 0.99.
High-performance liquid chromatography was used for assessment of 25-hydroxycholecalciferol (25 (OH) D3) and 1.25-dihydroxycholecalciferol (1,25(OH)2 D3) with a radioreceptor assay (Incstar). Serum levels of calcium, alkaline phosphatase, phosphate, and creatinine were analyzed with a routine autoanalyzer (Kodak Ektachem, 700xR-C, Eastman Kodak Co., Rochester, NY).
Costs
The costs for the operative procedure for the two groups of patients were calculated from official in-hospital charges for services performed by different departments. The cost for sestamibi scintigraphy (in U.S. dollars) was $134, intraoperative PTH $126, frozen section $155, and time for anesthesia $12/min.
RESULTS
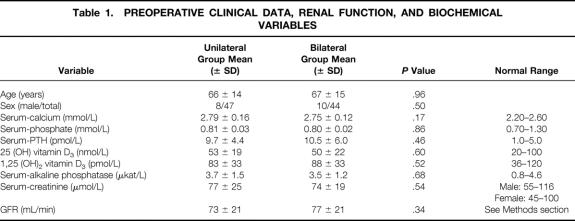
Forty-seven patients were randomized to the unilateral group and 44 patients to the bilateral group. The preoperative clinical and biochemical data as well as renal function were well balanced and did not differ between the two groups (Table 1). There was no difference in clinical signs and symptoms between the two groups (data not shown). Six patients in the unilateral group and seven patients in the bilateral group were considered asymptomatic (P = .67). The eight patients operated on outside the study all had a solitary parathyroid adenoma. They were normocalcemic at the 6-week follow-up.
Table 1. PREOPERATIVE CLINICAL DATA, RENAL FUNCTION, AND BIOCHEMICAL VARIABLES
Analysis of the Whole Group of Patients
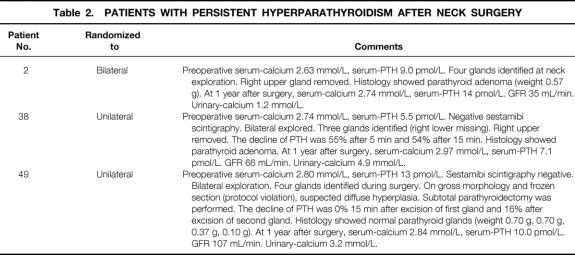
At surgery, 40 patients in the bilateral group had a solitary adenoma and 4 patients multiglandular disease. In the unilateral group, 41 patients had a solitary adenoma and 5 patients multiglandular disease (P > .99). The mean (± SD) weight of the parathyroid adenoma in the unilateral group was 1.24 ± 1.12 g; in the bilateral group it was 1.04 ± 1.29 g (P = .48). In 21 patients, the adenoma weighed less than 500 mg. In one patient in the unilateral group (explored bilaterally, see below), no enlarged parathyroid gland was found at neck exploration. Three patients had persistent hyperparathyroidism at 6 weeks after surgery, two in the unilateral group and one in the bilateral group. Clinical and biochemical data on these patients are shown in Table 2. Thus, the overall cure rate was 97%. There was no difference between the mean (± SD) time for operation in the unilateral group compared with the bilateral group (72 ± 42 minutes vs. 82 ± 37 minutes, P = .22). The costs for the surgical procedure were slightly but not significantly higher in the unilateral group ($2,258 ± 509 vs. $2,097 ± 505, P = .13).
Table 2. PATIENTS WITH PERSISTENT HYPERPARATHYROIDISM AFTER NECK SURGERY
In the unilateral group, 29 of 47 patients were unilaterally explored (62%). Sestamibi subtraction scintigraphy visualized one enlarged parathyroid gland in 35 of 47 patients (74%); in 12 patients (26%) the scan was negative. In comparison, had the same surgical strategy been used in the bilateral group (remove large gland, check PTH, no frozen section) and the left side first explored, 19 of 44 patients (44%) could have had a unilateral dissection.
The median weight of nonlocalized glands was 0.43 g (range 0.20–2.55 g) versus 0.87 g (range 0.20–5.85 g) for localized glands (P < .05, Mann-Whitney U test). Of the patients with negative scans, 1 patient had asymmetric hyperplasia with three enlarged glands and 10 patients had a solitary parathyroid adenoma; in 1 patient with four normal parathyroid glands identified during surgery, no enlarged gland was found. Of the 35 positive scans, a solitary parathyroid adenoma at the suggested location was confirmed in 29 patients. Thus, the sensitivity to localize a solitary parathyroid adenoma in the unilateral group was 71% (29 of 41 parathyroid adenomas) and the positive predictive value for an adenoma was 83%. In the six patients with incorrect scans, two patients with solitary parathyroid adenoma were not correctly lateralized and four patients had asymmetric hyperplasia with two enlarged glands each. Thus, in no patient was multiglandular disease predicted by the scan.
The mean (± SD) decline of PTH after excision of the first enlarged parathyroid gland was 54 ± 25% after 5 minutes (n = 44, three tests missing due to technical problems) and 69 ± 25% after 15 minutes. Fifteen minutes after excision of the enlarged parathyroid gland, 35 patients (74%) declined by more than 60%. These patients were cured by surgery (solitary parathyroid adenoma). Twelve patients (36%) declined by less than 60%. Five of these patients were found to have multiglandular disease during neck exploration, and they were cured. In one patient, a 3.5-gland resection was performed due to suspicion of diffuse hyperplasia macroscopically as well as on frozen section (protocol violation). However, histology showed normal parathyroid glands. The patient has persistent hyperparathyroidism, and therefore a solitary parathyroid adenoma in a fifth gland is suspected (see Table 2, patient 49). One patient declined by more than 50% at 5 minutes after surgery, and thus the operation was terminated. However, this patient has persistent HPT as predicted by the PTH level 15 minutes after gland excision (see Table 2, patient 38).
In three patients, no other enlarged gland was found despite comprehensive bilateral exploration. These patients are cured (serum calcium 2.21, 2.46, and 2.48 mmol/L at 1 year after surgery, with normal levels of intact PTH).
Thus, the sensitivity for a solitary parathyroid adenoma at 15 minutes was 92%, the specificity 100%, the positive predictive value 100%, and the negative predictive value 75%.
During the first 4 postoperative days, patients in the unilateral group consumed significantly less oral calcium (0.78 ± 1.07 g) compared to patients in the bilateral group (1.94 ± 2.69 g, P < .01).
On the first postoperative day, 19 of 39 patients in the bilateral group (49%) and 12 of 43 patients (28%) in the unilateral group reported mild hypocalcemic symptoms (tingling in the lips, fingers, and toes) (P = .052). Furthermore, 4 of 39 patients (10%) in the bilateral group versus zero of 43 patients in the bilateral group reported severe symptoms (i.e., muscle cramps) (P < .05). No difference was found in the frequency of self-reported hypocalcemic symptoms on postoperative days 2 to 4. There was no significant difference between the two groups in terms of postoperative pain recorded by the patients (Fig. 2).
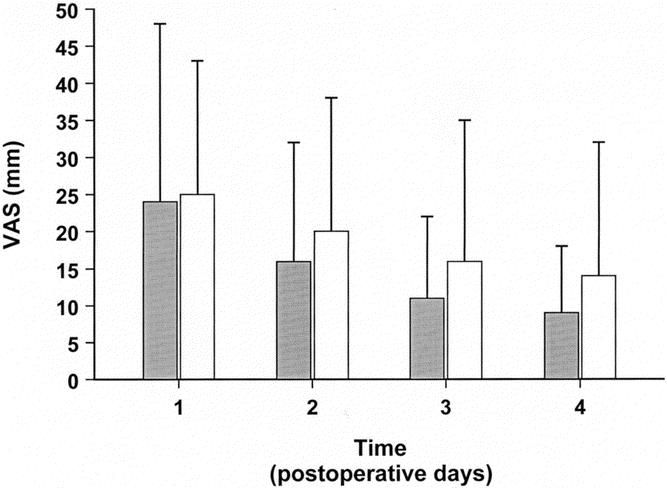
Figure 2. Postoperative pain, as estimated on a visual analogue scale (VAS), during the first 4 days after surgery in patients with unilateral or bilateral neck exploration for primary hyperparathyroidism. Bilateral group, □; unilateral group ▪. Mean (± SD) is shown. No difference was found between the two groups of patients (AUC;P = .24).
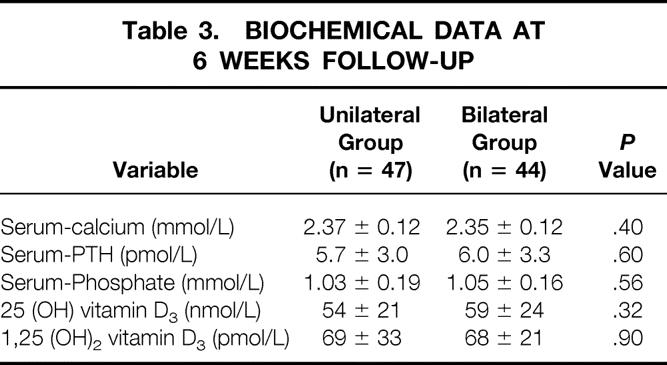
The serum calcium levels during the first 4 postoperative days for the patients in the unilateral and the bilateral group are shown in Figure 3. On the second postoperative day, the serum calcium concentration was significantly lower in the bilateral group compared with the unilateral group (2.15 ± 0.14 mmol/L vs. 2.26 ± 0.17 mmol/L, P < .01). Furthermore, the AUC for serum calcium during the first 4 postoperative days was smaller in the bilateral group (6.53 ± 0.42 vs. 6.71 ± 0.44, P < .05). During the first 6 weeks after surgery (excluding the first 4 postoperative days), patients in the bilateral group consumed more oral calcium (4.20 ± 6.67 g) than patients in the unilateral group (1.92 ± 3.86 g, P < .05), although self-reported hypocalcemic symptoms did not differ between the two groups. There was no difference in the biochemical variables measured at 6 weeks after surgery (Table 3).
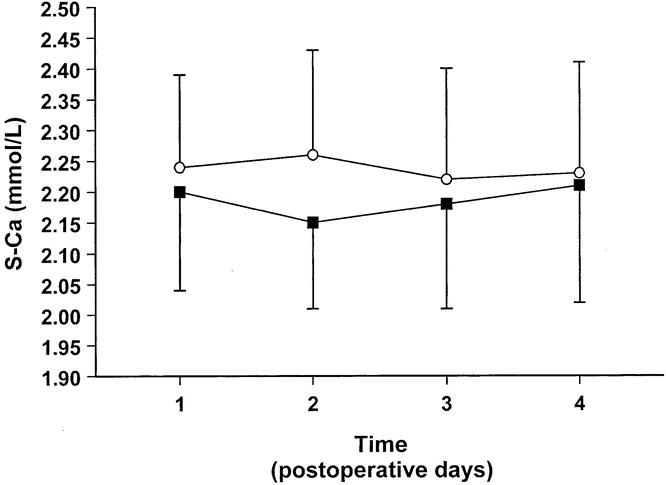
Figure 3. Serum calcium values (S-Ca) for the first 4 postoperative days in patients enrolled in a prospective randomized trial comparing unilateral with bilateral neck exploration for patients with primary hyperparathyroidism. Bilateral group, ▪; unilateral group, ⊙ Mean (± SD) is shown.
Table 3. BIOCHEMICAL DATA AT 6 WEEKS FOLLOW-UP
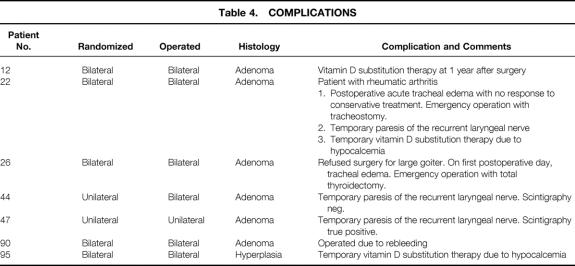
Three patients had vocal cord palsy on indirect laryngoscopy after surgery, two in the unilateral and one in the bilateral group (P = .99); all were temporary.
Two patients with a solitary parathyroid adenoma and one patient with multiglandular disease experienced postoperative hypoparathyroidism with vitamin D substitution therapy, all in the bilateral group (P = .11). In two of these cases (one patient with adenoma and one patient with multiglandular disease), the medication was temporary, whereas one patient with adenoma still requires vitamin D substitution 1 year after surgery. Three other significant complications were recorded, all in the bilateral group (Table 4). Thus, 5 of 44 patients (11%) in the bilateral group and 2 of 47 patients (4%) in the unilateral group had a significant complication (P = .27; Fisher’s exact test).
Table 4. COMPLICATIONS
Analysis of Patients With Solitary Parathyroid Adenoma
The mean (± SD) operative time was significantly shorter in the unilateral group compared to the bilateral group (62 ± 29 minutes vs. 84 ± 38 minutes, P < .01). During the first 4 postoperative days, patients in the unilateral group consumed significantly less oral calcium (0.66 ± 0.89 g) compared to patients in the bilateral group (1.85 ± 2.77 g, P = .01). On the first postoperative day, 4 of 35 patients in the bilateral group (11%) and zero of 38 patients in the unilateral group reported severe hypocalcemic symptoms (i.e., muscle cramps) (P < .05). Self-reported hypocalcemic symptoms did not differ day 2 to 4. Patients with a solitary parathyroid adenoma in the bilateral group had lower serum levels of calcium on the second postoperative day compared to patients in the unilateral group (2.15 ± 0.14 mmol/L vs. 2.25 ± 0.15 mmol/L, P < .01). Furthermore, the nadir of serum calcium during the first 4 postoperative days was lower in the bilateral group (2.09 ± 0.15 mmol/L) compared with the unilateral group (2.15 ± 0.12, P < .05). In 10 of 40 patients in the bilateral group (25%) and 3 of 41 patients (7%) in the unilateral group, severe biochemical hypocalcemia (<2.00 mmol/L) was recorded during the first 4 postoperative days (P = .04).
The AUC for serum calcium levels during the first 4 postoperative days was significantly smaller for patients in the bilateral group compared to the unilateral group (6.5 ± 0.42 vs. 6.7 ± 0.39, P < .05). At the 6-week follow-up, there was no difference in the biochemical variables measured or in self-reported hypocalcemic symptoms and oral calcium medication.
DISCUSSION
During the past decade, new surgical procedures have evolved for the treatment of pHPT. From a principle point of view, the main difference is still between bilateral and unilateral neck exploration. The latter could be performed using a variety of forms of general and local anesthesia. The main claim of the proponents of unilateral neck exploration is that compared with bilateral exploration, the unilateral approach carries a decreased risk for temporary and permanent hypocalcemia, 10–13,40 without an increased risk for persistent or recurrent pHPT. 13 To the best of our knowledge, the present trial is the first prospective randomized study analyzed on an intention-to-treat basis between unilateral and bilateral neck exploration.
The results from the present study are quite clear. Although only 29 of 47 patients (62%) in the unilateral group ultimately underwent focused adenoma excision, the unilateral approach offered some distinct benefits. Patients operated on using a unilateral approach consumed less oral calcium during the first 4 postoperative days. They also had less incidence and severity of symptomatic and biochemical hypocalcemia. For patients with a solitary parathyroid adenoma, we also found that the operative time was shorter in the unilateral group. Furthermore, there was no difference in cure rate between the two patient groups. The complications were found mainly in the bilaterally explored patients (see Table 4).
Our trial raises a number of possible questions.
Although the costs for the operative procedures did not differ between the two groups, the moderate sensitivity for a solitary parathyroid adenoma by the sestamibi scintigraphy, in this study 71%, is a cause of concern. A high sensitivity of the preoperative localization procedure is of great importance for a successful focused neck exploration. Furthermore, in agreement with previous investigations, we confirmed that preoperative sestamibi scintigraphy does not reliably predict multiglandular disease. 38,41 We have previously reported a high sensitivity for solitary parathyroid adenoma, 38 but the results were not reproduced in the present trial. Since gland weight has been shown to be one of the chief determinants of sestamibi sensitivity, 42 one reason could be the relatively high incidence of small adenomas. In the present study the adenoma weight was less than 500 mg in 21 patients, and the mean weight for nonlocalized glands was lower than the weight for glands localized by sestamibi scintigraphy. Another possibility is that the previous study was confounded by a referral bias; that is, patients tend to be referred for surgery more often if sestamibi scintigraphy is positive.
To optimize the cost-effectiveness of the unilateral method, the accuracy of sestamibi scintigraphy clearly needs to be improved. By adding delayed sestamibi scans based on differential washout kinetics 43 and single photon emission computed tomography (SPECT) 44 or oblique views with a higher-dose 99mTc sestamibi, 45 an increased sensitivity might be possible. However, this remains to be proven in prospective controlled trials.
The incidence of multiglandular disease has previously been estimated to be about 15% of patients being operated on due to pHPT. 7,8 However, the incidence of multiglandular disease in a patient cohort in which intraoperative PTH guided the extent of tissue resection was recently found to be as low as 5%. 46 In this study, histologically proven multiglandular disease was found in 5 of 47 patients in the unilateral group and in 4 of 44 patients in the bilateral group. One patient in each group had persistent hyperparathyroidism despite one enlarged gland being excised. Thus, the true incidence of multiglandular disease was 13% in the unilateral group and 11% in the bilateral group. The data therefore strongly suggest that the incidence of multiglandular disease was not underestimated in the unilateral group.
One patient in whom the PTH level declined by more than 50% 5 minutes after excision of an enlarged parathyroid gland was not cured. This finding is in agreement with previous investigations 47–49 suggesting that a 50% decrease in PTH level is not an entirely reliable predictor for postoperative normocalcemia.
To enhance the accuracy of the intraoperative PTH measurement, we have developed a rigid protocol. First, blood samples are always drawn in a peripheral vein. Second, the baseline sample should be obtained when the first enlarged parathyroid gland is visualized, since we have shown that after general anesthesia the levels of ionized calcium decrease and the levels of PTH increase. 50 Third, the dissection of the enlarged parathyroid gland must be extremely precise, without pressure on the gland and with clipping of the vascular pedicle as the last measure. Fourth, we have previously shown that a decline of PTH by more than 60% at 15 minutes after excision of an enlarged parathyroid gland is highly specific in predicting cure of patients with pHPT. 29 In agreement, in the present investigation a decline by more than 60% at 15 minutes after gland excision predicted cure in all patients.
In the present investigation, the cure rate was 97%. Three patients, two in the unilateral group (both bilaterally explored according to the study protocol) and one in the bilateral group, had persistent hyperparathyroidism. In agreement, retrospective comparative studies have not shown an increased incidence of persistent or recurrent pHPT for patients explored with a unilateral approach. 11,13,40
In summary, in this prospective randomized trial, patients operated on according to a unilateral approach consumed less oral calcium and had a lower incidence of biochemical and early severe symptomatic hypocalcemia compared with patients explored bilaterally, with no difference in cure rate. Whether endoscopic or video-assisted surgery or other minimally invasive techniques could provide additional benefits in terms of early ambulation and less local discomfort and pain compared to the classical “open” unilateral method needs to be answered in future randomized trials.
Footnotes
Correspondence: Anders Bergenfelz, MD, PhD, Department of Surgery, Lund University Hospital, S-221 85 Lund, Sweden.
E-mail: anders.bergefelz@skane.se
Accepted for publication April 2, 2002.
References
- 1.Lundgren E, Rastad J, Thurfjell E, et al. Population-based screening for primary hyperparathyroidism with serum calcium and parathyroid hormone in menopausal women. Surgery 1997; 121: 287–294. [DOI] [PubMed] [Google Scholar]
- 2.Jorde R, Bonaa KH, Sundsfjord J. Primary hyperparathyroidism detected in a health screening. The Tromso study. J Clin Epidemiol 2000; 53: 1164–1169. [DOI] [PubMed] [Google Scholar]
- 3.Van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg 1991; 15: 688–692. [DOI] [PubMed] [Google Scholar]
- 4.Delbridge LW, Younes NA, Guinea AL, et al. Surgery for primary hyperparathyroidism 1962–1996: indications and outcome. Med J Aust 1998; 168: 153–156. [DOI] [PubMed] [Google Scholar]
- 5.Funke M, Kim M, Hasse C, et al. Results of a standardized treatment concept in primary hyperparathyroidism [in German]. Dtsch Med Wochenschr 1997; 122: 1475–1484. [DOI] [PubMed] [Google Scholar]
- 6.Tibblin S, Bondesson AG, Udén P. Current trends in the surgical treatment of solitary parathyroid adenoma. A questionnaire study from 53 surgical departments in 14 countries. Eur J Surg 1991; 157: 103–107. [PubMed] [Google Scholar]
- 7.Russell CF, Edis AJ. Surgery for primary hyperparathyroidism: experience with 500 consecutive cases and evaluation of the role of surgery in the asymptomatic patient. Br J Surg 1982; 69: 244–247. [DOI] [PubMed] [Google Scholar]
- 8.Rudberg C, Åkerström G, Palmér M, et al. Late results of operation for primary hyperparathyroidism in 441 patients. Surgery 1986; 99: 643–651. [PubMed] [Google Scholar]
- 9.Wang CA. Surgical management of primary hyperparathyroidism. Curr Prob Surg 1985; 22: 1–50. [DOI] [PubMed] [Google Scholar]
- 10.Tibblin S, Bondesson A-G, Ljungberg O. Unilateral parathyroideactomy in hyperparathyroidism due to single adenoma. Ann Surg 1982; 195: 245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Worsey MJ, Carty SE, Watson CG. Success of unilateral neck exploration for sporadic primary hyperparathyroidism. Surgery 1993; 114: 1024–1030. [PubMed] [Google Scholar]
- 12.Tibblin S, Bondeson AG, Bondeson L, et al. Surgical strategy in hyperparathyroidism due to solitary adenoma. Ann Surg 1984; 200: 776–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tibblin S, Bizard JP, Bondeson AG, et al. Primary hyperparathyroidism due to solitary adenoma. A comparative multicentre study of early and long-term results of different surgical regimens. Eur J Surg 1991; 157: 511–515. [PubMed] [Google Scholar]
- 14.Westerdal J, Lindblom P, Valdemarsson S, et al. Risk factors for postoperative hypocalcemia after surgery for primary hyperparathyroidism. Arch Surg 2000; 135: 142–147. [DOI] [PubMed] [Google Scholar]
- 15.Chapuis Y, Fulla Y, Bonnichon P, et al. Values of ultrasonography, sestamibi scintigraphy and intraoperative measurement of 1–84 PTH for unilateral neck exploration of primary hyperparathyroidism. World J Surg 1996; 20: 835–840. [DOI] [PubMed] [Google Scholar]
- 16.Koslin DB, Adams J, Andersen P, et al. Preoperative evaluation of patients with primary hyperparathyroidism: role of high-resolution ultrasound. Laryngoscope 1997; 107: 1249–1253. [DOI] [PubMed] [Google Scholar]
- 17.Inabnet WB, Fulla Y, Richard B, et al. Unilateral neck exploration under local anesthesia: the procedure of choice for asymptomatic primary hyperparathyroidism. Surgery 1999; 126: 1004–1009. [DOI] [PubMed] [Google Scholar]
- 18.Tsukamoto E, Russell CF, Fergurson WR, et al. The role of preoperative thallium-technetium subtraction scintigraphy in the surgical management of patients with solitary parathyroid adenoma. Clin Radiol 1995; 50: 677–680. [DOI] [PubMed] [Google Scholar]
- 19.Borley NR, Collins RE, O’Doherty M, et al. Technetium-99m sestamibi is accurate enough for scan-directed unilateral neck exploration. Br J Surg 1996; 83: 989–991. [DOI] [PubMed] [Google Scholar]
- 20.Carty SE, Worsey J, Virji MA, et al. Concise parathyroidectomy: the impact of preoperative SPECT 99mTc sestamibi scanning and intraoperative quick parathormone assay. Surgery 1997; 122: 1107–1116. [DOI] [PubMed] [Google Scholar]
- 21.Norman J, Chheda H. Minimally invasive parathyroidectomy facilitated by intraoperative nuclear mapping. Surgery 1999; 122: 1107–1116. [DOI] [PubMed] [Google Scholar]
- 22.Murphy C, Norman J. The 20% rule: a single instantaneous radioactivity measurement defines cure and allows elimination of frozen section and hormone assays during parathyroidectomy. Surgery 1999; 126: 1023–1028. [DOI] [PubMed] [Google Scholar]
- 23.Goldstein RE, Blevini L, Delbeke D, et al. Effect of minimally invasive radioguided parathyroidectomy of efficacy, length of stay and costs in the management of primary hyperparathyroidism. Ann Surg 2000; 231: 732–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bergenfelz A, Algotsson L, Ahrén B. Surgery for primary hyperparathyroidism performed under local anaesthesia. Br J Surg 1992; 79: 931–934. [DOI] [PubMed] [Google Scholar]
- 25.Chen H, Sokoll LJ, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery 1999; 126: 1016–1021. [DOI] [PubMed] [Google Scholar]
- 26.Nussbaum S, Thompson A, Hutcheson K, et al. Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism. Surgery 1988; 104: 1121–1127. [PubMed] [Google Scholar]
- 27.Bergenfelz A, Nordén NE, Ahrén B. Intraoperative fall in plasma levels of intact parathyroid hormone after removal of one enlarged parathyroid gland in hyperparathyroid patients. Eur J Surg 1991; 157: 109–112. [PubMed] [Google Scholar]
- 28.Bergenfelz A, Isaksson A, Ahrén B. Intraoperative monitoring of intact PTH during surgery for primary hyperparathyroidism. Langenbecks Arch Surg 1994; 379: 178–181. [DOI] [PubMed] [Google Scholar]
- 29.Bergenfelz A, Isaksson A, Lindblom P, et al. Measurement of parathyroid hormone in patients with primary hyperparathyroidism undergoing first an reoperative surgery. Br J Surg 1998; 85: 1129–1132. [DOI] [PubMed] [Google Scholar]
- 30.Irvin GL, Prudhomme DL, Deriso GT, et al. A new approach to parathyroidectomy. Ann Surg 1994; 219: 574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry JF, Defechereux T, Gramatic L, et al. Minimally invasive videoscopic parathyroidectomy by lateral approach. Langenbecks Arch Surg 1999; 384: 298–301. [DOI] [PubMed] [Google Scholar]
- 32.Gauger PG, Reeve TS, Delbridge LW. Endoscopically assisted minimally invasive parathyroidectomy. Br J Surg 1999; 86: 1563–1566. [DOI] [PubMed] [Google Scholar]
- 33.Miccoli P, Berti P, Conte M, et al. Minimally invasive video-assisted parathyroidectomy: lesson learned from 137 cases. J Am Coll Surg 2000; 191: 613–618. [DOI] [PubMed] [Google Scholar]
- 34.Dralle H, Lorenz K, Nguyen-Thanh P. Minimally invasive video-assisted parathyroidectomy-selective approach to localized single gland adenoma. Langenbecks Arch Surg 1999; 384: 556–562. [DOI] [PubMed] [Google Scholar]
- 35.Reeve TS, Babidge WJ, Parkyn RF, et al. Minimally invasive surgery for primary hyperparathyroidism: Systematic review. Arch Surg 2000; 135: 481–487. [DOI] [PubMed] [Google Scholar]
- Sosa J, Powe N, Levine M, et al. Cost implications of different surgical strategies for primary hyperparathyroidism. Surgery 1998; 124: 1028–1036. [DOI] [PubMed] [Google Scholar]
- 37.Grimelius L, Åkerström G, Bondesson L, et al. The role of the pathologist in the diagnosis and surgical decision making in hyperparathyroidism. World J Surg 1991; 15: 698–705. [DOI] [PubMed] [Google Scholar]
- 38.Bergenfelz A, Tennvall J, Valdemarsson S, et al. Sestamibi versus thallium subtraction scintigraphy in parathyroid localization: A comparative prospective study in patients with predominantly mild hyperparathyroidism. Surgery 1997; 121: 601–605. [DOI] [PubMed] [Google Scholar]
- 39.Krutzén E, Bäck SE, Nilsson-Ehle I, et al. Plasma clearance of a new contrast agent, iohexol: a method for the assessment of glomerular filtration rate. J Lab Clin Med 1984; 104: 955–961. [PubMed] [Google Scholar]
- 40.Petti GHJ, Chonkich GD, Morgan JW. Unilateral parathyroidectomy: the value of localizing scan. J Otolaryngol 1993; 22: 307–310. [PubMed] [Google Scholar]
- 41.McBiles M, Lambert AT, Cote MG, et al. Sestamibi parathyroid imaging. Semin Nucl Med 1995; 25: 221–234. [DOI] [PubMed] [Google Scholar]
- 42.Lee VS, Wilkinsson RH, Leight GS Jr, et al. Hyperparathyroidism in high-risk surgical patients: evaluation with double-phase technetium-99m sestamibi imaging. Radiology 1995; 197: 627–633. [DOI] [PubMed] [Google Scholar]
- 43.Billotey C, Aurengo A, Najean Y, et al. Identifying abnormal parathyroid glands in the thyroid uptake area using technetium-99m sestamibi and factor analysis of dynamic structures. J Nucl Med 1994; 35: 1631–1636. [PubMed] [Google Scholar]
- 44.Taillefer R. 99mTc sestamibi parathyroid scintigraphy. In: Freeman EM, ed. Nuclear medicine annual 1995. New York: Raven Press, 1995: 51–79.
- 45.Norman J, Chheda H, Farrell C. Minimally invasive parathyroidectomy for primary hyperparathyroidism: decreasing operative time and potential complications while improving cosmetic results. Am Surg 1998; 64: 391–396. [PubMed] [Google Scholar]
- 46.Molinari AS, Irvin GL III, Deriso GT, et al. Incidence of multiglandular disease in primary hyperparathyroidism as determined by parathyroid hormone. Surgery 1996; 120: 934–936. [DOI] [PubMed] [Google Scholar]
- 47.Garner SC, Leight GS Jr. Initial experience with intraoperative PTH determinations in the surgical management of 130 consecutive cases of primary hyperparathyroidism. Surgery 1999; 126: 1132–1137. [DOI] [PubMed] [Google Scholar]
- 48.Weber CJ, Ritchie JC. Retrospective analysis of sequential changes in serum intact parathyroid hormone levels during conventional parathyroid exploration. Surgery 1999; 126: 1139–1143. [DOI] [PubMed] [Google Scholar]
- 49.Gordon LL, Snyder WH III, Wians F Jr, et al. The validity of quick intraoperative parathyroid hormone assay: an evaluation in seventy-two patients based on gross morphologic criteria. Surgery 1999; 126: 1030–1035. [DOI] [PubMed] [Google Scholar]
- 50.Lindblom P, Valdemarsson S, Westerdahl J, et al. Hyperthyroidism after surgery for primary hyperparathyroidism. Langenbecks Arch Surg 1999; 384: 568–575. [DOI] [PubMed] [Google Scholar]