Abstract
Purpose
To determine preoperative risk factors predictive of adverse outcomes after gastric bypass surgery.
Summary Background Data
Gastric bypass results in sustained weight loss for seriously obese patients, but perioperative complications can be formidable. Preoperative risk assessment is important to establish the risk-benefit ratio for patients undergoing these operations.
Methods
Data for 10 risk factors predictive of adverse outcomes were collected on 1,067 consecutive patients undergoing gastric bypass surgery at the UCLA Medical Center from December 1993 until June 2000. Univariate analyses were performed for individual risk factors to determine their potential significance as predictors for complications. All 10 risk factors were entered into a logistic regression model to determine their significance as predictors for complications. Sensitivity analysis was performed.
Results
Univariate analysis revealed that male gender and weight were predictive of severe life-threatening adverse outcomes. Multistep logistic regression yielded only male gender as a risk factor. Male patients were heavier than female patients on entry to the study, accounting for weight as a potential risk factor. Patients older than 55 years had a threefold higher mortality from surgery than younger patients, although the complication rate, 5.8%, was the same in both groups. Sensitivity analysis demonstrated that the risk for severe life-threatening adverse outcomes in women increased from 4% for a 200-lb female patient to 7.5% for a 600-lb patient. The risk increased from 7% for a 200-lb male patient to 13% for a 600-lb patient.
Conclusions
Large male patients are at greater risk for severe life-threatening complications than smaller and/or female patients. Risk factors thought to be predictive of adverse outcomes, such as a history of smoking or diabetes, proved not to be significant in this analysis. Older patients had the same complication rate but a threefold higher mortality, suggesting that they lack the reserve to recover from complications when they occur.
The incidence of obesity is increasing in epidemic proportions in the United States. Overweight patients are at increased risk for the development of diabetes, hypertension, hyperlipidemia, sleep apnea, and osteoarthritis and other degenerative diseases. These secondary diseases culminate in increased mortality that exceeds twofold in women 1,2 and 12-fold in men. 3 Diet and exercise can be effective for inducing weight loss, and small amounts of weight loss can result in substantial reductions in obesity-induced early mortality. 4,5 Unfortunately, for very obese patients, sustained weight loss following medical treatment is short-lived. More than 90% of seriously obese individuals will regain their weight after it is lost with dieting. 6 It is these patients who have the highest risk for obesity-induced early mortality. Mortality increases logarithmically for body mass indices that exceed 30. 1–3 The largest patients have the most compelling need for weight loss, yet medical treatments are rarely successful for them.
Only surgery results in sustained weight loss for seriously obese patients. The Roux-en-Y gastric bypass results in the greatest, most sustained weight loss of the restrictive gastric bariatric procedures. Surgically induced weight loss ameliorates obesity-related risk factors, such as diabetes and hypertension, that cause early mortality in obese patients. Although surgery in obese patients has acceptable levels of morbidity and mortality, severe life-threatening complications such as pulmonary embolism and anastomotic leakage do occur. Management of these complications can be difficult, and they can result in substantial morbidity and mortality. Identification of preoperative risk factors predictive of adverse events is necessary to minimize the risk of adverse events. Preoperative conditions predictive of surgical complications can be treated before surgery to minimize risk. For cases where the risk cannot be minimized, the informed consent process can be improved by presenting patients with the full spectrum of potential complications, along with a realistic estimate for the rate at which they occur.
The purpose of this study was to prospectively collect risk factor and complication data on a large cohort of patients undergoing gastric bypass procedures at a single institution. The relationship between preoperative risk factors and severe life-threatening complications was assessed by univariate analysis and multistep logistic regression to determine which of the risk factors was predictive of adverse outcomes. Complication data were compiled to determine the rate at which individual complications occur. Preoperative conditions that individually predicted adverse events were identified and a model predicting outcomes was developed. Sensitivity analysis was then performed on the model to quantitate the effect individual risk factors had on the probability of postoperative severe life-threatening adverse events.
METHODS
Patients and Risk Factors
We studied all patients undergoing Roux-en-Y gastric bypass for obesity at the UCLA Medical Center from December 1993 until December 2000. We identified 10 preoperative clinical features that potentially increased the risk of adverse outcomes: weight, height, body mass index (BMI), gender, history of smoking, the presence of hypertension, diabetes, osteoarthritis, sleep apnea, and the need for continuous positive airway pressure (CPAP) during the perioperative period. Patients who had prior obesity surgery and were undergoing conversions to gastric bypass were included in this study.
Outcomes
All gastric bypass operations at the UCLA Medical Center were considered index procedures during the study period. All cases were reviewed for adverse outcomes. The attending physicians or house staff reported complications to the QA manager, who entered them into a database. Major complications or deaths following hospital discharge that were reported to the obesity surgery team members were also catalogued in the database. Major complications were defined as those that were life-threatening or required ICU admission within 30 days of the gastric bypass operation. Complications requiring unanticipated surgeries at any time following the gastric bypass, such as those for bowel obstruction, were also counted as complications. Mortality was defined as death from any cause within 30 days of the gastric bypass procedure, or if it occurred as a direct result of a perioperative complication irrespective of the time interval between surgery and death.
Statistical Analysis
All severe life-threatening complications were analyzed separately. Each death was preceded by at least one complication. Some patients had multiple complications. The dependent variable for statistical analysis was the number of patients with complications and/or deaths. Thus, patients with multiple complications or complications preceding death were counted only once.
Each risk factor was assessed in a univariate analysis to assess whether it significantly predicted severe life-threatening postoperative complications and/or death. Statistical significance relating risk factors with continuous variables to the outcome of complication and/or death was determined by t tests. Risk factors with dichotomous variables were tested by chi-square analysis. Each risk factor was tested independently to determine if it significantly contributed to the outcome of complications or death. Multistep logistic regression was performed to confirm the significance of preoperative risk factors identified in the univariate analysis. Sensitivity analysis was performed by entering a range of values into the regression equation variables and determining their effect on the probability of developing postoperative complications. This facilitated assessment of the relative contribution of individual risk factors to the overall severe life-threatening complication rate.
RESULTS
Patient Demographics
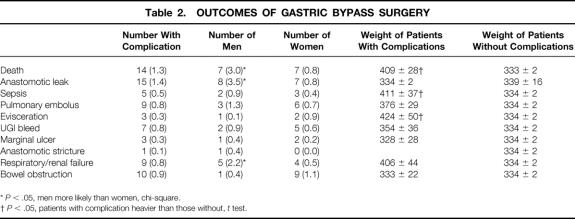
During the study period, 1,067 patients underwent Roux-en-Y gastric bypass operations. Table 1 summarizes the patient demographic information. Seventy-eight percent of the patients were female. Male patients were taller and larger than female patients. Comorbid conditions were more frequent in men. The incidences of hypertension, diabetes, and sleep apnea and the need for CPAP were significantly higher in men compared to women. There were no differences in age, smoking history, osteoarthritis, or the performance of revision operations between men and women.
Table 1. PATIENT DEMOGRAPHICS
*P < .05, women vs. men, t test.
†P < .05, women vs. men, chi-square.
Data are presented as the mean ± standard error of the mean. Percentages are relative to the number of patients referred to in a column. In our population there were 22% men and 78% women.
Complications
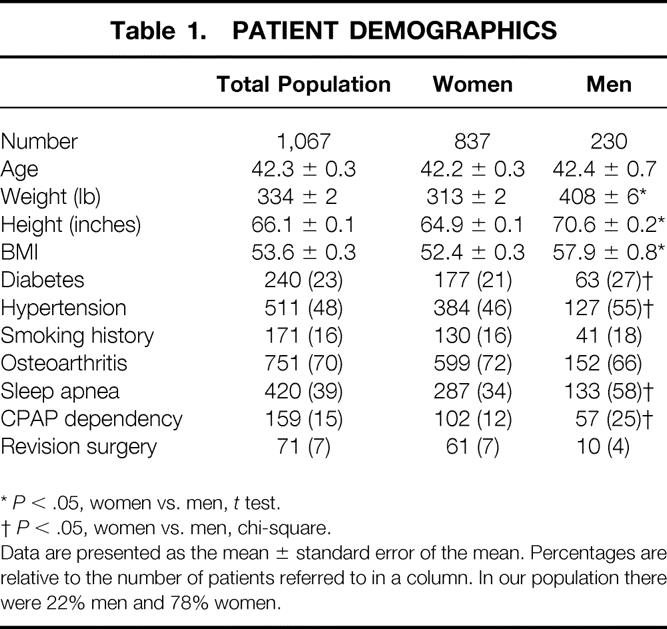
Table 2 lists the numbers of deaths and severe life-threatening complications and the types of complications occurring in this series of gastric bypass patients. There were 14 deaths. Deaths occurred more frequently in men, and patients who died were heavier than those who lived. Six deaths were secondary to pulmonary emboli; thus, 67% of pulmonary emboli in this series were fatal. Three patients died from sepsis of unknown etiology; a fourth died from sepsis secondary to an anastomotic leak. One of the patients who died of sepsis developed this several months after a liver transplant necessitated by an iatrogenic portal vein injury at the time of the gastric bypass. Two died from respiratory and/or renal failure of uncertain etiology. One of these had pulmonary hypertension that was refractory to medical therapy, but the cause of the pulmonary hypertension could not be determined at autopsy. Two patients died following massive UGI hemorrhage.
Table 2. OUTCOMES OF GASTRIC BYPASS SURGERY
*P < .05, men more likely than women, chi-square.
†P < .05, patients with complication heavier than those without, t test.
Anastomotic leaks were the most frequent complication (n = 15). These were more common in men than in women; in contrast to deaths, however, there were no significant differences in weight between those with or without leaks. Only 2 of the 10 anastomotic leaks occurred with patients undergoing revision operations. Ten patients developed small bowel obstructions, and one patient developed an anastomotic stricture requiring reoperation. There were nine pulmonary emboli that were not related to gender or weight. Nine patients developed various combinations of respiratory and renal failure for which the underlying etiology was never identified. Two patients developed respiratory failure, three renal failure, and four combined respiratory and renal failure. Respiratory failure was secondary to either renal failure or congestive heart failure, or was from primary lung failure. This syndrome occurred more frequently in men, and there was a trend of being heavier than those without the complication, but the difference in weight did not reach statistical significance. All these patients underwent extensive testing including UGI studies, abdominal CT scans, and exploratory laparotomy. Despite aggressive attempts at identifying the septic focus, none was found. There were no cases of pneumonia in this series. There were seven upper GI bleeds. Three marginal ulcers occurred, and one of these patients had a UGI bleed from the ulcer. Three patients were returned to the operating room due to evisceration. Of these, one died of a pulmonary embolus following the second operation. Patients with eviscerations were heavier than those without them. One patient developed cholecystitis requiring urgent cholecystectomy, and one patient had an iatrogenic portal vein injury. One patient had an evisceration and died at home a week later.
Thus, there were 64 major complications in 62 patients. Fourteen complications preceded mortality. Although serious, 48 patients suffered complications that they survived. Since all deaths were preceded by a complication, the aggregate number of deaths and complications used for statistical analysis in this series was 62.
There was no statistically significant difference in the anastomotic leak rate between patients receiving and not receiving postoperative CPAP. There were two anastomotic leaks that occurred in the 159 patients receiving postoperative CPAP (1.3%). Among the 908 patients not receiving postoperative CPAP there were 10 anastomotic leaks (1.1%).
There were 71 revision operations in this series. Only six of these patients experienced significant complications. Three of these were anastomotic leaks, one patient developed sepsis without an identifiable source, and two developed bowel obstructions. Of the 62 patients with complications, 56 had primary and 6 had revision operations. The total number of primary operations was 996, giving a complication rate of 5.6%. Six of 71 revision cases had complications, yielding a complication rate of 8.5%. There was no statistically significant increase in complication rates in the revision cases.
One hundred thirteen patients in this series were 55 years of age or older. In this group there were six complications (5.3%). Nine hundred fifty-four patients were less than 55 years old and had 56 complications (5.8%). Four of the 14 (29%) deaths occurred with patients aged greater than 55; thus, the mortality for patients 55 years of age and greater was 3.5%, and that for patients less than 55 years of age was 1.1% (P < .05, chi-square). One of these four deaths occurred in a 478-lb 61-year-old patient who developed sepsis, the source of which could never be identified. The second patient was a 356-lb 57-year-old with known cardiac disease and poor functional status who developed arrhythmias postoperatively, then developed a GI bleed and ultimately hypotension with necrosis of her Roux limb, which culminated in her death from sepsis. The third was a 295-lb 58-year-old patient who died of sepsis following an anastomotic leak. The final patient was a 361-lb 61-year-old man who eviscerated, then developed a perforated colon and died of sepsis and GI bleeds.
Risk Factors Predicting Complications
Analysis of the preoperative risk factors revealed that only weight and male gender were predictive for the development of severe life-threatening complications (Tables 3 and 4). Neither age nor BMI was associated with a greater number of severe life-threatening complications. Smoking history, hypertension, osteoarthritis, diabetes, sleep apnea, use of CPAP, and revision cases also did not correlate with the development of complications. Logistic regression revealed an equation predictive of complications:
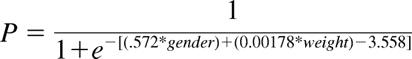 |
where P = the probability of a complication developing, 0 = female gender, 1 = male gender, and the weight is in pounds. Results of sensitivity analysis utilizing this equation are presented in Figure 1. Men have a higher probability of developing complications for all weight ranges and for both women and men there is a nonlinear increase in the probability of having complications with increasing weights, with the rate of increase rising more rapidly for men than women.
Table 3. RISK FACTORS PREDICTING COMPLICATIONS—CONTINUOUS VARIABLES
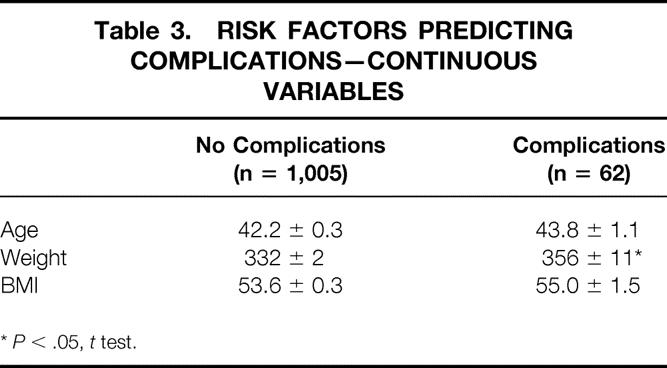
*P < .05, t test.
Table 4. RISK FACTORS PREDICTING COMPLICATIONS—DICHOTOMOUS VARIABLES
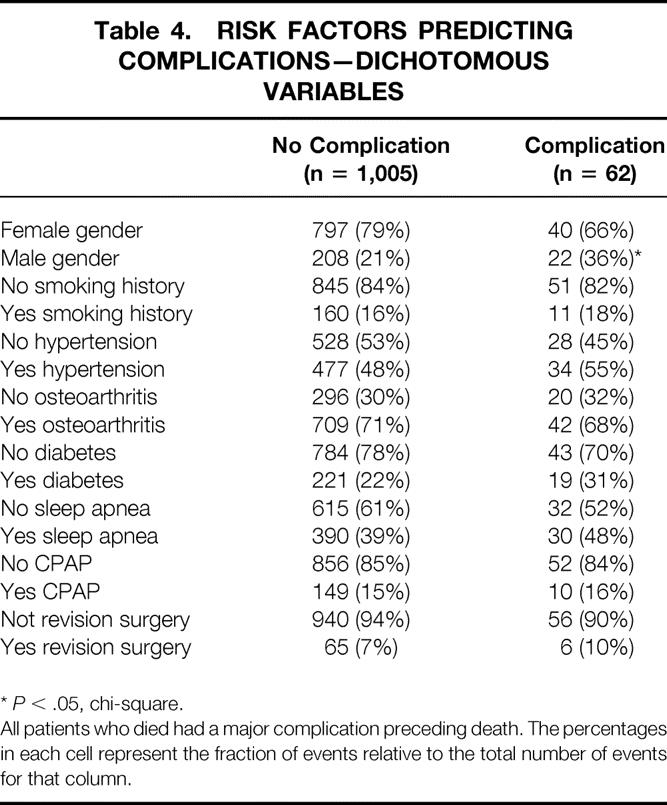
*P < .05, chi-square.
All patients who died had a major complication preceding death. The percentages in each cell represent the fraction of events relative to the total number of events for that column.
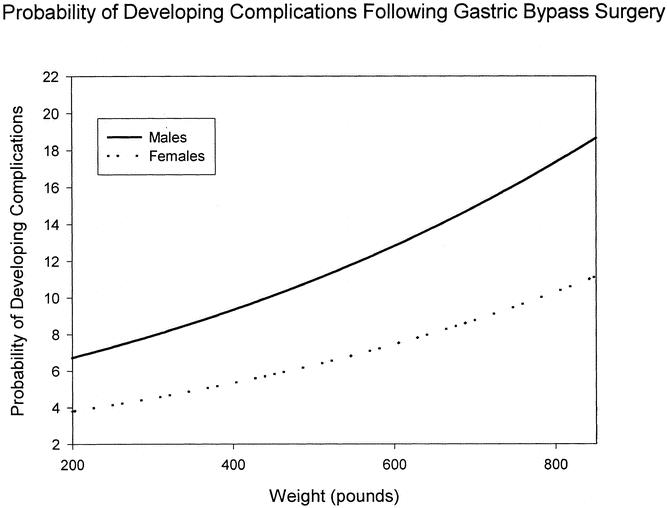
Figure 1. Sensitivity analysis of the effect of gender and weight on the risk of adverse events for patients undergoing Roux-en-Y gastric bypass surgery. The probability of adverse events is represented on the ordinate and weight on the axis of the graph. For a 200-lb women, the risk of developing complications is slightly less than 4% and rises to 12% at 900 lb. The complication risk is higher for men at each weight and rises more steeply for men compared to women as weight increases. A 200-lb man has a 6.5% risk of complications that increases to 20% at 900 lb.
DISCUSSION
This report is the largest reported single-institution gastric bypass series prospectively examining risk factors predictive for severe life-threatening postoperative complications. Male gender and superobesity were the most significant predictors of severe life-threatening complications following these operations. Although the morbidity rate was the same in older and younger patients, those over 55 years of age had a threefold-higher mortality rate relative to younger patients, suggesting that younger patients tolerate complications better than older ones. In contrast to most other series, the complication rate for revision procedures was no greater than for primary operations.
Despite the high risk for pulmonary complications in obese patients, there were no cases of postoperative pneumonia. The use of CPAP in our patients following surgery apparently prevented respiratory complications without inducing anastomotic complications. Use of positive pressure ventilation for patients immediately following gastric anastomosis has the potential complication of air insufflation of the stomach, with consequent anastomotic disruption. Sleep apnea was present in one third of female and nearly two thirds of male patients in our series. Many patients were CPAP-dependent, requiring it immediately postoperatively to avoid hypoventilation. The anastomotic leak rate was the same for patients who received or did not receive postoperative CPAP (1.3% vs. 1.1%). These anastomotic leak rates are consistent with those reported in most other gastric bypass series; however, in contrast to previous reports, we did not have any cases of pneumonia. 7 This finding suggests that CPAP use protected patients from respiratory complications without resulting in anastomotic leakage.
Major complications following revision operations have been more frequent than in primary gastric bypass procedures in most reported series. 8–11 Anastomotic leaks following revision procedures were reported in 8.3% of cases, compared to 2.0% for primary operations, in an early series of gastric bypass procedures. 12 In 58 patients undergoing conversion of vertical banded gastroplasty to gastric bypass, Sugerman et al. reported several leaks, but 20 patients developed anastomotic stricture or marginal ulceration. 13 Most of our revision surgeries were conversions of banded gastroplasties to Roux-en-Y gastric bypass, similar to the series reported by Sugerman et al. When performing revision gastric bypass for strictured banded or ring gastroplasties with intact staple lines, we mobilize only the lesser curve immediately adjacent to the strictured pouch outlet and wedge the band with GIA staplers, performing a partial gastric resection. We then anastomose the Roux-en-Y limb to the anterior surface of the pouch, completely eliminating dissection of the posterior pouch and greater curvature.
Conversion of patients with small bowel bypasses to gastric bypass can have very high complication rates. 14 When revising jejunoileal bypasses, we stage the procedures. Because the bypassed small bowel limb is usually atrophic, the risk of anastomotic stricture is high if it is used for an anastomosis. We reverse the jejunojejunostomy at the first operation, then perform the gastric bypass 6 to 12 months later when the bowel atrophy has resolved. The major complication rate of 5.8% for revision operation is identical to that reported in a series where most conversion operations were to a gastric bypass. 15
Morbid obesity is commonly associated with a high risk for the development of deep venous thrombosis and pulmonary embolism. Venous stasis is frequent in obese individuals. Additionally, obesity is associated with elevated plasma lipids, which in turn can accelerate clotting mechanisms. 16 Retrospective surgical series and autopsy studies have suggested that obesity is an independent risk factor for the development of pulmonary emboli. 17 Results of 131I-labeled fibrinogen experiments evaluating thrombus deposition following surgery have shown conflicting results. Some have demonstrated increases in obese patients, 18 whereas others have not. 19 Joint replacements are associated with a very high rate of deep venous thrombosis and pulmonary embolus, but no increase in these complications attributable to obesity has been found. 20 Review of several gastric bypass series revealed that the incidence of pulmonary embolus is approximately 0.6% to 0.7%, frequencies comparable to the 0.8% observed in our series. 21 Although the incidence of pulmonary emboli is low, when they occur they are often fatal: we found that two thirds of patients with pulmonary emboli died. All our patients received venous thrombosis prophylaxis consisting of both lower extremity pulsatile stockings and subcutaneous heparin. We use both methodologies because the stockings fit poorly on patients with very large legs. Since all patients received this prophylactic regimen, we cannot determine its effect on pulmonary embolism. However, because the outcomes for pulmonary emboli are poor and the risks of prophylaxis negligible, we advocate aggressive venous embolus prophylaxis for obese patients undergoing gastric bypass surgery.
Obesity has been identified as an independent risk factor for the development of fascial dehiscence. 22 Despite the massive tension placed on abdominal wounds in obese patients, fascial dehiscence is uncommon: only 0.3% of cases in our series experienced a dehiscence. The three patients with this complication weighed 521, 398, and 352 lb. Although these three patients were heavier on a statistical basis than those without the complication, this was due to the 521-lb patient skewing the data. No specific risk factor could account for this complication. Fascial dehiscence with evisceration is uncommon in obesity surgery. A randomized controlled trial of running versus interrupted closure techniques confirmed that this complication is uncommon and that running closures are safe in this high-risk group of patients. 23
There have been conflicting reports regarding the safety of bariatric procedures in elderly patients. 24,25 For our series, univariate analysis failed to demonstrate age as an independent risk factor predictive of adverse events. However, when mortality was categorized by groups of patients aged above or below 55 years old, a significant pattern emerged. The mortality rate for patients more than 55 years old was 3.5% versus 1.1% (P < .05, chi-square analysis) for those less than 55. Printen and Mason found a higher mortality for older patients undergoing gastric bypass procedures. 24 In their series of 503 patients, 36 were more than 50 years old. There was an 8% mortality in the older patients compared to 2.8% for younger patients. Both groups had a mortality double that of our series, most likely reflecting overall better surgical results in the modern era compared to 30 years ago, when that study was performed. However, the threefold increase in mortality for older patients remains the same. Most likely, older patients are less able to tolerate operative complications, resulting in higher mortality rates superimposed on a similar incidence of complications. Macgregor and Rand reported no increase in mortality for a series of 77 patients undergoing various obesity operations including gastric bypass and gastroplasty. 25 The mean weight for these patients was 227 lb for women and 268 lb for men. They found no increase in age-specific morbidity and mortality. The difference between these results and ours and Printen and Mason’s probably reflects a cohort of smaller patients, most of whom underwent the less technically complex gastroplasty operation.
The major purpose of our study was to identify major, life-threatening complications of gastric bypass. Our ultimate goal was to identify controllable risk factors to facilitate identification of high-risk patients. We did not analyze less than life-threatening complications. Minor complications are frequent in bariatric surgery: wound infections occur in 15%, 26 venous thrombosis in 2%, and incisional hernias in 15% to 20%27 of cases. Taken together, the major and minor bariatric surgery complication rate is high for elective surgery, mandating appropriate counseling for prospective patients.
The National Bariatric Surgery Registry maintains a database of voluntarily reported outcomes from numerous centers performing obesity operations. Analysis of 5,178 bariatric operations revealed that larger men were more likely to experience complications. 28 This series included a variety of operations; only 29% of them were gastric bypasses, and none of the procedures analyzed were revision cases. On average, men undergoing antiobesity operations were larger than women in the current series and in the cases reported to the Registry. In contrast to Printen and Mason’s registry report, we did not find an association between the patient’s age or BMI and the development of postoperative complications. Although the mortality was higher in our older patients, the rate at which complications developed was unaffected by age. Taken together, our data suggest that very large men be counseled to lose weight before gastric bypass surgery to minimize the risk of adverse outcomes. Alternative procedures such as jejunoileal bypass may be considered in these otherwise high-risk patients. Older patients have a higher mortality than younger ones. Mortality for older patients is within acceptable limits, but they should be counseled regarding the higher risk relative to younger patients.
Footnotes
Supported by the UCLA Training Grant in Nutrition and Obesity, Grant No. T32 DK 07688 (D.H.).
Correspondence: Edward H. Livingston, MD, Director, UCLA Bariatric Surgery Program, UCLA General Surgery, 10833 Le Conte, 72-215 CHS, Los Angeles, CA 90095-6904.
E-mail: elivingston@mednet.ucla.edu
Accepted for publication February 21, 2002.
References
- 1.Manson JE, Willett WC, Stampfer MJ, et al. Body weight and mortality among women. N Engl J Med 1995; 333: 677–685. [DOI] [PubMed] [Google Scholar]
- 2.Stevens J, Cai J, Pamuk ER, et al. The effect of age on the association between body-mass index and mortality. N Engl J Med 1998; 338: 1–7. [DOI] [PubMed] [Google Scholar]
- 3.Drenick EJ, Bale GS, Seltzer F, et al. Excessive mortality and causes of death in morbidly obese men. JAMA 1980; 243: 443–445. [PubMed] [Google Scholar]
- 4.Pi-Sunyer FX. Short-term medical benefits and adverse effects of weight loss. Ann Intern Med 1993; 119: 722–726. [DOI] [PubMed] [Google Scholar]
- 5.Williamson DF, Pamuk ER. The association between weight loss and increased longevity: A review of the evidence. Ann Intern Med 1993; 119: 731–736. [DOI] [PubMed] [Google Scholar]
- 6.Methods for Voluntary Weight Loss, Control. Proceedings of NIH Technology Assessment Conference. Bethesda, MD, 30 March-1 April 1992. Ann Intern Med 1993; 119:641–770. [PubMed]
- 7.Flancbaum L, Choban PS. Surgical implications of obesity. Annu Rev Med 1998; 49: 215–234. [DOI] [PubMed] [Google Scholar]
- 8.Buckwalter JA, Herbst CA Jr, Khouri RK. Morbid obesity. Second gastric operations for poor weight loss. Am Surg 1985; 51: 208–211. [PubMed] [Google Scholar]
- 9.Sugerman HJ, Wolper JL. Failed gastroplasty for morbid obesity. Revised gastroplasty versus Roux-Y gastric bypass. Am J Surg 1984; 148: 331–336. [DOI] [PubMed] [Google Scholar]
- 10.Linner JH. Revisional surgery. In Linner JH, ed. Surgery for Morbid Obesity. New York: Springer-Verlag, 1984: 109–126.
- 11.Forse RA, Deitel M, MacLean LD. The conversion of a horizontal to vertical banded gastroplasty: a hazardous procedure. Gastroenterol Clin North Am 1987; 16: 533–535. [PubMed] [Google Scholar]
- 12.Buckwalter JA, Herbst CA Jr. Leaks occurring after gastric bariatric operations. Surgery 1988; 103: 156–160. [PubMed] [Google Scholar]
- 13.Sugerman HJ, Kellum JM Jr, DeMaria EJ, et al. Conversion of failed or complicated vertical banded gastroplasty to gastric bypass in morbid obesity. Am J Surg 1996; 171: 263–269. [DOI] [PubMed] [Google Scholar]
- 14.Cates JA, Drenick EJ, Abedin MZ, et al. Reoperative surgery for the morbidly obese. A university experience. Arch Surg 1990; 125: 1400–1403. [DOI] [PubMed] [Google Scholar]
- 15.Peltier G, Hermreck AS, Moffat RE, et al. Complications following gastric bypass procedures for morbid obesity. Surgery 1979; 86: 648–654. [PubMed] [Google Scholar]
- 16.Conner WZ. The acceleration of thrombus formation by certain amino acids. J Clin Invest 1962; 41: 1199–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coon WW. Risk factors in pulmonary embolism. Surg Gynecol Obstet 1976; 143: 385–390. [PubMed] [Google Scholar]
- 18.Borow M, Goldson H. Postoperative venous thrombosis. Evaluation of five methods of treatment. Am J Surg 1981; 141: 245–251. [DOI] [PubMed] [Google Scholar]
- 19.Printen KJ, Miller EV, Mason EE, et al. Venous thromboembolism in the morbidly obese. Surg Gynecol Obstet 1978; 147: 63–64. [PubMed] [Google Scholar]
- 20.Lemos MJ, Sutton D, Hozack WJ, et al. Pulmonary embolism in total hip and knee arthroplasty. Risk factors in patients on warfarin prophy-laxis and analysis of the prothrombin time as an indicator of warfarin’s prophylactic effect. Clin Orthop 1992; 158–163. [PubMed] [Google Scholar]
- 21.Pasulka PS, Bistrian BR, Benotti PN, et al. The risks of surgery in obese patients. Ann Intern Med 1986; 104: 540–546. [DOI] [PubMed] [Google Scholar]
- 22.Riou JP, Cohen JR, Johnson HJ. Factors influencing wound dehiscence. Am J Surg 1992; 163: 324–330. [DOI] [PubMed] [Google Scholar]
- 23.McNeil PM, Sugerman HJ. Continuous absorbable vs. interrupted nonabsorbable fascial closure. A prospective, randomized comparison. Arch Surg 1986; 121: 821–823. [DOI] [PubMed] [Google Scholar]
- 24.Printen KJ, Mason EE. Gastric bypass for morbid obesity in patients more than fifty years of age. Surg Gynecol Obstet 1977; 144: 192–194. [PubMed] [Google Scholar]
- 25.Macgregor AM, Rand CS. Gastric surgery in morbid obesity: Outcome in patients aged 55 and older. Arch Surg 1993; 128: 1153–1157. [DOI] [PubMed] [Google Scholar]
- 26.Derzie AJ, Silvestri F, Liriano E, et al. Wound closure technique and acute wound complications in gastric surgery for morbid obesity: A randomized prospective trial. J Am Coll Surg 2000; 191: 238–243. [DOI] [PubMed] [Google Scholar]
- 27.Byrne TK. Complications of surgery for obesity. Surg Clin North Am 2001; 81: 1181–1193. [DOI] [PubMed] [Google Scholar]
- 28.Mason EE, Renquist KEJS. Perioperative risks and safety of surgery for severe obesity. Am J Clin Nutr 1992; 55: 573S–576S. [DOI] [PubMed] [Google Scholar]