Abstract
Objective
Clinical studies show that the incidence of postoperative wound complications is higher in smokers than nonsmokers. In this study, we evaluated the effect of abstinence from smoking on incisional wound infection.
Methods
Seventy-eight healthy subjects (48 smokers and 30 never-smokers) were included in the study and followed for 15 weeks. In the first week of the study, the smokers smoked 20 cigarettes per day. Subsequently, they were randomized to continuous smoking, abstinence with transdermal nicotine patch (25 mg per day), or abstinence with placebo patch. At the end of the first week and 4, 8, and 12 weeks after randomization, incisional wounds were made lateral to the sacrum to excise punch biopsy wounds. At the same time identical wounds were made in 6 never-smokers. In 24 never-smokers a wound was made once. All wounds were followed for 2 weeks for development of wound complications.
Results
A total of 228 wounds were evaluated. In smokers the wound infection rate was 12% (11 of 93 wounds) compared with 2% (1 of 48 wounds) in never-smokers (P <0.05). Wound infections were significantly fewer in abstinent smokers compared with continuous smokers after 4, 8, and 12 weeks after randomization. No difference between transdermal nicotine patch and placebo was found.
Conclusions
Smokers have a higher wound infection rate than never-smokers and 4 weeks of abstinence from smoking reduces the incidence of wound infections.
Key Words: smoking cessation, surgical wound infection, wound dehiscence, postoperative complications, nicotine replacement therapy, neutrophils
Smokers who undergo general and orthopedic surgery have a higher incidence of wound infections than nonsmokers.1-3 The proposed mechanism is a detrimental effect of smoking on tissue oxygen,4-8 which impairs the reparative processes of wound healing and the neutrophil defense against surgical pathogens.9-12
Clinical studies show that wound hypoxia predicts wound infection,13 and that perioperative supplemental oxygen increases tissue oxygen tension and decreases incisional wound infection.14,15 Recently, a study found that smoking intervention before hip and knee alloplasty reduces postoperative wound infections.16
We hypothesized that smoking abstinence enhances wound healing and decreases the risk of infection. Accordingly, we aimed to identify the optimal period of abstinence from smoking by evaluating wounds in habitual smokers applied during smoking and after 4, 8, and, 12 weeks of abstinence, and in addition, to test the effect of transdermal nicotine patch versus placebo.
MATERIALS AND METHODS
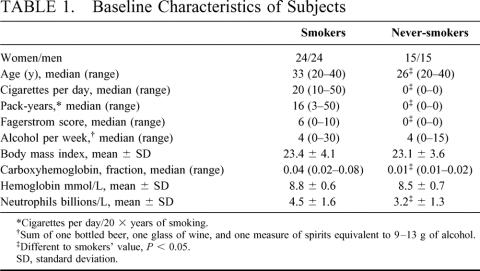
Seventy-eight healthy subjects between 18 and 40 years of age were included in the study after obtaining written informed consent according to the Helsinki II declaration. Forty-eight were smokers with a history of smoking 20 cigarettes per day for at least 2 years and 30 never-smokers were control subjects. Subjects were matched for gender between both groups and similar age was aimed (Table 1). Exclusion criteria were chronic medical disease, atopic dermatitis or other skin disease, pregnancy, menopause, allergy to local anesthetics, dressing, or patches, and current or recent medication with corticosteroids, NSAID, or aspirin. The Ethical Committee of Copenhagen approved the study (KF 02-037/00).
TABLE 1. Baseline Characteristics of Subjects
The study period covered 15 weeks. During the first week smokers smoked 20 filter cigarettes per day (Red Prince, Scandinavian Tobacco Company A/S, Copenhagen, Denmark). From the second week, they were randomized to continuous smoking (20 cigarettes per day), smoking abstinence with transdermal nicotine patch (15 mg/16 h plus 10 mg/16 h, Nicorette, Pharmacia & Upjohn A/S, Copenhagen, Denmark), or smoking abstinence with placebo patch. Each subgroup comprised 8 women and 8 men.
A total of 4 sutured incisional wounds were made to excise a 5-mm full-thickness punch biopsy wound, which had been made lateral to the sacrum 7 days earlier as a wound healing model.17 The first wound was made at the end of the first week of smoking and the subsequent wounds 4, 8, and, 12 weeks after randomization to either treatment. The first and third wounds were made to the right of the sacrum and the second and fourth made to the left of the sacrum. In the control group identical wounds were made at the same time in 6 never-smokers, whereas a wound was made once in the remaining 24 never-smokers.
Under local anesthesia with 20 mL 1% mepivacaine with adrenalin and after surgical disinfection with 0.5% ethanol-chlorhexidine liniment, the biopsy wound was excised by 2 curved incisions producing an elliptical wound 15-to 18-mm long and 8- to 10-mm wide. The wound was sutured with Ethilon 4-0 nonabsorbable suture or intradermally with Vicryl Rapid 3-0 absorbable suture (Ethicon, Norderstedt, Germany). Nonabsorbable wound sutures were removed 10 days after excision.
All wounds were followed for 2 weeks and complications were recorded. A surgeon and a wound-healing expert unaware of the subjects’ group assignment evaluated the wounds clinically. A wound infection was defined according to the National Prevalence Survey study group as purulent discharge with or without wound dehiscence or painful, hot extending erythema indicative of cellulitis.18,19 A wound rupture was defined as a complete separation of wound edges without signs of infection. All wound infections were treated with Dicloxacillin for 5 days. Wound ruptures healed on second intention.
Before excision of biopsy wounds, peripheral venous blood was drawn in potassium-EDTA test tubes to determine hemoglobin and neutrophil count and in heparin test tubes to determine carboxyhemoglobin and plasma cotinine. Hemoglobin and carboxyhemoglobin were determined by an ABX Pentra 120 and an ABL 700, respectively (Radiometer A/S, Copenhagen, Denmark). Neutrophil count level was determined by a Technicon cell counter (Technicon, NY, US), and cotinine level was determined by a HP 5890A gas chromatograph (USA). A CO breath test (MicroSmokerlyzer, Bedfont Instruments, UK) in all smokers was recorded twice a week as well as use of nicotine patches by those randomized to abstinence.
Comparison between groups was performed with Fisher’s exact test for binary data. Unpaired and paired continuous data was analyzed with Student t-test or Mann-Whitney U test depending on the distribution. Effect of transdermal nicotine patch was estimated by Fisher’s exact test or by one-factor analysis of variance (ANOVA). The level of statistical significance was set at P <0.05.
RESULTS
Seventy-four of 78 subjects (95%) completed the study. Four smokers withdrew of whom 1 was randomized to continuous smoking and 3 were randomized to abstinence.
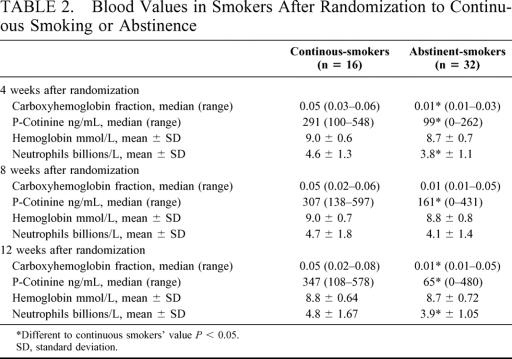
The carboxyhemoglobin level was higher in smokers compared with never-smokers (Table 1). After 4 weeks of abstinence carboxyhemoglobin level fell to a minimum in abstinent smokers compared with the period with smoking (P <0.05) (Table 2). Similar results were found with CO breath tests (data not shown). Likewise, the cotinine level was lower in the abstinent group. When comparing the group randomized to nicotine patch to the placebo group, the latter had a lower cotinine level after 4 weeks (180 [range, 18-262] vs 7 [range, 0-153], P <0.05), after 8 weeks (257 [range, 9-431] vs 8 [range, 0-294], P <0.05), and after 12 weeks of abstinence (201 [range, 6-480] vs 0 [range, 0-268], P <0.05).
TABLE 2. Blood Values in Smokers After Randomization to Continuous Smoking or Abstinence
The neutrophil count was higher in smokers than in those who never smoked (Table 1). After 4 weeks of abstinence, the neutrophil count declined by 17% (P <0.05), irrespective of transdermal nicotine patch or placebo, and remained reduced throughout the study (Table 2). In contrast, hemoglobin level was not affected by smoking or abstinence.
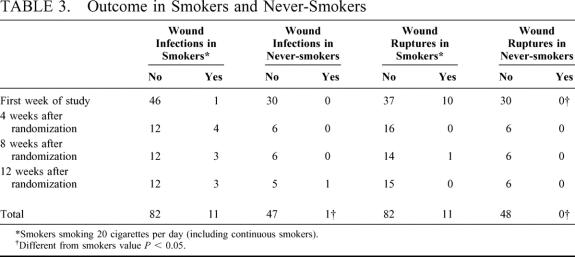
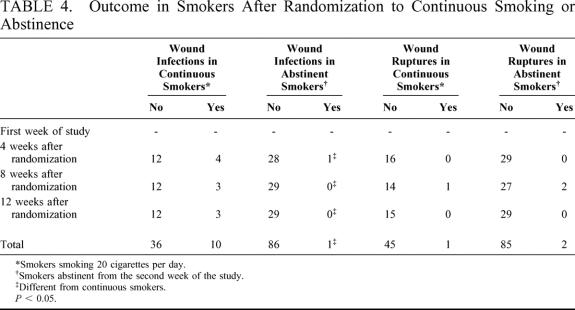
The total wound infection rate in smokers was 12% compared with 2% in never smokers (P <0.05) (Table 3). After 4 weeks of randomization wound infections were significantly fewer in the abstinent smokers’ group compared with the group of continuous smokers (Table 4). Similar differences were found after 8 and 12 weeks of randomization. The total wound infection rate in abstinent smokers was 1% (P <0.05) when compared with smokers).
TABLE 3. Outcome in Smokers and Never-Smokers
TABLE 4. Outcome in Smokers After Randomization to Continuous Smoking or Abstinence
Wound ruptures occurred in 12% of the smokers compared with none in never-smokers (P <0.05). No difference between abstinent smokers and continuous smokers was found after 4, 8, or 12 weeks of randomization.
The technique of wound closure did not affect the incidence of either wound complication. No difference between transdermal nicotine patch and placebo was found.
DISCUSSION
The incidence of infection and rupture of incisional wounds was significantly higher in smokers compared with never-smokers. Abstinence from smoking reduced the infection rate, but did not affect wound ruptures.
We aimed to identify the optimal abstinence period in habitual heavy smokers to enhance wound healing, and found that 4 weeks of abstinence reduced wound infections to a level similar to never-smokers. This finding suggests that 1 month of preoperative abstinence might be sufficient to reduce postoperative wound infections.
The neutrophil count was higher in smokers compared with never-smokers and decreased after 4 weeks of abstinence. This finding is consistent with other studies, which found a decline in neutrophil count in healthy smokers after 2 and 6 weeks of abstinence.20,21 Accordingly, a reduction in neutrophil count in healthy abstinent smokers appears to occur independent of wound infection. We hypothesize that the function and bactericidal activity of neutrophils is modified by smoking and reverted by abstinence, and studies are now in progress.
Abstinence from smoking did not affect the incidence of wound ruptures within 12 weeks after smoking cessation. The difference in wound rupture between smokers and never-smokers is consistent with experimental and clinical studies, which have found less collagen production and a higher incidence of postoperative tissue and wound dehiscence in smokers.9,22-24 The fact that no difference in wound rupture between continuous and abstinent smokers was found challenges the hypothesis that tissue hypoxia induced by smoking is the primary cause for reduced collagen production and wound dehiscence in smokers.5,9,22
We did not find any adverse effect on wound infection or rupture by use of transdermal nicotine patches during abstinence. This finding adds to others, which found minor adverse effects like sleep disturbances and nausea to be associated with transdermal nicotine patch.25 The administered dose of 25 mg of nicotine per day was intended to be equal to the amount of nicotine delivered by smoking 20 cigarettes per day and not lower than the amount delivered by a standard nicotine replacement therapy.26
The punch biopsy wound healing model has previously been used on the inside of the upper arm and no complications have been reported.17 In our study, the area lateral of the sacrum below the belt was unexposed to sunlight and was chosen for cosmetic reasons. Each wound healed independent of the previous, which was ensured by the placing and the interval of 4 weeks between the wounds. The punch biopsy wound was covered with a semiocclusive dressing until excision, but potential contamination from the adjacent anal region cannot be excluded. The location of the wounds might have implied considerable traction on the wound edges. Yet, all wounds were applied under identical conditions in all subjects.
In conclusion, healthy smokers have a higher incidence of wound infections and ruptures than never-smokers, and 4 weeks of abstinence from smoking reduces wound infections to a level similar to never-smokers.
ACKNOWLEDGMENTS
This study was supported by grants from The Danish Research Council (no. 9801273) and The Danish Health Insurance Fund. Pharmacia & Upjohn sponsored transdermal nicotine patches and Scandinavian Tobacco Company the cigarettes used in the study. The authors thank nurse U. Hemmingsen and laboratory technician R. Roel for their generous assistance.
Footnotes
Reprints: Lars Tue Sorensen, MD, Department of Surgery K, Bispebjerg University Hospital, DK-2400 Copenhagen NV, Denmark. E-mail: lts@dadlnet.dk.
REFERENCES
- 1.Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–1215. [DOI] [PubMed] [Google Scholar]
- 2.Lind J, Kramhoft M, Bodtker S. The influence of smoking on complications after primary amputations of the lower extremity. Clin Orthop. 1991;267:211–217. [PubMed] [Google Scholar]
- 3.Sorensen LT, Horby J, Friis E, et al. Risk factors for impaired wound healing and infection in breast cancer surgery. Eur J Surg Oncol 2002;28;815–820. [DOI] [PubMed] [Google Scholar]
- 4.Morecraft R, Blair WF, Brown TD, et al. Acute effects of smoking on digital artery blood flow in humans. J Hand Surg. 1994;19:1–7. [DOI] [PubMed] [Google Scholar]
- 5.Jensen JA, Goodson WH, Williams H, et al. Cigarette smoking decreases tissue oxygen. Arch Surg. 1991;126:1131–1134. [DOI] [PubMed] [Google Scholar]
- 6.Cryer PE, Haymond MW, Santiago JV, et al. Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events. N Engl J Med. 1976;295:573–577. [DOI] [PubMed] [Google Scholar]
- 7.Jensen JA, Jonsson K, Goodson WH, et al. Epinephrine lowers subcutaneous wound oxygen tension. Curr Surg. 1985;42:472–474. [PubMed] [Google Scholar]
- 8.Astrup P, Hellung-Larsen P, Kjeldsen K, et al. The effect of tobacco smoking on the dissociation curve of oxyhemoglobin. Investigations in patients with occlusive arterial diseases and in normal subjects. Scand J Clin Lab Invest. 1966;18:450–457. [DOI] [PubMed] [Google Scholar]
- 9.Jorgensen LN, Kallehave F, Christensen E, et al. Less collagen production in smokers. Surgery. 1998;123:450–455. [PubMed] [Google Scholar]
- 10.Hunt TK, Hopf HW. Wound healing and wound infection. What surgeons and anesthesiologists can do. Surg Clin North Am. 1997;77:587–606. [DOI] [PubMed] [Google Scholar]
- 11.Babior BM. Oxygen-dependent microbial killing by phagocytes. N Engl J Med. 1978;298:659–668. [DOI] [PubMed] [Google Scholar]
- 12.Allen DB, Maguire JJ, Mahdavian M, et al. Wound hypoxia and acidosis limit neutrophil bacterial killing mechanisms. Arch Surg. 1997;132:991–996. [DOI] [PubMed] [Google Scholar]
- 13.Hopf HW, Hunt TK, West JM, et al. Wound tissue oxygen tension predicts the risk of wound infection in surgical patients. Arch Surg. 1997;132:997–1004. [DOI] [PubMed] [Google Scholar]
- 14.Greif R, Akca O, Horn EP, et al. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. Outcomes Research Group. N Engl J Med. 2000;342:161–167. [DOI] [PubMed] [Google Scholar]
- 15.Gottrup F. Prevention of surgical-wound infections. N Engl J Med. 2000;342:202–204. [DOI] [PubMed] [Google Scholar]
- 16.Moller AM, Villebro N, Pedersen T, et al. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet. 2002;359:114–117. [DOI] [PubMed] [Google Scholar]
- 17.Ashcroft GS, Greenwell-Wild T, Horan MA, et al. Topical estrogen accelerates cutaneous wound healing in aged humans associated with an altered inflammatory response. Am J Pathol. 1999;155:1137–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruce J, Russell EM, Mollison J, et al. The quality of measurement of surgical wound infection as the basis for monitoring: a systematic review. J Hosp Infect. 2001;49:99–108. [DOI] [PubMed] [Google Scholar]
- 19.National prevalence survey of hospital acquired infections: definitions. A preliminary report of the Steering Group of the Second National Prevalence Survey. J Hosp Infect. 1993;24:69-76. [DOI] [PubMed]
- 20.Bain BJ, Rothwell M, Feher MD, et al. Acute changes in haematological parameters on cessation of smoking. J R Soc Med. 1992;85:80–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jensen EJ, Pedersen B, Frederiksen R, et al. Prospective study on the effect of smoking and nicotine substitution on leucocyte blood counts and relation between blood leucocytes and lung function. Thorax. 1998;53:784–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sorensen LT, Jorgensen T, Kirkeby LT, et al. Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg. 1999;86:927–931. [DOI] [PubMed] [Google Scholar]
- 23.Fawcett A, Shembekar M, Church JS, et al. Smoking, hypertension, and colonic anastomotic healing; a combined clinical and histopathological study. Gut. 1996;38:714–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sorensen LT, Friis E, Jorgensen T, et al. Smoking is a risk factor for recurrence of groin hernia. World J Surg. 2002;26:397–400. [DOI] [PubMed] [Google Scholar]
- 25.Greenland S, Satterfield MH, Lanes SF. A meta-analysis to assess the incidence of adverse effects associated with the transdermal nicotine patch. Drug Safety. 1998;18:297–308. [DOI] [PubMed] [Google Scholar]
- 26.Fant RV, Owen LL, Henningfield JE. Nicotine replacement therapy. Primary Care. 1999;26:633–652. [DOI] [PubMed] [Google Scholar]